Abstract
The obesity epidemic is attributed in part to reduced physical activity. Evidence supports that reducing time spent sitting, regardless of activity, may improve the metabolic consequences of obesity. Analyses were conducted in a large prospective study of US adults enrolled by the American Cancer Society to examine leisure time spent sitting and physical activity in relation to mortality. Time spent sitting and physical activity were queried by questionnaire on 53,440 men and 69,776 women who were disease free at enrollment. The authors identified 11,307 deaths in men and 7,923 deaths in women during the 14-year follow-up. After adjustment for smoking, body mass index, and other factors, time spent sitting (≥6 vs. <3 hours/day) was associated with mortality in both women (relative risk = 1.34, 95% confidence interval (CI): 1.25, 1.44) and men (relative risk = 1.17, 95% CI: 1.11, 1.24). Relative risks for sitting (≥6 hours/day) and physical activity (<24.5 metabolic equivalent (MET)-hours/week) combined were 1.94 (95% CI: 1.70, 2.20) for women and 1.48 (95% CI: 1.33, 1.65) for men, compared with those with the least time sitting and most activity. Associations were strongest for cardiovascular disease mortality. The time spent sitting was independently associated with total mortality, regardless of physical activity level. Public health messages should include both being physically active and reducing time spent sitting.
Keywords: mortality, motor activity, prospective studies, sedentary lifestyle
It is now well established that the US obesity epidemic will have major public health consequences. This epidemic is attributed, at least in part, to reduced overall physical activity expenditure. It has long been recognized that physical activity has a beneficial impact on the incidence and mortality of many chronic diseases, including cardiovascular disease, diabetes, stroke, and various types of cancer including colon and postmenopausal breast cancer (1–5). Dose-response relations between physical activity and improved health outcomes have been reported, and substantial evidence supports health benefits even with physical activity below recommended levels (1, 3, 6, 7).
There is a growing body of evidence showing that reducing the amount of time spent sitting, regardless of the amount of physical activity, may improve the metabolic consequences of obesity (8–11). However, current public health guidelines focus largely on increasing physical activity with little or no reference to reducing time spent sitting (12–15). Numerous studies support an association with sitting time and endpoints such as obesity, type 2 diabetes, cardiovascular disease (11, 16, 17), and unhealthy dietary patterns in children and adults (18–20). However, to our knowledge, few studies have examined time spent sitting in relation to total mortality (21–23), but they were limited by sample size (21, 22) or qualitatively assessed time spent sitting (21).
To better assess the relation between time spent sitting and total mortality, both independent of and in combination with physical activity, we conducted a detailed analysis in the American Cancer Society's Cancer Prevention Study II (CPS-II) Nutrition Cohort. This cohort has the advantage of being very large with approximately 184,000 US adults and over 19,000 deaths for whom detailed information on time spent sitting and physical activity was collected at baseline.
MATERIALS AND METHODS
Study population
Men and women in this analysis were drawn from the 184,190 participants in the CPS-II Nutrition Cohort (hereafter referred to as the “Nutrition Cohort”), a prospective study of cancer incidence and mortality begun by the American Cancer Society in 1992 (24). The Nutrition Cohort is a subgroup of approximately 1.2 million participants in the baseline CPS-II cohort, a prospective mortality study established by the American Cancer Society in 1982 (25). Members of the CPS-II cohort who resided in 21 states with population-based state cancer registries and were 50–74 years of age in 1992 were invited to participate by completing a mailed questionnaire. The 10-page mailed questionnaire included questions on demographic, reproductive, medical, behavioral, and lifestyle factors. The recruitment and characteristics of the Nutrition Cohort are described in detail elsewhere (24).
We excluded sequentially from this analysis men and women who reported a personal history of cancer (n = 21,785), heart attack (n = 11,560), stroke (n = 2,513), or emphysema/other lung disease (n = 9,321) at the time of enrollment. We also excluded individuals with missing data on physical activity (n = 4,240), missing sitting time (n = 2,954), missing or extreme (top and bottom 0.1%) values of body mass index (n = 2,121), or missing smoking status (n = 1,347) at baseline. Finally, to reduce the possibility of undiagnosed serious illness at baseline that would preclude or interfere with physical activity, we excluded individuals who reported both no daily life activities and no light housekeeping (n = 4,730), as well as those who died from any cause within the first year of follow-up (n = 403). After exclusions, the analytical cohort consisted of 123,216 individuals (53,440 men and 69,776 women) with a mean age of 63.6 (standard deviation, 6.0) years in men and 61.9 (standard deviation, 6.5) years in women when enrolled in the study in 1992.
Mortality endpoints
The primary endpoint was death from any cause occurring between 1 year after the time of enrollment and December 31, 2006. Deaths were identified through biennial automated linkage of the entire cohort with the National Death Index (26). Death certificates or codes for cause of death have been obtained for 98.7% of all known deaths. Causes of death were classified by using the International Classification of Diseases (ICD), Ninth Revision (27), for deaths occurring from 1992 to 1998 and the Tenth Revision (28) for deaths from 1999 to 2006. Specific causes of death were grouped into 3 broad categories: cardiovascular disease (ICD, Ninth Revision, codes 390–459 and ICD, Tenth Revision, codes I00–I99); cancer (ICD, Ninth Revision, codes 140–195 and 199–208 and ICD, Tenth Revision, codes C00–C76 and C80–C97); and all other causes.
Measures of time spent sitting and physical activity
Time spent sitting was assessed by using the question, “During the past year, on an average day (not counting time spent at your job), how many hours per day did you spend sitting (watching television, reading, etc.)?” Responses included “none, <3, 3–5, 6–8, >8 hours per day.” Time spent sitting was categorized as 0–<3, 3–5, or ≥6 hours/day.
