Abstract
Objective:
To compare the duration of birth hospitalization in mothers with multiple sclerosis (MS) and their newborns relative to the general population and to investigate the impact of MS-related clinical factors on the length of birth hospitalization stays.
Methods:
Data from the British Columbia Perinatal Database Registry and the British Columbia MS database were linked in this retrospective cohort study. The duration of birth hospitalization in mothers with MS and their newborns (n = 432) were compared with a frequency-matched sample of the general population (n = 2,975) from 1998 to 2009. Clinical factors investigated included disease duration and disability, as measured by the Expanded Disability Status Scale. A multivariable model (generalized estimating equations) was used to analyze the association between MS and duration of birth hospitalization, adjusting for factors such as maternal age, diabetes, hypertension, and consecutive births to the same mother. Additional analyses included propensity score matching to further balance cohort characteristics.
Results:
Compared with the general population, the duration of birth hospitalization was not statistically or clinically different for mothers with MS or their newborns (median differences = +1.5 and +2.1 hours, respectively; adjusted p > 0.4). Lengths of birth hospitalization were not significantly associated with disease duration (adjusted p > 0.7) or level of disability (adjusted p > 0.5). Findings remained virtually unchanged after propensity score matching.
Conclusions:
Birth hospitalization has been understudied in women with MS. Contrary to existing studies, we found that MS was not associated with a longer birth hospitalization. This study provides assurance to expectant mothers with MS, their families, and health care providers.
Multiple sclerosis (MS) is a chronic degenerative disease of the CNS, often manifesting in women of childbearing age.1 Fatigue and pelvic organ dysfunction are common,2 which may cause difficult labor and prolonged birth hospitalization. MS has been associated with a greater risk of difficult labor,3 assisted vaginal delivery,3 cesarean delivery,4 as well as impaired fetal growth and prematurity.3–6 Although not all agree, more recent studies found no link between MS and adverse perinatal outcomes.7–10 However, the durations of birth hospitalization were not examined in these studies. To our knowledge, only 2 studies have examined birth hospitalization in MS4,11; both were from the United States and reported longer hospital stays for mothers with MS4,11 and their newborns11 compared with the general population. Prolonged stays can have negative consequences, including an increased risk of hospital-acquired infection as well as creating a strain on scarce health care resources.12 By linking 2 comprehensive population databases, the British Columbia Multiple Sclerosis (BCMS) database and the British Columbia Perinatal Database Registry (BCPDR), we set out to validate earlier observations regarding the length of birth hospitalization for mothers with MS and their newborns, relative to the general population, as well as explore any association with MS clinical factors.
METHODS
Data sources
The BCMS database contains clinical data collected since September 1980 (when the first British Columbia [BC] MS clinic opened) for an estimated 80% of MS patients in BC.13,14 MS specialist neurologists generated the data for this study, which were collected from 4 MS clinics in BC (Kelowna, Prince George, Vancouver, and Victoria). The BCPDR, a province-wide database overseen by Perinatal Services BC, contains pregnancy data recorded at prenatal visits as well as at the time of birth. Data collection began in 1994 with full provincial coverage established in April 2000. The BCPDR is estimated to capture more than 99% of births reaching at least 20 weeks’ gestation.15 The BCMS database and BCPDR are reliable and objective sources of data, being collected largely in a prospective manner by trained health care professionals without a specific research question in mind. For this current study, birth hospitalization data collected up to March 31, 2009 were used.
Study participants
This cohort of mothers and newborns has been described previously.7 Briefly, births were classified as “births to MS mothers” if women had a neurologist-confirmed diagnosis of laboratory-supported or clinically definite MS (Poser16 or McDonald17 criteria) with disease onset before delivery. Birth hospitalization data of MS mothers were obtained by linking the BCMS database to the BCPDR at the individual level via the Personal Health Number, a unique identifier assigned to all residents of BC, verified by maternal names and dates of birth. Birth hospitalization data from the general population were obtained from a frequency-matched sample of births matched by maternal age (±1 year), local health authority, and delivery year. We excluded births occurring before onset of MS. We also excluded non-singleton births (i.e., twins and triplets) because of associated complications that could prolong the length of birth hospitalization. Pregnancies ending before 20 weeks’ gestation were not available.
Demographics, clinical characteristics, and outcomes
Maternal characteristics included the following: age; body mass index (BMI); gravidity; parity; number of antenatal visits; lone parent status; alcohol, drug, and cigarette use (as identified by a physician or midwife as a risk during pregnancy); hypertension (preexisting, gestational, or preeclampsia); abnormal serum glucose levels or diabetes (preexisting or identified during pregnancy); duration of the second stage of labor; assisted vaginal delivery (forceps and/or vacuum extraction); and cesarean delivery. Newborn characteristics included birth weight, gestational age, 5-minute Apgar score, and congenital anomalies. MS clinical characteristics included disease course (relapsing-onset, primary progressive, or unknown), age at MS onset, disease duration, and level of disability around the time of delivery (±3 years) as measured by the Expanded Disability Status Scale (EDSS) score.18 Primary outcomes were the length of maternal and neonatal hospitalization related to delivery. Secondary outcomes included neonatal intensive care unit (NICU) admission rates and length of stay in the NICU.
