Abstract
Objective
To identify validated ICD-9-CM/ICD-10 coded case definitions for acute myocardial infarction (AMI).
Data Sources
Ovid Medline (1950–2010) was searched to identify studies that validated acute myocardial infarction (AMI) case definitions. Hospital discharge abstract data and chart data were linked to validate identified AMI definitions.
Study Design
Systematic literature review, chart review, and administrative data analysis.
Data Collection/Extraction Methods
Data on sensitivity/specificity/positive and negative predictive values (PPV and NPV) were extracted from previous studies to identify validated case definitions for AMI. These case definitions were validated in administrative data through chart review and applied to hospital discharge data to assess in-hospital mortality.
Principal Findings
Of the eight ICD-9-CM definitions validated in the literature, use of ICD-9-CM code 410 to define AMI had the highest sensitivity (94 percent) and specificity (99 percent). In our data, ICD-9-CM/ICD-10 codes 410/I21-I22 in all available coding fields had high sensitivity (83.3 percent/82.8 percent) and PPV (82.8 percent/82.2 percent). The in-hospital mortality among AMI patients identified using this case definition was 7.6 percent in ICD-9-CM data and 6.6 percent in ICD-10 data.
Conclusions
We recommend that ICD-9-CM 410 or ICD-10 I21-I22 in the primary diagnosis coding field should be used to define AMI. The use of a consistent validated case definition would improve comparability across studies
Keywords: Administrative data, acute myocardial infarction, validation studies, international classification of disease (ICD) codes, mortality
Acute myocardial infarction (AMI) is an important health issue that has been widely studied in the literature both in terms of its clinical impact on the population and its inclusion as part of performance indicators (Yeh and Go 2010). However, the essential question of what constitutes an AMI clinically remains unaddressed, resulting in heterogeneity between study findings (Thygesen et al. 2007; Yeh and Go 2010). The lack of a common clinical definition further complicates population-based studies that rely on administrative data that are coded from this heterogeneous pool of clinical definitions.
Administrative data such as hospital discharge abstract data, physician billing data, health insurance plan registries, and vital statistics repositories are employed for many different purposes in part due to their wide population-coverage, their cost-effectiveness, and the fact that they are often a readily available source of data. Administrative health databases typically code medical conditions using the World Health Organization International Classification of Diseases and Related Disorders (ICD) codes, and as such are very useful tool for research. Today, most countries use ICD-9 (first released in 1975), ICD-9-CM (Clinical Modification), or ICD-10 (first released in 1990) to classify their national morbidity and mortality data, making these coding systems the most widely used classification systems underlying health care data internationally (Jette et al. 2010; World Health Organization 2010).
Although administrative data are used to estimate the incidence and prevalence of acute conditions requiring hospital admission, administrative data were not originally intended to be collected for disease surveillance (Tu et al. 1999; Austin, Daly, and Tu 2002). As a result, it is important to assess disease coding validity from administrative databases for conditions such as AMI before proceeding with any outcome analysis or epidemiological studies. A case definition for a disease can simply consist of the appearance of a single disease code at any point in time in any administrative data source (i.e., if a patient has one physician visit for the condition of interest, he or she is classified as having the disease), or it can use an algorithm to identify patients with the disease (i.e., a patient is only classified as having the disease if he or she had two physician visits and one emergency room visit coded with the condition of interest within a 2-year period) (Quan et al. 2009). Numerous studies have been published using administrative hospitalization data to study various AMI outcomes; however, the case definitions used have often not been validated prior to their implementation and are inconsistent across studies, which may lead to incomparable findings.
The objectives of this study were to (1) perform a systematic review of hospital-based studies to identify validated ICD-9-, ICD-9-CM-, or ICD-10-based AMI case definitions; (2) identify what case definitions have been used in the literature; (3) validate previously validated case definitions in dually coded ICD-9-CM and ICD-10 data through medical chart review; and (4) apply validated AMI case definitions to Canadian hospital discharge abstract data to assess the impact of various case definitions on estimates of AMI admissions and in-hospital mortality.
METHODS
Literature Review of Validated AMI Case Definitions
A systematic literature search was conducted in July 2010 using Ovid Medline (1950 to present) for the following terms: myocardial infarction or cardiac infarct or heart infarct or myocardial infarct or acute myocardial infarction; AND case definition or admin data or administrative data or algorithms or computer algorithms or registries or International Classification of Diseases or ICD-9 or ICD-9CM or ICD-10 or ICD code or patient coding or patient classification or disease classification or disease coding or international classification disease. The search was limited to English language articles only. All abstracts were reviewed independently by two authors, and full-text articles were reviewed if one of the two reviewers thought the article may be relevant at the abstract review stage. Full-text articles were included if both reviewers agreed that the article met all eligibility criteria: validated AMI ICD-9 or ICD-10 codes (including any country-specific modification in these coding frameworks); specified the ICD codes used in hospital discharge abstract data; and reported sensitivity, specificity, positive predictive value (PPV), or negative predictive value (NPV) or provided the data required to calculate these values. Reference lists were also hand searched to ensure no additional studies were missed. Disagreements between reviewers were resolved by consensus.
Data on sensitivity, specificity, PPV, and NPV (when available) were abstracted by two reviewers from validated case definitions and summarized in tabular form. In addition, data were also abstracted on study characteristics (such as sample size, years of data collection, validation database, and gold standard) and the specific ICD codes used in the validation.
Literature Review of Case Definitions Used in AMI studies
Due to the high volume of publications on AMI, we searched high-impact general medical journals (i.e., British Medical Journal, Canadian Medical Association Journal, Journal of the American Medical Association, Lancet, New England Journal of Medicine) and high-impact cardiovascular journals (i.e., American Journal of Cardiology, Circulation, Heart, Journal of the American College of Cardiology) and determined what ICD-based case definitions for AMI were most commonly used in the scientific literature. A literature search of these journals using Ovid Medline (2007–2012) was conducted in February 2012 using the following terms: myocardial infarction or acute myocardial infarction; and medical records or health services or health services research or insurance, hospitalization, or length of stay or risk adjustment or hospitals or databases, factual. Journal articles were included if they used an ICD-9- or ICD-10-based case definition for AMI and reported the ICD codes used.
Validating AMI Case Definitions in Dually Coded ICD-9-CM and ICD-10 Hospital Discharge Data
We randomly selected 4,008 inpatients records from hospital discharge abstract data who were admitted between January 1 and June 30, 2003, for any indication. Up to 25 diagnoses per encounter were coded using ICD-10. Trained health coders recoded these inpatient charts using ICD-9-CM using standard coding methodology. Charts were then independently reviewed by trained reviewers with nursing backgrounds. Reviewers were instructed to examine the entire chart, including the cover page, admission notes, laboratory results, and discharge summaries. A chart was coded as indicating the presence of AMI based on all available documentation and if the AMI was not present on admission. Thus, for 4,008 inpatients, three datasets were created: ICD-9-CM, ICD-10, and chart review datasets. Details were reported elsewhere (Quan et al. 2008). Sensitivity, specificity, PPV, and NPV were calculated for ICD-9-CM and ICD-10 data (found in any coding position), respectively, accepting the chart data as a reference standard for each AMI case definition.
AMI Case Volume and In-Hospital Mortality in Hospital Discharge Data
AMI case definitions were applied to the hospital discharge abstract data from Calgary, Alberta, Canada, from April 2001 to March 2002 (ICD-9 coded data) and April 2006 to March 2007 (ICD-10 coded data). Hospitals in Calgary serve a population of 1.4 million individuals. These data encompass all patients who were admitted to hospital and include numerous variables such as length of stay, diagnoses, interventions, and in-hospital mortality. Up to 50 diagnoses per case are recorded in this database. AMI patients were defined using the primary diagnosis alone and then using primary and secondary diagnoses (i.e., conditions were coded in any coding field). Patients were included in this analysis if they were 18 years of age or older at the time of admission. For patients with multiple admissions, only the first admission in the fiscal year was used in the analysis. For each case definition, the number of patients identified and the in-hospital mortality rate was assessed among those identified.
Results
Literature Review of Validated AMI Case Definitions
Of 3,603 articles identified, 26 articles from nine countries, including Australia, Canada, Finland, Korea, the Netherlands, New Zealand, Scotland, Sweden, and United States, met all inclusion criteria (Figure 1). Nine ICD-9 and two ICD-10 codes were used in these studies in eight combinations (see Tables 1 and 2). All these studies included ICD-9 code 410 (AMI) in either the primary (major reason for admission or resource consumption) or one of the secondary diagnostic code positions (co-existing condition) to identify patients with AMI. The second most frequently used code was ICD-9 411 (other acute and subacute forms of ischemic heart disease). Only one study validated ICD-10 codes, I21 (acute myocardial infarction, disregarding any ICD-10 subgroups) and I22 (subsequent myocardial infarction, disregarding any ICD-10 subgroups), and combined these codes with ICD-9 code 410 (Pajunen et al. 2005). Most studies did not differentiate whether a particular code of interest was in the primary position or in one of the secondary positions. Of the 26 studies reviewed, 17 used medical records and 9 used registry data as the gold standard to validate AMI diagnosis in hospital discharge data. ICD-9 codes 410–414 had the highest reported sensitivity (range: 79–95 percent), whereas ICD-9 code 410 used in isolation had the highest reported specificity (range: 89–99 percent) (see Table 2).
Figure 1.
