Abstract
The purpose of this study was to assess the efficacy and toxicity of definitive radiotherapy (RT) for the recurrence of epithelial ovarian cancer, which is limited to one or two gross regions, after complete remission had been achieved with aggressive front-line therapy. Twenty-seven patients were treated with definitive RT and were retrospectively analyzed. Their median tumor size was 3.0 cm. Twenty-six (96%) patients received external irradiation at a median total dose of 60 Gy, and a median daily dose of 2 Gy. Only two patients received intracavitary brachytherapy. Twenty (74%) of the 27 patients received systemic chemotherapy for the treatment of a limited recurrent tumor followed by definitive RT. Six (22%) of the patients received concurrent chemotherapy and seven (26%) of the patients also underwent regional hyperthermia during definitive RT. Twenty-two (82%) patients had an objective response (CR: 11, PR: 11). The 2-year overall survival, progression-free survival and local (in-field) control rates after RT were 53%, 39% and 96%, respectively. The toxicities were mild, no Grade 3 or higher toxicity was observed in any of the patients. The tumor size( < 3 cm), period between front-line therapy and RT (≥2 year) and objective tumor response (CR) were significant prognostic factors of the overall survival rate. In conclusion, definitive RT for limited recurrence of epithelial ovarian cancer achieves a better local control rate without severe toxicity, and it may therefore be a potentially effective modality for inducing long-term survival in selected patients.
Keywords: epithelial ovarian cancer, recurrence, radiotherapy, complete remission
INTRODUCTION
The standard therapy for patients with a primary epithelial ovarian cancer is cytoreductive surgery followed by chemotherapy. Despite significant advances in primary treatment, 60% of patients with an advanced stage epithelial ovarian cancer ultimately suffer disease recurrence [1]. As most cases of recurrent ovarian cancer are multifocal and the prognoses of such patients are rarely curative, the standard management for these patients with recurrent disease has been chemotherapy. In general, second-line chemotherapy in patients with recurrent ovarian cancer will lead to response rates of 50–60%, 20–30% and 10% in platinum-sensitive, platinum-resistant and platinum-refractory patients, respectively [2,3]. In the 1980s and 1990s, the use of salvage whole abdominopelvic radiation therapy (RT) after cis-platinum failure was investigated [4–6]. However, the consensus of these studies was that salvage whole abdominopelvic RT was minimally effective and too toxic in this situation.
The role of secondary cytoreductive surgery for recurrent epithelial ovarian cancer remains controversial. Recent data have indicated that complete cytoreduction, with appropriate surgical selection criteria (prolonged disease-free interval > 6 months, largest dimension of the recurrent tumor ≤ 10 cm, high performance status, and no symptoms due to recurrence), for recurrent ovarian cancer is associated with a significant prolongation of survival [7]. Thus, in a subset of patients, secondary cytoreductive surgery might significantly improve survival [2]. On the other hand, modern three-dimensional conformal RT planning techniques allow the administration of a conformal dose distribution around the tumor, potentially minimizing the dose of radiation administered to adjacent critical structures, and permitting escalated dose delivery to the tumor. Recently, several studies have shown that curative-intent RT using modern techniques in patients with limited recurrent or oligometastatic disease, including breast cancer, colorectal cancer, lung cancer and pancreatic cancer, resulted in good local tumor control without severe toxicity [8–11].
In this context, we hypothesized that definitive RT for the recurrence of epithelial ovarian cancer limited to one or two regions, after complete remission had been achieved with aggressive front-line therapy, may improve survival. However, there have been only a few reports of definitive RT for tumor control of recurrent ovarian cancer [12–14]. The purpose of this study was to assess the efficacy and toxicity of definitive RT for the limited recurrence of epithelial ovarian cancer after complete remission had been achieved with aggressive front-line therapy, and to identify the predictors of long-term survival.