Statistical analyses
Maternal and newborn characteristics were compared between births and mothers with MS and the general population using the χ2 test or Fisher exact test for categorical variables and the Mann-Whitney U test for continuous variables. The generalized estimating equations approach was used to account for multiple singleton births to the same mother (clustering effects) and confounders. In building the generalized estimating equations, a logarithmic transformation was applied to the length of birth hospitalization to account for the right-skewed data distribution. A priori potential confounders considered in the maternal hospitalization analysis included cesarean delivery,19,20 maternal age,19 maternal comorbidity19 (hypertension or diabetes), number of antenatal visits,19 obesity as measured by BMI,21 parity,19 and prolonged labor.19 For newborns, the following a priori confounders were considered: 5-minute Apgar score,19 birth weight,19 congenital anomaly,19 maternal age,19 comorbidity19 (hypertension or diabetes), and substance use exposure19 (i.e., alcohol, cigarettes, or drugs of abuse). When data on confounders were unavailable for >20% of the MS cohort (i.e., BMI and duration of the second stage of labor), the effect of including, then excluding, each variable was examined; where no significant effect on the outcome was found, then the confounder(s) was excluded from the final model. In addition, because any adverse event affecting the duration of newborn hospitalization was deemed a potential factor in the causal pathway affecting the duration of maternal hospitalization22 and vice versa, the newborn's duration of hospitalization was not included as a potential confounder when examining the mother’s duration of stay (and vice versa). Propensity score (PS) matching was used as an additional means of balancing the MS and general population cohorts, as outlined in appendix e-1 on the Neurology® Web site at www.neurology.org. In the analysis of MS mothers, MS disease duration was included as a continuous variable, with