Abstract
Background
Adolescents with anorexia nervosa (AN) have low bone density and low levels of surrogate markers of bone formation. Low bone density is a consequence of hormonal alterations that include hypogonadism and decreases in IGF-1, a bone trophic factor. Although IGF-1 is key to pubertal bone accretion, and effects have been demonstrated in adults, there are no data regarding the effect of recombinant human (rh) IGF-1 administration in adolescents with AN.
Objectives
We hypothesized that rhIGF-1 would cause an increase in PINP, a bone formation marker, in girls with AN, without any effect on CTX, a bone resorption marker.
Subjects and methods
RhIGF-1 was administered at a dose of 30–40 mcg/k twice daily to 10 consecutive girls with AN 12–18 years old for 7–9 days. Ten age-matched girls with AN were followed without rhIGF-1 for a similar period. IGF-1, PINP and CTX levels were measured.
Results
RhIGF-1 administration caused an increase in IGF-1 from day-1 to day-4/5 (p < 0.0001) and day-1 to day-8/9 (p < 0.0001). Simultaneously, PINP increased from day-1 to day-4/5 (p=0.004) and day-1 to day-8/9 (p=0.004), with a smaller increase from day-4/5 to day-8/9 (p=0.048). CTX levels did not change with rhIGF-1 administration. No changes occurred in IGF-1 or PINP levels in girls not receiving rhIGF-1; however, CTX levels increased significantly (p=0.01). Percent change in PINP was significantly higher (p=0.02) and percent change in CTX was significantly lower (p=0.006) in girls who received rhIGF-1 compared to those who did not receive any intervention. RhIGF-1 was well tolerated without hypoglycemia.
Conclusion
Short-term administration of rhIGF-1 causes an increase in a surrogate bone formation markers in girls with AN without significant side effects.
Keywords: IGF-1, Bone turnover markers, Adolescents, Anorexia nervosa, Bone metabolism
Introduction
Anorexia nervosa (AN), an eating disorder characterized by self-imposed severe nutritional restriction and weight loss, has a high prevalence (0.2–4.0%) amongst adolescent and college-aged women [1,2]. Low bone mineral density (BMD) is common in adolescents with AN [3,4] and is of particular importance in this younger age group because the pubertal years are critical for bone mass accrual. In fact, BMD is more severely affected when AN develops in childhood than when it develops in adult life, despite a similar duration of amenorrhea [5]. Hormonal contributors of low BMD in adolescents with AN include hypogonadism, relative hypercortisolemia, and alterations in other hormones that affect bone metabolism such as ghrelin, leptin, adiponectin and peptide YY [4,6–10]. Although hypoestrogenemia is an important contributing factor to low BMD given the known anti-resorptive effects of estrogen [11], estrogen containing oral contraceptive pills do not increase BMD in this condition [12,13]. These data suggest that correction of nutritionally dependent factors in addition to estrogen deficiency may be essential to improve BMD in adolescents with AN.
An important observation regarding low bone mass in girls with AN has been that a nutritionally acquired resistance to growth hormone (GH) with low levels of insulin like growth factor-1 (IGF-1) occurs [7]. IGF-1 is a nutritionally dependent bone trophic hormone which stimulates osteoblast function and collagen formation [14–16], and IGF-1 levels peak around mid-puberty [17], in concordance with rising GH levels. GH and IGF-1 levels are markedly increased in adolescent girls compared to adults and play a major role in bone accretion. Our group has demonstrated that girls with AN have significantly lower IGF-1 levels than healthy adolescents [7,18], and increases in IGF-1 with weight recovery predict increases in bone formation markers [18]. These data indicate that low circulating or local IGF-I resulting from undernutrition may contribute to low BMD in AN. However, the impact of rhIGF-1 administration on bone formation in children with AN has not been studied.
Our group previously used an experimental model of short-term caloric restriction in normal adult women leading to low levels of IGF-I and low levels of markers of bone turnover to investigate effects of recombinant human (rh) IGF-I administration. In such women as well as in adult women with AN, rhIGF-1 caused an increase in surrogate markers of bone formation [19,20]. However, there are no studies investigating effects of rhIGF-1 administration on bone metabolism in adolescent girls with AN. Bone accretion in children is a physiologically different state from the maintenance of bone mass in adults, with the former being a high formation and resorption state (especially in early puberty) [21] with formation exceeding resorption leading to a net increase in bone mass, while in the latter, similar rates of bone formation and resorption result in no net changes in bone mass. Because IGF-1 is an important determinant of the pubertal increase in bone mass [14], effects of rhIGF-1 may differ in adolescent AN girls than observed in adults with this disorder and are important to determine. In addition, the safety of rhIGF-1 administration in adolescents with this disorder is unknown.
To investigate the hypothesis that subcutaneous rhIGF-1 administration in adolescents with AN would stimulate bone formation, we investigated responses of a surrogate marker of bone formation (PINP: N-terminal propeptide of type 1 procollagen) and of bone resorption (CTX: C-telopeptide) to short-term rhIGF-I administration for a 7–9 day period in 10 consecutive adolescent girls with AN. We also assessed the safety profile of rhIGF-1 administration. In addition, we assessed changes in levels of PINP and CTX over a similar duration in 10 girls with AN matched for age and pubertal stage, who did not receive rhIGF-1.