MATERIALS AND METHODS
Patients
From September 1983 to January 2010, 48 patients with ovarian cancer were treated with RT in the Division of Therapeutic Radiology at our University Hospital. There were consecutive 27 patients (56%) with one or two gross recurrent lesions who were treated with definitive RT and were retrospectively analyzed. All 27 patients satisfied the following requirements and were included in this retrospective study: patients had a pathologically confirmed epithelial ovarian carcinoma, had achieved a complete remission after aggressive front-line therapy, and had one or two gross recurrent lesions at the start of the RT. Written informed consent for treatment was obtained from all patients. Patients treated with secondary cytoreductive surgery were not included in this study. The study was approved by the Institutional Review Board of the University of Occupational and Environmental Health.
The characteristics and treatments of the patients are listed in Tables 1and 2. For aggressive front-line therapy, Total Abdominal Hysterectomy (TAH), Bilateral Salpingo-Oophorectomy (BSO) and omentectomy were performed in 10 patients; TAH, BSO, omentectomy and appendectomy in seven; TAH, left salpingo-oophorectomy (LSO), omentectomy, and appendectomy in four; supracervical hystectomy, BSO and omentectomy in three; BSO in one; right salpingo-oophorectomy and omentectomy in one; and LSO in one patient.
Table 1.
Patient characteristics
| Variable | n(%) |
|---|---|
| Age | |
| Median (range) | 52 (32–79) |
| Performance statusa | |
| 0 | 4 (15) |
| 1 | 18 (66) |
| 2 | 5 (19) |
| Histological type | |
| Serous adenocarcinoma | 16 (59) |
| Non-classified adenocarcinoma | 6 (22) |
| Clear cell carcinoma | 5 (19) |
| Postoperative stage | |
| I | 3 (11) |
| II | 4 (15) |
| III | 18 (66) |
| IV | 2 (7) |
| Site(s) of the limited recurrence | |
| One site | 19 (70) |
| Paraaortic LN | 8 (36) |
| Douglas' pouch | 5 (19) |
| Vagina | 4 (15) |
| Iliac LN | 2 (7) |
| Two sites | 8 (30) |
| Iliac and paraaortic LN | 4 (15) |
| Douglas' pouch and inguinal LN | 1 (4) |
| Douglas' pouch + paraaortic LN | 1 (4) |
| Vagina + liver | 1 (4) |
| Douglas' pouch and spleen | 1 (4) |
| Recurrent tumor size (cm) | |
| Median (range) | 3.0 (1.0–6.1) |
LN = lymph node.
aat the start of the radiotherapy.
Table 2.
Treatment methods
| Variable | n(%) |
|---|---|
| Radiotherapy | |
| External irradiation alone | 25 (93) |
| Median total dose (Gy, range) | 60.0, 50.0–61.2 |
| Median daily dose (Gy, range) | 2.0, 1.8–2.0 |
| External irradiation plus brachytherapy | 1 (4) |
| Brachytherapy alone | 1 (4) |
| Chemotherapy for the recurrent tumor before RT | 20 (74) |
| Number of the regimens for the recurrent tumor before RT | |
| 1 | 15 |
| 2 | 2 |
| 3 | 3 |
| Response to chemotherapy immediately before RT | |
| CR | 0 |
| PR | 5 |
| NC | 9 |
| PD | 6 |
| Concurrent chemotherapy during RT | 6 (22) |
| Adjuvant chemotherapy after RT | 3 (11) |
| Hyperthermia during RT | 7 (26) |
RT = radiotherapy; CR = complete response; PR = partial response; NC = no change.
The tumor/node/metastasis (TNM) stages (International Union Against Cancer TNM classification, 6th edition) were pathologically evaluated at the initial surgery: T1bN0M0 in one patient, T1cN0M0 in two patients, T2cN0M0 in four, T3bN0M0 in three, T3cN0M0 in 13, T3cN1M0 in two, T3cN0M1 in one patient and T3cN1M1 in one. The time between front-line surgery and RT for the limited recurrence ranged from 6–58 months (median 22 months). The period between completion of adjuvant chemotherapy and recurrence ranged from 1–46 months (median 8 months). The median recurrent tumor size was 3.0 cm (range 1.0–6.1 cm). The Eastern Cooperative Oncology Group performance status was evaluated at the start of the RT. All patients were diagnosed as having recurrent disease based on longitudinal computed tomography (CT) scans and tumor marker levels, and, in some cases, 18F-fluorodeoxyglucose positron emission tomography/CT and/or magnetic resonance imaging were also used.
