Abstract
To evaluate low-dose X-ray radiation effects on the eye by measuring the amount of light scattering in specific regions of the lens, we compared exposed subjects (interventional radiologists) with unexposed subjects (employees of medical service companies), as a pilot study. According to numerous exclusionary rules, subjects with confounding variables contributing to cataract formation were excluded. Left eye examinations were performed on 68 exposed subjects and 171 unexposed subjects. The eye examinations consisted of an initial screening examination, followed by Scheimpflug imaging of the lens using an anterior eye segment analysis system. The subjects were assessed for the quantity of light scattering intensities found in each of the six layers of the lens. Multiple stepwise regression analyses were performed with the stepwise regression for six variables: age, radiation exposure, smoking, drinking, wearing glasses and workplace. In addition, an age-matched comparison between exposed and unexposed subjects was performed. Minimal increased light scattering intensity in the posterior subcapsular region showed statistical significance. Our results indicate that occupational radiation exposure in interventional radiologists may affect the posterior subcapsular region of the lens. Since by its very nature this retrospective study had many limitations, further well-designed studies concerning minimal radiation-related lens changes should be carried out in a low-dose exposure group.
Keywords: eye lens, cataract, radiation-related lens change, interventional radiology, occupational radiation exposure
INTRODUCTION
The lens of the eye is recognized as one of the most radio-sensitive tissues in the human body, and radiation-induced cataract is a well-known adverse effect. From a review of epidemiologic data, the threshold dose for cataract formation may be judged to be 0.5 Gy [1, 2]. A recent draft report by the International Commission on Radiological Protection (ICRP) documented that better techniques for detecting, quantifying and documenting early radiation-associated lens changes, as well as better dosimetry, have potentially contributed to recent findings of radiation cataract risk at lower exposure levels than previously considered [3]. For occupational exposure, a new ICRP positional statement recommended that an equivalent dose limit for the lens be reduced from 150 mSv/year to 20 mSv/year, averaged over defined periods of 5 years, with no single year exceeding 50 mSv [2].
The cross-sectional data from astronauts and matched subjects found using an automated anterior eye segment analysis system (EAS-1000, NIDEK, Aichi, Japan) were analyzed and revealed a small deleterious effect of space radiation for cortical cataracts and possibly for PSC cataracts [4]. We hypothesized that interventional radiologists (IRs) are exposed to low-dose scattered radiation, which may cause radiation-related lens changes well before they would otherwise be appreciated by slit-lamp examination, and may therefore be picked up by directed objective scoring systems [5, 6]. Even recent studies [7, 8] lack quantitative assessment of radiation-induced lens changes utilizing the metric variable of light scattering intensities (LSIs). We and others believe that LSIs represent focal aggregated proteins that form from various effects, such as radiation exposure, and that an increase in LSIs might be predictive of cataract formation [9, 10]. To evaluate minimal LSI changes in specific regions in the lens of the eye, we carried out a pilot study on our described exposed subjects and unexposed subjects using EAS-1000.
MATERIALS AND METHODS
Screening examination and subjects
Following institutional review board (IRB) approval, written informed consent was obtained from all participants. All exposed subjects were Japanese volunteer male IRs in the Japanese Society of Interventional Radiology (JSIR), and all unexposed subjects were Japanese volunteer male employees of medical service companies with no history of occupational radiation exposure. Exposed subjects' examinations were conducted during the annual JSIR meeting in Osaka, Japan, on 18–19 May 2006, and unexposed subjects' examinations took place in Tokyo, Japan, 31 May and 1 June 2007. Examiners were aware of the status of the two groups, specifically whether they were exposed or unexposed subjects. Eye examinations were performed following a health survey questionnaire inquiring about eye health, general medical health and lifestyle. Questions included age, radiation exposure in interventional procedures (yes/no), smoking (smoking index = cigarettes smoked per day × years of smoking), drinking (ever/never), wearing glasses (ever/never) and solar ultraviolet ray exposure during working hours (working indoors only, versus working both indoors and outdoors). For the exposed subjects of IRs the survey also included a self-report of professional experience as an IR.