Subjects and methods
Subject selection
All study subjects were between 12 and 18 years old and met DSM-IV criteria for the diagnosis of AN [22] as confirmed by the treating physician and the study psychiatrist. Ten consecutive adolescent girls with AN (16.2±0.4 years) who met inclusion criteria were enrolled to receive rhIGF-1 for 7–9 days. These girls were matched for age and pubertal stage with 10 AN girls (16.3±0.6 years), who were followed without intervention for a similar duration. The AN girls who served as controls were drawn from a previously compiled dataset (not published), and matching was performed by a blinded observer before blood samples were run for IGF-1 and bone turnover markers. For matching, the first subject who received rhIGF-1 was matched for age (within one year) and pubertal stage (within one Tanner stage) with the first available subject from the dataset, the second subject receiving rhIGF-1 with the second available subject from the dataset and matching was similarly performed for all subsequent subjects. Median duration since diagnosis of AN was 6.1 months in the group that received rhIGF-1 and 9 months in the group that did not receive rhIGF-1 (p not significant). All subjects had the restrictive form of anorexia nervosa. Five subjects, two in the group that received rhIGF-1 and three in the group that did not receive rhIGF-1 admitted to occasional purging, but did not meet criteria for bulimia nervosa. Subjects and their parents gave written assent and consent for the study, which was approved by the Institutional Review Board of Partners Health Care.
Experimental design
Subjects were studied as outpatients at the General Clinical Research Center (GCRC) of the Massachusetts General Hospital. Abnormal thyroid function, primary ovarian failure, hypokalemia and hypoglycemia were exclusion criteria. We also excluded subjects with history of any illness other than AN known to affect bone mineral metabolism, or history of use of medications known to affect bone density within three months of study initiation. The baseline (day 1) visit included a complete history and physical examination, and fasting blood was drawn between 7 and 8 a.m. for IGF-1, PINP and CTX. Weight was measured on a single electronic scale in a hospital gown. Height was measured on a single stadiometer at the GCRC in triplicate and averaged. Body composition was assessed by dual energy X-ray absorptiometry (DXA: Hologic 4500, Waltham, MA). Bone age was estimated from left hand and wrist X-rays using the standards of Greulich and Pyle [23]. Both bone age and pubertal stage were assessed by a single pediatric endocrinologist.
For the 10 consecutive girls with AN who received rhIGF-1, rhIGF-1 treatment was begun on the day of baseline evaluation. In order to minimize the risk of hypoglycemia, rhIGF-1 was administered subcutaneously using U100 insulin syringes twice a day 20 min after breakfast and after dinner. A graded dose escalation was performed to assess safety of rhIGF-1 administration. We started the study with the adult dose of 30 mcg/k twice daily [24] in the first five subjects, and when we observed no significant side effects with this dose, we increased the dose in a pubertal stage specific manner to 35 mcg/k twice daily for girls who were at Tanner stages 3 and 4 of puberty, and 40 mcg/k twice daily for girls in Tanner stage 5 of puberty (based on pubertal stage specific IGF-1 reference ranges). We considered it important to examine effects of a higher dose of rhIGF-1 in adolescents with AN than used in our study in adult women with AN, given that children with primary IGF-1 deficiency and short stature require even higher doses of rhIGF-1 (up to 120 mcg/k/dose twice daily) for replacement therapy [25]. Three girls with AN received the 35 mcg/k twice daily dose and two received the 40 mcg/k twice daily dose based on Tanner staging.
The first injection of rhIGF-1 was administered at the GCRC by a nurse, and the subject's glucose level monitored by a glucose meter every 30 min for 3 h, given the possible association of rhIGF-1 administration with hypoglycemia. To confirm the accuracy of the fingerstick glucose level at each of the time points, plasma glucose levels were sent to the laboratory. After the initial injection, the GCRC nurse taught the subject and/or her parents how to administer the rhIGF-1 injection, and reviewed the technique of fingerstick glucose testing. Subsequent rhIGF-1 injections were administered at home twice daily by the subject or her parents for the duration of the study. To collect data in order to develop a safety profile of rhIGF-1 administration in girls with AN, subjects were instructed to check and record glucose levels using a glucose meter at 1 and 2 h after each injection. Furthermore, subjects were asked to check a fingerstick glucose level if they experienced any symptoms suggestive of hypoglycemia. Symptoms of hypoglycemia were reviewed with the subject and her parents, as well as appropriate actions to take if the subject developed hypoglycemia. We defined hypoglycemia as a fingerstick or plasma glucose level of <60 mg/dl. Subjects maintained a diary for the duration of the study that included a record of all fingerstick glucose levels as well as any side effects experienced during the study. We also compared recorded glucose values in the diary against those obtained from the glucose meter.
Subjects receiving rhIGF-1 returned for evaluation on day 4 or 5 and day 8 or 9 for a history and physical examination (including weight measurement and fundoscopy), and to have blood drawn fasting between 7 and 8 a.m. to evaluate biochemical endpoints (IGF-1, PINP and CTX). Subjects with AN not receiving rhIGF-1 did not come for the day 4 or 5 visit. Pregnancy was excluded in subjects at study visits. All subjects were enrolled in active outpatient eating disorder programs. Although IGF-1 levels can change with weight changes, nutritional restriction was not required for study participation because we did not want the study to impact ongoing therapy. Instead, we examined weight changes in the groups that did or did not receive rhIGF-1 and did not find any differences between the groups. We also controlled for weight changes in our statistical analysis.