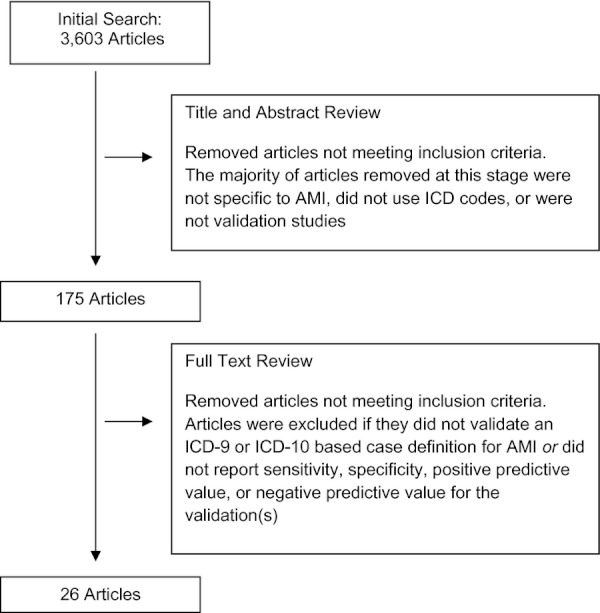
Flow Chart of Systematic Literature Review to Identify Studies That Validated Case Definitions for Acute Myocardial Infarction
Table 1.
International Classification of Disease (ICD) Codes Used as Part of Validated Acute Myocardial Infarction Case Definitions
| ICD-9-CM Code | Definition | ICD-10-CA Code | Definition |
|---|---|---|---|
| 410 | Acute myocardial infarction | I21 | Acute myocardial infarction |
| 410.x0 | Acute myocardial infarction: episode of care unspecified | I22 | Subsequent myocardial infarction |
| 410.x1 | Acute myocardial infarction: initial episode of care | – | – |
| 410.0 | Acute myocardial infarction of anterolateral wall | – | – |
| 410.1 | Acute myocardial infarction of other anterior wall | – | – |
| 410.2 | Acute myocardial infarction of inferolateral wall | – | – |
| 410.3 | Acute myocardial infarction of inferoposterior wall | – | – |
| 410.4 | Acute myocardial infarction of other inferior wall | – | – |
| 410.5 | Acute myocardial infarction of other lateral wall | – | – |
| 410.6 | True posterior wall infarction | – | – |
| 410.7 | Subendocardial infarction | – | – |
| 410.8 | Acute myocardial infarction of other specified sites (infarction of atrium, papillary muscle, septum alone) | – | – |
| 410.9 | Acute myocardial infarction: unspecified site | – | – |
| 411 | Other acute and subacute forms of ischemic heart disease | – | – |
| 412 | Old myocardial infarction | – | – |
| 413 | Angina pectoris | – | – |
| 414 | Other forms of chronic ischemic heart disease | – | – |
| 427.4 | Ventricular fibrillation and flutter | – | – |
| 427.5 | Cardiac arrest | – | – |
Table 2.
Validation Studies and Results until July 2010
| Author | Country | N | Year of Data Collection | Administrative Database | Gold Standard | ICD Code* | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Austin, Daly, and Tu (2002) | Canada | 58,816 | Jan 1996–Mar 2000 | Hospital discharge | Registry data | 410 | MRD: 88.8 Any: 92.8 | MRD: 92.8 Any: 89.2 | MRD: 88.5 Any: 84.2 | |
| Beaglehole, Stewart, and Walker (1987) | New Zealand | 858 | 1983 | Hospital discharge | Registry data | 410 | 86.0 | – | 67.1 | – |
| 410–414 | 95.1 | – | 25.6† | – | ||||||
| Boyle and Dobson (1995) | Australia | 5,283 | Aug 1986–Dec 1991 | Hospital discharge | Registry data | 410 | 78.9 | – | 65.6 | – |
| Dobson et al. (1988) | Australia | 2,947 | 1979, 1984–1985 | Hospital discharge | Registry data | 410 | 84.8 (1979) 84.8 (1984) | – | 79.3 (1979) 70.2 (1984) | – |
| 410–414 | 78.6 (1979) 91.6 (1984) | – | 67.9 (1979) 42.7 (1984) | – | ||||||
| Ellerbeck et al. (1995) | USA | 14,108 | June 1992–Feb 1993 | Hospital discharge | Chart review | 410 | – | – | 87.4 | – |
| Fisher et al. (1992) | USA | Any: 271 Principle: 204 | Oct 1984–Mar 1985 | Hospital discharge | Chart review | 410 | Any diagnostic field: 90.0 Primary diagnostic field: 94.0 | – | Any diagnostic field: 87.0 Primary diagnostic field: 92.0 | – |
| Hammar et al. (2001) | Sweden | 713 | 1987–1995 | Hospital discharge | Chart review | 410 | 94.0 | – | 86.0 | – |
| Heckbert et al. (2004) | USA | 1,042 | Jan 1994–Nov 2000 | Hospital discharge | Chart review | 410, 427.4, 427.5 | 80.0 | 99.4† | 77.7 | 99.5† |
| Kennedy, Stern, and Crawford (1984) | USA | 20,386 | 12-month period before 1984 | Hospital discharge | Registry data | 410 | 94.3 | 99.8 | 60.9 | 100.0 |
| Kiyota et al. (2004) | USA | 2,022 | 1999, 2000 | Hospital discharge | Chart review | 410.x0 410.x1 | – | – | Any diagnostic field: 94.1 Primary diagnostic field: 95.1 | – |
| Levy et al. (1999) | Canada | 234 | 1994 | Hospital discharge | Chart review | 410 | – | – | 96.0 | – |
| Lindblad et al. (1993) | Sweden | 432 | 1977–1987 | Hospital admissions | Chart review | 410–411 | – | – | 91.4† | – |
| Mahonen et al. (1997) | Finland | 397 | 1983–1990 | Hospital discharge | Registry data | 410 | Men: 86.0 Women: 81.3 | – | Men: 85.9 Women: 80.7 | – |
| 410–411 | Men: 79.6 Women: 73.9 | – | Men: 84.8 Women: 79.0 | – | ||||||
| Mascioli, Jacobs, and Kottke (1989) | USA | 1,845 | Jan–June 1979 | Hospital discharge | Chart review | 410–411 | 84.7 | 92.8 | 94.6 | – |
| 412–414 | – | – | 18.8 | – | ||||||
| McAlpine et al. (1998) | Scotland | 154 | Oct 1993–Oct 1995 | Hospital discharge | Chart review | 410 | 67.0 | 100.0 | 100.0 | – |
| 411 | 5.6 | 99.0 | 50.0 | – | ||||||
| 413 | 5.6 | 94.0 | 9.1 | – | ||||||
| 414 | 5.6 | 86.0 | 4.5 | – | ||||||
| Merry et al. (2009) | The Netherlands | 21,110 | 1987–1997 | Hospital discharge | Registry data | 410 | 84.0 | – | 97.0 | – |
| Newton et al. (1999) | USA | 121 | Jan 1992–Mar 1996 | Hospital data | Chart review | 410, 427.4, 427.5 | 94.4 | 86.4 | 56.8 | – |
| Nova Scotia-Saskatchewan Cardiovascular Disease Epidemiology Group (1992) | Canada | 410: 1,810 411–414: 1,059 | 1977–1985 | Hospital discharge | Chart review | 410 | – | – | 85.5† | – |
| 411–414 | – | – | 7.1† | – | ||||||
| Pajunen et al. (2005) | Finland | 37,062 CHD events | 1988–2002 | Hospital discharge | Chart review | 410, I21, I22 | 83.0 | – | 90.0 | – |
| Palomaki et al. (1994) | Finland | 1,565 | 1987–1990 | Hospital discharge | Registry data | 410.0 | 88.7† | 93.8† | 86.4† | 92.4† |
| 410.0–410.9 | 72.3† | 90.6† | 92.0† | 68.8† | ||||||
| 410, 411 | 71.0† | 74.9† | 89.6† | 45.8† | ||||||
| Petersen et al. (1999) | USA | 4,565 | Jan 1994–Sep 1995 | Hospital discharge | Chart review | 410 | – | – | 96.9 | – |
| Pladevall et al. (1996) | USA | 734 | May 1988–Apr 1990 | Hospital discharge | Registry data | 410 | 80.9 | 93.1 | 54.6 | 97.9 |
| 410–411 | 86.5 | 80.2 | 31.0 | 98.3 | ||||||
| Rosamond et al. (2004) | USA | 17,900 | 1987–2000 | Hospital Discharge | Chart review | 410 | Men: 69.0 | – | Men: 58.0 | – |
| Women: 66.0 | Women: 52.0 | |||||||||
| Ryu et al. (2000) | Korea | 258 | 1993–1997 | Hospital discharge | Chart review | 410 | – | – | 76.0 | – |
| Varas-Lorenzo et al. (2008) | Canada | ICD-9 code 410:193 | Nov 1999–Dec 2001 | Hospital discharge | Chart review | 410 | – | – | 94.8† | – |
| 411 | – | – | 8.7† | – | ||||||
| ICD-9 code 411:763 | ||||||||||
| Yeh et al. (2010) | USA | 640 | 1999–2007 | Hospital discharge | Chart review | 410.x0, 410.x1 | – | – | 96.7 | – |
All are ICD-9 codes except for I21 and I22, which are ICD-10 codes.
Derived values.
AMI, acute myocardial infarction; CHD, coronary heart disease; MRD, most responsible diagnosis; NPV, negative predictive value; PPV, positive predictive value.
PPV was reported in 22 studies (range: 5.6–98.7 percent). The ICD-9 code 410 used in isolation had the highest reported PPV (range: 54.6–98.7 percent) but PPV decreased when ICD-9 410 was used in combination with other codes (range: 19–90 percent) that were not specific to AMI. NPV was only calculated in four studies (Kennedy, Stern, and Crawford 1984; Palomaki et al. 1994; Pladevall et al. 1996; Heckbert et al. 2004), where values ranged from 68.8 to 100 percent for ICD-9 410 in isolation, and from 45.8 to 98.3 percent for ICD-9 410–411.
