Abstract
The EEG report is structured to include demographics of the patient studied and reason for the EEG; specifics of the EEG techniques used; a description of the patterns, frequencies, voltages, and progression of the EEG pattern that were recorded; and finally a clinical impression of the EEG significance. The interpretation should be concise, clear and to the point, avoid jargon and EEG specifics, and should be understandable by any health care practitioner.
The EEG report has several purposes. It is designed to convey a written impression of the visual analysis of the EEG, along with an interpretation of its clinical significance. Often, a clinical correlation is offered, directed at the specific diagnostic implications for the study patient. Typically, the report encompasses 3 parts with a clinical correlation accompanying the interpretation or summary. The 3 parts are: an outline of the study parameters, description of the record, and an interpretation or summary that includes an impression of whether the study is normal or abnormal, the degree of abnormality, and the correlation of the EEG with the clinical picture.1 This review is based on the American Clinical Neurophysiology Society Guidelines for writing an EEG report along with the authors' opinions.1
An initial outline includes information about the patient including age, gender, conditions prevalent at the time of the recording (e.g., fasting, sleep deprivation), level of consciousness, and use of medications that might modify the EEG. The different states during which the EEG was then recorded (awake, drowsy, asleep, eyes closed, etc.) should be noted. There is then a brief history that notes the reason for the EEG and the techniques used. The number and types of electrodes are noted along with how they are applied, whether placed according to the standard International 10-20 System, or other recording system (i.e., combined system, field studies, special electrodes). Other channels of physiologic display should be described, such as those reserved for measurement of the ECG, for breathing, for limb movements, or, for example, for chin EMG. When eye movements are of concern, the placement of superior, inferior, lateral, or other locations for electrode placement should be noted. The duration of the study needs to be stated. Although 20 minutes is the minimum time for a standard EEG recording, reasons for a shorter study (e.g., interruption to go for an MRI; the patient removed the electrodes or refused further recording) should be mentioned. Conversely, longer records are encouraged if sleep recording is desired. As structured by the American Clinical Neurophysiology Society “Guidelines for Writing an EEG Report” state: “The aim is to produce a complete and objective report enabling another electroencephalographer (EEGer) to arrive at a conclusion regarding the normality or degree of abnormality of the record from the written report without the benefit of looking at the EEG.”
The description is a mandatory part (sometimes forgotten) and represents the “body” of the report. Here, the interpreter provides a complete and objective description of the EEG. A description includes all the salient features in the record. The contributing EEG activities are noted, commenting on the background activity or the dominant (usually posterior) background frequency in Hertz (Hz) or cycles per second. All frequencies in turn will be described regarding their frequency, location, persistence (e.g., continuous or intermittent), amplitude in microvolts, symmetry (comparing side-to-side and anterior vs posterior), and any apparent rhythmicity of the pattern, or conversely irregular or arrhythmic runs of activity. Some comment can be made regarding the actual shape of the waveforms, such as arcuate for a mu rhythm, or blunted, for example. The basic normal rhythms can be described in terms of their typical characteristics. We believe that in describing background activity, comment should be made on response to eye opening and closing, or to purposeful limb movement. Descriptions might include whether these responses are symmetric or asymmetric, whether there is complete or incomplete suppression (e.g., of the alpha or mu rhythm), or whether these effects are sustained or not. For example, eye closure can bring out focal asymmetries with the appearance of sustained posterior alpha on one side.
It is important to state which forms of stimulation or arousal were performed to evaluate EEG reactivity, particularly in cases of encephalopathy or coma. Forms of stimuli used might include touch, sound, eye opening, nasal tickle, mouth or tracheal suctioning, or sternal pressure. State whether intermittent photic stimulation, hyperventilation, or other procedures were used. Also important is the pattern of the EEG response to stimulation, e.g., increase in delta activity, or return of waking background activity. Comment on the EKG, notably if there is a significant abnormality, avoiding interpretative statements such as ischemia. When epileptiform discharges occur in the EEG, note whether they are congruent with the EKG complexes. Finally, comment on any artifacts that significantly obscure the record, or that could lead to misinterpretation, e.g., electrode pop; muscle or movement artifact. When discussing a focal abnormality, it should be described by brain region (e.g., anterior temporal), or more precisely by electrode placement, for example at T3.
The summary, interpretation, or classification is a concise summary of the findings. Here, the interpreter clearly states whether the record is normal or abnormal. If it is abnormal, then the abnormalities are listed in order of importance. It is written in a manner such that another EEGer may conceptualize the record, and be able to review the record at a later date. The reviewer should be able to compare it qualitatively and quantitatively with other EEG records. In many classification systems, the “significance” of the abnormalities can be graded according to whether the abnormalities are specific. Some institutions have categorized EEG interpretations into classification systems that are not widely used. Although not stated in the guidelines, we suggest that these classifications, while they have a role within the institution particularly for longitudinal studies involving EEG, can confuse practicing physicians or academics who read these data at other institutions. As a result, the report becomes less informative and might best be avoided. Outside EEGers should be able to understand a report without recourse to the original classification system. Some experts avoid potentially unclear terms such as “dysrhythmia” or “disorganized” because these are nonspecific.