Information on recreational physical activity was collected by using the question, “During the past year, what was the average time per week you spent at the following kinds of activities: walking, jogging/running, lap swimming, tennis or racquetball, bicycling or stationary biking, aerobics/calisthenics, and dancing?” Responses to each individual activity included “none,” “1–3 hours/week,” “4–6 hours/week,” or “≥7 hours/week.” The summary metabolic equivalent of energy expenditure (MET)-hours/week was calculated for each participant. A MET is estimated by dividing the energy cost of a given activity by resting energy expenditure (29). The summary MET score for each participant was calculated by multiplying the lowest number of hours within each category by the general MET level of each activity according to the Compendium of Physical Activities (29) to provide conservatively estimated summary measures because of the likelihood of overreporting physical activity and the older age of study participants. MET scores assigned for various activities include the following: 3.5 for walking, 7.0 for jogging/running, 7.0 for lap swimming, 6.0 for tennis or racquetball, 4.0 for bicycling/stationary biking, 4.5 for aerobics/calisthenics, and 3.5 for dancing.
We also assessed daily life physical activities with the question, “During the past year, what was the average time per week you spent at the following kinds of activities: gardening/mowing/planting, heavy housework/vacuuming, heavy home repair/painting, and shopping?” We calculated MET-hours/week from these activities using the following values (29): 3.0 for gardening/mowing/planting, 2.5 for heavy housework/vacuuming, 3.0 for heavy home repair/painting, and 2.5 for shopping.
The primary purpose in this analysis was to examine the relation of leisure-time sitting to all-cause death rates. Therefore, we combined recreational and daily life activity into total leisure-time physical activity at baseline, because the relation between regular physical activity and all-cause mortality has been well documented. Total leisure-time activity was categorized in MET-hours/week as <17.5, 17.5–<24.5, 24.5–<31.5, 31.5–<42.0, 42.0–<52.5, 52.5–<63.0, or ≥63.0. The lowest cutpoint corresponds with approximately the 10th percentile of activity level in our population, and each subsequent category increases by the metabolic equivalent of approximately 3 hours of light-intensity daily life activities per week.
Statistical analysis
Cox proportional hazards modeling (30) was used to compute relative risk, with follow-up time in days as the time axis. All Cox models were stratified on exact year of age. For each exposure variable, we assessed risk in 3 models: 1) adjusted only for age, 2) adjusted for age and other potential confounding factors, and 3) mutually adjusting for both physical activity and time spent sitting in addition to all potential confounders. The potential confounders included were race (white, black, other), smoking status (never, current, former), duration (≤35, >35 years) and frequency (<20, ≥20 cigarettes/day) of smoking among current smokers, years since quitting among former smokers (≤5, 6–10, 11–15, 16–20, 21–25, >25 years), body mass index (weight (kg)/height (m)2) (<18.5, 18.5–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9, ≥30.0), marital status (married, widowed, divorced, separated, never married), education (less than high school, high school graduate, some college, college graduate, graduate school or higher), alcohol consumption (0, <1, 1, >1 drink/day), total caloric intake (quartiles), and comorbidity score (0, 1, ≥2). Dietary intake was assessed by using a 68-item modified brief food frequency questionnaire by Block et al. (31) and validated in a subset of cohort members (32). The comorbidities score included high blood pressure, diabetes, and high cholesterol. Other potential confounders assessed were fruit and vegetable intake, fat intake, red meat intake, and occupational status (employed, retired, homemaker), but these factors were not included in the model as they had no impact on any risk estimates for physical activity or time spent sitting.
Tests of linear trend for sitting time and physical activity measures were calculated by assigning the median value within each category to that category. We also examined the combined effects of physical activity and time spent sitting. For these models, the number of categories of total daily physical activity was reduced from 7 to 5 (<24.5, 24.5–<31.5, 31.5–<42.0, 42.0–<52.5, ≥52.5 MET-hours/week). Men and women who were most physically active and spent the least time sitting (≥52.5 MET-hours/week and <3 hours/day sitting) served as the referent group.
Secondary analyses also examined the associations between body mass index and mortality from all cardiovascular diseases, all cancers, and all other causes of death among men and women separately. We also tested for effect modification by gender, body mass index, smoking status, attained age, and follow-up time. Because there was no statistically significant effect modification by gender, all other factors were tested for effect modification in both sexes combined to maximize statistical power.
We also conducted a sensitivity analysis to further examine whether the amount of time spent sitting at baseline was a result of undiagnosed illness that was not accounted for through exclusions for prevalent disease or excluding the first year of follow-up. Using data on physical activity and time spent sitting in 1992, as well as our first follow-up survey in 1997, we examined long-term (5-year) sitting time and physical activity in relation to subsequent mortality rates. Finally, we conducted a sensitivity analysis among men and women who were either retired or homemakers to eliminate the potential impact of occupational time spent sitting or in physical activity.
RESULTS
We observed 11,307 deaths in men and 7,923 in women over the 1,610,728 person-years of follow-up. Men and women who spent the least leisure time sitting were leaner, more likely to have never smoked cigarettes, more likely to be employed, and had lower total energy intake (Table 1). Leisure time spent sitting was not associated with physical activity (r = −0.03). Study participants generally engaged in light- to moderate-intensity activities, such as walking for exercise, gardening, shopping, and housework. Moderate- to vigorous-intensity activities were relatively uncommon in this older population; 83% of men and 87% of women reported walking for exercise, and 37% of men and 36% of women listed walking as their only form of recreational physical activity.
Table 1.