A team of ophthalmologists performed all initial examinations. To screen suitable subjects for pharmacologic mydriasis, an ophthalmologist performed an initial screening slit-lamp examination (Slit Lamp BQ 900 HAAG-STREIT, Koeniz, Switzerland) of the left eye anterior eye segment, in addition to intraocular pressure measurement (Non-contact totometer NT-4000, NIDEK, Aichi, Japan). One hundred and sixty exposed subjects and 326 unexposed subjects were included following screening and mydriasis safety assessment, and subsequently underwent examination of the left eye with pharmacologic pupillary dilation using a drop of Midrin-P (tropicamide and phenylephrine; Santen Pharmaceuticals, Japan). Because the examinations were performed in the daytime while exposed subjects were attending their annual professional society meeting, and during the daytime while the unexposed subjects were also working, only single eye pharmacologic dilations were performed. Therefore only examination of the left eye was conducted. The left side was specifically chosen since the IR's left eye is closer than the right eye to the X-ray tube in the vast majority of instances. In addition a recent study showed that the dose on the side nearest to the X-ray tube was three to five times greater than for the farthest side of the head [11].
Quantitative analyses
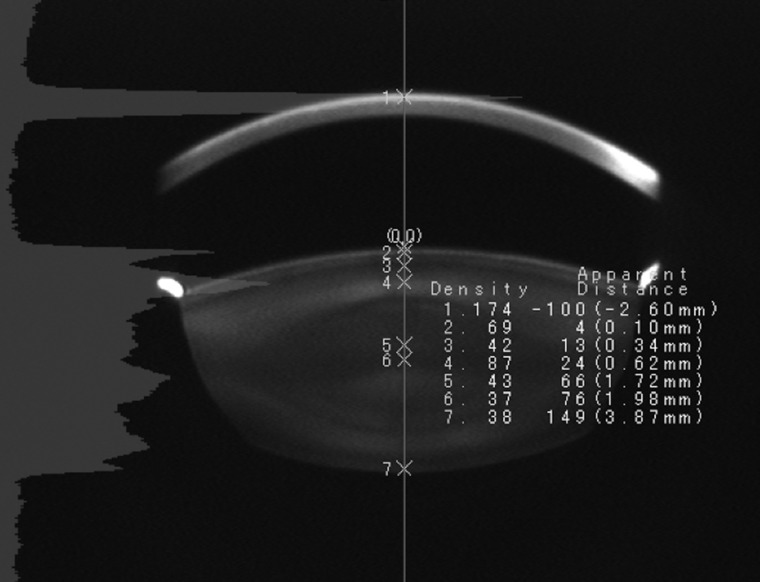
For all qualified subjects the lens of the left eye was examined with Scheimpflug slit images obtained using EAS-1000, with a representative slit image shown in Fig. 1. Scheimpflug photography and densitometric image analysis are techniques applied to light scattering measurement and biometry in the anterior eye segment. They reproducibly characterize the anterior eye and allow discrimination of minimal light scattering changes, using a grading system from otherwise aging, disease or toxic effects. These tools help quantify threshold levels or maximum allowable dosages of physical and chemical noxious factors, which are causative or associative with opacifying ocular pathologies. Therefore, most epidemiological studies dealing with ocular pathologies in the lens use either cataract scoring or the Scheimpflug technique [9].
Fig. 1.
Scheimpflug slit image obtained using an anterior eye segment analysis system Digitalized anterior eye segment image is demonstrated at a mid-sagittal section, the front of the cornea is at the top of the image. The seven numbers depicted on the axis sequentially indicate the cornea (1), anterior capsule (2), most transparent layer of the anterior superficial cortex (3), anterior adult nucleus (4), anterior fetal nucleus (5), central clear zone (6) and posterior subcapsular region (7). The peak light scattering intensity for each segment is demonstrated to the right of each respective layer.