Laboratory methods
An immunoradiometric assay (Diagnostic Systems Laboratories, Inc, Webster, TX) was used to measure serum IGF-I. The detection limit was 2.06 ng/ml and the intra-assay CV was 3.9%. PINP was measured using a RIA (Orion Diagnostica, Espoo, Finland), with a detection limit of 2 ng/ml and an intra-assay CV of 6.5–10.2%, and CTX using an ELISA (Immunodiagnostics Systems Limited; Tyne and Wear, UK) with a detection limit of 0.02 ng/ml and an intra-assay CV of 1.7–3.0%. LH, FSH, TSH, potassium, glucose levels were assessed by the hospital laboratory using published methods [26].
Statistical methods
Data are reported as means±SE, and were analyzed using the JMP program (version 4, SAS Institute Inc., Cary, NC). Baseline comparisons were performed using the Student t-test. We used paired t-tests to assess (i) differences in levels of IGF-1, PINP and CTX at day 4/5 and day 8/9 from baseline levels in girls with AN receiving rhIGF-1, and (ii) differences in levels of IGF-1, PINP and CTX from baseline levels in girls with AN not receiving rhIGF-1. These data are reported as means± SEM. We also compared percent change in PINP and CTX from day 1 to day 8/9 between girls who did or did not receive rhIGF-1. Associations between changes in IGF-1 levels (Δ IGF-1) with changes in PINP (Δ PINP) and CTX (Δ CTX) were determined. Because these data were not normally distributed and logarithmic conversions were not successful in approximating a normal distribution, we used Spearman's correlation to determine these associations. We also used mixed model multiple regression analysis to determine whether changes in IGF-1 levels predicted changes in levels of bone turnover markers independent of weight changes (p < 0.11 to enter and <0.10 to leave the model), and also independent of age and pubertal stage.
Results
Baseline characteristics
Girls with AN who received rhIGF-1 did not differ from girls not receiving rhIGF-1 for age, bone age, height, weight, BMI, BMI SDS, fat mass, lean mass or IGF-1 levels (Table 1).
Table 1.
Baseline characteristics of adolescent girls with anorexia nervosa who received rhIGF-1 (n=10) or did not receive rhIGF-1 (n=10).
| AN: rhIGF-1+ | AN: rhIGF-1− | |
|---|---|---|
| Age (years) | 16.2±0.5 | 16.3±0.6 |
| Bone age (years) | 15.3±0.5 | 16.2±0.5 |
| Tanner stage (breasts) | 4.5±0.2 | 4.8±0.1 |
| Height (cm) | 160.3±2.3 | 163.9±2.6 |
| Weight (kg) | 44.5±2.1 | 47.2±1.9 |
| BMI (kg/m2) | 17.2±0.4 | 17.5±0.3 |
| BMI SDS | −1.6±0.3 | −1.3±0.2 |
| Fat mass (kg) | 9.2±0.6 | 9.2±0.8 |
| Percent body fat | 20.7±1.3 | 18.8±1.4 |
| IGF-1 (ng/ml) | 312±36 | 246±26 |
| IGF-1 SDS | −1.23±0.22 | −1.53±0.14 |
| PINP (ng/ml) | 129.6±20.5 | 116.4±54.0 |
| CTX (ng/ml) | 1.07±0.13 | 1.07±0.22 |
AN: rhIGF-1+: Girls with anorexia nervosa who received rhIGF-1; AN: rhIGF-1−: Girls with anorexia nervosa who did not receive rhIGF-1.
There were no significant differences between the groups for baseline characteristics.
Changes in IGF-1, PINP and CTX with or without RhIGF-1 administration
Changes in IGF-1 and in levels of surrogate markers of bone turnover in girls with AN who received rhIGF-1 or were followed without rhIGF-1 administration are shown in Table 2. IGF-1 levels increased significantly in girls with AN with rhIGF-1 administration, but did not change in girls with AN who did not receive rhIGF-1.
Table 2.
Paired t-test comparing changes in IGF-1, PINP and CTX levels with or without rhIGF-1 administration at day 4/5 compared to day 1 (D 4/5–D 1), at day 8/9 compared to day 1 (D 8/9–D 1), and at day 8/9 compared to day 4/5 (D 8/9–D 4/5) in adolescent girls with anorexia nervosa: data are presented as the mean difference in levels of IGF-1, PINP and CTX (SEM).
| Mean difference (SEM) (D 4/5–D 1) | p value | Mean difference (SEM) (D 8/9–D 1) | p value | Mean difference (SEM) (D 8/9–D 4/5) | p value | |
|---|---|---|---|---|---|---|
| Girls with AN who received rhIGF-1 | ||||||
| IGF-1 (ng/ml) | 507.8 (36.3) | < 0.0001a | 542.9 (40.9) | < 0.0001a | 35.1 (56.3) | Ns |
| IGF-1 SDS | 3.31 (0.31) | < 0.0001a | 3.49 (0.31) | < 0.0001a | 0.19 (0.35) | Ns |
| PINP (ng/ml) | 31.2 (7.5) | 0.004a | 39.3 (9.3) | 0.004a | 8.1 (3.4) | 0.048 |
| CTX (ng/ml) | −0.13 (0.14) | Ns | −0.11 (0.15) | Ns | 0.03 (0.15) | Ns |
| Girls with AN who did not receive rhIGF-1 | ||||||
| IGF-1 (ng/ml) | – | – | −22.9 (16.2) | Ns | – | – |
| IGF-1 SDS | −0.12 (0.09) | Ns | ||||
| PINP (ng/ml) | – | – | 5.7 (6.0) | Ns | – | – |
| CTX (ng/ml) | – | – | 0.50 (0.16) | 0.01 | – | – |
D 1: day 1 of study; D 4/5: day 4–5 of study; D 8/9: day 8 or 9 of study; Ns: not significant.