Age-adjusted Percentages and Means of Selected Baseline Characteristics in 1992, by Hours of Leisure Time Spent Sitting for Women and Men, Cancer Prevention Study II Nutrition Cohort
| Sitting in 1992 |
||||||||||||
| Women |
Men |
|||||||||||
| <3 hours/day (n = 34,075) |
3–5 hours/day (n = 29,335) |
≥6 hours/day (n = 6,366) |
<3 hours/day (n = 22,876) |
3–5 hours/day (n = 23,723) |
≥6 hours/day (n = 6,841) |
|||||||
| Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | |
| Age at baseline, years | 60.7 (0.04) | 62.8 (0.04) | 63.4 (0.08) | 62.6 (0.04) | 64.1 (0.04) | 64.8 (0.07) | ||||||
| Body mass index in 1992, kg/m2 | 24.9 (0.02) | 25.9 (0.03) | 26.8 (0.06) | 26.1 (0.02) | 26.6 (0.02) | 27.0 (0.04) | ||||||
| Total MET-hours/week | 42.8 (0.12) | 40.7 (0.13) | 39.9 (0.29) | 46.1 (0.16) | 44.4 (0.16) | 44.5 (0.29) | ||||||
| Retired/homemaker | 61.6 | 69.9 | 73.1 | 50.0 | 61.0 | 64.7 | ||||||
| Race | ||||||||||||
| White | 97.4 | 97.4 | 96.9 | 97.3 | 97.4 | 97.5 | ||||||
| Black | 1.4 | 1.5 | 1.6 | 1.2 | 1.3 | 1.2 | ||||||
| Other | 1.2 | 1.1 | 1.5 | 1.4 | 1.4 | 1.3 | ||||||
| Educational level | ||||||||||||
| Less than high school | 4.7 | 4.7 | 5.5 | 7.8 | 7.2 | 7.2 | ||||||
| High school graduate | 30.5 | 33.9 | 33.0 | 18.8 | 19.5 | 16.9 | ||||||
| Some college | 31.1 | 31.3 | 31.1 | 24.3 | 27.3 | 25.1 | ||||||
| College graduate | 19.9 | 18.2 | 17.3 | 22.2 | 21.7 | 22.5 | ||||||
| Graduate school | 13.2 | 11.2 | 12.3 | 26.3 | 23.7 | 27.8 | ||||||
| Smoking status | ||||||||||||
| Never | 60.1 | 53.8 | 48.7 | 39.5 | 31.7 | 30.8 | ||||||
| Current | 6.7 | 9.9 | 13.4 | 7.1 | 9.7 | 12.7 | ||||||
| Former | 32.4 | 35.7 | 37.0 | 52.1 | 57.4 | 55.1 | ||||||
| Alcohol use | ||||||||||||
| Never | 45.3 | 44.5 | 47.7 | 32.5 | 31.3 | 31.8 | ||||||
| <1 drink/day | 38.8 | 39.2 | 35.2 | 39.2 | 39.5 | 38.1 | ||||||
| 1 drink/day | 7.7 | 7.9 | 7.4 | 12.9 | 13.1 | 12.1 | ||||||
| >1 drink/day | 4.3 | 5.0 | 5.7 | 11.3 | 12.9 | 14.4 | ||||||
| Caloric intake, kcal/day | 1,326.69 (2.7) | 1,383.78 (2.9) | 1,455.24 (6.2) | 1,770.64 (4.3) | 1,839.98 (4.1) | 1,923.58 (7.8) | ||||||
Abbreviations: MET, metabolic equivalent; SE, standard error.
Associations of leisure time spent sitting, physical activity, and their combined effects with mortality are shown in Table 2. After multivariate adjustment, leisure time spent sitting was positively associated with all-cause mortality rates in both women and men; however, associations appeared stronger in women (for ≥6 vs. <3 hours/day, relative risk = 1.37, 95% confidence interval (CI): 1.27, 1.47) than men (relative risk = 1.18, 95% CI: 1.12, 1.25) (Pheterogeneity = 0.003). After further adjustment for physical activity, these associations remained virtually unchanged. There was a dose-related, inverse relation between physical activity and mortality rates in women and in men beginning at relatively low levels of activity (Table 2). Risk estimates for physical activity similarly were virtually unchanged after further adjustment for time spent sitting.
Table 2.
Relative Risk of Death From All Causes According to Leisure Time Sitting and Physical Activity Among Women and Men, Cancer Prevention Study II Nutrition Cohort, 1993–2006
| Women |
Men |
|||||||||||
| No. of Deaths | Person-Years | Relative Riska | 95% CI | Relative Riskb | 95% CI | No. of Deaths | Person-Years | Relative Riska | 95% CI | Relative Riskb | 95% CI | |
| Sitting in 1992, hours/day | ||||||||||||
| 0–<3 | 3,038 | 456,987 | 1.00 | Referent | 1.00 | Referent | 4,030 | 298,227 | 1.00 | Referent | 1.00 | Referent |
| 3–5 | 3,781 | 386,736 | 1.14 | 1.08, 1.19 | 1.13 | 1.07, 1.18 | 5,413 | 301,973 | 1.08 | 1.03, 1.12 | 1.07 | 1.03, 1.12 |
| ≥6 | 1,104 | 81,963 | 1.37 | 1.27, 1.47 | 1.34 | 1.25, 1.44 | 1,864 | 84,842 | 1.18 | 1.12, 1.25 | 1.17 | 1.11, 1.24 |
| Ptrend | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||||||||
| Total physical activity in 1992, MET-hours/week | ||||||||||||
| <17.5 | 1,157 | 107,418 | 1.00 | Referent | 1.00 | Referent | 1,186 | 63,336 | 1.00 | Referent | 1.00 | Referent |
| 17.5–<24.5 | 699 | 63,751 | 0.98 | 0.89, 1.07 | 0.98 | 0.89, 1.07 | 991 | 59,365 | 0.89 | 0.82, 0.97 | 0.90 | 0.82, 0.97 |
| 24.5–<31.5 | 1,382 | 159,718 | 0.81 | 0.75, 0.88 | 0.82 | 0.75, 0.88 | 1,397 | 86,898 | 0.84 | 0.78, 0.91 | 0.85 | 0.78, 0.92 |