After initial surgery, all patients received adjuvant chemotherapy as follows: paclitaxel in combination with carboplatin in 15 patients, and a combination of cyclophosphamide, adriamycin and cisplatin in 12 patients. Twenty (74%) of the 27 patients received systemic chemotherapy for the limited recurrent tumor followed by definitive RT as follows: paclitaxel in combination with carboplatinin in 10 patients, docetaxel in combination with carboplatin in six, irinotecan in combination with mitomycin C in three, cyclophophamide and adriamycin in combination with cisplatin in two, cyclophosphamide in combination with adriamycin in one, etoposide in combination with cisplatin in one, etoposide in combination with carboplatin in one, irinotecan in combination with cisplatin in one, irinotecan in combination with carboplatin in one, cisplatin in one and Tegafur-uracil in one patient.
Although no specific chemotherapy protocol existed, six (22%) of the 27 patients were treated with concomitant systemic chemotherapy during the course of RT as follows: paclitaxel in combination with carboplatin in three patients, carboplatin in two and cisplatin in one. Three (11%) patients received adjuvant chemotherapy using paclitaxel in combination with carboplatin after RT. Seven (26%) of the 27 patients were also treated with whole abdominal (n= 2) or pelvic (n= 5) regional hyperthermia during RT. Hyperthermia was applied after irradiation once a week for radio-sensitization. An 8-MHz radiofrequency (RF)-capacitive regional hyperthermia system (Thermotron RF-8; Yamamoto Vinita, Osaka, Japan) was used. Using this system, the patient is placed between two electrodes connected to a high power RF generator [15–16]. The electrodes are then covered by a circulating water bolus to cool the skin. The heating duration was adjusted from 40–60 min based on the patient's tolerance (median 50 min). The number of hyperthermia treatments during the RT ranged from 2 to 11 (median 5). The RF-output power was increased to the maximum level tolerated by the patients, and was maintained with the goal of 42°C based on the correlative data between the RF-output power and the deep regional temperature [17].
Radiotherapy
Twenty-five (93%) of the 27 patients were treated with external RT, one patient with external RT plus brachytherapy and the remaining patient with brachytherapy alone (Table 2). The total radiation dose of external RT, using a 4-, 6- or 10-MV linear accelerator, ranged from 50.0–61.2 Gy (median 60.0 Gy), and the daily dose was 1.8–2.0 Gy (median 2.0 Gy). CT-assisted three-dimensional treatment planning (Xio or FOCUS; CMS Japan, Tokyo, Japan) was used to determine the radiation fields in 23 (85%) of the 27 patients between October 1995 and January 2010. Prophylactic nodal irradiation for paraaortic lymph node (LN) lesions was administered in all 14 patients with paraaortic LN metastases; the clinical target volume (CTV) was defined as the gross tumor volume (GTV) and the paraaortic LN area (the upper margin of the field was at the Th11–Th12 inter-vertebral space, and the lower margin was at the L5–S1 inter-vertebral space) plus a 0.5-cm margin. Prophylactic irradiation for the whole pelvic region was also performed in five (26%) of 19 patients with limited recurrence in the pelvic lesion. The planning target volume (PTV) included the CTV plus a 1.0–2.0-cm margin for daily set-up variation. Normally, the initial field area covered the PTV with a four-field box technique, and the field was then shrunk to the GTV (limited recurrent tumor) with 0.5–1.5 cm margins at a dose of 40–50 Gy for the boost doses of 10–20 Gy using a four-field beam arrangement or conformational therapy. The remaining patients were treated without the prophylactic irradiation and with RT using a four-field box technique or conformational therapy; the CTV was defined as the gross tumor volume plus 0.5 cm, and the PTV was the CTV plus 0.5–1.5 cm for the daily setup variation and respiratory movement. Two patients with recurrence in the vagina underwent brachytherapy delivered to the limited recurrent tumor of the vagina at a high dose rate (60Co) using a vaginal cylinder, which was prescribed to 1 cm below the mucosa at a dose of 30 Gy in six fractions or 9 Gy in three fractions immediately after external RT doses of 50.4 Gy in 28 fractions.