One experienced technician performed all examinations using the EAS-1000. The highest quality Scheimpflug photograph obtained in one session was recorded, and quantitative analysis of the crystalline lens LSIs was provided and saved as an 8-bit digital value. The data of exposed and unexposed subjects were analyzed at the same time, although the technologist was not blinded to the condition of exposure status. The peak LSI value was measured in each of the six layers of the lens automatically and measured points were confirmed manually. These six layers included the anterior capsule, the most transparent layer of the anterior superficial cortex, the anterior adult nucleus, the anterior fetal nucleus, the central clear zone and the posterior subcapsular region (PSR) (Fig. 1).
Selection of subjects
Subjects with cataract risk factors other than occupational radiation exposure were excluded from analysis to increase the comparability of the groups and reduce the influence of group bias risk. Such other factors included a history of diabetes mellitus (exposed subjects n= 4; unexposed subjects n= 6), eye trauma (exposed subjects n= 0; unexposed subjects n= 1), ophthalmic surgery (exposed subjects n= 1; unexposed subjects n= 4) and ocular inflammation (exposed subjects n= 0; unexposed subjects n= 2). Subjects with uncorrectable factors causing poor-quality photographs on the EAS-1000 were also excluded (exposed subjects n= 15; unexposed subjects n= 35). Poor photographic factors included insufficient pupillary dilation (exposed subjects n= 44; unexposed subjects n= 62), congenital cataracts (exposed subjects n= 5; unexposed subjects n= 9), excessive myopia by a spherical equivalent (SE) of less than –6.00 diopters (exposed subjects n= 31; unexposed subjects n= 61), excessive hypermetropia by an SE larger than 5.25 diopters (exposed subjects and unexposed subjects n= 0), ocular hypertension (tonometer pressure >20 mmHg) (exposed subjects n= 8; unexposed subjects n= 7), corneal abnormalities (exposed subjects n= 2; unexposed subjects n= 15) and miscellaneous contributory congenital ocular abnormalities (exposed subjects n= 4; unexposed subjects n= 7). Subjects with an insufficient number of lens images to permit proper tabulation were also excluded. The technician performing the EAS-1000 examination performed all determinations of technical factor exclusion criteria.
After consideration of the above exclusion criteria, 92 of the 160 exposed subjects and 155 of the 326 unexposed subjects were excluded. In the final count, many excluded subjects had more than one exclusion criterion. The eligible population for quantitative analyses consisted of 68 exposed subjects and 171 unexposed subjects. None of the selected subjects had any visual complaints or any subjective decrease in visual acuity. Age-related increases in LSIs have been demonstrated in prior investigations as a physiological change [9]. To reduce the effect of aging, the eligible subjects were matched and selected with a chosen ratio of one IR to two randomly selected unexposed subjects within 1-year difference. The age-matched group consisted of 54 exposed subjects and 108 unexposed subjects.
Statistical analysis
For intergroup comparison, Student's t-test was performed for descriptive characteristics and light scattering intensity in the six lens layers. Multiple regression analyses were carried out using the stepwise method to evaluate LSIs in the six layers of the left lens adjusting for age, smoking, drinking, wearing glasses, sunlight exposure during working hours and scattered radiation exposure during working hours. The selected variables were evaluated with an automatic model selection procedure using a sequence of F-tests in the stepwise method (the Pvalue for additional variables was 0.25 and for removal of variables was 0.10). Comparison of the average LSIs between the age-matched groups was performing using analysis of variance (ANOVA). Welch's t-test was used for samples with unequal variances. The statistical analysis was performed using commercial software (JMP 7.01J). Statistical significance was tested assuming a standard Pvalue of 0.05.
RESULTS
In the screening examination for all subjects without exclusion, slit-lamp examination of the left eye under pupillary dilation showed posterior subcapsular cataract (PSC) in three (1.9%) of 160 exposed subjects (45, 62 and 63 years) and one (0.3%) of 326 unexposed subjects (51 years). One exposed subject showed a dense patchy opacity and two showed vacuoles in the PSR on retroillumination images. One unexposed subject showed vacuoles in the PSR. All four subjects were excluded from quantitative analyses because they met other predetermined exclusion criteria (two had excessive myopia and one had poor pupillary dilation in the exposed subjects, and one had excessive myopia in the unexposed subjects).