| 31.5–<42 | 1,588 | 195,423 | 0.78 | 0.72, 0.84 | 0.78 | 0.73, 0.85 | 2,284 | 133,341 | 0.88 | 0.82, 0.94 | 0.88 | 0.82, 0.95 |
| 42–<52.5 | 1,255 | 157,978 | 0.76 | 0.70, 0.82 | 0.76 | 0.70, 0.83 | 1,857 | 115,894 | 0.81 | 0.75, 0.87 | 0.81 | 0.75, 0.87 |
| 52.5–<63 | 772 | 99,477 | 0.75 | 0.68, 0.82 | 0.76 | 0.69, 0.83 | 1,453 | 88,468 | 0.79 | 0.73, 0.85 | 0.79 | 0.74, 0.86 |
| ≥63 | 1,070 | 141,921 | 0.73 | 0.67, 0.80 | 0.74 | 0.68, 0.81 | 2,139 | 137,740 | 0.79 | 0.74, 0.85 | 0.80 | 0.74, 0.86 |
| Ptrend | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||||||||
| Physical activity, MET-hours/week, and sitting, sitting-hours/day, in 1992 | ||||||||||||
| ≥52.5, <3 | 788 | 126,961 | 1.00 | Referent | 1,401 | 100,780 | 1.00 | Referent | ||||
| ≥52.5, 3–5 | 831 | 94,582 | 1.12 | 1.02, 1.24 | 1,640 | 96,805 | 1.02 | 0.95, 1.09 | ||||
| ≥52.5, ≥6 | 223 | 19,854 | 1.25 | 1.07, 1.45 | 551 | 26,623 | 1.07 | 0.97, 1.18 | ||||
| 42–<52.5, <3 | 490 | 77,704 | 1.01 | 0.90, 1.13 | 656 | 50,122 | 0.98 | 0.89, 1.07 | ||||
| 42–<52.5, 3–5 | 596 | 66,885 | 1.14 | 1.03, 1.27 | 903 | 52,499 | 1.04 | 0.95, 1.13 | ||||
| 42–<52.5, ≥6 | 169 | 13,389 | 1.31 | 1.10, 1.54 | 298 | 13,274 | 1.20 | 1.06, 1.36 | ||||
| 31.5–<42, <3 | 603 | 96,191 | 1.00 | 0.90, 1.11 | 806 | 57,814 | 1.08 | 0.99, 1.18 | ||||
| 31.5–<42, 3–5 | 797 | 83,531 | 1.20 | 1.09, 1.33 | 1,131 | 59,678 | 1.13 | 1.05, 1.23 | ||||
| 31.5–<42, ≥6 | 188 | 15,701 | 1.35 | 1.15, 1.58 | 347 | 15,849 | 1.23 | 1.09, 1.38 | ||||
| 24.5–<31.5, <3 | 525 | 76,992 | 1.10 | 0.98, 1.23 | 467 | 38,048 | 0.96 | 0.86, 1.06 | ||||
| 24.5–<31.5, 3–5 | 682 | 68,555 | 1.20 | 1.09, 1.34 | 699 | 37,945 | 1.18 | 1.07, 1.29 | ||||
| 24.5–<31.5, ≥6 | 175 | 14,171 | 1.39 | 1.18, 1.64 | 231 | 10,905 | 1.13 | 0.99, 1.31 | ||||
| <24.5, <3 | 632 | 79,138 | 1.30 | 1.17, 1.44 | 700 | 51,464 | 1.09 | 0.99, 1.19 | ||||
| <24.5, 3–5 | 875 | 73,184 | 1.42 | 1.29, 1.57 | 1,040 | 55,045 | 1.23 | 1.13, 1.33 | ||||
| <24.5, ≥6 | 349 | 18,847 | 1.94 | 1.70, 2.20 | 437 | 16,192 | 1.48 | 1.33, 1.65 | ||||
Abbreviations: CI, confidence interval; MET, metabolic equivalent.
Adjusted for age at interview, race, marital status, education, smoking status, body mass index in 1992, alcohol use, total caloric intake, and comorbidities score.
Adjusted for all of the above plus total physical activity (for sitting) and hours sitting (for total physical activity).
When examining the combined effects of time spent sitting and physical activity on all-cause death rates, time spent sitting was associated with increased risk regardless of level of physical activity (Figures 1 and 2). The relative risks for the joint effects of sitting and physical activity (≥6 hours/day sitting and <24.5 MET-hours/week activity) were 1.94 (95% CI: 1.70, 2.20) and 1.48 (95% CI: 1.33, 1.65), for women and men respectively, compared with women and men who reported both sitting the least (<3 hours/day) and being the most physically active (≥52.5 MET-hours/week).
Figure 1.
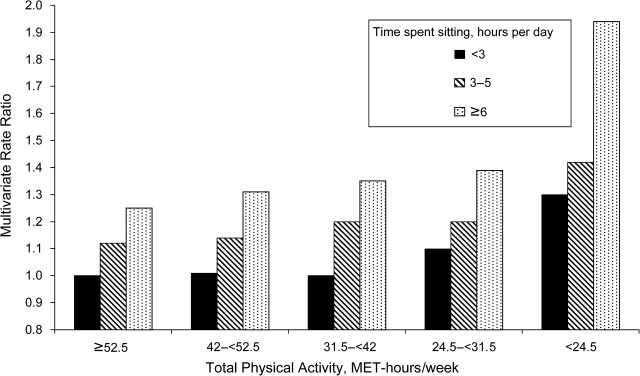
Combined multivariate-adjusted rate ratios (P < 0.05) for leisure time spent sitting and physical activity in relation to all-cause mortality, women only, in the Cancer Prevention Study II Nutrition Cohort, 1993–2006. MET, metabolic equivalent.
Figure 2.
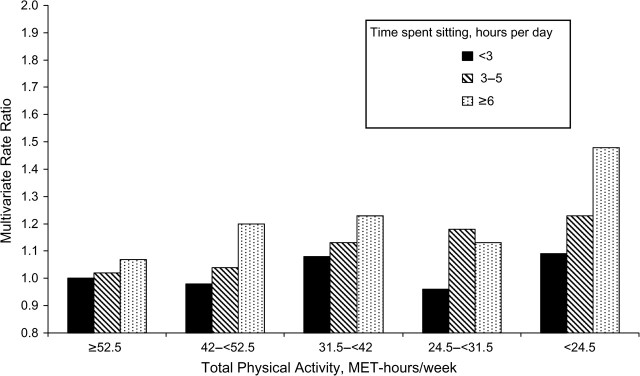
Combined multivariate-adjusted rate ratios (P < 0.05) for leisure time spent sitting and physical activity in relation to all-cause mortality, men only, in the Cancer Prevention Study II Nutrition Cohort, 1993–2006. MET, metabolic equivalent.
We examined the association between time spent sitting and total mortality in men and women combined, stratified by body mass index (Table 3). Although time spent sitting and physical activity were more strongly associated with mortality among lean persons (for time spent sitting, Pinteraction = 0.06; for physical activity, Pinteraction = 0.002), both measures were significantly associated with risk of total mortality regardless of body mass index. No other factors examined, including smoking status or attained age, appeared to modify the associations between time spent sitting and physical activity in relation to total mortality (data not shown). Results from the sensitivity analysis among participants who are retired or homemakers also did not differ from those in the overall cohort (data not shown).
Table 3.