The final section is the impression and clinical interpretation. Unlike the above, the impression is for clinicians, not EEGers, and its role is to explain what the EEG findings mean (or do not mean!). In most cases, it may be the only part of the report that will be read. Consequently, it is the most important part of the report. Critical rules for a good impression include:
An integration of the EEG findings with the history in order to give a clinical interpretation. The EEGer should discuss how the EEG findings fit (or do not fit) the clinical picture.
The interpretation should be easily understood by a general practitioner or an allied health professional such as a nurse.
Preferably, the impression should contain few technical EEG terms except for some more universally used terms such as spike-slow waves. A clinical correlation can be added, for example: “This EEG pattern of burst-suppression during normothermia but occurring after cardiac arrest (in the absence of anesthetics) indicates a very poor prognosis.” However, avoid specific therapeutic suggestions such as “this pattern warrants antiepileptic drugs.”
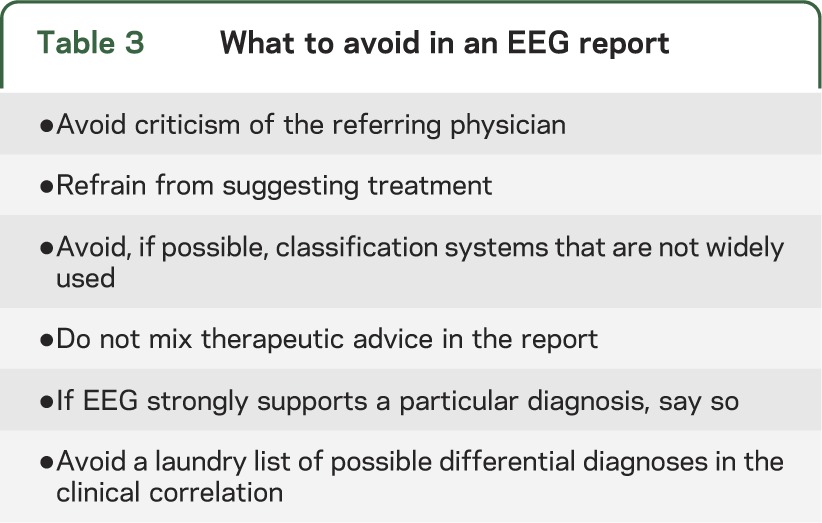