Literature Review of Case Definitions Used in AMI Studies
Sixty-three articles were identified, including eight studies from Canada, six from Denmark, one from Italy, two from the Netherlands, one from New Zealand, two from Scotland, two from Sweden, one from the United Kingdom, and forty-one from the United States. Fifty-three studies used ICD-9 coding, all of which used some variation in ICD-9 code 410 to identify cases of AMI (see Table 3). Fifteen studies used ICD-10 codes, all of which used some variation in ICD-10 code I21 to identify cases of AMI (see Table 3).
Table 3.
Case Definitions of Acute Myocardial Infarction Commonly Used in the Literature (2007–2012)
| Author | Country | Study Years | ICD-9 Case Definition | ICD-10 Case Definition |
|---|---|---|---|---|
| Agyemang et al. (2009) | The Netherlands | 1995 | 410 | |
| Berger et al. (2008) | USA | 2001 | 410 | |
| Brown, Xie, and Mensah (2007) | USA | 2003–2004 | 410 | |
| Buch et al. (2007) | Denmark | 1994–2002 | I21, I22 | |
| Chan et al. (2008) | New Zealand | 1993–2005 | 410 | I21 |
| Chen et al. (2010) | USA | 2002–2007 | 410.x0, 410.x1 | |
| Curtis et al. (2009) | USA | 2005 | 410.x0, 410.x1 | |
| Dudas et al. (2011) | Sweden | 1991–2006 | 410 | I21 |
| Ezekowitz et al. (2009) | Canada | 1994–2005 | 410 | |
| Fazel et al. (2009) | USA | 2000–2006 | 410.x1 | |
| Friberg et al. (2009) | Sweden | 2002 | I21 | |
| Garg et al. (2008) | USA | 2003–2004 | 410.x1 | |
| Habel et al. (2011) | USA | 1986–2005 | 410 | I21, I22 |
| Hammill et al. (2009) | USA | 1999–2006 | 410.x1 | |
| Ho et al. (2008) | USA | 2003–2005 | 410 | |
| Hvelplund et al. (2010) | Denmark | 2005–2007 | I21, I22 | |
| Jackevicius, Li, and Tu (2008) | Canada | 1999–2001 | 410 | |
| Jensen et al. (2010) | Denmark | 2002–2005 | I21 | |
| Joynt et al. (2011a) | USA | 2009 | 410.x0, 410.x1 | |
| Joynt, Orav, and Jha (2011b) | USA | 2006–2009 | 410.x0, 410.x1 | |
| Khan et al. (2010) | Canada | 1994–2003 | 410 | |
| King, Khan, and Quan (2009) | Canada | 2002–2006 | I21, I22 | |
| Ko et al. (2007) | Canada and USA | 1998–1999 | 410 | |
| Ko et al. (2008) | USA | 1998–2001 | 410 | |
| Kosiborod et al. (2008) | USA | 2000–2005 | 410.x0, 410.x1 | |
| Kosiborod et al. (2009) | USA | 2000–2005 | 410.x0, 410.x1 | |
| Kostis et al. (2007) | USA | 1987–2005 | 410 | |
| Krumholz et al. (2009) | USA | 1995–2006 | 410.x0, 410.x1 | |
| Kulik et al. (2010) | USA | 1995–2004 | 410.x1, 411 | |
| Lambert et al. (2010) | Canada | 2006–2007 | 410 | |
| Lipscombe et al. (2007) | Canada | 2002–2005 | I21, I24, I25.4 | |
| Mauri et al. (2008) | USA | 2003–2004 | 410.x1 | |
| Mazzini et al. (2008) | USA | 2002–2003 | 410 | |
| McAlister et al. (2008) | Canada | 1994–2000 | 410 | |
| McNamara et al. (2007) | USA | 1999–2002 | 410.x1 | |
| Mehta et al. (2010) | USA | Not stated | 410 | |
| Mehta et al. (2008) | USA | 2000–2008 | 410 | |
| Movahed et al. (2009) | USA | 1998–2004 | 410.01, 410.11, 410.21, 410.31, 410.41, 410.51, 410.61, 410.81 | |
| Nallamothu et al. (2007a) | USA | 2003 | 410.x0, 410.x1 | |
| Nallamothu et al. (2007b) | USA | 2002–2005 | 410.x1 | |
| Pearte et al. (2008) | USA | 1987–2001 | 402, 410–414, 427, 428, 518.4 | |
| Popescu, Cram, and Vaughan-Sarrazin (2011) | USA | 2005 | 410 | |
| Popescu, Vaughan-Sarrazin, and Rosenthal (2007) | USA | 2000–2005 | 410 | |
| Roger et al. (2010) | USA | 1987–2006 | 410 | |
| Ross et al. (2010) | USA | 2004–2006 | 410.x0, 410.x1 | |
| Saia et al. (2009) | Italy | 2002, 2004 | 410 | |
| Schjerning Olsen et al. (2011) | Denmark | 1997–2006 | I21, I22 | |
| Sekhri et al. (2007) | United Kingdom | 2003–2005 | I21–I23 | |
| Setoguchi et al. (2007) | USA | 1995–2004 | 410 | |
| Setoguchi et al. (2008a) | USA | 1995–2004 | 410 | |
| Setoguchi et al. (2008b) | USA | 1999–2000 | 410 | |
| Shen and Hsia (2011) | USA | 2000–2006 | 410.x0, 410.x1 | |
| Shreibati, Baker, and Hlatky (2011) | USA | 2005–2008 | 410.x | |
| Sorensen et al. (2011) | Denmark | 2002–2008 | I21, I22 | |
| Sorensen et al. (2009) | Denmark | 2000–2005 | I21, I22 | |
| Suaya et al. (2007) | USA | 1997 | 410 | |
| Taylor et al. (2008) | Scotland | 1996–2000 | 410 | I21, I22 |
| Towfighi, Markovic, and Ovbiagele (2011) | USA | 1997–2006 | 410.x0, 410.x1 | |
| van der Elst et al. (2007) | The Netherlands | 1991–2000 | 410 | |
| Volpp et al. (2007a) | USA | 2000–2005 | 410.00–410.19, 410.20–410.69, 410.7x, 410.80–410.99 | |
| Volpp et al. (2007b) | USA | 2000–2005 | 410.00–410.19, 410.20–410.69, 410.7x, 410.80–410.99 | |
| Wei et al. (2008) | Scotland | 1994–2003 | 410 | I21 |
| Yeh et al. (2010) | USA | 1999–2008 | 410.x0, 410.x1 |
Validating AMI Case Definitions in Dually Coded ICD-9-CM and ICD-10 Hospital Discharge Data
Of the 4,008 charts reviewed, 169 indicated that the patient had AMI resulting in a prevalence of 4.2 percent. All previously validated case definitions had specificity values of at least 99 percent and NPV 86 percent or above; however, sensitivity ranged from 20.9 percent (ICD-9 411) to 84.0 percent (ICD 9 410.x0, 410.x1) and PPV ranged from 13.6 percent (ICD-9 411) to 97.6 percent (ICD 9 410–414) (see Table 4). Use of either ICD-9 410 or ICD-10 I21–I22 resulted in similar validity.
Table 4.
Validation of International Disease Classification (ICD) Hospital Discharge Abstract Data Based on Chart Review Data for Acute Myocardial Infarction
| Case Definition | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) |
|---|---|---|---|---|
| ICD-9-CM | ||||
| 410 | 83.3 | 99.2 | 82.8 | 99.3 |
| 410.x0, 410.x1 | 84.0 | 99.2 | 81.1 | 99.3 |
| 410, 411 | 56.5 | 99.4 | 87.0 | 97.1 |
| 410–414 | 24.2 | 99.9 | 97.6 | 86.5 |
| 410, 427.4, 427.5 | 73.1 | 99.3 | 83.4 | 98.6 |
| 411 | 20.9 | 96.3 | 13.6 | 97.7 |
| 411–414 | 22.7 | 99.4 | 87.6 | 86.8 |
| ICD-10 | ||||
| I21, I22 | 81.8 | 99.2 | 82.2 | 99.2 |
AMI Case Volume and In-Hospital Mortality in Hospital Discharge Data
The eight previously validated case definitions were applied to hospital discharge abstract data (n = 94,937 for ICD-9-CM, 2001/2002 and n = 118,839 for ICD-10, 2006/2007) to assess their impact on number of AMI cases and in-hospital mortality (Table 5). The ICD-9 code combination 410–414 identified the greatest number of AMI cases in any diagnostic field (n = 14,645) and in the primary diagnostic field (n = 3,581). The ICD-9 code 410, the most commonly validated AMI code in the literature, identified 1,958 cases using all diagnostic fields and 1,488 cases using only the primary diagnostic field. In-hospital mortality from validated case definitions ranged from 0 percent (ICD-9 411 used in isolation and found in either the primary diagnostic field or any diagnostic field) to 10.3 percent (ICD-9 410.0 used in isolation and found in the primary diagnostic field). The mortality was 6.1 percent (n = 91 deaths) among AMI cases identified using ICD-9 code 410 on the primary diagnosis coding field, and 6.6 percent (n = 129 deaths) among AMI cases using ICD-9 code 410 in any diagnostic coding fields.
Table 5.