The characteristics of the study subjects for quantitative analysis are shown in Table 1. There was a significant difference in the ages of the two groups, with the exposed subjects showing a greater age than the unexposed subjects. The light scattering intensity in the six lens layers is shown in Table 2. There were significant differences in the LSIs in five out of six eye layers when comparing exposed subjects with the unexposed subjects.
Table 1.
Descriptive characteristics of the study subjects who met the eligibility criteria
| IRs | Controls | Pvalue | |
|---|---|---|---|
| Variable | (n= 68) | (n= 171) | |
| Age | 42.2 ± 8·5 | 39.8 ± 6·9 | 0.0059 |
| Smoking (yes), n(%) | 40 (58.8) | 115 (67.2) | 0.180 |
| Smoking index | 177·0 ± 28.5 | 211.7 ± 18.0 | 0.06 |
| Drinking (yes), n(%) | 53 (77.9) | 147 (85.9) | 0.080 |
| Wearing glasses (yes), n(%) | 54 (79.4) | 120 (70.5) | 0.101 |
| Workplace (indoors only), n(%) | 68 (100) | 82 (48.0) | <0.0001 |
| Years of interventional experience, | 15.6 ± 7.8 | NA | |
| median (minimum–maximum) | 14 (1–32) | ||
| Total number of angiographies, | 1846.1 ± 1998.6 | NA | |
| median (minimum–maximum) | 1500 (0–10 000) | ||
| Total number of interventions, | 1982.3 ± 2056.5 | NA | |
| median (minimum–maximum) | 1200 (10–12 000) |
IRs = interventional radiologists, Values are means ± SD, NA = not applicable.
Table 2.
Light scattering intensity in the six lens layers between exposed and unexposed group (8-bit grayscale value)
| Layer of lens | IRs | Controls | Pvalue |
|---|---|---|---|
| (n= 68) | (n= 171) | ||
| Anterior capsule | 63.0 ± 7.8 | 60.3 ± 7.9 | 0.020 |
| Most transparent layer of the anterior superficial cortex | 41.1 ± 8.3 | 39.5 ± 7.7 | 0.157 |
| Anterior adult nucleus | 96.6 ± 33.0 | 81.3 ± 25.5 | 0.0002 |
| Anterior fetal nucleus | 50.7 ± 11.5 | 47.4 ± 10.9 | 0.039 |
| Central clear zone | 38.3 ± 9.6 | 35.3 ± 8.4 | 0.018 |
| Posterior subcapsular region | 39.7 ± 14.7 | 36.4 ± 9.6 | 0.043 |
Values are means ± SD.
The results of the stepwise method for LSI assessment in each of the six layers of the eye lens are shown in Table 3. In all six layers of the eye lens, the variable of age was statistically significant for increased LSIs. In the layer of the central clear zone, smoking was also significant for increased LSIs (P= 0.002). In the PSR, radiation exposure from interventional procedures was significant (P= 0.012) for increased LSIs following adjustment for the other variables including age.
Table 3.