disability categorized into 4 groups: EDSS score of 0 (normal neurologic exam), 1.0 to 1.5 (no disability but minimal neurologic symptoms present), 2.0 to 2.5 (minimal disability), and ≥3.0 (mild to moderate disability or higher).18 Associations between MS (as well as disease duration and disability) and birth hospitalization on the logarithm scale were reported with regression coefficients (β), 95% confidence interval (CI) and p values. Admissions to the NICU were reported descriptively only. All reported p values were 2-sided with an α of 0.05. Statistical analyses were conducted using SPSS 17.0 (IBM, Armonk, NY) with R (version 2.15.1) used for the PS matching.
Standard protocol approvals, registrations, and patient consents
The University of British Columbia's Clinical Research Ethics Board and the Vancouver Coastal Health Research Institute approved the study, which involved informed consent.
RESULTS
Demographics and clinical characteristics
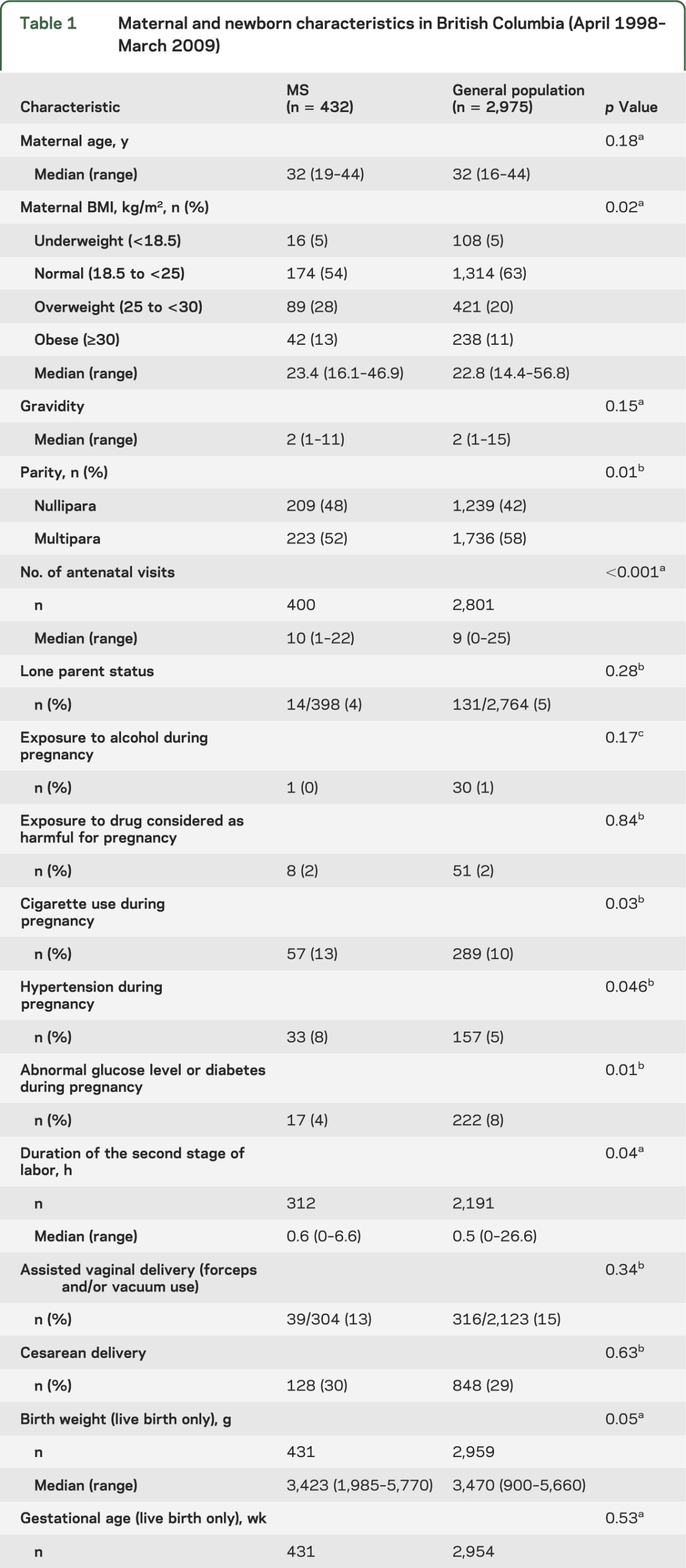
Linkage of 7,056 female patients in the BCMS database to pregnancy data from the BCPDR identified 762 births to 550 women with MS. A frequency-matched sample of 3,048 births from the general population was selected for comparison. Non-singleton infants (n = 101), births to mothers without a diagnosis of clinically definite MS (n = 225), or mothers with MS onset after delivery (n = 76) were excluded, resulting in 432 births to 321 women with MS and 2,975 births to 2,958 women from the general population. In this cohort, women with MS had 1 stillbirth whereas the sample of women in the general population had 16 stillbirths. The cohort characteristics have been previously reported7 and are summarized in table 1. Women in the MS group were more likely to be first-time mothers, hypertensive, nondiabetic, to smoke cigarettes during pregnancy, have a higher BMI, attend more antenatal visits, and have a longer duration of the second stage of labor. All other characteristics were comparable (table 1).
Table 1.
Maternal and newborn characteristics in British Columbia (April 1998–March 2009)