Significant even after adjusting for multiple comparisons.
Girls with AN who received rhIGF-1 for 7–9 days (Table 2)
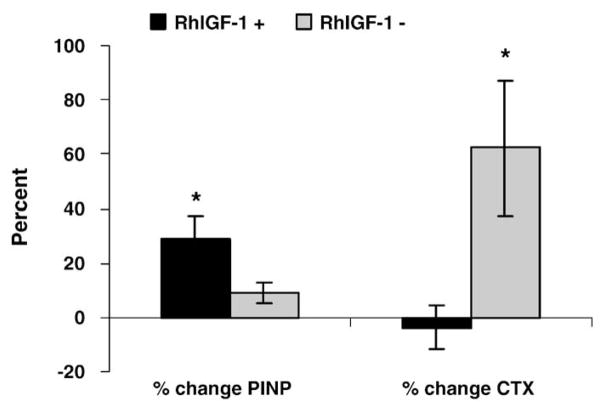
On a paired t-test there was a significant increase in IGF-1 levels following rhIGF-1 administration from day 1 to day 4/5 (p < 0.0001) and from day 1 to day 8/9 (p < 0.0001). Maximal increases were seen by day 4/5 and were sustained with no further increase from day 4/5 to day 8/9. IGF-1 levels returned to baseline following discontinuation of rhIGF-1 in all subjects who returned for the day 23/24 visit. Commensurate with an increase in IGF-1, levels of PINP, a bone formation marker, increased significantly from day 1 to day 4/5 (p=0.004) and from day 1 to day 8/9 (p=0.004), with a smaller but significant increase from day 4/5 to day 8/9 (p=0.048). CTX levels (bone resorption marker) did not significantly change following rhIGF-1 administration. Percent change in PINP levels over the study duration was significantly higher (29.4±9.8 versus 2.5±4.8%, p=0.02), and percent change in CTX levels significantly lower (−3.7±7.6 versus 62.3±18.3%, p=0.006), in girls with AN who received rhIGF-1 compared with those that did not (Fig. 1).
Fig. 1.
Percent change in levels of PINP and CTX in girls with anorexia nervosa who did (black bars) or did not (gray bars) receive rhIGF-1. A significant increase occurred in PINP following 7–9 days of rhIGF-1 administration in girls receiving rhIGF-1. In contrast, a significant increase occurred in CTX over the study duration in girls who did not receive rhIGF-1. *p < 0.05.
We also examined changes in IGF-1, PINP and CTX within girls with AN who received the lower dose of rhIGF-1 (30 mcg/k/dose twice daily) (first five subjects) and those who received the higher dose of rhIGF-1 (35–40 mcg/k/dose twice daily) (last five subjects). In a paired t-test, with the lower dose, the mean difference in IGF-1 levels was 433.5±15.7 ng/ml (p=0.0001) from day 1 to day 4/5 and 522.8± 80.1 ng/ml (p=0.007) from day 1 to day 8/9. With the higher dose, mean difference in IGF-1 was 582.0±47.3 ng/ml (p=0.001) from day 1 to day 4/5 and 563.0±33.7 ng/ml (p=0.0005) from day 1 to day 8/ 9 (Fig. 1). Associated mean difference in PINP with the lower dose was 35.9±10.7 ng/ml (p=0.04) from day 1 to day 4/5 and 41.5± 15.1 ng/ml (p=0.07) from day 1 to day 8/9, and with the higher dose, 26.4±11.5 ng/ml (p=0.10) and 37.2±13.0 ng/ml (p=0.05) respectively. No differences in CTX were observed with either dose.
Girls with AN who did not receive rhIGF-1
No change in IGF-1 levels occurred in this group over the follow-up period as assessed using the paired t-test (Table 2). Similarly, no significant change in PINP levels was observed. A significant increase occurred in levels of CTX (p=0.01).
Association between changes in IGF-1 levels and changes in PINP and CTX
There was a positive association between the change in IGF-1 levels (Δ IGF-1) from day 1 to day 8/9 and the change in PINP (Δ PINP) over the same period within girls who received rhIGF-1 (r=0.89, p=0.0005), those who did not receive rhIGF-1 (r=0.71, p=0.003), and for all girls with AN taken together (r=0.74, p=0.0003) using Spearman's correlation. Interestingly, for the group of AN girls as a whole, but not for the individual groups, we found an inverse association between Δ IGF-1 and change in CTX (Δ CTX) (r=−0.59, p=0.008). These associations held when we used Δ IGF-1 SDS rather than Δ IGF-1.