Evaluation of light scattering intensity in the six lens layers by multiple regression analysis using the stepwise method in all subjects (n= 239)
| Layer of lens | Variable | Parameter estimate (95% CI) | Pvalue |
|---|---|---|---|
| Anterior capsule | |||
| Age | 0.691 (0.616–0.766) | <0.0001 | |
| Most transparent layer of the anterior superficial cortex | |||
| Age | 0.153 (0.035–0.270) | 0.011 | |
| Workplace | 0.580 (–0.291–1.452) | 0.191 | |
| Smoking | –0.003 (–0.007–0.001) | 0.094 | |
| Anterior adult nucleus | |||
| Radiation exposure | 2.307 (–0.620–5.233) | 0.122 | |
| Age | 2.644 (2.288–2.999) | <0.0001 | |
| Work place | 1.793 (–0.910–4.496) | 0.192 | |
| Anterior fetal nucleus | |||
| Age | 1.405 (1.235–1.574) | <0.0001 | |
| Smoking | 0.003 (–0.002–0.008) | 0.290 | |
| Wearing glasses | –1.072 (–2.785–0.641) | 0.219 | |
| Central clear zone | |||
| Age | 1.132 (1.057–1.207) | <0.0001 | |
| Smoking | 0.004 (0.001–0.006) | 0.002 | |
| Posterior subcapsular region | |||
| Radiation exposure | 2.089 (0.466–3.711) | 0.012 | |
| Age | –0.307 (–0.528 to –0.086) | 0.007 | |
| Smoking | –0.004 (–0.010–0.003) | 0.277 | |
| Wearing glasses | 0.925 (–0.735–2.586) | 0.273 | |
CI = confidence interval.
The mean age ± standard deviation (SD) of age-matched exposed subjects and unexposed subjects were 39.5 ± 6.9 and 39.4 ± 6.9, respectively. In the age-matched comparison, there was a significant difference in LSIs in the PSR (Table 4).
Table 4.
Evaluation of light scattering intensity in the six layers between exposed and unexposed group by age-matched comparison (8-bit grayscale value)
| Layer of lens | IRs | Controls | Pvalue |
|---|---|---|---|
| (n= 54) | (n= 108) | ||
| Anterior capsule | 61.3 ± 7.3 | 59.4 ± 7.3 | 0.10 |
| Most transparent layer of the anterior superficial cortex | 41.1 ± 8.8 | 38.7 ± 7.6 | 0.07 |
| Anterior adult nucleus | 87.6 ± 26.9 | 82.2 ± 26.9 | 0.23 |
| Anterior fetal nucleus | 47.7 ± 10.3 | 47.2 ± 11.1 | 0.80 |
| Central clear zone | 35.6 ± 8.4 | 35.1 ± 8.6 | 0.75 |
| Posterior subcapsular region | 40.5 ± 13.4 | 34.5 ± 7.2 | 0.0031 |
Values are means ± SD.
DISCUSSION
Lens opacities were classified into three types according to their anatomical location: cortical region, nucleus and PSR. It has been demonstrated that high-dose ionizing radiation primarily associated with PSC can also induce cortical cataract formation [12, 13]. In the widely used grading system for radiation-induced cataracts by slit-lamp examination, the early stage of PSC shows a lens change consisting of the formation of small dots and vacuoles [14]. In a cross-sectional study in interventional cardiologists, PSCs were significantly more frequent among interventional cardiologists than the control subjects [15]. The increased LSIs in exposed subjects compared with unexposed subjects analyzed by multiple regression analysis and age-matched comparison suggest a potential adverse effect on the lens with low-dose radiation exposure. In spite of the minimal increased LSIs, the functional effect of these increased LSIs on visual acuity and undesirable risk is unclear. This phenomenon may be a predictor of a primary effect of low-dose radiation on the eye. Smoking is independently recognized to correlate with a higher risk of incident nuclear cataract development [16]. Our findings regarding smoking reinforce previous studies and suggest that the increase in LSIs in the central clear zone may be an early sign of nuclear cataracts.
In our study, the variable of age was significant for LSIs in all six layers of the eye lens. We performed multiple regression analyses including exposed subjects and unexposed subjects to adjusting the variables. Aging does not affect light scattering in the lens as a purely independent variable. Other factors such as ultraviolet light exposure, diabetes, renal failure, drug intake and malnutrition also individually and collectively contribute over time to further increase light scattering and cannot be readily separated from aging [10]. LSIs in the six layers of the lens increase in the anterior five layers and decrease in the PSR in a linear manner with aging [17]. This decrease in apparent LSIs in the PSR over time is likely related to age-related reduction in lens transparency. In the exposed subjects, however, there was an increase in the degree of LSIs at the PSR. Therefore radiation exposure shows a positive relation to LSIs in the PSR. In the most transparent layer of the anterior superficial cortex, LSIs did not show a significant difference between IRs and controls, and the parameter estimate of age was relative lower than for the other layers. This may be related to the fact that the age-related cortical cataract began on the outer edge of the lens cortex and slowly extended to the center [14].
