Abstract
Context:
The epidemiology of primary hyperparathyroidism (PHPT) has generally been studied in Caucasian populations.
Objective:
The aim was to examine the incidence and prevalence of PHPT within a racially mixed population.
Design:
A descriptive epidemiologic study was performed.
Patients/Setting:
The study population included 3.5 million enrollees within Kaiser Permanente Southern California.
Methods:
All patients with at least one elevated serum calcium level (>10.5 mg/dL, 2.6 mmol/L) between 1995 and 2010 were included. Cases of PHPT were identified by electronic query of laboratory values using biochemical criteria, after exclusion of secondary or renal and tertiary hyperparathyroidism cases. The incidence and prevalence rates of PHPT were calculated according to sex, race, age group by decade, and year.
Results:
Initial case finding identified 15,234 patients with chronic hypercalcemia, 13,327 (87%) of which had PHPT as defined by elevated or inappropriately normal parathyroid hormone levels. The incidence of PHPT fluctuated from 34 to 120 per 100 000 person-years (mean 66) among women, and from 13 to 36 (mean 25) among men. With advancing age, incidence increased and sex differences became pronounced (incidence 12–24 per 100 000 for both sexes younger than 50 y; 80 and 36 per 100 000 for women and men aged 50–59 y, respectively; and 196 and 95 for women and men aged 70–79 y, respectively). The incidence of PHPT was highest among blacks (92 women; 46 men, P < .0001), followed by whites (81 women; 29 men), with rates for Asians (52 women, 28 men), Hispanics (49 women, 17 men), and other races (25 women, 6 men) being lower than that for whites (P < .0001). The prevalence of PHPT tripled during the study period, increasing from 76 to 233 per 100 000 women and from 30 to 85 per 100 000 men. Racial differences in prevalence mirrored those found in incidence.
Conclusions:
PHPT is the predominant cause of hypercalcemia and is increasingly prevalent. Substantial differences are found in the incidence and prevalence of PHPT between races.
Primary hyperparathyroidism (PHPT) is a relatively common endocrine disorder, with prevalence estimates of one to seven cases per 1000 adults (1–4). It is believed to be the most common cause of hypercalcemia, predominantly affecting elderly populations and women two to three times as often as men (5). To date, reports on the epidemiology of PHPT have been derived from geographic locations populated predominantly by Caucasian individuals, such as Sweden, Norway, Finland, Scotland, and Rochester, Minnesota. Therefore, such data may not accurately reflect patterns of disease across the racially diverse United States.
The incidence of PHPT has been difficult to assess. Available estimates vary widely from 0.4 to 21.6 cases per 100 000 person-years (4, 6). This variation arises from heterogeneity in screening methods, case definitions, the populations studied, and annual fluctuations in incidence within the same population that remain unexplained.
The aim of the current study is to determine the incidence and prevalence of PHPT in a racially mixed population by applying a uniform biochemical algorithm. Race- and age-related differences in incidence and prevalence are examined.
Subjects and Methods
Study population
The study population included all active enrollees in Kaiser Permanente Southern California (KPSC), an integrated health care delivery system serving approximately 3.5 million subscribers, representing 20% of the insured population in the region. The KPSC membership closely mirrors the population of the greater Los Angeles metropolitan area demographically and socioeconomically, except for the extremes of the income distribution (7, 8). Because most members receive employer-based insurance benefits, outmigration rates are low, with two-thirds of subscribers maintaining membership for 5 years or more.
Case definitions
After approval from the KPSC institutional review board, the Kaiser Permanente Medical Center laboratory management system was queried electronically to identify patients with a biochemical diagnosis of PHPT during the years 1995 through 2010. A three-level algorithm was employed to identify cases of PHPT strictly by biochemical criteria. Initial case finding was performed by identifying all patients with at least one elevated calcium level (serum calcium greater than 10.5 mg/dL [2.6 mmol/L ]; normal 8.5–10.5). Initial exclusions were applied to patients with membership terms of less than 6 mo, those younger than 20 y, and those with secondary (renal) hyperparathyroidism (serum creatinine greater than 2.5 mg/dL [221.0 mmol/L]). Any patient who had at least two separate blood samples drawn for cyclosporine, tacrolimus, or sirolimus levels was considered a likely kidney transplant recipient with possible tertiary hyperparathyroidism and was excluded.
Patients with classic PHPT were defined as those with hypercalcemia (serum calcium greater than 10.5 mg/dL) and parathyroid hormone (PTH) excess (PTH greater than 65 pg/mL [6.8 pmol/L]; normal 15–65). Patients with nonclassic PHPT were defined as those with hypercalcemia (serum calcium greater than 10.5 mg/dL) and inappropriately normal or nonsuppressed PTH levels ranging from 21 to 65 pg/mL. Patients not meeting either of these PTH criteria were followed up forward in time for a second high serum calcium level within 3 to 24 months to confirm chronic hypercalcemia. Patients with only a single high calcium level were considered spurious cases and excluded. Additional exclusions were applied to patients with a history of invasive cancer at any time before or within 24 months after the index high calcium date, those with a history of thiazide diuretic use (hydrochlorothiazide, chlorothiazide, chlorthalidone, metolazone, indapamide, methyclothiazide, alone or in combination) at any time before or within 24 months after the index high calcium date, and those with documented low PTH values less than 21 pg/mL. Invasive cancer diagnoses were determined using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 140 to 209 and 235 to 239 to encompass neoplasms of undetermined behavior or pathology. The remaining patients with chronic hypercalcemia, unknown PTH levels, and no thiazide use or invasive cancer were considered cases of possible PHPT.