Relative Risk of Death From All Causes According to Leisure Time Spent Sitting and Physical Activity, Stratified by Body Mass Index, Among Women and Men, Cancer Prevention Study II Nutrition Cohort, 1993–2006
| Body Mass Index, kg/m2 |
|||||||||
| <25.0 |
25.0–<30.0 |
≥30.0 |
|||||||
| No. of Deaths | Relative Riska | 95% CI | No. of Deaths | Relative Riska | 95% CI | No. of Deaths | Relative Riska | 95% CI | |
| Sitting in 1992, hours/day | |||||||||
| 0–<3 | 3,278 | 1.00 | Referent | 2,768 | 1.00 | Referent | 1,022 | 1.00 | Referent |
| 3–5 | 3,768 | 1.10 | 1.05, 1.15 | 3,852 | 1.11 | 1.05, 1.16 | 1,574 | 1.05 | 0.97, 1.14 |
| ≥6 | 1,119 | 1.28 | 1.20, 1.37 | 1,220 | 1.21 | 1.12, 1.29 | 629 | 1.19 | 1.08, 1.32 |
| Ptrend | <0.0001 | <0.0001 | 0.001 | ||||||
| Pinteraction = 0.06 | |||||||||
| Total physical activity in 1992, MET-hours/week | |||||||||
| <17.5 | 866 | 1.00 | Referent | 935 | 1.00 | Referent | 542 | 1.00 | Referent |
| 17.5–<24.5 | 669 | 0.94 | 0.85, 1.04 | 668 | 0.90 | 0.81, 0.99 | 353 | 0.94 | 0.82, 1.08 |
| 24.5–<31.5 | 1,202 | 0.86 | 0.79, 0.94 | 1,054 | 0.79 | 0.72, 0.86 | 523 | 0.86 | 0.76, 0.97 |
| 31.5–<42 | 1,605 | 0.80 | 0.73, 0.87 | 1,622 | 0.86 | 0.80, 0.94 | 645 | 0.86 | 0.76, 0.96 |
| 42–<52.5 | 1,380 | 0.77 | 0.70, 0.83 | 1,250 | 0.78 | 0.72, 0.85 | 482 | 0.86 | 0.76, 0.98 |
| 52.5–<63 | 996 | 0.76 | 0.69, 0.83 | 937 | 0.79 | 0.72, 0.87 | 292 | 0.79 | 0.69, 0.92 |
| ≥63 | 1,447 | 0.72 | 0.66, 0.79 | 1,374 | 0.82 | 0.76, 0.89 | 388 | 0.78 | 0.69, 0.89 |
| Ptrend | <0.0001 | 0.0003 | 0.0001 | ||||||
| Pinteraction = 0.002 | |||||||||
Abbreviations: CI, confidence interval; MET, metabolic equivalent.
Adjusted for age at interview, race, marital status, education, smoking status, body mass index in 1992, alcohol use, total caloric intake, comorbidities score, and total physical activity (for sitting) and hours sitting (for total physical activity).
Although we excluded the first year of follow-up and prevalent disease, we further examined whether observed associations were a result of unidentified prevalent illness in 2 ways. First, we examined the associations between baseline exposures stratified by follow-up time. Although associations were slightly attenuated, they persisted and remained statistically significant over the 14-year follow-up (data not shown). Second, we conducted a sensitivity analysis combining questions about sitting time and physical activity at baseline with those from our first follow-up survey in 1997 to examine sustained (5-year) measures. Results from these analyses did not differ from those presented for baseline alone (data not shown).
Associations between time spent sitting and physical activity were stronger for cardiovascular disease mortality than for cancer (Table 4). Time spent sitting was associated with an increased risk of cardiovascular disease mortality in both men and women, whereas it was associated with increased cancer mortality only among women. There was a statistically significant inverse relation between physical activity and cardiovascular disease mortality beginning at relatively low levels of activity in both men (Ptrend = 0.0001) and women (Ptrend < 0.0001). In contrast, total physical activity was not significantly associated with lower cancer mortality among men and only modestly associated with lower cancer mortality in women. Longer time spent sitting was associated with higher death rates from all other causes, and physical activity was inversely associated with death rates from other causes. The most common conditions in this category were respiratory diseases (22.7% in men, 20.4% in women), central nervous system diseases (20.3% in men, 19.8% in women), digestive diseases (9.6% in men, 10.4% in women), and diabetes (7.8% in men, 6.3% in women).
Table 4.
Relative Risk of Death From Cardiovascular Disease, Cancer, and All Other Causes According to Leisure Time Spent Sitting and Physical Activity Among Women and Men, Cancer Prevention Study II Nutrition Cohort, 1993–2006
| Cardiovascular Disease |
Cancer |
Other Causes |
|||||||
| No. of Deaths | Relative Riska | 95% CI | No. of Deaths | Relative Riska | 95% CI | No. of Deaths | Relative Riska | 95% CI | |
| Women | |||||||||
| Sitting in 1992, hours/day | |||||||||
| 0–<3 | 833 | 1.00 | Referent | 1,284 | 1.00 | Referent | 921 | 1.00 | Referent |
| 3–5 | 1,196 | 1.20 | 1.10, 1.32 | 1,413 | 1.07 | 0.99, 1.16 | 1,172 | 1.13 | 1.04, 1.24 |
| ≥6 | 331 | 1.33 | 1.17, 1.52 | 411 | 1.30 | 1.16, 1.46 | 362 | 1.41 | 1.25, 1.60 |
| Ptrend | <0.0001 | <0.0001 | <0.0001 | ||||||
| Total physical activity in 1992, MET-hours/week | |||||||||
| <17.5 | 370 | 1.00 | Referent | 413 | 1.00 | Referent | 374 | 1.00 | Referent |
| 17.5–<24.5 | 224 | 0.98 | 0.83, 1.15 | 260 | 1.02 | 0.88, 1.20 | 215 | 0.93 | 0.78, 1.10 |
| 24.5–<31.5 | 400 | 0.74 | 0.64, 0.86 | 536 | 0.88 | 0.78, 1.00 | 446 | 0.82 | 0.71, 0.94 |
| 31.5–<42 | 484 | 0.76 | 0.67, 0.87 | 608 | 0.82 | 0.73, 0.94 | 496 | 0.76 | 0.67, 0.87 |
| 42–<52.5 | 369 | 0.72 | 0.62, 0.84 | 499 | 0.83 | 0.73, 0.95 | 387 | 0.74 | 0.64, 0.85 |
| 52.5–<63 | 224 | 0.71 | 0.60, 0.84 | 328 | 0.87 | 0.75, 1.01 | 220 | 0.68 | 0.57, 0.80 |
| ≥63 | 289 | 0.66 | 0.56, 0.77 | 464 | 0.86 | 0.75, 0.99 | 317 | 0.69 | 0.59, 0.80 |
| Ptrend | <0.0001 | 0.03 | <0.0001 | ||||||
| Men | |||||||||
| Sitting in 1992, hours/day | |||||||||
| 0–<3 | 1,413 | 1.00 | Referent | 1,457 | 1.00 | Referent | 1,160 | 1.00 | Referent |
| 3–5 | 1,911 | 1.06 | 0.99, 1.14 | 1,853 | 1.05 | 0.98, 1.12 | 1,649 | 1.13 | 1.04, 1.22 |
| ≥6 | 685 | 1.18 | 1.08, 1.30 | 571 | 1.04 | 0.94, 1.15 | 608 | 1.33 | 1.20, 1.47 |
| Ptrend | 0.0007 | 0.29 | <0.0001 | ||||||