Acute Myocardial Infarction (AMI) Case Volume and In-Hospital Deaths by Case Definition
| ICD Codes | AMI Defined Using Primary Diagnosis (A) | Number of Death (B) | Death Rate (A/B%) | AMI Defined Using Primary and Secondary Diagnosis (C) | Number of Death (D) | Death Rate (C/D%) | |
|---|---|---|---|---|---|---|---|
| Year 2001/2002 (ICD-9-CM) | |||||||
| ICD-9-CM case definitions | 410 | 1,488 | 91 | 6.1 | 1,958 | 129 | 6.6 |
| 410.x0, 410,x1 | 1,477 | 91 | 7.0 | 1,855 | 129 | 7.0 | |
| 410, 411 | 1,621 | 91 | 5.6 | 3,352 | 129 | 3.8 | |
| 410–414 | 3,581 | 111 | 3.1 | 14,645 | 219 | 1.5 | |
| 410, 427.4, 427.5 | 1,515 | 100 | 6.6 | 2,322 | 143 | 6.2 | |
| 411 | 130 | 0 | 0.0 | 1,306 | 0 | 0.0 | |
| 411–414 | 1,961 | 20 | 1.0 | 11,974 | 88 | 0.7 | |
| Relative contribution of each code to ICD-9-CM case definitions | 410.x0 | 11 | 2 | 18.2 | 17 | 2 | 11.8 |
| 410.x1 | 1,466 | 89 | 6.1 | 1,838 | 127 | 6.9 | |
| 410.0 | 68 | 7 | 10.3 | 75 | 7 | 9.3 | |
| 410.1 | 249 | 23 | 9.2 | 303 | 24 | 7.9 | |
| 410.2 | 57 | 7 | 12.3 | 65 | 7 | 10.8 | |
| 410.3 | 65 | 3 | 4.6 | 77 | 3 | 3.9 | |
| 410.4 | 285 | 8 | 2.8 | 331 | 14 | 4.2 | |
| 410.5 | 26 | 1 | 3.8 | 41 | 2 | 4.8 | |
| 410.6 | 7 | 0 | 0.0 | 12 | 0 | 0.0 | |
| 410.7 | 566 | 19 | 3.4 | 744 | 29 | 3.9 | |
| 410.8 | 14 | 3 | 21.4 | 26 | 3 | 11.5 | |
| 410.9 | 53 | 14 | 26.4 | 167 | 33 | 19.8 | |
| 412 | 0 | 0 | 0.0 | 2,637 | 9 | 0.3 | |
| 413 | 76 | 0 | 0.0 | 1,271 | 3 | 0.2 | |
| 414 | 1,755 | 20 | 1.1 | 6,760 | 76 | 1.1 | |
| 427.4 | 17 | 3 | 17.6 | 119 | 0 | 0.0 | |
| 427.5 | 9 | 6 | 66.7 | 224 | 43 | 19.2 | |
| Year 2006/2007 (ICD-10) | |||||||
| ICD-10 case definition | I21, I22 | 1,425 | 94 | 6.6 | 2,450 | 186 | 7.6 |
| Relative contribution of each code to ICD-10 case definition | I21 | 1,422 | 94 | 6.6 | 2,443 | 186 | 7.6 |
| I22 | 3 | 0 | 0.0 | 7 | 0 | 0.0 | |
Some component parts of various case definitions identified few cases, but they had very high mortality rates. For example, when used in the primary position, the ICD-9 code 427.5 (cardiac arrest) identified nine hospitalized patients, but it was associated with a mortality rate of 66.7 percent; the mortality rate for this code dropped to 19.2 percent when found in any diagnostic coding field. In other instances, specific codes contributed very little to case definitions. For example, the validated case definition ICD-10 I21 or I22 identified 1,425 admissions when either code was found in the primarily position, and 2,450 admissions when either code was found in any diagnostic coding field; however, the ICD-10 code I22 only identified three admissions if it was coded in the primary diagnostic coding field and seven admissions if it was coded in any diagnostic coding field and no deaths (regardless of coding field).
DISCUSSION
Through a systematic review of the literature, this study identified eight validated AMI case definitions using hospital discharge abstract data. These validated case definitions had varying ranges of validity. Based on reported values for sensitivity, specificity, PPV, and NPV, it appears that the three-digit ICD-9 code 410 (acute myocardial infarction) used in isolation had the highest validity. When these eight case definitions were validated in one dataset, ICD-9 410 still had high validity. Although a substantial amount of heterogeneity was noted in the content of case definitions, which is reflected in the variability of their performance characteristics, there is a substantial amount of agreement with regard to case definitions that are used in the published literature. An examination of ICD-9 and ICD-10 codes used in the published literature revealed very few differences in the codes used—all studies that used ICD-9 used some variation in code 410, while all studies that used ICD-10 used some variation in ICD-10 code I21, thus allowing for meaningful comparisons across studies. However, as more countries transition from ICD-9 to ICD-10, the ICD-10-based case definitions for AMI codes should be validated.
While the reasoning for the variation in reported values of sensitivity and specificity for the same case definition is unclear, it could be due to the underlying definition of AMI. Many studies included ICD-9 code 411 (other acute and subacute forms of ischemic heart disease) in their definition. As this code is not the correct assignment of true AMI cases, its inclusion reduces the specificity of the case definition. Inclusion of ICD-9 codes 412 (old myocardial infarction) and 413 (angina pectoris) in the case definition further reduces the specificity of a case definition that aims to identify cases of acute myocardial infarction as it mixes symptoms with disease and includes conditions that are clinically distinct from AMI. Limiting the administrative data case definition to codes found in the primary diagnostic coding field can also impact the sensitivity and specificity of reported definitions as codes in this position merely represent the main reason for hospitalization or resource consumption, but they cannot capture all health events that occurred in hospital or that motivated hospital admission. Searching secondary code positions for codes of interest will increase the sensitivity of a case definition. The heterogeneity in the codes used to identify AMI may also reflect underlying clinical uncertainty in the definition of AMI. Multiple clinical diagnostics such as imaging, biochemistry, electrocardiography, and pathology are used to clinically establish whether a patient experienced an AMI (Thygesen et al. 2007). As the science of each of these fields has advanced, clinicians have been able to more accurately diagnosis AMI events; this is particularly true for biochemistry, as the rapid introduction of new biomarkers in recent years, such as the introduction of troponin as a biochemical marker of AMI, has increased the clinical sensitivity and specificity of AMI diagnoses (Thygesen et al. 2007). While changing clinical definitions of AMI are not currently reflected in ICD codes, any clinical changes that improve the accuracy of AMI diagnoses will impact the incidence and prevalence of this condition when studied using administrative data.
Differences in the predictive ability of case definitions could also be related to the gold standard used to confirm the AMI diagnosis and the population studied. Studies have shown that accepting the diagnosis coded in the chart at face value is not always valid (Iezzoni et al. 1988; Hennessy et al. 2010). The use of clinical parameters in the chart to assess for the presence or absence of AMI instead of accepting the diagnosis as written in the chart likely increases the sensitivity of the case definition. In addition, the source population captured by the gold standard will influence the predictive ability of case definitions. Patient registries will typically capture a different population than that identified by general medical record review as registries tend to focus on higher risk populations, thus artificially increasing the sensitivity of a case definition as only the sickest individuals are captured in the reference standard. The reporting of PPV, in addition to sensitivity, can help overcome this limitation.
Also of note is the variation in health care systems across countries with regard to coder variation (trained health coders vs. physician coders) (Hennessy et al. 2010), the number of secondary diagnoses allowed (World Health Organization 2010), and country-specific modifications to ICD coding manuals (Jette et al. 2010; World Health Organization 2010); all of these factors may impact the validity of case definitions.
This study draws to light the differences in reporting practices for validation studies and indicates the need for reporting guidelines for this body of literature to enhance comparability between studies. This study also calls into question what values of sensitivity and specificity are required to call a case definition “validated”. While sensitivity and specificity values of greater than 80 percent are considered excellent, sensitivity values as low as 66 percent for AMI are found in the literature (Rosamond et al. 2004). While a specificity value below 80 percent was only found in one study included in the review (Palomaki et al. 1994), only eight (Kennedy, Stern, and Crawford 1984; Mascioli, Jacobs, and Kottke 1989; Palomaki et al. 1994; Pladevall et al. 1996; McAlpine et al. 1998; Newton et al. 1999; Austin, Daly, and Tu 2002; Heckbert et al. 2004) of the 26 studies reported data on specificity.
While ICD-10 has been available for over 20 years (World Health Organization 2010) and its coding descriptions dramatically changed compared with ICD-9, no studies could be found that exclusively validated ICD-10 codes for AMI. ICD-10 and ICD-9 specified AMI using inconsistent duration from onset; the longer duration in ICD-9 than ICD-10 (8 weeks or less vs. 4 weeks or less) might result in more AMIs being coded in ICD-9 than ICD-10. In addition, the ICD-9 code 410 and ICD-10 code I21 (AMI) are subdivided into transmural AMI and nontransmural AMI; however, this subdivision is not defined by ST segment elevation. Although modified versions of ICD-9-CM (Steinberg et al. 2008) and ICD-10 Canadian modification have been developed to distinguish between ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation myocardial infarction (NSTEMI), not all countries make use of these modifications. The ICD-11 will specify STEMI and NSTEMI.
This study has some limitations. The literature review was limited to papers written in English only and validation studies published in the gray literature were not included. Publication bias was not specifically assessed; however, as several studies were identified with low sensitivity, specificity, positive, and negative predictive values, this is not believed to have substantially influenced the results. It is possible that individual authors selectively reported only their best case definition as opposed to all case definitions tested. As inter-country differences exist in administrative coding practices (Hennessy et al. 2010; Jette et al. 2010), it is also possible that the results generated by applying the validated case definitions to Alberta data may not be generalizable to other regions. Furthermore, as 2001–2002 was in the early phases of troponin use as a clinical biomarker of AMI, the comparison of results from 2001/02 to 2006/07 is likely to be influenced by changing clinical practices in addition to changes in administrative data coding practices.