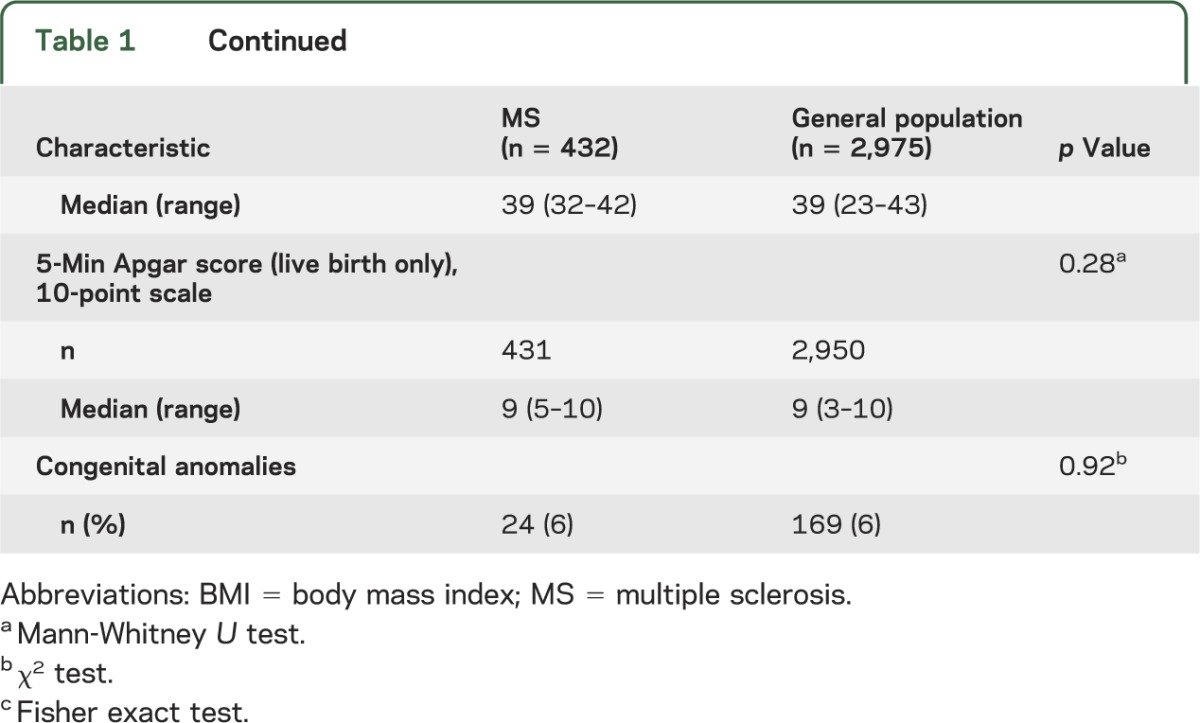
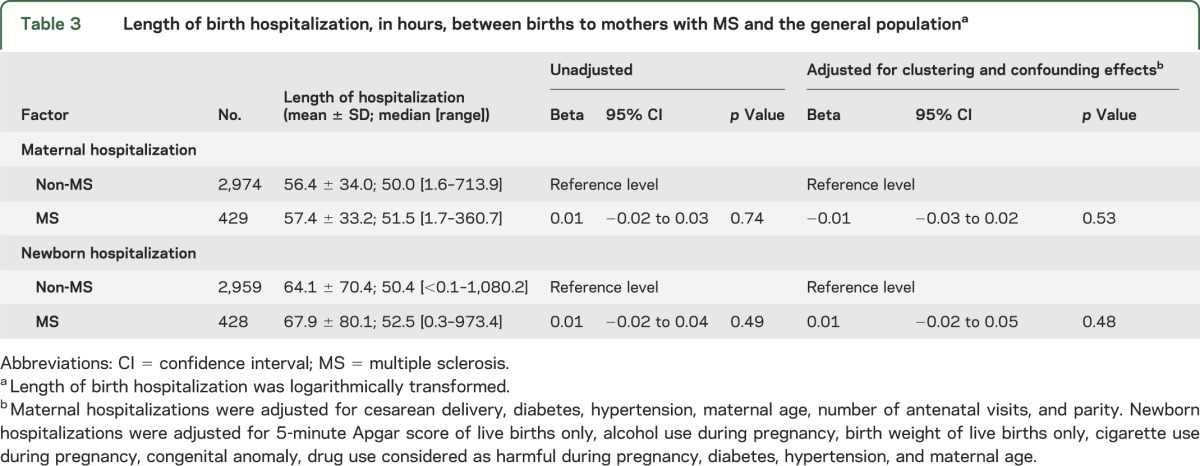
The majority of MS women had relapsing-onset MS, of which 18 births were to women with secondary progressive MS. Other clinical characteristics of the MS cohort (age at MS onset, disease duration, EDSS score) are provided in table 2.
Table 2.
Clinical characteristics of women with MS who gave birth in British Columbia (April 1998–March 2009)
Birth hospitalization
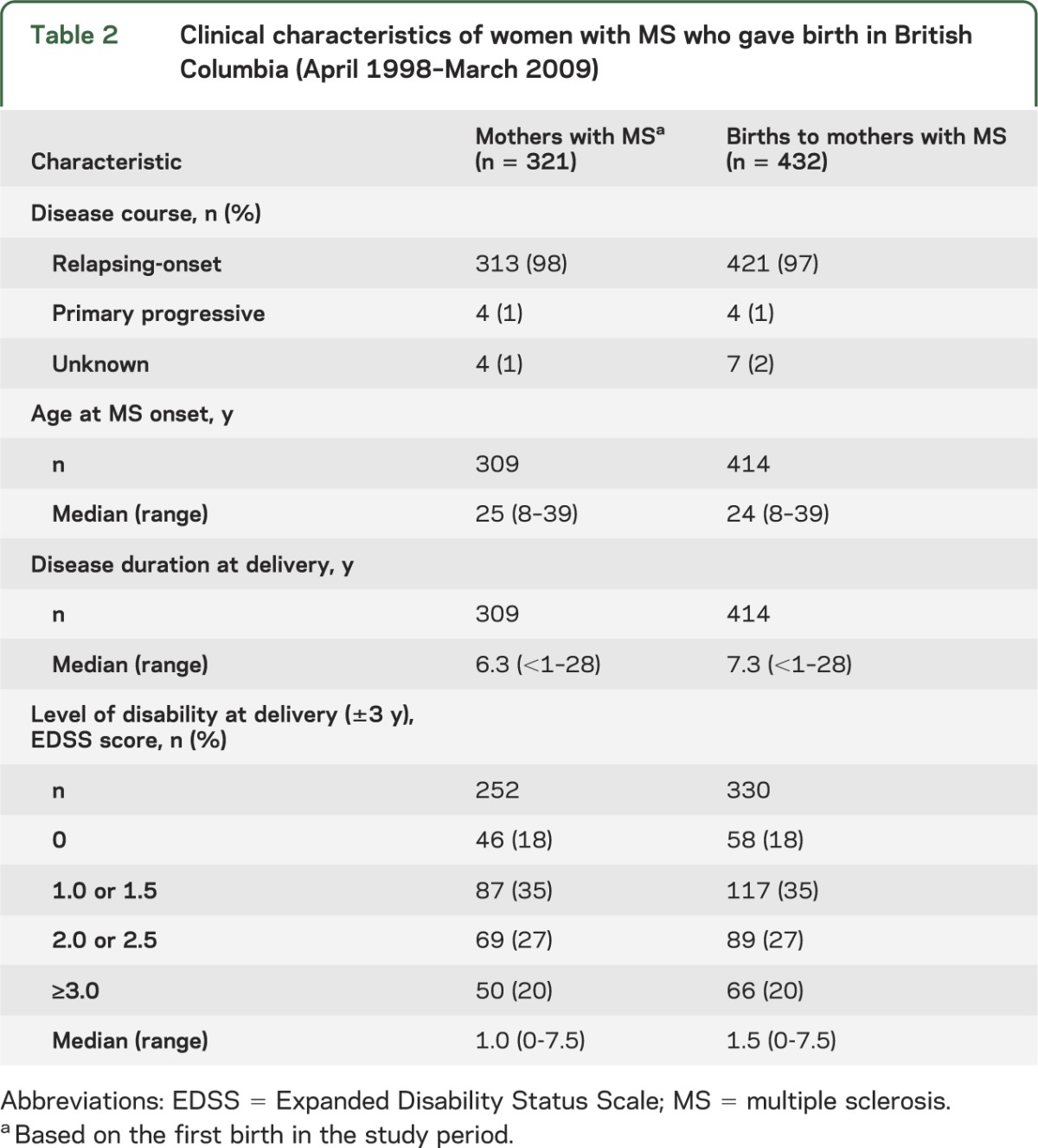
After accounting for clustering (multiple singleton births to the same mother) and confounding, the difference in length of maternal hospitalization on the logarithm scale was not statistically or clinically significant for mothers with MS (median difference of +1.5 hours) compared with the general population (table 3). Predictors of a longer length of maternal hospitalization in this sample of births in BC included older maternal age (p = 0.03), primiparity (giving birth for the first time) (p < 0.001), cesarean delivery (p < 0.001), and presence of hypertension (p = 0.047). In contrast, the number of antenatal visits or presence of diabetes was not significantly associated with the length of maternal hospitalization (p > 0.05) (data not shown).
Table 3.
Length of birth hospitalization, in hours, between births to mothers with MS and the general populationa
The duration of newborn hospitalization was also not significantly different between births to mothers with MS and the general population (median difference of +2.1 hours) (table 3). Overall, a longer length of newborn hospitalization was significantly associated with lower birth weight (p < 0.001), lower 5-minute Apgar score (p < 0.001), presence of congenital anomaly (p = 0.01), maternal hypertension (p = 0.001), and cigarette (p = 0.02) and drug use (p = 0.003) identified as a risk during pregnancy, but not maternal age, diabetes, or alcohol use (p > 0.05) (data not shown).
Findings for both maternal and newborn hospitalizations remained virtually unchanged after PS matching (see tables e-1 to e-6).