The biologically effective dose (BED) can be used to compare the efficacy of various dose-fractionation regimens in providing tumor control [10,11]. The BED (total dose) × (1 + daily dose/[a/b]) using a linear quadratic model with a/b ratios of [10] ranged from 45.0 to 87.2 Gy10(median 72.0Gy10).
Evaluation and follow-up
The objective tumor response was evaluated by measuring the tumor size by CT before and after RT, and follow-up evaluations were performed by CT every 1–6 months. The treatment response was evaluated according to the World Health Organization criteria [18]. A complete response (CR) was defined as the complete disappearance of all clinically detectable tumors for at least 4 weeks. A partial response (PR) required at least a 50% reduction in the sum of the products of the longest perpendicular diameters of all measurable lesions. Progressive disease required either a 25% increase in measurable lesions or the appearance of any new measurable or non-measurable lesions. Patients who did not meet the definitions of response or progression were classified as having no change.
The overall, progression-free and local control (defined as failure to have a recurrence within the radiation field) survival rates were calculated from the start of RT using the Kaplan–Meier method. The statistical significance of the difference between the actuarial curves was assessed using the log-rank test. To identify prognostic factors for overall survival, disease progression-free survival and the local control rates, univariate analyses were performed using the performance status, tumor size, number of recurrent lesions, period between front-line therapy and RT, total radiation dose (BED), objective tumor response, concurrent chemotherapy, hyperthermia and response to chemotherapy immediately before RT. Multivariate analyses using the Cox proportional-hazards model were performed to determine the overall and progression-free survival rates related to such factors as the tumor size, period between front-line therapy and RT and the objective tumor response.
The National Cancer Institute Common Toxicity Criteria version 3 (CTCAE) was used to score the patient toxicity. The highest toxicity grade for each patient was used for the toxicity analysis. The toxicity was defined as acute (during therapy and up to 3 months after the combination therapy) or late (over 3 months after the completion of the combination therapy).
RESULTS
Both the observed hematologic and non-hematologic toxicities were mild. Acute toxicities ≥Grade 2 occurred in six patients (22%); Grade 3 leucopenia/neutropenia in one, Grade 2 anemia in two, Grade 2 thrombocytopenia in one, Grade 2 gastritis in one and Grade 2 diarrhea in one. No late toxicity ≥Grade 2 was observed.
The median follow-up for the surviving patients was 25 months (range 3 to 95 months). All patients completed the planned radiation treatments. Twenty-two (82%) of the 27 patients experienced an objective response (CR in 11 patients, PR in 11, NC in five). The first sites of disease progression were local (in-field) in two patients (7%) (paraaortic LN in one patient and peritoneum in one), out-field in 13 patients (peritoneum in six patients, paraaortic LN in four, liver in three, supraclavicular LN in two, lung in two, spleen in one and soft tissue in one), and both in-field (paraaortic LN) and out-field (liver and pleura) in one patient (4%).