| Total physical activity in 1992, MET-hours/week | |||||||||
| <17.5 | 435 | 1.00 | Referent | 379 | 1.00 | Referent | 372 | 1.00 | Referent |
| 17.5–<24.5 | 353 | 0.87 | 0.75, 1.00 | 314 | 0.91 | 0.78, 1.06 | 324 | 0.92 | 0.79, 1.07 |
| 24.5–<31.5 | 496 | 0.81 | 0.71, 0.92 | 488 | 0.96 | 0.84, 1.10 | 413 | 0.77 | 0.67, 0.89 |
| 31.5–<42 | 818 | 0.86 | 0.77, 0.97 | 781 | 0.98 | 0.87, 1.11 | 685 | 0.81 | 0.71, 0.92 |
| 42–<52.5 | 638 | 0.76 | 0.68, 0.86 | 636 | 0.91 | 0.80, 1.03 | 583 | 0.77 | 0.67, 0.87 |
| 52.5–<63 | 516 | 0.78 | 0.68, 0.88 | 511 | 0.92 | 0.81, 1.05 | 426 | 0.70 | 0.61, 0.80 |
| ≥63 | 753 | 0.77 | 0.68, 0.87 | 772 | 0.95 | 0.84, 1.07 | 614 | 0.68 | 0.60, 0.78 |
| Ptrend | 0.0001 | 0.52 | <0.0001 | ||||||
Abbreviations: CI, confidence interval; MET, metabolic equivalent.
Adjusted for age at interview, race, marital status, education, smoking status, body mass index in 1992, alcohol use, total caloric intake, comorbidities score, and total physical activity (for sitting) and hours sitting (for total physical activity).
DISCUSSION
In this large prospective cohort, women who reported sitting for more than 6 hours during their leisure time versus less than 3 hours a day had an approximately 40% higher all-cause death rate, and men had an approximately 20% higher death rate. This association was independent of the amount of physical activity. The combination of both sitting more and being less physically active (>6 hours/day sitting and <24.5 MET-hours/week physical activity) was associated with a 94% and a 48% increase in all-cause death rates in women and men, respectively, compared with those who reported sitting the least and being most active (<3 hours/day sitting and ≥52 MET-hours/week physical activity).
Our findings for time spent sitting are consistent with those from the 3 other studies that have previously examined the association between time spent sitting and mortality (21–23). One study included approximately 17,000 Canadian adults with 1,832 deaths, and the authors reported a significant dose-response relation between a qualitative measure of time spent sitting (almost none of the time, one fourth of the time, half of the time, three fourths of the time, almost all of the time) and total mortality (21). The second study, which included 8,800 Australian adults and 284 deaths, found an almost 50% increase in total mortality with 4 or more hours of television viewing compared with less than 2 hours per day (22). In both of these studies, associations were strongest for cardiovascular disease mortality (21, 22). The third study included approximately 83,000 Japanese adults and reported a positive association with sedentary behavior and total mortality among men, but not women (23).
Our physical activity findings were similar to those reported from the majority of other studies (1, 2, 33). Mortality rates were approximately 25% lower among men and women who reported the most versus the least daily physical activity. Although optimal health benefits are achieved at a much higher level of physical activity, death rates were substantially lower even in the second lowest category compared with the lowest category, suggesting a benefit from even relatively light levels of physical activity. As mentioned, the participants in our study were older and engaged in primarily light-intensity activities, such as walking for exercise and gardening. It should be noted that no previous study has examined the combined effects of sitting time and physical activity.
Several factors could explain the positive association between time spent sitting and higher all-cause death rates. First, time spent sitting might be more easily measured than physical activity and/or may reflect a different aspect of inactivity than other indices usually used in epidemiologic studies. However, this potential misclassification of exposure is unlikely to fully explain our findings, because time spent sitting was significantly associated with mortality even among men and women with the highest levels of physical activity.
Second, time spent sitting might be associated with other unhealthy behaviors that are either not captured or incompletely captured through questionnaires. Total energy expenditure is reduced among individuals who are sedentary. However, consistent with previous studies, the present study found no correlation between physical activity and time spent sitting (r = −0.03). Time spent sitting is also associated with greater food consumption and subsequent weight gain, especially when watching television (16, 34, 35). Time spent sitting was previously shown to be associated with increased weight gain in this cohort (18). While residual confounding by obesity could contribute to the association between sitting time and mortality, this association was attenuated but not eliminated by controlling for or stratifying on body mass index.
Third, prolonged time spent sitting, independent of physical activity, has important metabolic consequences that may influence specific biomarkers (such as triglycerides, high density lipoprotein cholesterol, fasting plasma glucose, resting blood pressure, and leptin) of obesity and cardiovascular and other chronic diseases (8–11). Animal studies have also shown that sedentary time substantially suppresses enzymes centrally involved in lipid metabolism within skeletal muscle, and low levels of daily life activity are sufficient to improve enzyme activity (36–38). Furthermore, substantial evidence in both adults and children from observational studies and randomized clinical trials shows that reducing time spent sitting lowers the risk of obesity and type II diabetes (19, 39–42).