Change in weight (Δ weight) over the week was −0.01±0.40 kg for girls receiving rhIGF-1 and −0.01±0.25 kg for girls not receiving rhIGF-1 (p not significant). For all girls with AN taken together, Δ IGF-1 remained a significant positive predictor of Δ PINP (accounting for 52% of the variability) and an inverse predictor of Δ CTX (accounting for 38% of the variability) in a regression model that included Δ weight over the study duration. Within girls who received rhIGF-1, Δ IGF-1 levels over a week contributed to 56% of the variability of Δ PINP over that period after controlling for Δ weight (p=0.03), but did not predict Δ CTX. Similarly, within girls who did not receive rhIGF-1, Δ IGF-1 levels over a week contributed to 50% of the variability of Δ PINP over that period after controlling for Δ weight (p=0.03), but did not predict Δ CTX. Baseline anthropometric measures (including age, bone age and pubertal stage) and IGF-1 levels did not predict subsequent changes in PINP levels.
Safety profile of RhIGF-1
RhIGF-1 was overall well tolerated by our subjects. Table 3 shows details of all reported side effects. None of our subjects had fingerstick or plasma glucose levels of <60 mg/dl. Reports of dizziness in one subject and headaches in four subjects were not associated with low fingerstick or plasma glucose levels or with abnormal examination on fundoscopy. Visual fields were normal in all. One subject had moderate headaches associated with initiation of trazodone therapy for associated depression, and her headaches decreased after weaning the trazodone dose after a week of study completion. Headaches resolved spontaneously in two other subjects, and with medication in a third in one to two days. All three subjects with possible study-related headaches had received 35–40 mcg/k/dose twice weekly of rhIGF-1 (thus the higher dose). None of the subjects who received the lower dose of rhIGF-1 reported headaches over the study duration.
Table 3.
Side effects from rhIGF-1 administration.
| Side effects | Number of subjects | Severity | Relatedness to study | Associated conditions |
|---|---|---|---|---|
| Headaches | 4 | All had normal fundoscopic examinations and normal fingerstick or plasma glucose levels | ||
| 1 mild, 3 moderate | 1 unrelated | Unrelated: associated with simultaneous use of trazodone | ||
| 3 possibly or probably related (all associated with the higher dose of rhIGF-1) | Possibly/probably related: headaches resolved spontaneously or with medication in 1–2 days | |||
| Nausea and abdominal pain | 1 | Moderate | Unlikely | Constipation |
| Dizziness | 1 | Mild | Unlikely | Normal fingerstick and plasma glucose |
| Increased frequency of bowel movements | 1 | Mild | Unlikely | |
| Symptoms of URI and/or sinusitis | 2 | Mild | Unrelated | |
| Hospitalization for concerns of weight loss | 1 | Severe | Unrelated | Known morbidity associated with anorexia nervosa |
Unrelated or unlikely to be related adverse events included an upper respiratory infection in two subjects, nausea with abdominal pain and increased frequency of bowel movements in two subjects, and a hospitalization for anorexia nervosa associated weight loss in a fifth.
Discussion
Our data are the first to examine the effects of rhIGF-1 administration on bone formation markers in adolescents with AN. We found that rhIGF-1, when given in a dose of 30–40 mcg/k twice daily, successfully increases IGF-1 levels to a high normal range in adolescent girls with AN and is associated with significant selective increases in levels of PINP, a marker of bone formation, without a concomitant increase in CTX, a bone resorption marker. The effect of rhIGF-1 administration is immediate; occurring over a short duration of 7–9 days. The administration of rhIGF-1 was well tolerated in our cohort without significant side effects. These data demonstrate that rhIGF-1 administration increases bone formation markers in adolescents with AN, a state of decreased bone formation and low bone mass.
These data are of particular interest in this adolescent age group given that IGF-1 levels peak in the pubertal years [17], and because IGF-1 has a very important role in optimizing peak bone mass. Both GH and IGF-1 are bone anabolic and increase bone formation rates [14]. Together with anti-resorptive effects of estrogen, the bone anabolic effects of rising levels of GH and IGF-1 are integral to the increase in bone mass characteristic of puberty. More than 25% of peak bone mass is accrued in the two perimenarchal years, with more than 90% of peak bone mass being achieved by the end of the second decade [27]. Disorders such as AN that are associated with a state of acquired GH resistance and low levels of IGF-1 [7] would be expected to be also associated with low rates of bone formation, and consistent with this, we have reported low levels of bone formation markers in adolescent girls with AN [7,18,28]. In fact, adolescents with AN appear to be in a state of reduced bone turnover overall, with a decrease in levels of both bone formation and bone resorption markers [29]. This is in contrast to normal adolescence, which is a state of increased bone turnover [21], with bone formation rates exceeding bone resorption, resulting in a net increase in bone accrual, and also in contrast to adults with AN, who have an increase in bone resorption markers [19,30]. We have also reported that IGF-1 is an important predictor of bone metabolism, and changes in IGF-1 directly predict increases in bone formation markers [18].
Weight recovery in girls with AN is associated with an increase in IGF-1 and bone formation markers [18]. However, increase in bone density is modest, at least over a short duration of follow-up, even with recovery of weight and menses [31]. Conversely, girls who recover weight do not demonstrate the decrease in bone density observed in non-recovered girls, and the expectation is that sustained recovery will eventually cause an increase in bone mass accrual rates. However, given that there is a very narrow window in time in which to optimize bone mass accrual during adolescence, with evidence that deficits incurred in this time may be permanent [5], there is a need to consider therapeutic interventions to optimize bone mass accrual and bone density during these critical years. Estrogen deficiency is an important contributor to low bone density in AN, yet estrogen replacement as oral contraceptive pills does not increase bone density in girls with AN [13]. IGF-1 replacement is another possible therapeutic strategy to increase bone accrual rates and therefore bone density, and our data are encouraging in that modest doses of rhIGF-1 are successful in increasing markers of bone formation even over a short period of just 7–9 days. Changes in IGF-1 levels positively predicted changes in levels of PINP for girls who received rhIGF-1, those that did not receive rhIGF-1, and for the group as a whole. Long-term rhIGF-1 therapy may thus lead to sustained increases in bone formation rates and in bone density.