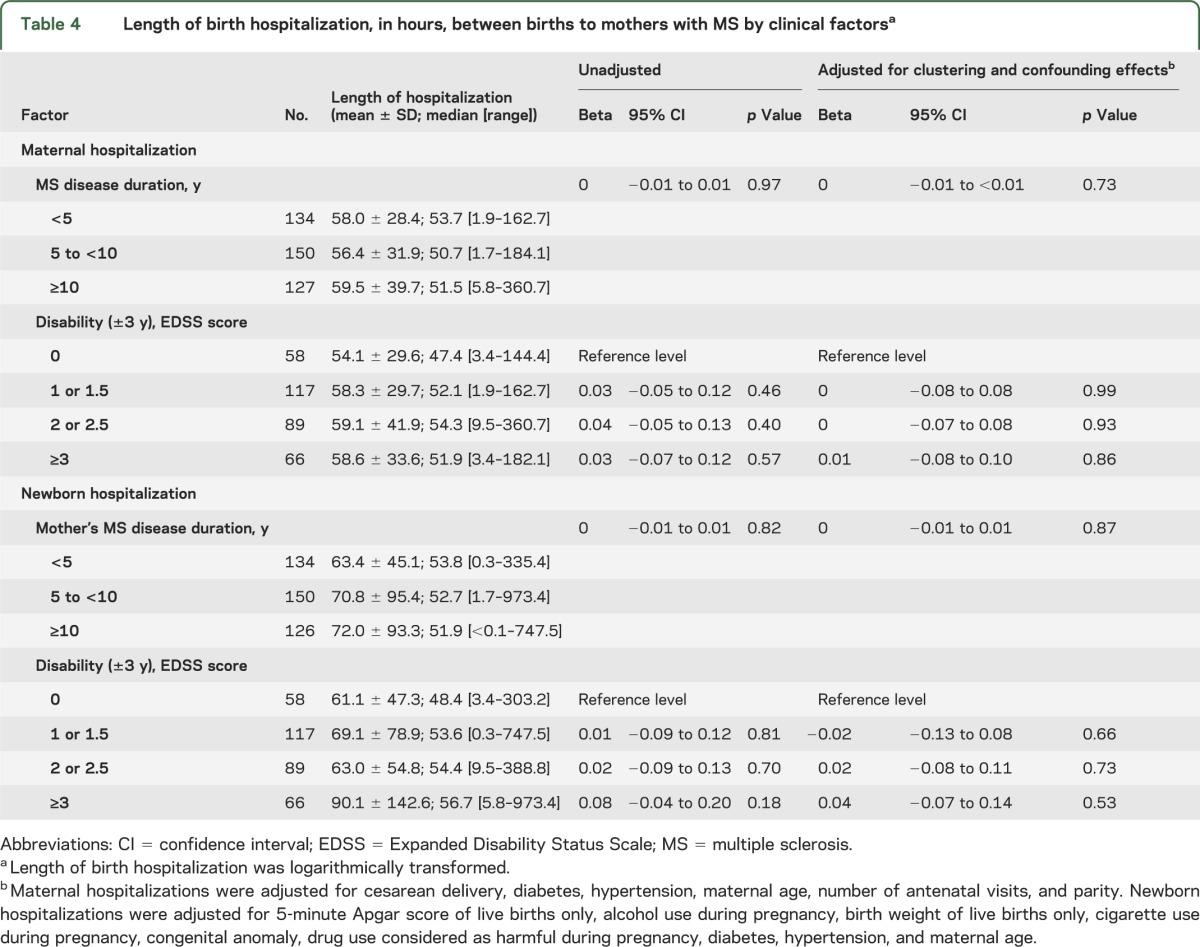
No significant associations were found between length of maternal/newborn hospitalization and MS clinical factors (table 4).
Table 4.
Length of birth hospitalization, in hours, between births to mothers with MS by clinical factorsa
Admissions to NICU
Similar to the general population (n = 53, 2%), a small proportion of newborns to mothers with MS (n = 12, 3%) were admitted to the NICU after birth. The median length of stay for newborns in the NICU was 4.5 days (range: 1–16 days) to mothers with MS, and 2 days (range: 1–40 days) to mothers from the general population.
DISCUSSION
Mothers with MS and their newborns had a similar duration of birth hospitalization as the general population, in contrast with 2 other studies whose authors reported longer birth hospitalizations.4,11 The authors of one US study in Washington state concluded that mothers with MS (n = 198) were more likely to have birth hospitalizations lasting 4 to 6 days (but not shorter [1–3 days] or longer [>6 days] stays) compared with the general population (relative risk = 1.7; 95% CI: 1.2–2.6; adjusted for maternal age and delivery method).11 Another study, accessing a nationally representative database from all nonfederal short-stay hospitals in the United States, reported a slightly longer duration of birth hospitalization (72 hours) in mothers with MS (n = 7,697) compared with mothers from the general population (64.8 hours, n = 15,200,000) after adjustment for maternal age and ethnicity (p < 0.001).4 This 7.2-hour difference, although statistically significant, is likely not of clinical significance. Findings between studies may differ for a number of reasons, including variations in socioeconomic factors and comorbidities between study populations of mothers with MS, local health care policy, clinician practice, as well as the composition of public and private health care services. In addition, identification of subjects via unvalidated methods, for instance requiring only a single