In conclusion, a variety of case definitions for AMI using administrative data have been found in the literature, with variable validity. While reporting guidelines for validation studies have recently been released (Benchimol et al. 2011), their application is essential to ensure comparability between studies and to ensure adequate reporting of results. In addition, international consensus on what constitutes an AMI and validation of ICD-10 codes for AMI is critically needed as more countries introduce this coding framework for epidemiological and outcomes study of AMI. We recommend ICD-9-CM code 410 and ICD-10 codes I21 and I22 in the primary diagnosis coding field should be used to define AMI.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Amy Metcalfe holds a Canadian Institutes of Health Research Award in Genetics (Ethics, Law, and Society) and a CIHR Strategic Training Program Studentship award in Genetics, Child Development, and Health. Hude Quan holds a Senior Scholar award from Alberta Innovates Health Solutions (AIHS). Nathalie Jetté holds a New Investigator Award from AIHS and a Canada Research Chair Tier 2 in Neurological Health Services Research. Please refer to SA1 for additional information.
Disclaimers: None.
Disclosures: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Agyemang C, Vaartjes I, Bots ML, Berger-van Sijl IG, van Valkengoed JS, de Munter A, de Bruin M, Reitsma JB, Stronks K. “Risk of Death after First Admission for Cardiovascular Diseases by Country of Birth in the Netherlands: A Nationwide Record-Linked Retrospective Cohort Study”. Heart. 2009;95(9):747–53. doi: 10.1136/hrt.2008.159285. [DOI] [PubMed] [Google Scholar]
- Austin PC, Daly PA, Tu JV. “A Multicenter Study of the Coding Accuracy of Hospital Discharge Administrative Data for Patients Admitted to Cardiac Care Units in Ontario”. American Heart Journal. 2002;144(2):290–6. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- Beaglehole R, Stewart AW, Walker P. “Validation of Coronary Heart Disease Hospital Discharge Data”. Australian and New Zealand Journal of Medicine. 1987;17(1):43–6. doi: 10.1111/j.1445-5994.1987.tb05048.x. [DOI] [PubMed] [Google Scholar]
- Benchimol EI, Manuel DG, To T, Griffiths AM, Rabeneck L, Guttmann A. “Development and Use of Reporting Guidelines for Assessing the Quality of Validation Studies of Health Administrative Data”. Journal of Clinical Epidemiology. 2011;64(8):821–9. doi: 10.1016/j.jclinepi.2010.10.006. [DOI] [PubMed] [Google Scholar]
- Berger AK, Duval S, Jacobs DR, Jr, Barber C, Vazquez G, Lee S, Luepker RV. “Relation of Length of Hospital Stay in Acute Myocardial Infarction to Postdischarge Mortality”. American Journal of Cardiology. 2008;101(4):428–34. doi: 10.1016/j.amjcard.2007.09.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle CA, Dobson AJ. “The Accuracy of Hospital Records and Death Certificates for Acute Myocardial Infarction”. Australian and New Zealand Journal of Medicine. 1995;25(4):316–23. doi: 10.1111/j.1445-5994.1995.tb01896.x. [DOI] [PubMed] [Google Scholar]
- Brown DW, Xie J, Mensah GA. “Electrocardiographic Recording and Timeliness of Clinician Evaluation in the Emergency Department in Patients Presenting with Chest Pain”. American Journal of Cardiology. 2007;99(8):1115–8. doi: 10.1016/j.amjcard.2006.12.023. [DOI] [PubMed] [Google Scholar]
- Buch P, Rasmussen S, Gislason GH, Rasmussen JN, Kober L, Gadsboll N, Stender S, Madsen M, Torp-Pedersen C, Abildstrom SZ. “Temporal Decline in the Prognostic Impact of a Recurrent Acute Myocardial Infarction 1985 to 2002”. Heart. 2007;93(2):210–5. doi: 10.1136/hrt.2006.092213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan WC, Wright C, Tobias M, Mann S, Jackson R. “Explaining Trends in Coronary Heart Disease Hospitalisations in New Zealand: Trend for Admissions and Incidence Can Be in Opposite Directions”. Heart. 2008;94(12):1589–93. doi: 10.1136/hrt.2008.142588. [DOI] [PubMed] [Google Scholar]
- Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. “Recent Declines in Hospitalizations for Acute Myocardial Infarction for Medicare Fee-for-Service Beneficiaries: Progress and Continuing Challenges”. Circulation. 2010;121(11):1322–8. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- Curtis JP, Schreiner G, Wang Y, Chen J, Spertus JA, Rumsfeld JS, Brindis RG, Krumholz HM. “All-Cause Readmission and Repeat Revascularization after Percutaneous Coronary Intervention in a Cohort of Medicare Patients”. Journal of the American College of Cardiology. 2009;54(10):903–7. doi: 10.1016/j.jacc.2009.04.076. [DOI] [PubMed] [Google Scholar]
- Dobson AJ, Gibberd RW, Leeder SR, Alexander HM, Young AF, Lloyd DM. “Ischemic Heart Disease in the Hunter Region of New South Wales, Australia, 1979–1985”. American Journal of Epidemiology. 1988;128(1):106–15. doi: 10.1093/oxfordjournals.aje.a114933. [DOI] [PubMed] [Google Scholar]
- Dudas K, Lappas G, Stewart S, Rosengren A. “Trends in Out-of-Hospital Deaths due to Coronary Heart Disease in Sweden (1991 to 2006)”. Circulation. 2011;123(1):46–52. doi: 10.1161/CIRCULATIONAHA.110.964999. [DOI] [PubMed] [Google Scholar]
- Ellerbeck EF, Jencks SF, Radford MJ, Kresowik TF, Craig AS, Gold JA, Krumholz HM, Vogel RA. “Quality of Care for Medicare Patients with Acute Myocardial Infarction. A Four-State Pilot Study from the Cooperative Cardiovascular Project”. Journal of the American Medical Association. 1995;273(19):1509–14. [PubMed] [Google Scholar]
- van der Elst ME, Bouvy ML, de Blaey CJ, de Boer A. “Effect of Drug Combinations on Admission for Recurrent Myocardial Infarction”. Heart. 2007;93(10):1226–30. doi: 10.1136/hrt.2006.098053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezekowitz JA, Kaul P, Bakal JA, Armstrong PW, Welsh RC, McAlister FA. “Declining In-Hospital Mortality and Increasing Heart Failure Incidence in Elderly Patients with First Myocardial Infarction”. Journal of the American College of Cardiology. 2009;53(1):13–20. doi: 10.1016/j.jacc.2008.08.067. [DOI] [PubMed] [Google Scholar]
- Fazel R, Krumholz HM, Bates ER, French WJ, Frederick PD, Nallamothu BK. “Choice of Reperfusion Strategy at Hospitals with Primary Percutaneous Coronary Intervention: A National Registry of Myocardial Infarction Analysis”. Circulation. 2009;120(24):2455–61. doi: 10.1161/CIRCULATIONAHA.109.860544. [DOI] [PubMed] [Google Scholar]
- Fisher ES, Whaley FS, Krushat WM, Malenka DJ, Fleming C, Baron JA, Hsia DC. “The Accuracy of Medicare's Hospital Claims Data: Progress Has Been Made, But Problems Remain”. American Journal of Public Health. 1992;82(2):243–8. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friberg L, Hammar N, Edvardsson N, Rosenqvist M. “The Prognosis of Patients with Atrial Fibrillation is Improved When Sinus Rhythm Is Restored: Report from the Stockholm Cohort of Atrial Fibrillation (SCAF)”. Heart. 2009;95(12):1000–5. doi: 10.1136/hrt.2008.149237. [DOI] [PubMed] [Google Scholar]
- Garg P, Normand SL, Silbaugh TS, Wolf RE, Zelevinsky K, Lovett A, Varma MR, Zhou Z, Mauri L. “Drug-Eluting or Bare-Metal Stenting in Patients with Diabetes Mellitus: Results from the Massachusetts Data Analysis Center Registry”. Circulation. 2008;118(22):2277–85. doi: 10.1161/CIRCULATIONAHA.108.820159. [DOI] [PubMed] [Google Scholar]
- Habel LA, Cooper WO, Sox CM, Chan KA, Fireman BH, Arbogast PG, Cheetham TC, Quinn VP, Dublin S, Boudreau DM, Andrade SE, Pawloski PA, Raebel MA, Smith DH, Achacoso N, Uratsu C, Go AS, Sidney S, Nguyen-Huynh MN, Ray WA, Selby JV. “ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged Adults”. Journal of the American Medical Association. 2011;306(24):2673–83. doi: 10.1001/jama.2011.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammar N, Alfredsson L, Rosen M, Spetz CL, Kahan T, Ysberg AS. “A National Record Linkage to Study Acute Myocardial Infarction Incidence and Case Fatality in Sweden”. International Journal of Epidemiology. 2001;30(suppl 1):S30–4. doi: 10.1093/ije/30.suppl_1.s30. [DOI] [PubMed] [Google Scholar]