We did not observe an increase in surrogate markers of bone resorption (CTX) over the study duration, similar to a study of rhIGF-1 administration in adults with AN [19]. Typically, bone turnover is coupled such that an increase in bone formation is associated with an increase in bone resorption. Interestingly, a lag period (referred to as the anabolic window) has been reported following initiation of PTH therapy, when bone resorption rates are still low [32–34]. PTH is a bone anabolic hormone, and it is possible that this lag period may also occur with other anabolic therapies such as rhIGF-1. It is thus possible that a longer duration of rhIGF-1 administration may demonstrate an increase in CTX in addition to an increase in PINP. In this short-term study, CTX did not change with rhIGF-1 administration, but increased in girls not receiving rhIGF-1, and the change in IGF-1 was an inverse predictor of change in CTX. These data suggest an inhibitory effect of rhIGF-1 on bone resorption at least over a short duration of therapy, which needs to be better elucidated. Importantly, this association was not maintained within the group that received rhIGF-1 or did not receive rhIGF-1, and was only observed for the group as a whole. Further studies are necessary to determine whether levels of bone resorption markers decrease or increase over time with a longer duration of rhIGF-1 administration. A sustained inhibition of bone resorption rates associated with an increase in bone formation with rhIGF-1 administration may cause bone mass accrual to be even greater than expected.
Although much higher doses of rhIGF-1 are used in children with severe primary IGF-1 deficiency than used in this study, the doses we used were sufficient to increase IGF-1 levels to the upper half of the normal range, and were also sufficient to cause an increase in bone formation markers over the week of administration. Interestingly, we observed significant increases in IGF-1 and PINP levels even with the 30 mcg/k twice daily dose of rhIGF-1. Therefore, even though this is a relatively small dose compared to doses used in primary IGF-1 deficiency, this dose of rhIGF-1 may be sufficient to cause an increase in bone formation and bone density in secondary causes of IGF-1 deficiency, such as AN.
We did not observe any episodes of hypoglycemia in our subjects, despite their low weights, which may be a consequence of rhIGF-1 administration soon after meals. Conversely, a larger number of subjects may be necessary before we observe this particular side effect. Importantly, in another study, we did not observe hypoglycemia following rhIGF-1 administration in adult women with AN over a nine-month period [24], and children with primary IGF-1 deficiency are reported to have a higher risk of hypoglycemia even before rhIGF-1 administration. No evidence of raised intracranial pressure was evident in subjects reporting headaches, as assessed by fundoscopy by study investigators at days 4 to 5 and again at days 8 to 9 of rhIGF-1 administration. Mild to moderate intensity headaches that were possibly study related occurred with the higher dose (35–40 mcg/k/dose twice daily) of rhIGF-1, but not with the lower dose (30 mcg/k/dose twice weekly), although our sample size was not large enough to be definitive about this. Because PINP effects were similar with both IGF-1 dosing regimes, the higher dose of rhIGF-1 does not appear to be necessary in girls with AN.
A limitation of our study is that this was not a randomized controlled trial of rhIGF-1 versus placebo. However, by enrolling consecutive girls with AN who met inclusion criteria for rhIGF-1 administration, and by matching these girls sequentially by age and pubertal stage to another group of AN girls not receiving any intervention, we sought to eliminate some of the biases associated with a non-randomized design. Importantly, matching was performed before biochemical data were available to further minimize bias. Of importance, no significant differences were observed in weight changes between the two groups. In addition, other hormones that could potentially impact bone metabolism were not measured at follow-up. However, the short duration of the study and lack of weight changes over the study duration make it unlikely that significant changes occurred in body composition and other hormones likely to impact bone metabolism. These parameters will need to be assessed in a subsequent study of longer duration.
Another question is whether supraphysiological doses of rhGH could overcome the state of GH resistance in AN and lead to an increase in bone formation and bone density. One non-randomized study demonstrated an increase in IGF-1 levels with rhGH administration in AN [10]. However, women in this study who received rhGH also had significant increases in weight over the study duration and it is unclear whether increases in IGF-1 were related to increases in weight or to rhGH administration, or whether weight gain during GH administration was associated with an increase in total body water. In addition, this study did not examine markers of bone turnover or bone density. There is also a risk for side effects with very high doses of rhGH.
Our data indicate that short-term rhIGF-1 administration can increase levels of surrogate markers of bone formation in adolescent girls with AN without significant side effects. The effect of chronic rhIGF-1 administration on bone density in this population is unknown and remains to be determined.
Acknowledgments
We would like to thank the research nurses and bionutritionists at the General Clinical Research Center of Massachusetts General Hospital and our subjects, without whom this study would not have been possible. We would also like to thank Patrick Sluss, PhD, of Massachusetts General Hospital, and Dr. Clifford Rosen at Maine Medical Center Research Institute, Portland, ME, for performing the IGF-1, PINP and CTX assays. We would like to thank Hang Lee, PhD, for support with the statistical analysis required for this study.