International Classification of Diseases (ICD) billing code, and requiring it to be present around the time of the birth hospitalization may result in a bias toward patients with more active or severe MS in some studies. Consistent with this was the observation of an increased risk of cesarean deliveries, a known cause of longer birth hospitalizations,19,20 in women with MS when MS was identified by ICD billing codes alone4—something not found in other studies with a more comprehensive case ascertainment.7 One study examining hospital stays in newborns of mothers with MS11 reported longer stays (relative risk = 1.5; 95% CI: 0.99–2.3) compared with newborns of mothers without MS11; however, the authors speculated this was attributable to the common practice of discharging mother and newborn home together, as no other adverse birth outcomes were observed.
Our study differed from previous studies4,11 examining birth hospitalizations in a number of ways: first, our study included a cohort of women with clinically definite MS confirmed by an MS specialist neurologist, rather than relying on a single ICD code (a valid algorithm for MS requires multiple ICD billing codes recorded over a period of time)23 to identify MS. Second, we found that the length of birth hospitalization in patients with MS was not associated with disease duration or level of disability, which was not previously examined. These findings should be considered exploratory in nature and require confirmation. Third, we were able to account for data clustering arising from consecutive births to the same mother and control for confounders not considered in previous studies. Failure to adjust for these important factors may over- or underestimate the true effect of MS on birth hospitalization. We also matched mothers with MS by delivery year and local health authority to a sample of mothers from the general population to minimize potential temporal and regional differences in birth discharge practices. Finally, findings remained virtually unchanged when PS matching was applied.