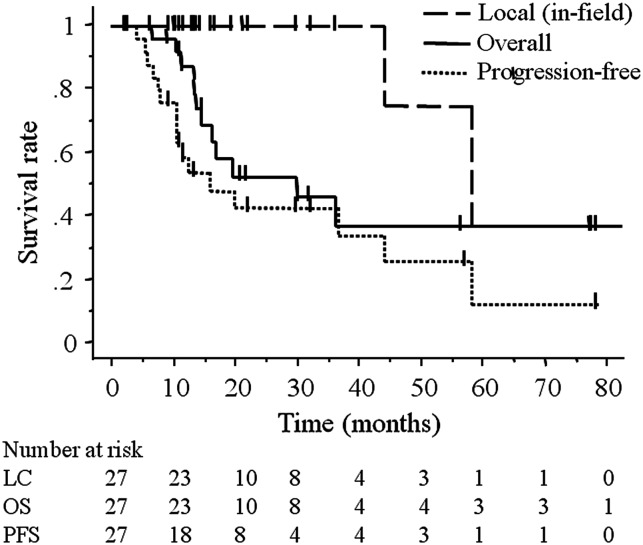
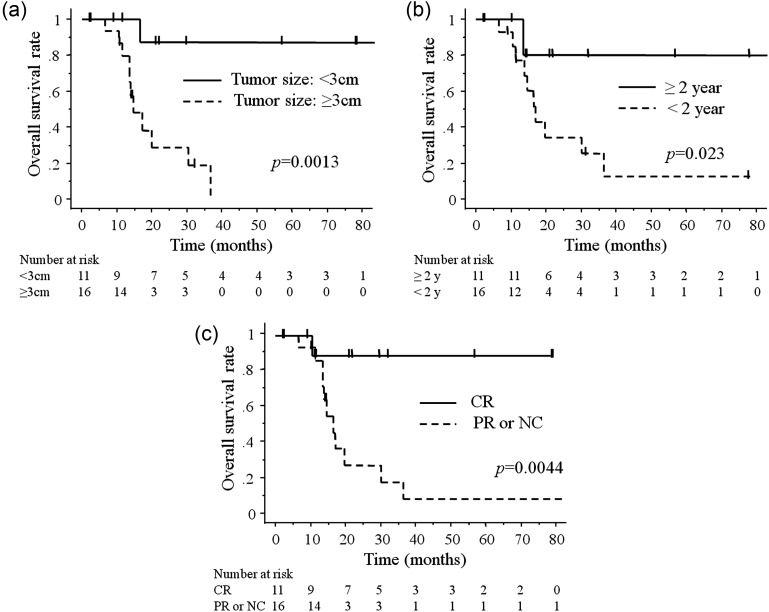
The 3-year overall survival, progression-free survival and local (in-field) control rates after RT were 46%, 39% and 96%, respectively (Fig. 1). The 2-year overall survival, progression-free survival and local (in-field) control rates after RT were 53%, 39% and 96%, respectively. The median survival times (MST) with regard to the overall and progression-free survival rates after RT were 25 and 12 months, respectively. Univariate analyses showed the tumor size( < 3 cm), period between front-line therapy and RT (≥2 year), objective tumor response (CR) and response to chemotherapy immediately before RT (PR) to be significant prognostic factors of the overall survival rate (Table 3, Fig. 2). The tumor size( < 3 cm) and objective tumor response (CR) were also significant prognostic factors for the rates of disease-free survival. Regarding the overall and progression-free survival rates based on the multivariate analyses, none of these factors (tumor size < 3 cm, period between front-line therapy and RT ≥ 2 years or objective tumor response (CR)) were significant.
Fig. 1.
Overall survival (OS), progression-free survival (PFS) and local (in-field) control rates (LC) after RT of all patients.
Table 3.
The results of the univariate analyses of factors predicting the survival rates
| Variable | Pt. (n) | Overall survival rate |
Progression-free survival rate |
Local (in-field) control rate |
|||
|---|---|---|---|---|---|---|---|
| 2-year (%) | P | 2-year (%) | P | 2-year (%) | P | ||
| Performance status | |||||||
| 0–1 | 22 | 46 | 0.17 | 38 | 0.83 | 95 | 0.27 |
| 2 | 5 | 80 | 40 | 100 | |||
| Tumor size | |||||||
| <3 cm | 11 | 88 | 0.0013 | 64 | 0.016 | 100 | 0.41 |
| ≥3 cm | 16 | 29 | 22 | 93 | |||
| Irradiated lesion | |||||||
| One lesion | 19 | 52 | 0.28 | 38 | 0.79 | 100 | 0.11 |
| Two lesions | 8 | 54 | 43 | 86 | |||
| Period between start of first-line treatment and RT | |||||||
| <2 years | 16 | 35 | 0.023 | 19 | 0.088 | 93 | 0.40 |
| ≥2 years | 11 | 80 | 64 | 100 | |||
| Total dose of radiation (BED, Gy10) | |||||||
| <72 | 13 | 49 | 0.72 | 51 | 0.11 | 92 | 0.68 |
| ≥72 | 14 | 57 | 26 | 100 | |||
| Concurrent chemotherapy | |||||||
| Yes | 6 | 0 | 0.31 | NR | 0.23 | 100 | NR |
| No | 21 | 57 | 42 | 95 | |||
| Hyperthermia | |||||||
| Yes | 7 | 0 | 0.89 | NR | 0.73 | 100 | NR |
| No | 20 | 56 | 42 | 95 | |||
| Objective tumor response | |||||||
| CR | 11 | 89 | 0.0044 | 67 | 0.013 | 100 | 0.079 |
| PR or NC | 16 | 28 | 21 | 93 | |||
| Response to chemotherapy immediately before RT | |||||||
| PR | 5 | 100 | 0.019 | 80 | 0.069 | 100 | NR |
| NC or PD | 15 | 47 | 34 | 100 | |||
BED = biologically effective dose; NR = not reached; CR = complete response; PR = partial response; NC = no change.