Over the past century, a number of technologic changes have contributed to a decrease in total daily energy expenditure. For example, during the 2006–2007 broadcast year, the average US household reported 8 hours of television watching per day, which is an increase of 1 hour per day of television watching from only a decade ago (43). Although leisure-time physical activity levels have remained relatively constant over the past few decades (44, 45), it is well recognized that technologic advances in the workplace have also greatly reduced occupational physical activity. This reduction in overall physical activity, in conjunction with increased time spent sitting and higher caloric intake, has contributed in large part to the rise in obesity and likely influenced temporal trends in cardiovascular disease, type 2 diabetes, and some cancers.
The strengths of our study include the large sample size, prospective design, and ability to control for many potential confounding factors. The lack of occupational physical activity data is a potential limitation; however, we believe this to have minimal impact on daily physical activity levels because the majority of study participants were retired/homemakers (57% of men and 80% of women) and, among those that were not retired, few worked in jobs that involved any activity (21% of men and 7% of women). Because we measured only leisure time spent sitting, the lack of occupational sitting time may have underestimated sitting time among working individuals, since much of their sitting time may have occurred at work. However, adjusting for employment status (employed, retired, or homemaker) did not change risk estimates for time spent sitting or physical activity. Furthermore, we conducted a sensitivity analysis among only men and women who were retired or homemakers, and results were virtually identical to those in the overall cohort. Another limitation is the use of self-reported measures of time spent sitting, physical activity, and all other covariates including height and weight. Although the physical activity and sitting time questions we used are subject to misreporting, they are very similar to those used and validated in the Nurses’ Health Study II, a prospective study with similar participant characteristics, which found a correlation of 0.79 between activity reported on recalls and questionnaire (46). These measures have also been associated with various cancers in this cohort (47–50). Finally, we were not able to differentiate between types of sitting (i.e., while watching television, reading, driving), and the energy expenditure and other behaviors may vary with different types of sitting.
In conclusion, we found that both leisure time spent sitting and physical activity are independently associated with total mortality. Associations were stronger for cardiovascular disease mortality than for cancer mortality. Public health messages and guidelines should be refined to include reducing time spent sitting in addition to promoting physical activity. Because a sizeable fraction of the population spends much of their time sitting, it is beneficial to encourage sedentary individuals to stand up and walk around as well as to reach optimal levels of physical activity.
Acknowledgments
Author affiliations: Epidemiology Research Program, American Cancer Society, Atlanta, Georgia (Alpa V. Patel, Ausila Deka, Peter T. Campbell, Susan M. Gapstur, Michael J. Thun); City of Hope, Duarte, California (Leslie Bernstein); Kaiser Permanente, Denver, Colorado (Heather Spencer Feigelson); and Washington University Siteman Cancer Center, St. Louis, Missouri (Graham A. Colditz).
The authors would like to acknowledge the late Drs. Eugenia E. Calle and Carmen Rodriguez who were instrumental in conducting and guiding this research. The preparation of this manuscript would not have been possible without them.
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- CPS-II
Cancer Prevention Study II
- ICD
International Classification of Diseases
- MET
metabolic equivalent
References
- 1.Leitzmann MF, Park Y, Blair A, et al. Physical activity recommendations and decreased risk of mortality. Arch Intern Med. 2007;167(22):2453–2460. doi: 10.1001/archinte.167.22.2453. [DOI] [PubMed] [Google Scholar]
- 2.Nocon M, Hiemann T, Müller-Riemenschneider F, et al. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008;15(3):239–246. doi: 10.1097/HJR.0b013e3282f55e09. [DOI] [PubMed] [Google Scholar]
- 3.Paffenbarger RS, Jr, Hyde RT, Wing AL, et al. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314(10):605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 4.World Cancer Research Fund/American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective. Washington, DC: American Institute for Cancer Research; 2007. [Google Scholar]
- 5.Blair SN, Morris JN. Healthy hearts—and the universal benefits of being physically active: physical activity and health. Ann Epidemiol. 2009;19(4):253–256. doi: 10.1016/j.annepidem.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Kushi LH, Fee RM, Folsom AR, et al. Physical activity and mortality in postmenopausal women. JAMA. 1997;277(16):1287–1292. [PubMed] [Google Scholar]
- 7.Rockhill B, Willett WC, Manson JE, et al. Physical activity and mortality: a prospective study among women. Am J Public Health. 2001;91(4):578–583. doi: 10.2105/ajph.91.4.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fung TT, Hu FB, Yu J, et al. Leisure-time physical activity, television watching, and plasma biomarkers of obesity and cardiovascular disease risk. Am J Epidemiol. 2000;152(12):1171–1178. doi: 10.1093/aje/152.12.1171. [DOI] [PubMed] [Google Scholar]
- 9.Ford ES, Kohl HW, III, Mokdad AH, et al. Sedentary behavior, physical activity, and the metabolic syndrome among U.S. adults. Obes Res. 2005;13(3):608–614. doi: 10.1038/oby.2005.65. [DOI] [PubMed] [Google Scholar]
- 10.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(4):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 11.Jakes RW, Day NE, Khaw KT, et al. Television viewing and low participation in vigorous recreation are independently associated with obesity and markers of cardiovascular disease risk: EPIC-Norfolk population-based study. Eur J Clin Nutr. 2003;57(9):1089–1096. doi: 10.1038/sj.ejcn.1601648. [DOI] [PubMed] [Google Scholar]
- 12.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 13.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 14.2008 Physical activity guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2008. ( http://www.health.gov/paguidelines/pdf/paguide.pdf) [Google Scholar]
- 15.Department of Health. United Kingdom. The Stationery Office; 2004. Physical Activity, Health Improvement, and Prevention. At Least Five Days a Week: Evidence on the Impact of Physical Activity and Its Relationship to Health. Norwich. [Google Scholar]