Regarding IR dose, the average lens dose received by Japanese radiologists measured by thermoluminescent dosimeters (TLDs) during hepatocellular carcinoma embolization has been calculated at an average dose per procedure of approximately 0.04 mSv [16]. The average estimated cumulative dose in exposed subjects was 79.3 mSv (mean number of interventional procedure = 1982.3). The estimated annual dose was 5.1 mSv (mean annual number of interventional procedure = 127.1). A multi-center study with continuous 2-month dose readings demonstrated extrapolated annual radiation doses at the collar badge of 48 mSv in the mean annual number of interventional procedure of 972 [19]. The estimated average lens dose in interventional cardiologists with estimated cumulative occupational dose considering eye protection was 6.0 ± 6.6 Sv (0.1–27 Sv) and 3.7 ± 7.5 Gy (0.02–43 Gy) [7, 8]. It is estimated that the lens dose of exposed subjects in our study is lower than that of previous reports. In our screening examination, the detection rate of the PSC in the exposed subjects is 1.9%, considerably lower than the 38% and 52% reported in interventional cardiologists [7, 8]. This lower incidence of PSC may also be a collateral finding of lower radiation exposure.
Lens dosimetry was not performed in this retrospective study since two categories of information were unavailable; first, collar-badge readings were not uniformly available for all practitioners and second, existing under-apron individual monitoring data were unreliable due to inconstant usage of personal dosimeter, employment changes and also the fact that full versus part-time employment was not noted, neither was individual positioning and wearing of protection devices. Due to the aforementioned challenges, we chose not to include estimated lens dose, which cannot be considered in such circumstances as objectively quantifiable, and we therefore chose to simply register presence or absence of radiation exposure status (yes or no) as the categorical variable. Individual dosimetry remains problematic, and alternative strategies will be needed [20] in order to more precisely evaluate the effects of radiation in specific occupational situations, since strict individual monitoring and strategic management will be necessary.
One of the largest study limitations is our choice of a single left-eye examination for the purposes of this study; the laterality of LSIs of the lens could not be assessed. In the ORAMED (Optimization of RAdiation protection for MEDical staff) project, the dosimeter on the near side eye to the X-ray tube showed a higher dose than the dosimeter in the region between the eyes [21]. And, in the study of dose distribution with ten TLDs on the eyebrow ridge, the dose on the side nearest to the X-ray tube was three to five times greater than those on the farthest side [11]. It was recommended that dosimeters for the monitoring of eye dosage should be positioned on the side of the brow ridge adjacent to the X-ray tube [22]. Because the majority of exposed subjects were primarily abdominal oncologic vascular interventionalists and the physician's left eye was commonly closer to the X-ray tube, we believed that the left-sided eye examination in this study was more likely to evaluate the side with the highest exposure. Further study is required that includes lens dosimetry and evaluation of LSIs on each side.
Our study limitations include our group choices for exposed subjects and unexposed subjects; a more comparable control group may have been physicians without radiation exposure. Similarly, we had numerous exclusion criteria that were only answered and served as exclusions following initial screening ophthalmologic examination. We felt that rigid adherence to the exclusionary criteria was necessary for the purposes of data integrity, although it resulted in a large number of exclusions reducing the sample size. The questionnaire was also imperfect; unfortunately questions regarding any medical history of ionizing radiation exposure to the head and neck, such as head computed tomography, were not included.