Fig. 2.
(a) Tumor size ( < 3 cm) was a significant predictor for overall survival rate after RT (P= 0.0013). (b) Period between front-line therapy and RT (≥2 years) was a statistically significant prognostic indicator for overall survival rate after RT (P= 0.023). (c) Objective tumor response (CR) was a significant predictor for overall survival rate after RT (P= 0.0044).
DISCUSSION
The essential treatment for recurrent ovarian cancer is chemotherapy, and in selected patients, secondary cytoreductive surgery can improve survival [1–3]. A number of studies have demonstrated that the most important factors for predicting the outcome for recurrent ovarian cancer are the initial response of the tumor recurrence and the length of the disease-free interval prior to tumor recurrence [2,3]. The role of RT for recurrent ovarian cancer has been considered as a palliative therapy for symptom relief, and whole abdominal radiation therapy has not been recommended due to its severe toxicity [19]. Many studies have reported that local external beam irradiation could resolve various symptoms caused by metastatic or recurrent tumors and may be useful for palliative treatment [20–22]. However, in the present study, we delivered RT with curative intent. Our selection of patients for RT is unique in this respect.
There have been only a few previous studies of RT with the aim of achieving a cure or prolongation of survival in patients with limited recurrence of epithelial ovarian cancer [12–14]. Albuquerque et al.reported treatment results using tumor volume-directed involved field RT (median dose 50.4 Gy) for localized extraperitoneal recurrence; of 20 patients, 17 had a CR after RT with acceptable toxicity, and the local recurrence-free and disease-free survival rates at 5 years from the date of RT were 66% and 34%, respectively [12]. Firat et al.reported the role of salvage irradiation in 28 patients with vaginal and/or perirectal recurrence or persistence of ovarian carcinoma; 21 patients were treated with external beam RT alone (median dose 50.4 Gy), two patients with brachytherapy alone and five patients with both external beam RT and brachytherapy. They indicated that pelvic local irradiation may be effective for salvage, and that a cure is possible in a subset of patients [13]. The median external RT dose of 60 Gy in the current study was relatively higher than that in the previous study. We also found that in the patients with limited recurrence in various sites, definitive RT was feasible, could achieve a better local control rate without severe toxicity, although two patients showed a local recurrence more than 3 years after RT, and many patients died within 2 years. The results justify further evaluation to clarify the optimal radiation dose and treatment fields for the treatment of limited recurrence.
Recently, a prospective study of curative-intent stereotactic RT in patients with five or fewer oligometastatic lesions of various sites demonstrated that aggressive local therapy for limited metastases can result in prolonged life [8]. The prospective study also implied that aggressive first-line therapy, including systemic chemotherapy, has the potential to downstage some patients to limited recurrence, such as oligometastatic disease, allowing for a prolonged life or cure with aggressive local therapy. Kim et al.reported the effects of hyperfractionated RT with concurrent chemotherapy for paraaortic LN recurrence in patients with cervical cancer of the uterus: patients with a latent period > 24 months until paraaortic LN recurrence had a more favorable survival rate than those with a latent period ≤ 24 months [23]. Traditionally, ovarian cancer is considered to be a disease with a high incidence of widespread metastases [12]. However, we have shown in the current study that patients with limited recurrence, who achieved a complete remission after aggressive front-line therapy, could be successfully salvaged, and further evaluation of the benefits of the definitive RT in the progression-free survivals would therefore be valuable, especially in patients with a smaller recurrent tumor or a longer period between the initial treatment and RT.