- Hammill BG, Curtis LH, Schulman KA, Whellan DJ. “Relationship between Cardiac Rehabilitation and Long-Term Risks of Death and Myocardial Infarction among Elderly Medicare Beneficiaries”. Circulation. 2009;121(1):63–70. doi: 10.1161/CIRCULATIONAHA.109.876383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckbert SR, Kooperberg C, Safford MM, Psaty BM, Hsia J, McTiernan A, Gaziano JM, Frishman WH, Curb JD. “Comparison of Self-Report, Hospital Discharge Codes, and Adjudication of Cardiovascular Events in the Women's Health Initiative”. American Journal of Epidemiology. 2004;160(12):1152–8. doi: 10.1093/aje/kwh314. [DOI] [PubMed] [Google Scholar]
- Hennessy DA, Quan H, Faris PD, Beck CA. “Do Coder Characteristics Influence Validity of ICD-10 Hospital Discharge Data?”. BMC Health Service Research. 2010;10:99. doi: 10.1186/1472-6963-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho PM, Peterson ED, Wang L, Magid DJ, Fihn SD, Larsen GC, Jesse RA, Rumsfeld JS. “Incidence of Death and Acute Myocardial Infarction Associated with Stopping Clopidogrel after Acute Coronary Syndrome”. Journal of the American Medical Association. 2008;299(5):532–9. doi: 10.1001/jama.299.5.532. [DOI] [PubMed] [Google Scholar]
- Hvelplund A, Galatius S, Madsen M, Rasmussen JN, Sorensen R, Fosbol EL, Madsen JK, Rasmussen S, Jorgensen E, Thuesen L, Moller CH, Abildstrom SZ. “Influence of Distance from Home to Invasive Centre on Invasive Treatment after Acute Coronary Syndrome: A Nationwide Study of 24 910 Patients”. Heart. 2010;97(1):27–32. doi: 10.1136/hrt.2010.203901. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Burnside S, Sickles L, Moskowitz MA, Sawitz E, Levine PA. “Coding of Acute Myocardial Infarction. Clinical and Policy Implications”. Annals of Internal Medicine. 1988;109(9):745–51. doi: 10.7326/0003-4819-109-9-745. [DOI] [PubMed] [Google Scholar]
- Jackevicius CA, Li P, Tu JV. “Prevalence, Predictors, and Outcomes of Primary Nonadherence after Acute Myocardial Infarction”. Circulation. 2008;117(8):1028–36. doi: 10.1161/CIRCULATIONAHA.107.706820. [DOI] [PubMed] [Google Scholar]
- Jensen LO, Maeng M, Thayssen P, Kaltoft A, Tilsted HH, Lassen JF, Hansen KN, Bottcher M, Rasmussen K, Madsen M, Johnsen SP, Sorensen HT, Thuesen L. “Long-term Outcomes after Percutaneous Coronary Intervention in Patients with and without Diabetes Mellitus in Western Denmark”. American Journal of Cardiology. 2010;105(11):1513–9. doi: 10.1016/j.amjcard.2010.01.007. [DOI] [PubMed] [Google Scholar]
- Jette N, Quan H, Hemmelgarn B, Drosler S, Maass C, Moskal L, Paoin W, Sundararajan V, Gao S, Jakob R, Ustun B, Ghali WA. “The Development, Evolution, and Modifications of ICD-10: Challenges to the International Comparability of Morbidity Data”. Medical Care. 2010;48(12):1105–10. doi: 10.1097/MLR.0b013e3181ef9d3e. [DOI] [PubMed] [Google Scholar]
- Joynt KE, Orav EJ, Jha AK. “Thirty-day Readmission Rates for Medicare Beneficiaries by Race and Site of Care”. Journal of the American Medical Association. 2011b;305(7):675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joynt KE, Harris Y, Orav EJ, Jha AK. “Quality of Care and Patient Outcomes in Critical Access Rural Hospitals”. Journal of the American Medical Association. 2011a;306(1):45–52. doi: 10.1001/jama.2011.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy GT, Stern MP, Crawford MH. “Miscoding of Hospital Discharges as Acute Myocardial Infarction: Implications for Surveillance Programs Aimed at Elucidating Trends in Coronary Artery Disease”. American Journal of Cardiology. 1984;53(8):1000–2. doi: 10.1016/0002-9149(84)90625-8. [DOI] [PubMed] [Google Scholar]
- Khan NA, Grubisic M, Hemmelgarn B, Humphries K, King KM, Quan H. “Outcomes after Acute Myocardial Infarction in South Asian, Chinese, and White Patients”. Circulation. 2010;122(16):1570–7. doi: 10.1161/CIRCULATIONAHA.109.850297. [DOI] [PubMed] [Google Scholar]
- King KM, Khan NA, Quan H. “Ethnic Variation in Acute Myocardial Infarction Presentation and Access to Care”. American Journal of Cardiology. 2009;103(10):1368–73. doi: 10.1016/j.amjcard.2009.01.344. [DOI] [PubMed] [Google Scholar]
- Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. “Accuracy of Medicare Claims-Based Diagnosis of Acute Myocardial Infarction: Estimating Positive Predictive Value on the Basis of Review of Hospital Records”. American Heart Journal. 2004;148(1):99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- Ko DT, Krumholz HM, Wang Y, Foody JM, Masoudi FA, Havranek EP, You JJ, Alter DA, Stukel TA, Newman AM, Tu JV. “Regional Differences in Process of Care and Outcomes for Older Acute Myocardial Infarction Patients in the United States and Ontario, Canada”. Circulation. 2007;115(2):196–203. doi: 10.1161/CIRCULATIONAHA.106.657601. [DOI] [PubMed] [Google Scholar]
- Ko DT, Wang Y, Alter DA, Curtis JP, Rathore SS, Stukel TA, Masoudi FA, Ross JS, Foody JM, Krumholz HM. “Regional Variation in Cardiac Catheterization Appropriateness and Baseline Risk after Acute Myocardial Infarction”. Journal of the American College of Cardiology. 2008;51(7):716–23. doi: 10.1016/j.jacc.2007.10.039. [DOI] [PubMed] [Google Scholar]
- Kosiborod M, Inzucchi SE, Krumholz HM, Xiao L, Jones PG, Fiske S, Masoudi FA, Marso SP, Spertus JA. “Glucometrics in Patients Hospitalized with Acute Myocardial Infarction: Defining the Optimal Outcomes-Based Measure of Risk”. Circulation. 2008;117(8):1018–27. doi: 10.1161/CIRCULATIONAHA.107.740498. [DOI] [PubMed] [Google Scholar]
- Kosiborod M, Inzucchi SE, Goyal A, Krumholz HM, Masoudi FA, Xiao L, Spertus JA. “Relationship between Spontaneous and Iatrogenic Hypoglycemia and Mortality in Patients Hospitalized with Acute Myocardial Infarction”. Journal of the American Medical Association. 2009;301(15):1556–64. doi: 10.1001/jama.2009.496. [DOI] [PubMed] [Google Scholar]
- Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. “Weekend versus Weekday Admission and Mortality from Myocardial Infarction”. New England Journal of Medicine. 2007;356(11):1099–109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- Krumholz HM, Wang Y, Chen J, Drye EE, Spertus JA, Ross JS, Curtis JP, Nallamothu BK, Lichtman JH, Havranek EP, Masoudi FA, Radford MJ, Han LF, Rapp MT, Straube BM, Normand SL. “Reduction in Acute Myocardial Infarction Mortality in the United States: Risk-Standardized Mortality Rates from 1995–2006”. Journal of the American Medical Association. 2009;302(7):767–73. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulik A, Singh JP, Levin R, Avorn J, Choudhry NK. “Association between Statin Use and the Incidence of Atrial Fibrillation Following Hospitalization for Coronary Artery Disease”. American Journal of Cardiology. 2010;105(12):1655–60. doi: 10.1016/j.amjcard.2010.01.341. [DOI] [PubMed] [Google Scholar]
- Lambert L, Brown K, Segal E, Brophy J, Rodes-Cabau J, Bogaty P. “Association between Timeliness of Reperfusion Therapy and Clinical Outcomes in ST-Elevation Myocardial Infarction”. Journal of the American Medical Association. 2010;303(21):2148–55. doi: 10.1001/jama.2010.712. [DOI] [PubMed] [Google Scholar]
- Levy AR, Tamblyn RM, Fitchett D, McLeod PJ, Hanley JA. “Coding Accuracy of Hospital Discharge Data for Elderly Survivors of Myocardial Infarction”. Canadian Journal of Cardiology. 1999;15(11):1277–82. [PubMed] [Google Scholar]
- Lindblad U, Rastam L, Ranstam J, Peterson M. “Validity of Register Data on Acute Myocardial Infarction and Acute Stroke: The Skaraborg Hypertension Project”. Scandinavian Journal of Social Medicine. 1993;21(1):3–9. doi: 10.1177/140349489302100102. [DOI] [PubMed] [Google Scholar]
- Lipscombe LL, Gomes T, Levesque LE, Hux JE, Juurlink DN, Alter DA. “Thiazolidinediones and Cardiovascular Outcomes in Older Patients with Diabetes”. Journal of the American Medical Association. 2007;298(22):2634–43. doi: 10.1001/jama.298.22.2634. [DOI] [PubMed] [Google Scholar]
- Mahonen M, Salomaa V, Brommels M, Molarius A, Miettinen H, Pyorala K, Tuomilehto J, Arstila M, Kaarsalo E, Ketonen M, Kuulasmaa K, Lehto S, Mustaniemi H, Niemela M, Palomaki P, Torppa J, Vuorenmaa T. “The Validity of Hospital Discharge Register Data on Coronary Heart Disease in Finland”. European Journal of Epidemiology. 1997;13(4):403–15. doi: 10.1023/a:1007306110822. [DOI] [PubMed] [Google Scholar]
- Mascioli SR, Jacobs DR, Jr, Kottke TE. “Diagnostic Criteria for Hospitalized Acute Myocardial Infarction: The Minnesota Experience”. International Journal of Epidemiology. 1989;18(1):76–83. doi: 10.1093/ije/18.1.76. [DOI] [PubMed] [Google Scholar]