The guidelines given above apply to routine scalp EEG recordings, and the format of how to report an EEG are listed in table 1. Approaches to reporting and how not to report an EEG are listed in table 2. In general, principles important for stylistic reporting that are best avoided are listed in table 3. Special procedures (i.e., continuous video-EEG monitoring), and special types of recording (i.e., neonatal records and electrocerebral inactivity) with technical descriptions of performance require more detail.1 With the advent of digital EEG and ability to transmit reports, this enables inclusion of EEG samples in the report or charted information and may be useful when “suspicious waveforms” arise.
Table 1.
Items to include in an EEG report
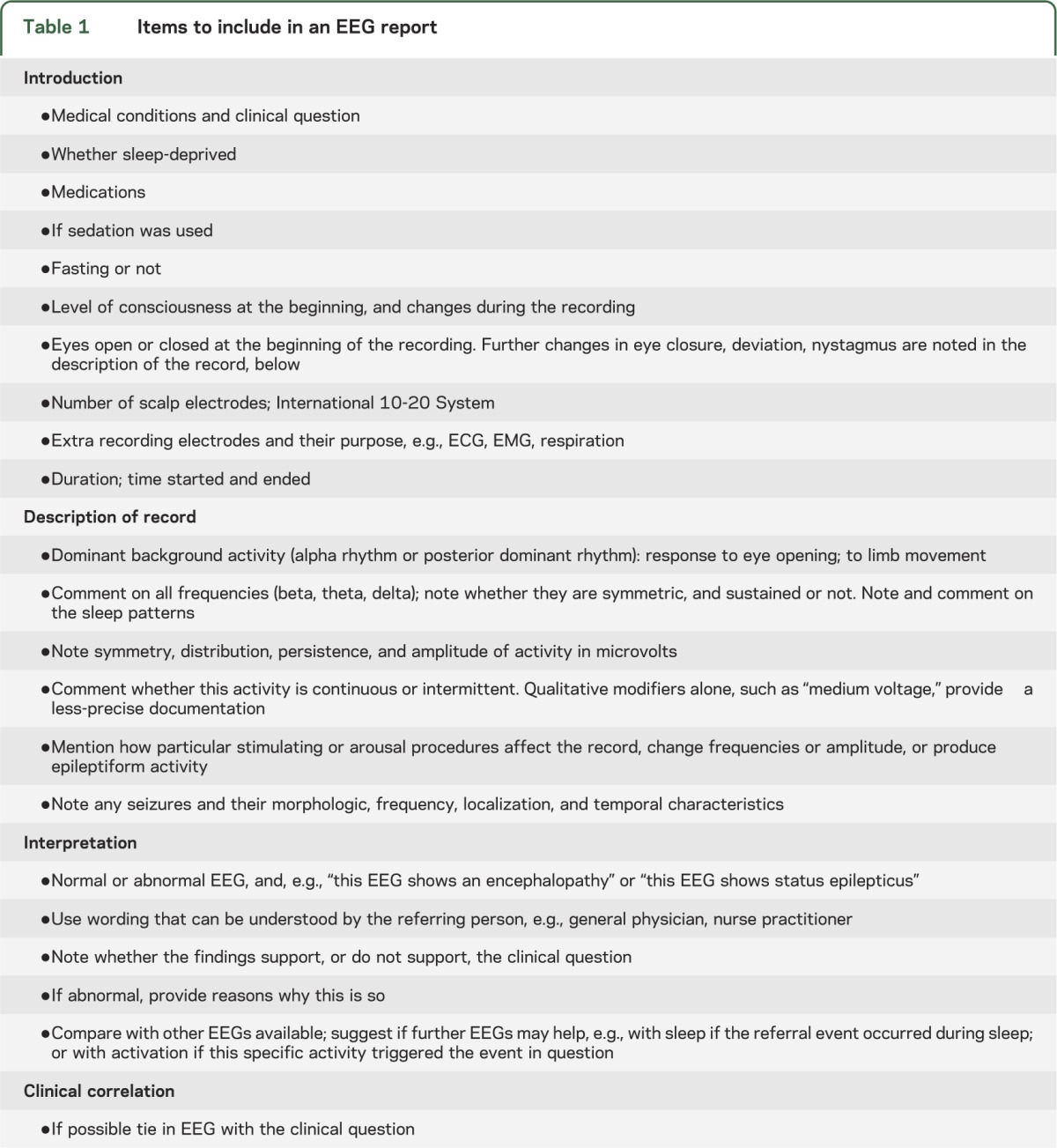
Table 2.
Some don’t’s: Frequently seen things to avoida
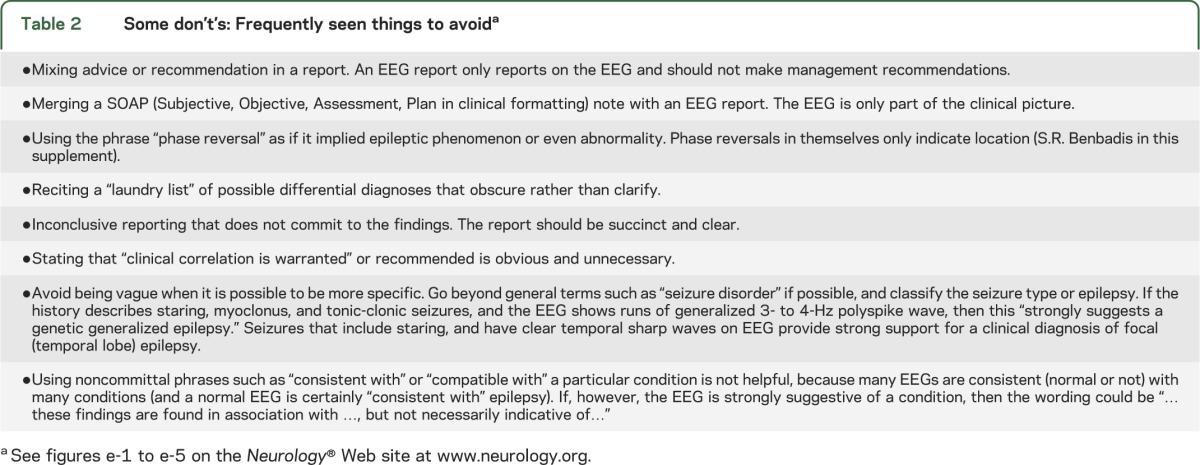
Table 3.
What to avoid in an EEG report
Glossary
- EEGer
electroencephalographer
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
P.W. Kaplan: drafting/revising the manuscript, study concept or design. S.R. Benbadis: drafting/revising the manuscript.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCE
- 1.American Clinical Neurophysiology Society Guideline 7:Guidelines for writing EEG reports. J Clin Neurophysiol 2006;23:118–121 [DOI] [PubMed] [Google Scholar]