Our single meridian cross-sectional analyses by EAS-1000 were performed in the mid-sagittal plane of the eye lens, therefore, there were no data obtained for off-center, off-angle and off-axis portions of the lens. As has been previously reported with the EAS-1000, the correlation coefficient in scatter light intensity measurement as measured over a 2-week interval may be greater than or equal to r= 0.9, additionally interoperator measurement error has previously been measured to range from 8 to 10% [23]. In order to confirm the reproducibility of the EAS-1000, mean individual coefficient of variation was segmentally measured in four different lens regions with a 1-week interval in measurements, and the variation was measured as between 3.6 and 5.1%, in keeping with the previously described examination [24]. As previously alluded to, a potential limitation of our study is also that the technologist was unblinded, although the automated nature of the LSI measurements for data collection, and the reliable proscriptive nature of mid-sagittal plane selection, suggests this is an unlikely cause for concern.
In conclusion, we found that there were minimal increased LSIs in the PSR of the lens in exposed subjects as compared with the unexposed subjects in this pilot study. Such findings will need to be longitudinally followed to establish their predictive value as far as cataractogenesis is concerned. Further quantitative studies concerning minimal radiation-related lens changes may additionally be required especially in low-dose exposure groups.
ACKNOWLEDGEMENTS
The authors acknowledge the Japanese Society of Interventional Radiology (JSIR) for partial funding of this study.
REFERENCES
- 1.Ainsbury EA, Bouffler SD, Dörr W, et al. Radiation cataractogenesis: a review of recent studies. Radiat Res. 2009;72:1–9. doi: 10.1667/RR1688.1. [DOI] [PubMed] [Google Scholar]
- 2. ICRP ref 488-6029-7736. Early and late effect of radiation in normal tissue and organs: threshold dose for tissue reaction and other non-cancer effects of radiation in a radiation protection context. Draft Report for Consultation in 2011. Ottawa, Canada, http://www.icrp.org/docs/Tissue%20Reactions%20Report%20Draft%20for%20Consultation.pdf. (29 July 2012, date last accessed) [Google Scholar]
- 3. ICRP ref 4825-3093-1164. Statement on tissue reactions in 2011. Ottawa, Canada, http://www.icrp.org/docs/ICRP%20Statement%20on%20Tissue%20Reactions.pdf. (29 July 2012, date last accessed) [Google Scholar]
- 4.Chylack LT, Jr, Peterson LE, Feiveson AH, et al. NASA study of cataract in astronauts (NASCA). Report 1: cross-sectional study of the relationship of exposure to space radiation and risk of lens opacity. Radiat Res. 2009;172:1–20. doi: 10.1667/RR1580.1. [DOI] [PubMed] [Google Scholar]
- 5.Merriam GR, Focht EF. A clinical and experimental study of the effect of single and divided doses of radiation on cataract production. Trans Am Ophthalmol Soc. 1962;60:35–52. [PMC free article] [PubMed] [Google Scholar]
- 6.Worgul BV, Kundiyev YI, Sergiyenko NM, et al. Cataract among Chernobyl clean-up workers: implications regarding permissible eye exposures. Radiat Res. 2007;167:233–43. doi: 10.1667/rr0298.1. [DOI] [PubMed] [Google Scholar]
- 7.Ciraj-Bjelac O, Rehani MM, Sim KH, et al. Risk for radiation induced cataract for staff in interventional cardiology: is there reason for concern? Catheter Cardiovasc Interv. 2010;76:826–34. doi: 10.1002/ccd.22670. [DOI] [PubMed] [Google Scholar]
- 8.Vano E, Kleiman NJ, Duran A, et al. Radiation cataract risk in interventional cardiology personnel. Radiat Res. 2010;174:490–5. doi: 10.1667/RR2207.1. [DOI] [PubMed] [Google Scholar]