- Mauri L, Silbaugh TS, Wolf RE, Zelevinsky K, Lovett A, Zhou Z, Resnic FS, Normand SL. “Long-Term Clinical Outcomes after Drug-Eluting and Bare-Metal Stenting in Massachusetts”. Circulation. 2008;118(18):1817–27. doi: 10.1161/CIRCULATIONAHA.108.781377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzini MJ, Stevens GR, Whalen D, Ozonoff A, Balady GJ. “Effect of an American Heart Association Get with the Guidelines Program-Based Clinical Pathway on Referral and Enrollment into Cardiac Rehabilitation after Acute Myocardial Infarction”. American Journal of Cardiology. 2008;101(8):1084–7. doi: 10.1016/j.amjcard.2007.11.063. [DOI] [PubMed] [Google Scholar]
- McAlister FA, Quan H, Fong A, Jin Y, Cujec B, Johnson D. “Effect of Invasive Coronary Revascularization in Acute Myocardial Infarction on Subsequent Death Rate and Frequency of Chronic Heart Failure”. American Journal of Cardiology. 2008;102(1):1–5. doi: 10.1016/j.amjcard.2008.02.089. [DOI] [PubMed] [Google Scholar]
- McAlpine R, Pringle S, Pringle T, Lorimer R, MacDonald TM. “A Study to Determine the Sensitivity and Specificity of Hospital Discharge Diagnosis Data Used in the MICA Study”. Pharmacoepidemiology and Drug Safety. 1998;7(5):311–8. doi: 10.1002/(SICI)1099-1557(199809/10)7:5<311::AID-PDS371>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- McNamara RL, Herrin J, Wang Y, Curtis JP, Bradley EH, Magid DJ, Rathore SS, Nallamothu BK, Peterson ED, Blaney ME, Frederick P, Krumholz HM. “Impact of Delay in Door-to-Needle Time on Mortality in Patients with ST-Segment Elevation Myocardial Infarction”. American Journal of Cardiology. 2007;100(8):1227–32. doi: 10.1016/j.amjcard.2007.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta RH, Liang L, Karve AM, Hernandez AF, Rumsfeld JS, Fonarow GC, Peterson ED. “Association of Patient Case-Mix Adjustment, Hospital Process Performance Rankings, and Eligibility for Financial Incentives”. Journal of the American Medical Association. 2008;300(16):1897–903. doi: 10.1001/jama.300.16.1897. [DOI] [PubMed] [Google Scholar]
- Mehta JL, Bursac Z, Mehta P, Bansal D, Fink L, Marsh J, Sukhija R, Sachdeva R. “Racial Disparities in Prescriptions for Cardioprotective Drugs and Cardiac Outcomes in Veterans Affairs Hospitals”. American Journal of Cardiology. 2010;105(7):1019–23. doi: 10.1016/j.amjcard.2009.11.031. [DOI] [PubMed] [Google Scholar]
- Merry AH, Boer JM, Schouten LJ, Feskens EJ, Verschuren WM, Gorgels AP, van den Brandt PA. “Validity of Coronary Heart Diseases and Heart Failure Based on Hospital Discharge and Mortality Data in the Netherlands Using the Cardiovascular Registry Maastricht Cohort Study”. European Journal of Epidemiology. 2009;24(5):237–47. doi: 10.1007/s10654-009-9335-x. [DOI] [PubMed] [Google Scholar]
- Movahed MR, Ramaraj R, Hashemzadeh M, Jamal MM. “Rate of Acute ST-Elevation Myocardial Infarction in the United States from 1988 to 2004 (from the Nationwide Inpatient Sample)”. American Journal of Cardiology. 2009;104(1):5–8. doi: 10.1016/j.amjcard.2009.02.058. [DOI] [PubMed] [Google Scholar]
- Nallamothu BK, Wang Y, Cram P, Birkmeyer JD, Ross JS, Normand SL, Krumholz HM. “Acute Myocardial Infarction and Congestive Heart Failure Outcomes at Specialty Cardiac Hospitals”. Circulation. 2007a;116(20):2280–7. doi: 10.1161/CIRCULATIONAHA.107.709220. [DOI] [PubMed] [Google Scholar]
- Nallamothu BK, Young J, Gurm HS, Pickens G, Safavi K. “Recent Trends in Hospital Utilization for Acute Myocardial Infarction and Coronary Revascularization in the United States”. American Journal of Cardiology. 2007b;99(6):749–53. doi: 10.1016/j.amjcard.2006.10.029. [DOI] [PubMed] [Google Scholar]
- Newton KM, Wagner EH, Ramsey SD, McCulloch D, Evans R, Sandhu N, Davis C. “The Use of Automated Data to Identify Complications and Comorbidities of Diabetes: A Validation Study”. Journal of Clinical Epidemiology. 1999;52(3):199–207. doi: 10.1016/s0895-4356(98)00161-9. [DOI] [PubMed] [Google Scholar]
- Nova Scotia-Saskatchewan Cardiovascular Disease Epidemiology Group. “Trends in Incidence and Mortality from Acute Myocardial Infarction in Nova Scotia and Saskatchewan 1974 to 1985. The Nova Scotia-Saskatchewan Cardiovascular Disease Epidemiology Group”. Canadian Journal of Cardiology. 1992;8(3):253–8. [PubMed] [Google Scholar]
- Pajunen P, Koukkunen H, Ketonen M, Jerkkola T, Immonen-Raiha P, Karja-Koskenkari P, Mahonen M, Niemela M, Kuulasmaa K, Palomaki P, Mustonen J, Lehtonen A, Arstila M, Vuorenmaa T, Lehto S, Miettinen H, Torppa J, Tuomilehto J, Kesaniemi YA, Pyorala K, Salomaa V. “The Validity of the Finnish Hospital Discharge Register and Causes of Death Register Data on Coronary Heart Disease”. European Journal of Cardiovascular Prevention and Rehabilitation. 2005;12(2):132–7. doi: 10.1097/00149831-200504000-00007. [DOI] [PubMed] [Google Scholar]
- Palomaki P, Miettinen H, Mustaniemi H, Lehto S, Pyorala K, Mahonen M, Tuomilehto J. “Diagnosis of Acute Myocardial Infarction by MONICA and FINMONICA Diagnostic Criteria in Comparison with Hospital Discharge Diagnosis”. Journal of Clinical Epidemiology. 1994;47(6):659–66. doi: 10.1016/0895-4356(94)90213-5. [DOI] [PubMed] [Google Scholar]
- Pearte CA, Myerson M, Coresh J, McNamara RL, Rosamond W, Taylor H, Manolio TA. “Variation and Temporal Trends in the Use of Diagnostic Testing during Hospitalization for Acute Myocardial Infarction by Age, Gender, Race, and Geography (the Atherosclerosis Risk in Communities Study)”. American Journal of Cardiology. 2008;101(9):1219–25. doi: 10.1016/j.amjcard.2008.01.001. [DOI] [PubMed] [Google Scholar]
- Petersen LA, Wright S, Normand SL, Daley J. “Positive Predictive Value of the Diagnosis of Acute Myocardial Infarction in an Administrative Database”. Journal of General Internal Medicine. 1999;14(9):555–8. doi: 10.1046/j.1525-1497.1999.10198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pladevall M, Goff DC, Nichaman MZ, Chan F, Ramsey D, Ortiz C, Labarthe DR. “An Assessment of the Validity of ICD Code 410 to Identify Hospital Admissions for Myocardial Infarction: The Corpus Christi Heart Project”. International Journal of Epidemiology. 1996;25(5):948–52. doi: 10.1093/ije/25.5.948. [DOI] [PubMed] [Google Scholar]
- Popescu I, Cram P, Vaughan-Sarrazin MS. “Differences in Admitting Hospital Characteristics for Black and White Medicare Beneficiaries with Acute Myocardial Infarction”. Circulation. 2011;123(23):2710–6. doi: 10.1161/CIRCULATIONAHA.110.973628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popescu I, Vaughan-Sarrazin MS, Rosenthal GE. “Differences in Mortality and Use of Revascularization in Black and White Patients with Acute MI Admitted to Hospitals with and without Revascularization Services”. Journal of the American Medical Association. 2007;297(22):2489–95. doi: 10.1001/jama.297.22.2489. [DOI] [PubMed] [Google Scholar]
- Quan H, Li B, Saunders LD, Parsons GA, Nilsson CI, Alibhai A, Ghali WA. “Assessing Validity of ICD-9-CM and ICD-10 Administrative Data in Recording Clinical Conditions in a Unique Dually Coded Database”. Health Services Research. 2008;43(4):1424–41. doi: 10.1111/j.1475-6773.2007.00822.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan H, Khan N, Hemmelgarn BR, Tu K, Chen G, Campbell N, Hill MD, Ghali WA, McAlister FA. “Validation of a Case Definition to Define Hypertension Using Administrative Data”. Hypertension. 2009;54(6):1423–8. doi: 10.1161/HYPERTENSIONAHA.109.139279. [DOI] [PubMed] [Google Scholar]
- Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. “Trends in Incidence, Severity, and Outcome of Hospitalized Myocardial Infarction”. Circulation. 2010;121(7):863–9. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosamond WD, Chambless LE, Sorlie PD, Bell EM, Weitzman S, Smith JC, Folsom AR. “Trends in the Sensitivity, Positive Predictive Value, False-Positive Rate, and Comparability Ratio of Hospital Discharge Diagnosis Codes for Acute Myocardial Infarction in Four US Communities, 1987–2000”. American Journal of Epidemiology. 2004;160(12):1137–46. doi: 10.1093/aje/kwh341. [DOI] [PubMed] [Google Scholar]