Previous studies have demonstrated the role of secondary cytoreductive surgery for recurrent epithelial ovarian cancer to be limited in selected patients. Numerous studies have shown that the median survival time after recurrence ranged from 38 to 61 months in patients who are left with no or minimal residual disease at the time of secondary cytoreductive surgery, and that the survival time is 5 to 27 months in patients who undergo suboptimal cytoreduction [2]. However, secondary cytoreductive surgery can be associated with significant morbidity and occasional mortality; in a meta-analysis, the rate of major perioperative complications and mortality were 11% and 1.4%, respectively [2]. In the current study for definitive local RT using mainly computed assisted three-dimensional RT in patients with limited recurrence after complete remission, a 3-year local control rate of 96% without severe toxicity is promising. In addition, the period between the front-line therapy and RT, tumor size ( < 3 cm) and objective tumor response (CR) were significant prognostic factors for the overall survival rate, and these factors were comparable with those for secondary cytoreductive surgery. Definitive RT may be a promising alternative to surgery in recurrent ovarian cancer patients with the above selection criteria. In addition, our retrospective results justify further evaluations of the role of definitive RT in a larger number of patients with recurrent epithelial ovarian cancer.
Due to the fact that the current study was a small retrospective case series with heterogeneous treatment, the possibility of some selection bias with regard to the prognostic factors could not be ruled out, although we did perform both univariate and multivariate analyses for the survival rates. A formal prospective trial is consequently needed to determine the efficacy and prognostic factors of this therapy in patients with recurrent epithelial ovarian cancer.
In summary, RT for curative intent in ovarian cancer patients with limited recurrence could achieve a better local control rate without severe toxicity, and is a promising treatment that may result in long-term survival in selected patients. At least, these results justify further evaluations with detailed treatment protocols to clarify whether definitive RT could improve survival in selected patients.
REFERENCES
- 1.Burke TW, Morris M. Secondary cytoreductive surgery for ovarian cancer. Obstet Gynecol Clin North Am. 1994;21:167–78. [PubMed] [Google Scholar]
- 2.Eltabbakh GH, Goodrich S. Update on the treatment of recurrent ovarian cancer. Womens Health (Lond Engl) 2006;2:127–39. doi: 10.2217/17455057.2.1.127. [DOI] [PubMed] [Google Scholar]
- 3.Markman M, Bookman MA. Second-line treatment of ovarian cancer. Oncologist. 2000;5:26–35. doi: 10.1634/theoncologist.5-1-26. [DOI] [PubMed] [Google Scholar]
- 4.Homesley HD, Scarantino CW, Muss HB, et al. Concurrent chemotherapy and single high-dose plus whole abdominopelvic radiation for persistent ovarian carcinoma. Gynecol Oncol. 1989;34:170–4. doi: 10.1016/0090-8258(89)90135-2. [DOI] [PubMed] [Google Scholar]
- 5.Schray MF, Martinez A, Howes AE, et al. Advanced epithelial ovarian cancer: toxicity of whole abdominal irradiation after operation, combination chemotherapy, and reoperation. Gynecol Oncol. 1986;24:68–80. doi: 10.1016/0090-8258(86)90009-0. [DOI] [PubMed] [Google Scholar]
- 6.Linstadt DE, Stern JL, Quivey JM, et al. Salvage whole-abdominal irradiation following chemotherapy failure in epithelial ovarian carcinoma. Gynecol Oncol. 1990;36:327–30. doi: 10.1016/0090-8258(90)90135-8. [DOI] [PubMed] [Google Scholar]
- 7.Eisenkop SM, Friedman RL, Spirtos NM. The role of secondary cytoreductive surgery in the treatment of patients with recurrent epithelial ovarian carcinoma. Cancer. 2000;88:144–53. doi: 10.1002/(sici)1097-0142(20000101)88:1<144::aid-cncr20>3.3.co;2-o. [DOI] [PubMed] [Google Scholar]