- 9.Wegener A, Laser-Junga H. Photography of the anterior eye segment according to Scheimpflug's principle: options and limitations – a review. Clin Experiment Ophthalmol. 2009;37:144–54. doi: 10.1111/j.1442-9071.2009.02018.x. [DOI] [PubMed] [Google Scholar]
- 10.Sasaki K, Sasaki H, Jonasson F, et al. Racial differences of lens transparency property with aging and prevalence of age related cataract applying a WHO classification system. Ophthalmic Res. 2004;36:332–40. doi: 10.1159/000081636. [DOI] [PubMed] [Google Scholar]
- 11.Domienidd J, Vrodecki M, Rusicka D. A study of the dose distribution in the region of the eye lens and extremities for staff working in interventional cardiology. Radiat Meas. 2012;47:130–8. [Google Scholar]
- 12.Vano E, Gonzalez L, Beneytez F, et al. Lens injuries induced by occupational exposure in non-optimized interventional radiology laboratories. Br J Radiol. 1998;71:728–33. doi: 10.1259/bjr.71.847.9771383. [DOI] [PubMed] [Google Scholar]
- 13.Yamada M, Wong FL, Fujiwara S, et al. Noncancer disease incidence in atomic bomb survivors, 1958–1998. Radiat Res. 2004;161:622–32. doi: 10.1667/rr3183. [DOI] [PubMed] [Google Scholar]
- 14.Chylack LT, Jr., Wolfe JK, Singer DM, et al. The lens opacities classification system III. Arch Ophthalmol. 1993;111:831–6. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- 15.Jacob S, Boveda S, Bar O, et al. Interventional cardiologists and risk of radiation-induced cataract: results of a French multicenter observation study. Int J Cardiol. doi: 10.1016/j.ijcard.2012.04.124. 10.1016/j.ijcard.2012.04.124. [DOI] [PubMed] [Google Scholar]
- 16.Ye J, He J, Wang C, et al. Smoking and risk of age-related cataract: a meta-analysis. Invest Ophthalmol Vis Sci. 2012;57:3885–95. doi: 10.1167/iovs.12-9820. [DOI] [PubMed] [Google Scholar]
- 17.Sasaki H, Hockwin O, Kasuga T, et al. An index for human lens transparency related to age and lens layer: comparison between normal volunteers and diabetic patients with still clear lenses. Ophthalmic Res. 1999;31:93–103. doi: 10.1159/000055519. [DOI] [PubMed] [Google Scholar]
- 18.Ishiguchi T, Nakamura H, Okazaki M, et al. Radiation exposure to patient and radiologist during transcatheter arterial embolization for hepatocellular carcinoma. Nippon Igaku Hoshasen Gakkai Zasshi. 2000;60:839–44. (in Japanese) [PubMed] [Google Scholar]
- 19.Niklason LT, Marx MV, Chan HP. Interventional radiologists: occupational radiation doses and risks. Radiology. 1993;187:729–33. doi: 10.1148/radiology.187.3.8497622. [DOI] [PubMed] [Google Scholar]
- 20.Padovani R, Heron J Le, Curz-Suarez R, et al. International project on individual monitoring and radiation exposure levels in interventional cardiology. Radiat Prot Dosim. 2010;144:437–41. doi: 10.1093/rpd/ncq326. [DOI] [PubMed] [Google Scholar]
- 21.Domienik J, Brodecki E, Carinou E, et al. Extremity and eye lens doses in interventional radiology and cardiology procedures: first results of the ORAMED project. Radiat Prot Dosim. 2011;144:442–7. doi: 10.1093/rpd/ncq508. [DOI] [PubMed] [Google Scholar]
- 22.Martin CJ. Personal dosimetry for interventional operators: when and how should monitoring be done? Br J Radiol. 2011;84:639–48. doi: 10.1259/bjr/24828606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakamoto Y, Sasaki K, Nakamura Y, et al. Reproducibility of data obtained by a newly developed anterior eye segment analysis system, EAS-1000. Ophthalmic Res. 1992;24(suppl 1):10–20. doi: 10.1159/000267202. [DOI] [PubMed] [Google Scholar]
- 24.Wegener A, Hockwin O, Laser H, et al. Comparison of the Nidek EAS 1000 system and the Topcon SL-45 in clinical application. Ophthalmic Res. 1992;24(suppl. 1):55–62. doi: 10.1159/000267209. [DOI] [PubMed] [Google Scholar]