Abbreviations
- AN
anorexia nervosa
- PINP
N-terminal propeptide of type 1 procollagen
- CTX
C-telopeptide
- BMD
bone mineral density
Footnotes
Statement of Financial Support: The study was supported by an investigator initiated grant received from Tercica, and in part by NIH grants R01 DK 062249, K23 RR018851 and M01-RR-01066.
References
- 1.Lucas AR, Beard CM, O'Fallon WM, Kurland LT. 50-year trends in the incidence of anorexia nervosa in Rochester, MN: a population-based study. Am J Psychiatry. 1991;148:917–22. doi: 10.1176/ajp.148.7.917. [DOI] [PubMed] [Google Scholar]
- 2.Pope H, Jr, Hudson J, Yurgelun-Todd D. Prevalence of anorexia nervosa and bulimia in three student populations. Int J Eat Disord. 1984;3:45–51. [Google Scholar]
- 3.Bachrach L, Guido D, Katzman D, Litt I, Marcus R. Decreased bone density in adolescent girls with anorexia nervosa. Pediatrics. 1990;86:440–7. [PubMed] [Google Scholar]
- 4.Misra M, Aggarwal A, Miller KK, Almazan C, Worley M, Soyka LA, et al. Effects of anorexia nervosa on clinical, hematologic, biochemical, and bone density parameters in community-dwelling adolescent girls. Pediatrics. 2004;114:1574–83. doi: 10.1542/peds.2004-0540. [DOI] [PubMed] [Google Scholar]
- 5.Biller B, Saxe V, Herzog D, Rosenthal D, Holzman S, Klibanski A. Mechanisms of osteoporosis in adult and adolescent women with anorexia nervosa. J Clin Endocrinol Metab. 1989;68:548–54. doi: 10.1210/jcem-68-3-548. [DOI] [PubMed] [Google Scholar]
- 6.Misra M, Miller K, Almazan C, Ramaswamy K, Lapcharoensap W, Worley M, et al. Alterations in cortisol secretory dynamics in adolescent girls with anorexia nervosa and effects on bone metabolism. J Clin Endocrinol Metab. 2004 doi: 10.1210/jc.2004-0723. [Submitted] [DOI] [PubMed] [Google Scholar]
- 7.Misra M, Miller K, Bjornson J, Hackman A, Aggarwal A, Chung J, et al. Alterations in growth hormone secretory dynamics in adolescent girls with anorexia nervosa and effects on bone metabolism. J Clin Endocrinol Metab. 2003;88:5615–23. doi: 10.1210/jc.2003-030532. [DOI] [PubMed] [Google Scholar]
- 8.Misra M, Miller K, Stewart V, Hunter E, Kuo K, Herzog D, et al. Ghrelin and bone metabolism in adolescent girls with anorexia nervosa and healthy adolescents. J Clin Endocrinol Metab. 2005;90:5082–7. doi: 10.1210/jc.2005-0512. [DOI] [PubMed] [Google Scholar]
- 9.Misra M, Miller K, Tsai P, Gallagher K, Lin A, Lee N, et al. Elevated peptide YY levels in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab. 2006;91:1027–33. doi: 10.1210/jc.2005-1878. [DOI] [PubMed] [Google Scholar]
- 10.Hashizume K, Suzuki S, Komatsu A, Hiramatsu K, Mori J, Yamazaki M, et al. Administration of recombinant human growth hormone normalizes GH-IGF1 axis and improves malnutrition-related disorders in patients with anorexia nervosa. Endocr J. 2007;54:319–27. doi: 10.1507/endocrj.k05-178. [DOI] [PubMed] [Google Scholar]
- 11.Riggs BL, Khosla S, Melton LJ., III Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev. 2002;23:279–302. doi: 10.1210/edrv.23.3.0465. [DOI] [PubMed] [Google Scholar]
- 12.Klibanski A, Biller B, Schoenfeld D, Herzog D, Saxe V. The effects of estrogen administration on trabecular bone loss in young women with anorexia nervosa. J Clin Endocrinol Metab. 1995;80:898–904. doi: 10.1210/jcem.80.3.7883849. [DOI] [PubMed] [Google Scholar]
- 13.Strokosch GR, Friedman AJ, Wu SC, Kamin M. Effects of an oral contraceptive (norgestimate/ethinyl estradiol) on bone mineral density in adolescent females with anorexia nervosa: a double-blind, placebo-controlled study. J Adolesc Health. 2006;39:819–27. doi: 10.1016/j.jadohealth.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Giustina A, Mazziotti G, Canalis E. Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev. 2008;29:535–59. doi: 10.1210/er.2007-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakasaki M, Yoshioka K, Miyamoto Y, Sasaki T, Yoshikawa H, Itoh K. IGF-I secreted by osteoblasts acts as a potent chemotactic factor for osteoblasts. Bone. 2008;43:869–79. doi: 10.1016/j.bone.2008.07.241. [DOI] [PubMed] [Google Scholar]
- 16.Ohlsson C, Bengtsson B, Isaksson O, Andreassen T, Slootweg M. Growth hormone and bone. Endocr Rev. 1998;19:55–79. doi: 10.1210/edrv.19.1.0324. [DOI] [PubMed] [Google Scholar]
- 17.Cara J, Rosenfield R, Furlanetto R. A longitudinal study of the relationship of plasma somatomedin-C concentration to the pubertal growth spurt. Am J Dis Child. 1987 May;141:562–4. doi: 10.1001/archpedi.1987.04460050104041. [DOI] [PubMed] [Google Scholar]