- 16.Hu FB, Li TY, Colditz GA, et al. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289(14):1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 17.Manson JE, Greenland P, Lacroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 18.Blanck HM, McCullough ML, Patel AV, et al. Sedentary behavior, recreational physical activity, and 7-year weight gain among postmenopausal U.S. women. Obesity (Silver Spring) 2007;15(6):1578–1588. doi: 10.1038/oby.2007.187. [DOI] [PubMed] [Google Scholar]
- 19.Hu FB, Leitzmann MF, Stampfer MJ, et al. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med. 2001;161(12):1542–1548. doi: 10.1001/archinte.161.12.1542. [DOI] [PubMed] [Google Scholar]
- 20.Lank NH, Vickery CE, Cotugna N, et al. Food commercials during television soap operas: what is the nutrition message? J Community Health. 1992;17(6):377–384. doi: 10.1007/BF01323999. [DOI] [PubMed] [Google Scholar]
- 21.Katzmarzyk PT, Church TS, Craig CL, et al. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 22.Dunstan DW, Barr EL, Healy GN, et al. Television viewing time and mortality: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Circulation. 2010;121(3):384–391. doi: 10.1161/CIRCULATIONAHA.109.894824. [DOI] [PubMed] [Google Scholar]
- 23.Inoue M, Iso H, Yamamoto S, et al. Daily total physical activity level and premature death in men and women: results from a large-scale population-based cohort study in Japan (JPHC Study) Ann Epidemiol. 2008;18(7):522–530. doi: 10.1016/j.annepidem.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Calle EE, Rodriguez C, Jacobs EJ, et al. The American Cancer Society Cancer Prevention Study II Nutrition Cohort: rationale, study design, and baseline characteristics. Cancer. 2002;94(2):500–511. doi: 10.1002/cncr.10197. [DOI] [PubMed] [Google Scholar]
- 25.Garfinkel L. Selection, follow-up, and analysis in the American Cancer Society prospective studies. Natl Cancer Inst Monogr. 1985;67:49–52. [PubMed] [Google Scholar]
- 26.Calle EE, Terrell DD. Utility of the National Death Index for ascertainment of mortality among Cancer Prevention Study II participants. Am J Epidemiol. 1993;137(2):235–241. doi: 10.1093/oxfordjournals.aje.a116664. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. International Classification of Diseases. Ninth Revision. Vol 1. Geneva, Switzerland: World Health Organization; 1977. [Google Scholar]
- 28.World Health Organization. International Statistical Classification of Diseases and Related Health Problems. Tenth Revision. Vol 1. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 29.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 30.Cox DR. Regression models and life tables (with discussion) J R Stat Soc (B) 1972;34(2):187–220. [Google Scholar]
- 31.Block G, Coyl L, Smucker R, et al. Health Habits and History Questionnaire: diet history and other risk factors [personal computer system documentation] Bethesda, MD: National Cancer Institute Division of Cancer Prevention and Control, National Institutes of Health; 1989. [Google Scholar]
- 32.Flagg EW, Coates RJ, Calle EE, et al. Validation of the American Cancer Society Cancer Prevention Study II Nutrition Survey Cohort food frequency questionnaire. Epidemiology. 2000;11(4):462–468. doi: 10.1097/00001648-200007000-00017. [DOI] [PubMed] [Google Scholar]
- 33.Hu FB, Willett WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351(26):2694–2703. doi: 10.1056/NEJMoa042135. [DOI] [PubMed] [Google Scholar]
- 34.Ching PL, Willett WC, Rimm EB, et al. Activity level and risk of overweight in male health professionals. Am J Public Health. 1996;86(1):25–30. doi: 10.2105/ajph.86.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coakley EH, Rimm EB, Colditz G, et al. Predictors of weight change in men: results from the Health Professionals Follow-up Study. Int J Obes Relat Metab Disord. 1998;22(2):89–96. doi: 10.1038/sj.ijo.0800549. [DOI] [PubMed] [Google Scholar]
- 36.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551(pt 2):673–682. doi: 10.1113/jphysiol.2003.045591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hamilton MT, Hamilton DG, Zderic TW. Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev. 2004;32(4):161–166. doi: 10.1097/00003677-200410000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56(11):2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 39.Hu FB. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids. 2003;38(2):103–108. doi: 10.1007/s11745-003-1038-4. [DOI] [PubMed] [Google Scholar]
- 40.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lynch J, Helmrich SP, Lakka TA, et al. Moderately intense physical activities and high levels of cardiorespiratory fitness reduce the risk of non-insulin-dependent diabetes mellitus in middle-aged men. Arch Intern Med. 1996;156(12):1307–1314. [PubMed] [Google Scholar]
- 42.Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 43.Nielsen Reports Television Tuning Remains at Record Levels. New York, NY: The Nielsen Company; 2007. [Google Scholar]
- 44.Trends in leisure-time physical activity by age , sex, and race/ethnicity—United States 1994–2004. MMWR Morb Mortal Wkly Rep. 2005;54(39):991–994. [PubMed] [Google Scholar]
- 45.Steffen LM, Arnett DK, Blackburn H, et al. Population trends in leisure-time physical activity: Minnesota Heart Survey, 1980–2000. Med Sci Sports Exerc. 2006;38(10):1716–1723. doi: 10.1249/01.mss.0000227407.83851.ba. [DOI] [PubMed] [Google Scholar]
- 46.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23(5):991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 47.Chao A, Connell CJ, Jacobs EJ, et al. Amount, type, and timing of recreational physical activity in relation to colon and rectal cancer in older adults: the Cancer Prevention Study II Nutrition Cohort. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2187–2195. [PubMed] [Google Scholar]
- 48.Patel AV, Calle EE, Bernstein L, et al. Recreational physical activity and risk of postmenopausal breast cancer in a large cohort of US women. Cancer Causes Control. 2003;14(6):519–529. doi: 10.1023/a:1024895613663. [DOI] [PubMed] [Google Scholar]
- 49.Patel AV, Feigelson HS, Talbot JT, et al. The role of body weight in the relationship between physical activity and endometrial cancer: results from a large cohort of US women. Int J Cancer. 2008;123(8):1877–1882. doi: 10.1002/ijc.23716. [DOI] [PubMed] [Google Scholar]
- 50.Patel AV, Rodriguez C, Pavluck AL, et al. Recreational physical activity and sedentary behavior in relation to ovarian cancer risk in a large cohort of US women. Am J Epidemiol. 2006;163(8):709–716. doi: 10.1093/aje/kwj098. [DOI] [PubMed] [Google Scholar]