- Ross JS, Normand SL, Wang Y, Ko DT, Chen J, Drye EE, Keenan PS, Lichtman JH, Bueno H, Schreiner GC, Krumholz HM. “Hospital Volume and 30-Day Mortality for Three Common Medical Conditions”. New England Journal of Medicine. 2010;362(12):1110–8. doi: 10.1056/NEJMsa0907130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu SY, Park JK, Suh I, Jee SH, Park J, Kim CB, Kim KS. “The Accuracy of Myocardial Infarction Diagnosis in Medical Insurance Claims. Korean Research Group for Cardiovascular Disease Prevention and Control”. Yonsei Medical Journal. 2000;41(5):570–6. doi: 10.3349/ymj.2000.41.5.570. [DOI] [PubMed] [Google Scholar]
- Saia F, Marrozzini C, Ortolani P, Palmerini T, Guastaroba P, Cortesi P, Pavesi PC, Gordini G, Pancaldi LG, Taglieri N, di Pasquale G, Branzi A, Marzocchi A. “Optimisation of Therapeutic Strategies for ST-Segment Elevation Acute Myocardial Infarction: The Impact of a Territorial Network on Reperfusion Therapy and Mortality”. Heart. 2009;95(5):370–6. doi: 10.1136/hrt.2008.146738. [DOI] [PubMed] [Google Scholar]
- Schjerning Olsen AM, Fosbol EL, Lindhardsen J, Folke F, Charlot M, Selmer C, Lamberts M, Bjerring Olesen J, Kober L, Hansen PR, Torp-Pedersen C, Gislason GH. “Duration of Treatment with Nonsteroidal Anti-Inflammatory Drugs and Impact on Risk of Death and Recurrent Myocardial Infarction in Patients with Prior Myocardial Infarction: A Nationwide Cohort Study”. Circulation. 2011;123(20):2226–35. doi: 10.1161/CIRCULATIONAHA.110.004671. [DOI] [PubMed] [Google Scholar]
- Sekhri N, Feder GS, Junghans C, Hemingway H, Timmis AD. “How Effective Are Rapid Access Chest Pain Clinics? Prognosis of Incident Angina and Non-Cardiac Chest Pain in 8762 Consecutive Patients”. Heart. 2007;93(4):458–63. doi: 10.1136/hrt.2006.090894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setoguchi S, Glynn RJ, Avorn J, Levin R, Winkelmayer WC. “Ten-year Trends of Cardiovascular Drug Use after Myocardial Infarction among Community-Dwelling Persons > or =65 Years of Age”. American Journal of Cardiology. 2007;100(7):1061–7. doi: 10.1016/j.amjcard.2007.04.052. [DOI] [PubMed] [Google Scholar]
- Setoguchi S, Glynn RJ, Avorn J, Mittleman MA, Levin R, Winkelmayer WC. “Improvements in Long-Term Mortality after Myocardial Infarction and Increased Use of Cardiovascular Drugs after Discharge: A 10-Year Trend Analysis”. Journal of the American College of Cardiology. 2008a;51(13):1247–54. doi: 10.1016/j.jacc.2007.10.063. [DOI] [PubMed] [Google Scholar]
- Setoguchi S, Solomon DH, Levin R, Winkelmayer WC. “Gender Differences in the Management and Prognosis of Myocardial Infarction among Patients > or = 65 Years of Age”. American Journal of Cardiology. 2008b;101(11):1531–6. doi: 10.1016/j.amjcard.2008.02.033. [DOI] [PubMed] [Google Scholar]
- Shen YC, Hsia RY. “Association between Ambulance Diversion and Survival among Patients with Acute Myocardial Infarction”. Journal of the American Medical Association. 2011;305(23):2440–7. doi: 10.1001/jama.2011.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shreibati JB, Baker LC, Hlatky MA. “Association of Coronary CT Angiography or Stress Testing with Subsequent Utilization and Spending among Medicare Beneficiaries”. Journal of the American Medical Association. 2011;306(19):2128–36. doi: 10.1001/jama.2011.1652. [DOI] [PubMed] [Google Scholar]
- Sorensen R, Hansen ML, Abildstrom SZ, Hvelplund A, Andersson C, Jorgensen C, Madsen JK, Hansen PR, Kober L, Torp-Pedersen C, Gislason GH. “Risk of Bleeding in Patients with Acute Myocardial Infarction Treated with Different Combinations of Aspirin, Clopidogrel, and Vitamin K Antagonists in Denmark: A Retrospective Analysis of Nationwide Registry Data”. Lancet. 2009;374(9706):1967–74. doi: 10.1016/S0140-6736(09)61751-7. [DOI] [PubMed] [Google Scholar]
- Sorensen R, Abildstrom SZ, Hansen PR, Hvelplund A, Andersson C, Charlot M, Fosbol EL, Kober L, Madsen JK, Gislason GH, Torp-Pedersen C. “Efficacy of Post-Operative Clopidogrel Treatment in Patients Revascularized with Coronary Artery Bypass Grafting after Myocardial Infarction”. Journal of the American College of Cardiology. 2011;57(10):1202–9. doi: 10.1016/j.jacc.2010.09.069. [DOI] [PubMed] [Google Scholar]
- Steinberg BA, French WJ, Peterson E, Frederick PD, Cannon CP. “Is Coding for Myocardial Infarction More Accurate Now that Coding Descriptions Have Been Clarified to Distinguish ST-Elevation Myocardial Infarction from Non-ST Elevation Myocardial Infarction?”. American Journal of Cardiology. 2008;102(5):513–7. doi: 10.1016/j.amjcard.2008.04.039. [DOI] [PubMed] [Google Scholar]
- Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. “Use of Cardiac Rehabilitation by Medicare Beneficiaries after Myocardial Infarction or Coronary Bypass Surgery”. Circulation. 2007;116(15):1653–62. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- Taylor GL, Murphy NF, Berry C, Christie J, Finlayson A, MacIntyre K, Morrison C, McMurray J. “Long-Term Outcome of Low-Risk Patients Attending a Rapid-Assessment Chest Pain Clinic”. Heart. 2008;94(5):628–32. doi: 10.1136/hrt.2007.125344. [DOI] [PubMed] [Google Scholar]
- Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, Galvani M, Katus HA, Newby LK, Ravkilde J, Chaitman B, Clemmensen PM, Dellborg M, Hod H, Porela P, Underwood R, Bax JJ, Beller GA, Bonow R, Van der Wall EE, Bassand JP, Wijns W, Ferguson TB, Steg PG, Uretsky BF, Williams DO, Armstrong PW, Antman EM, Fox KA, Hamm CW, Ohman EM, Simoons ML, Poole-Wilson PA, Gurfinkel EP, Lopez-Sendon JL, Pais P, Mendis S, Zhu JR, Wallentin LC, Fernandez-Aviles F, Fox KM, Parkhomenko AN, Priori SG, Tendera M, Voipio-Pulkki LM, Vahanian A, Camm AJ, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Widimsky P, Zamorano JL, Morais J, Brener S, Harrington R, Morrow D, Lim M, Martinez-Rios MA, Steinhubl S, Levine GN, Gibler WB, Goff D, Tubaro M, Dudek D, Al-Attar N. “Universal Definition of Myocardial Infarction”. Circulation. 2007;116(22):2634–53. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]
- Towfighi A, Markovic D, Ovbiagele B. “National Gender-Specific Trends in Myocardial Infarction Hospitalization Rates among Patients Aged 35 to 64 Years”. American Journal of Cardiology. 2011;108(8):1102–7. doi: 10.1016/j.amjcard.2011.05.046. [DOI] [PubMed] [Google Scholar]
- Tu J, Austin P, Naylor C, Iron K, Zhang H. “Acute Myocardial Infarction Outcomes in Ontario”. In: Naylor C, Slaughter P, editors. Cardiovascular Health and Services in Ontario: An ICES Atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. pp. 83–110. [Google Scholar]
- Varas-Lorenzo C, Castellsague J, Stang MR, Tomas L, Aguado J, Perez-Gutthann S. “Positive Predictive Value of ICD-9 Codes 410 and 411 in the Identification of Cases of Acute Coronary Syndromes in the Saskatchewan Hospital Automated Database”. Pharmacoepidemiology and Drug Safety. 2008;17(8):842–52. doi: 10.1002/pds.1619. [DOI] [PubMed] [Google Scholar]
- Volpp KG, Rosen AK, Rosenbaum PR, Romano PS, Even-Shoshan O, Canamucio A, Bellini L, Behringer T, Silber JH. “Mortality among Patients in VA Hospitals in the First 2 Years Following ACGME Resident Duty Hour Reform”. Journal of the American Medical Association. 2007a;298(9):984–92. doi: 10.1001/jama.298.9.984. [DOI] [PubMed] [Google Scholar]
- Volpp KG, Rosen AK, Rosenbaum PR, Romano PS, Even-Shoshan O, Wang Y, Bellini L, Behringer T, Silber JH. “Mortality among Hospitalized Medicare Beneficiaries in the First 2 years Following ACGME Resident Duty Hour Reform”. Journal of the American Medical Association. 2007b;298(9):975–83. doi: 10.1001/jama.298.9.975. [DOI] [PubMed] [Google Scholar]
- Wei L, Lang CC, Sullivan FM, Boyle P, Wang J, Pringle SD, MacDonald TM. “Impact on Mortality Following First Acute Myocardial Infarction of Distance between Home and Hospital: Cohort Study”. Heart. 2008;94(9):1141–6. doi: 10.1136/hrt.2007.123612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. 2010. “International Classification of Diseases (ICD)” [accessed on August 16, 2010]. Available at: http://www.who.int/classifications/icd/en/
- Yeh RW, Go AS. “Rethinking the Epidemiology of Acute Myocardial Infarction: Challenges and Opportunities”. Archives of Internal Medicine. 2010;170(9):759–64. doi: 10.1001/archinternmed.2010.88. [DOI] [PubMed] [Google Scholar]
- Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. “Population Trends in the Incidence and Outcomes of Acute Myocardial Infarction”. New England Journal of Medicine. 2010;362(23):2155–65. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