A potential limitation is that MS patients with mild disease and/or limited access to an MS clinic in BC because of geographic distance may not have been captured in our database. Women with MS had an EDSS score of less than 3.0 around the time of delivery in approximately 80% of births with an EDSS score available, making our study less applicable to women with higher MS disability. Nonetheless, our study is likely broadly representative of MS patients in BC and generalizable to populations of MS mothers in Western countries with a similar health care structure to Canada. Few newborns were admitted to the NICU (with a similar proportion being admitted in the MS and general population cohorts), such that we are unable to draw firm conclusions based on these data. Finally, factors such as parental ethnicity, parental perceptions of their childcare abilities, socioeconomic background, and the availability of support resources after discharge from hospital were not available, but could influence the length of birth hospitalization.19
Overall, our findings are reassuring for women with MS planning a pregnancy or already expecting a child; the presence of MS in the mother does not seem to alter the length of birth hospitalization for the mother or baby.
Supplementary Material
ACKNOWLEDGMENT
The authors gratefully acknowledge the BC MS Clinic neurologists (see Contributors on the Neurology® Web site at www.neurology.org) who contributed to the study through patient examination and data collection. Appreciation is extended to the MS patients, as well as the Perinatal Services BC, the BCMS database staff, and the Pharmacoepidemiology in MS Research Group for providing data used in this study.
GLOSSARY
- BC
British Columbia
- BCMS
British Columbia Multiple Sclerosis
- BCPDR
British Columbia Perinatal Database Registry
- BMI
body mass index
- CI
confidence interval
- EDSS
Expanded Disability Status Scale
- ICD
International Classification of Diseases
- MS
multiple sclerosis
- NICU
neonatal intensive care unit
- PS
propensity score
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
E. Lu: design and conceptualization of the study, analysis and interpretation of the data, drafting and revising the manuscript. Y. Zhao: review of the analysis methodologies and results, interpretation of the data, revising the manuscript. F. Zhu: review of the analysis methodologies and results, interpretation of the data, revising the manuscript. M.L. van der Kop: acquisition of data, interpretation of the data, revising the manuscript. A. Synnes: interpretation of the data, revising the manuscript. L. Dahlgren: interpretation of the data, revising the manuscript. A.D. Sadovnick: interpretation of the data, revising the manuscript. A.-L. Sayao: interpretation of the data, revising the manuscript. H. Tremlett: conceptualization of the study, acquisition of study funding (along with all coauthors, apart from Mr. Zhu) and data, interpretation of the data, drafting and revising the manuscript.
STUDY FUNDING
This study was funded by the Canadian Institutes of Health Research (Operating Grant MOP-106607; PI: Dr. Helen Tremlett). The British Columbia Multiple Sclerosis database is funded by CIHR, MS Society of Canada, National MS Society, the UBC MS/MRI Research Group, and an unrestricted grant from Dr. Donald Paty.
DISCLOSURE
E. Lu is funded by the Canadian Institutes of Health Research (Canada Graduate Scholarships: Master's and Doctoral Research Awards), the Multiple Sclerosis Society of Canada (MSc and PhD Research Studentships), and the University of British Columbia (Graduate Entrance Scholarship, Faculty of Medicine Graduate Awards, and Four Year Doctoral Fellowship). Y. Zhao, F. Zhu, M.L. van der Kop, A. Synnes, and L. Dahlgren report no disclosures. A.D. Sadovnick has received research support from the MS Society of Canada Scientific Research Foundation and CIHR, and speaker honoraria and/or travel expenses to attend conferences from Biogen-Idec, Merck-Serono, Teva Neurosciences, and Bayer. A.-L. Sayao was funded by the Multiple Sclerosis Society of Canada (Postdoctoral Fellowship). H. Tremlett is funded by the Multiple Sclerosis Society of Canada (Don Paty Career Development Award), Michael Smith Foundation for Health Research, and is the Canada Research Chair for Neuroepidemiology and Multiple Sclerosis. She has received research support from the US National Multiple Sclerosis Society, CIHR, and UK MS Trust; speaker honoraria and/or travel expenses to attend conferences from the Consortium of MS Centres, US National MS Society, the University of British Columbia Multiple Sclerosis Research Program, Bayer Pharmaceutical (speaker, 2010, honoraria declined), Teva Pharmaceuticals (speaker 2011), ECTRIMS (2011), UK MS Trust (2011), and the Chesapeake Health Education Program, US Veterans Affairs (2012, honorarium declined). Unless otherwise stated, all speaker honoraria are either donated to an MS charity or to an unrestricted grant for use by her research group. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Compston A, Coles A. Multiple sclerosis. Lancet 2008;372:1502–1517 [DOI] [PubMed] [Google Scholar]