- 8.Milano MT, Katz AW, Muhs AG, et al. A prospective pilot study of curative-intent stereotactic body radiation therapy in patients with 5 or fewer oligometastatic lesions. Cancer. 2008;112:650–8. doi: 10.1002/cncr.23209. [DOI] [PubMed] [Google Scholar]
- 9.Yeo SG, Kim DY, Kim TH, et al. Curative chemoradiotherapy for isolated retroperitoneal lymph node recurrence of colorectal cancer. Radiother Oncol. 2010;97:307–11. doi: 10.1016/j.radonc.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 10.Wilkowski R, Thoma M, Bruns C, et al. Combined chemoradiotherapy for isolated local recurrence after primary resection of pancreatic cancer. JOP. 2006;7:34–40. [PubMed] [Google Scholar]
- 11.Norihisa Y, Nagata Y, Takayama K, et al. Stereotactic body radiotherapy for oligometastatic lung tumors. Int J Radiat Oncol Biol Phys. 2008;72:398–403. doi: 10.1016/j.ijrobp.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Albuquerque KV, Singla R, Potkul RK, et al. Impact of tumor volume-directed involved field radiation therapy integrated in the management of recurrent ovarian cancer. Gynecol Oncol. 2005;96:701–4. doi: 10.1016/j.ygyno.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Firat S, Erickson B. Selective irradiation for the treatment of recurrent ovarian carcinoma involving the vagina or rectum. Gynecol Oncol. 2001;80:213–20. doi: 10.1006/gyno.2000.6059. [DOI] [PubMed] [Google Scholar]
- 14.Fujiwara K, Suzuki S, Yoden E, et al. Local radiation therapy for localized relapsed or refractory ovarian cancer patients with or without symptoms after chemotherapy. Int J Gynecol Cancer. 2002;12:250–6. doi: 10.1046/j.1525-1438.2002.01096.x. [DOI] [PubMed] [Google Scholar]
- 15.Song CW, Rhee JG, Lee CK, et al. Capacitive heating of phantom and human tumors with an 8 MHz radiofrequency applicator (Thermotron RF-8) Int J Radiat Oncol Biol Phys. 1986;12:365–72. doi: 10.1016/0360-3016(86)90352-4. [DOI] [PubMed] [Google Scholar]
- 16.Abe M, Hiraoka M, Takahashi M, et al. Multi-institutional studies on hyperthermia using an 8-MHz radiofrequency capacitive heating device (Thermotron RF-8) in combination with radiation for cancer therapy. Cancer. 1986;58:1589–95. doi: 10.1002/1097-0142(19861015)58:8<1589::aid-cncr2820580802>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 17.Imada H. Development of new heating technique. In: Matsuda T, Sugawara T, Abe M, Tanaka Y, editors. Hyperthermia No Rinsho. Tokyo: Iryokagaku; 1999. pp. 394–402. [Google Scholar]
- 18.Miller AB, Hoogstraten B, Staquet M, et al. Reporting results of cancer treatment. Cancer. 1981;47:207–14. doi: 10.1002/1097-0142(19810101)47:1<207::aid-cncr2820470134>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 19.Lanciano R, Reddy S, Corn B, et al. Update on the role of radiotherapy in ovarian cancer. Semin Oncol. 1998;25:361–71. [PubMed] [Google Scholar]
- 20.Tinger A, Waldron T, Peluso N, et al. Effective palliative radiation therapy in advanced and recurrent ovarian carcinoma. Int J Radiat Oncol Biol Phys. 2001;51:1256–63. doi: 10.1016/s0360-3016(01)01733-3. [DOI] [PubMed] [Google Scholar]
- 21.Corn BW, Lanciano RM, Boente M, et al. Recurrent ovarian cancer Effective radiotherapeutic palliation after chemotherapy failure. Cancer. 1994;74:2979–83. doi: 10.1002/1097-0142(19941201)74:11<2979::aid-cncr2820741114>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 22.Gelblum D, Mychalczak B, Almadrones L, et al. Palliative benefit of external-beam radiation in the management of platinum refractory epithelial ovarian carcinoma. Gynecol Oncol. 1998;69:36–41. doi: 10.1006/gyno.1998.4934. [DOI] [PubMed] [Google Scholar]
- 23.Kim JS, Kim SY, Kim KH, et al. Hyperfractionated radiotherapy with concurrent chemotherapy for para-aortic lymph node recurrence in carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2003;55:1247–53. doi: 10.1016/s0360-3016(02)04401-2. [DOI] [PubMed] [Google Scholar]