- 18.Soyka L, Misra M, Frenchman A, Miller K, Grinspoon S, Schoenfeld D, et al. Abnormal bone mineral accrual in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab. 2002;87:4177–85. doi: 10.1210/jc.2001-011889. [DOI] [PubMed] [Google Scholar]
- 19.Grinspoon S, Baum H, Lee K, Anderson E, Herzog D, Klibanski A. Effects of short-term recombinant human insulin-like growth factor I administration on bone turnover in osteopenic women with anorexia nervosa. J Clin Endocrinol Metab. 1996;81:3864–70. doi: 10.1210/jcem.81.11.8923830. [DOI] [PubMed] [Google Scholar]
- 20.Grinspoon S, Baum H, Peterson S, Klibanski A. Effects of rhIGF-I administration on bone turnover during short-term fasting. J Clin Invest. 1995;96:900–6. doi: 10.1172/JCI118137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mora S, Pitukcheewanont P, Kaufman FR, Nelson JC, Gilsanz V. Biochemical markers of bone turnover and the volume and the density of bone in children at different stages of sexual development. J Bone Miner Res. 1999;14:1664–71. doi: 10.1359/jbmr.1999.14.10.1664. [DOI] [PubMed] [Google Scholar]
- 22.Diagnostic and statistical manual of mental disorders. 34. Washington, D.C: American Psychiatric Association; 1987. pp. 65–7. revised 1987. [Google Scholar]
- 23.Greulich W, Pyle S. Radiographic atlas of skeletal development of the hand and wrist. 2. Stanford: Stanford University Press; 1959. [Google Scholar]
- 24.Grinspoon S, Thomas L, Miller K, Herzog D, Klibanski A. Effects of recombinant human IGF-I and oral contraceptive administration on bone density in anorexia nervosa. J Clin Endocrinol Metab. 2002;87:2883–91. doi: 10.1210/jcem.87.6.8574. [DOI] [PubMed] [Google Scholar]
- 25.Chernausek SD, Backeljauw PF, Frane J, Kuntze J, Underwood LE. Long-term treatment with recombinant insulin-like growth factor (IGF)-I in children with severe IGF-I deficiency due to growth hormone insensitivity. J Clin Endocrinol Metab. 2007;92:902–10. doi: 10.1210/jc.2006-1610. [DOI] [PubMed] [Google Scholar]
- 26.Case Records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Normal reference laboratory values (see comments) N Engl J Med. 1992;327:718–24. doi: 10.1056/NEJM199209033271009. [DOI] [PubMed] [Google Scholar]
- 27.Bachrach L. Acquisition of optimal bone mass in childhood and adolescence. Trends Endocrinol Metab. 2001;12:22–8. doi: 10.1016/s1043-2760(00)00336-2. [DOI] [PubMed] [Google Scholar]
- 28.Soyka L, Grinspoon S, Levitsky L, Herzog D, Klibanski A. The effects of anorexia nervosa on bone metabolism in female adolescents. J Clin Endocrinol Metab. 1999;84:4489–96. doi: 10.1210/jcem.84.12.6207. [DOI] [PubMed] [Google Scholar]
- 29.Misra M, Prabhakaran R, Miller KK, Goldstein MA, Mickley D, Clauss L, et al. Prognostic indicators of changes in bone density measures in adolescent girls with anorexia nervosa-II. J Clin Endocrinol Metab. 2008;93:1292–7. doi: 10.1210/jc.2007-2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hotta M, Shibasaki T, Sato K, Demura H. The importance of body weight history in the occurrence and recovery of osteoporosis in patients with anorexia nervosa: evaluation by dual X-ray absorptiometry and bone metabolic markers. Eur J Endocrinol. 1998;139:276–83. doi: 10.1530/eje.0.1390276. [DOI] [PubMed] [Google Scholar]
- 31.Misra M, Prabhakaran R, Miller KK, Goldstein MA, Mickley D, Clauss L, et al. Weight gain and restoration of menses as predictors of bone mineral density change in adolescent girls with anorexia nervosa-1. J Clin Endocrinol Metab. 2008;93:1231–7. doi: 10.1210/jc.2007-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Horwitz MJ, Tedesco MB, Sereika SM, Garcia-Ocana A, Bisello A, Hollis BW, et al. Safety and tolerability of subcutaneous PTHrP(1–36) in healthy human volunteers: a dose escalation study. Osteoporos Int. 2006;17:225–30. doi: 10.1007/s00198-005-1976-3. [DOI] [PubMed] [Google Scholar]
- 33.Plotkin H, Gundberg C, Mitnick M, Stewart AF. Dissociation of bone formation from resorption during 2-week treatment with human parathyroid hormone-related peptide-(1–36) in humans: potential as an anabolic therapy for osteoporosis. J Clin Endocrinol Metab. 1998;83:2786–91. doi: 10.1210/jcem.83.8.5047. [DOI] [PubMed] [Google Scholar]
- 34.Bilezikian JP. Combination anabolic and antiresorptive therapy for osteoporosis: opening the anabolic window. Curr Osteoporos Rep. 2008;6:24–30. doi: 10.1007/s11914-008-0005-9. [DOI] [PubMed] [Google Scholar]