- 2.Courtney AM, Castro-Borrero W, Davis SL, Frohman TC, Frohman EM. Functional treatments in multiple sclerosis. Curr Opin Neurol 2011;24:250–254 [DOI] [PubMed] [Google Scholar]
- 3.Dahl J, Myhr KM, Daltveit AK, Gilhus NE. Planned vaginal births in women with multiple sclerosis: delivery and birth outcome. Acta Neurol Scand Suppl 2006;183:51–54 [DOI] [PubMed] [Google Scholar]
- 4.Kelly VM, Nelson LM, Chakravarty EF. Obstetric outcomes in women with multiple sclerosis and epilepsy. Neurology 2009;73:1831–1836 [DOI] [PubMed] [Google Scholar]
- 5.Dahl J, Myhr KM, Daltveit AK, Gilhus NE. Pregnancy, delivery and birth outcome in different stages of maternal multiple sclerosis. J Neurol 2008;255:623–627 [DOI] [PubMed] [Google Scholar]
- 6.Chen YH, Lin HL, Lin HC. Does multiple sclerosis increase risk of adverse pregnancy outcomes? A population-based study. Mult Scler 2009;15:606–612 [DOI] [PubMed] [Google Scholar]
- 7.van der Kop ML, Pearce MS, Dahlgren L, et al. Neonatal and delivery outcomes in women with multiple sclerosis. Ann Neurol 2011;70:41–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez Liguori N, Klajn D, Acion L, et al. Epidemiological characteristics of pregnancy, delivery, and birth outcome in women with multiple sclerosis in Argentina (EMEMAR study). Mult Scler 2009;15:555–562 [DOI] [PubMed] [Google Scholar]
- 9.Finkelsztejn A, Brooks JB, Paschoal FM, Jr, Fragoso YD. What can we really tell women with multiple sclerosis regarding pregnancy? A systematic review and meta-analysis of the literature. BJOG 2011;118:790–797 [DOI] [PubMed] [Google Scholar]
- 10.Finkelsztejn A, Fragoso YD, Ferreira ML, et al. The Brazilian database on pregnancy in multiple sclerosis. Clin Neurol Neurosurg 2011;113:277–280 [DOI] [PubMed] [Google Scholar]
- 11.Mueller BA, Zhang J, Critchlow CW. Birth outcomes and need for hospitalization after delivery among women with multiple sclerosis. Am J Obstet Gynecol 2002;186:446–452 [DOI] [PubMed] [Google Scholar]
- 12.Mosen DM, Clark SL, Mundorff MB, Tracy DM, McKnight EC, Zollo MB. The medical and economic impact of the newborns' and mothers' health protection act. Obstet Gynecol 2002;99:116–124 [DOI] [PubMed] [Google Scholar]
- 13.Sadovnick AD, Ebers GC, Wilson RW, Paty DW. Life expectancy in patients attending multiple sclerosis clinics. Neurology 1992;42:991–994 [DOI] [PubMed] [Google Scholar]
- 14.Sweeney VP, Sadovnick AD, Brandejs V. Prevalence of multiple sclerosis in British Columbia. Can J Neurol Sci 1986;13:47–51 [DOI] [PubMed] [Google Scholar]
- 15.British Columbia Perinatal Health Program British Columbia Perinatal Database Registry Annual Report 2007. Vancouver, BC: British Columbia Perinatal Health Program; 2007 [Google Scholar]
- 16.Poser CM, Paty DW, Scheinberg L, et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol 1983;13:227–231 [DOI] [PubMed] [Google Scholar]
- 17.Polman CH, Reingold SC, Edan G, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the "McDonald criteria." Ann Neurol 2005;58:840–846 [DOI] [PubMed] [Google Scholar]
- 18.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983;33:1444–1452 [DOI] [PubMed] [Google Scholar]
- 19.Bernstein HH, Spino C, Finch S, et al. Decision-making for postpartum discharge of 4300 mothers and their healthy infants: the Life Around Newborn Discharge study. Pediatrics 2007;120:e391–e400 [DOI] [PubMed] [Google Scholar]
- 20.Declercq E, Barger M, Cabral HJ, et al. Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstet Gynecol 2007;109:669–677 [DOI] [PubMed] [Google Scholar]
- 21.Mamun AA, Callaway LK, O'Callaghan MJ, et al. Associations of maternal pre-pregnancy obesity and excess pregnancy weight gains with adverse pregnancy outcomes and length of hospital stay. BMC Pregnancy Childbirth 2011;11:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization Maternal health. In: World Health Organization Fact Sheets [online]. Available at: www.who.int/mediacentre/factsheets/fs348/en/index.html#. Accessed April 30, 2012
- 23.Marrie RA, Yu N, Blanchard JF, et al. The rising prevalence and changing age distribution of multiple sclerosis in Manitoba. Neurology 2010;74:465–471 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