Defining age, sex, and race
After case identification, laboratory data were linked to demographic information within the KPSC discharge abstract database. Adult women and men 20 years or older were included in the sample. Age ranged from 20 to 99 years. To study age differences in incidence and prevalence, seven age groups were created (20–29, 30–39, 40–49, 50–59, 60–69, 70–79, >80 y). Patients were classified by race and ethnicity as Asian, black, Hispanic, and white. The category “other” was used to include patients whose race or ethnicity were coded as “other” or who did not provide any information.
Statistical analysis
For each year, incidence was defined as the number of PHPT cases per year divided by number of KPSC enrollees for the same year. Cases were selected into a given year based on the index date (date of initial high calcium level). The ratio of PHPT in women to men has been reported to range from 2:1 to 3:1 (6). Consequently, to avoid an averaging effect that would yield figures applicable to neither sex, crude and age-adjusted incidence rates were calculated separately for women and men. Within each gender, annual rates were also calculated by race and by age group. Age-adjusted incidence was estimated by applying population data from the 2000 US Census (9). Confidence intervals for incidence were assumed to follow a Poisson distribution and were estimated by applying appropriate correction factors (10).
Once cases were categorized into classic, nonclassic, or possible PHPT, prevalence rates were calculated by tracking biochemical values over time. As long as a given case continued to have high serum calcium levels over the course of the patient's KPSC membership, the case was included as part of the annual prevalence of PHPT. Prevalence was censored for a case once a patient received a curative parathyroidectomy, had no high calcium levels recorded in a given year, was no longer actively enrolled in KPSC, or died. Prevalence rates used the same denominator as incidence. Crude and age-adjusted prevalence rates were calculated, and confidence intervals were estimated assuming a binomial distribution.
Results
The KPSC population grew from 1 179 690 to 2 044 305 members from 1995 to 2010. The population was 53.8% female and 63.3% nonwhite (Table 1). The mean intact PTH level in the classic PHPT group was 128.2 pg/mL compared with 40.0 pg/mL in the nonclassic PHPT group (Table 2). Despite the large difference in the PTH levels, the serum calcium levels were only slightly higher in the classic PHPT group (11.2 vs 10.9 mg/dL).
Table 1.
Demographics of Kaiser Permanente Southern California Population, 1995–2010
| KPSC Sample | N (Mean) | N (Range) | % |
|---|---|---|---|
| Population | 1 760 386 | 1 179 690–2 135 390 | 100.0 |
| Sex | |||
| Women | 947 754 | 771 767–1 006 511 | 53.8 |
| Men | 812 632 | 407 929–1 037 794 | 46.2 |
| Race | |||
| Asian | 87 373 | 27 097–116 895 | 5.0 |
| Black | 153 991 | 124 502–179 284 | 8.8 |
| Hispanic | 466 912 | 185 233–672 078 | 26.5 |
| Other | 405 727 | 192 576–620 309 | 23.0 |
| White | 646 383 | 592 011–703 725 | 36.7 |
Table 2.
Demographic and Biochemical Features of Primary Hyperparathyroidism Cases
| N (%) | Age, Mean (SD) | Serum Calcium (mg/dL), Mean (SD) | Intact PTH (pg/mL), Mean (SD) | |
|---|---|---|---|---|
| Classic PHPT | ||||
| Total | 6868 (100.0) | 64.0 (13.4) | 11.2 (0.7) | 128.2 (86.3) |
| Gender | ||||
| Women | 5311 (77.3) | 64.7 (12.8) | 11.3 (0.6) | 125.7 (82.6) |
| Men | 1,557 (22.7) | 61.9 (14.8) | 11.2 (0.8) | 136.9 (97.3) |
| Race | ||||
| Asian | 335 (4.9) | 60.5 (12.8) | 11.2 (0.6) | 132.5 (96.7) |
| Black | 1191 (17.3) | 64.2 (12.6) | 11.2 (0.7) | 137.9 (99.1) |
| Hispanic | 1054 (15.3) | 58.9 (14.2) | 11.2 (0.7) | 124.5 (102.8) |
| Other | 415 (6.1) | 61.0 (13.4) | 11.1 (0.5) | 118.8 (66.9) |
| White | 3873 (56.4) | 66.0 (12.9) | 11.1 (0.7) | 122.0 (76.7) |
| Nonclassic PHPT | ||||
| Total | 6459 (100.0) | 62.3 (13.8) | 10.9 (0.5) | 40.0 (12.4) |
| Gender | ||||
| Women | 5054 (78.2) | 63.9 (12.8) | 10.9 (0.5) | 40.2 (12.4) |
| Men | 1405 (21.8) | 56.7 (15.8) | 11.0 (0.5) | 39.2 (12.3) |
| Race | ||||
| Asian | 409 (6.3) | 60.3 (13.4) | 10.9 (0.3) | 38.3 (12.7) |
| Black | 681 (10.5) | 61.4 (13.2) | 11.0 (0.6) | 42.0 (12.8) |
| Hispanic | 694 (10.7) | 57.7 (14.9) | 11.0 (0.6) | 40.5 (12.5) |
| Other | 615 (9.5) | 56.0 (14.0) | 10.9 (0.3) | 39.8 (12.1) |
| White | 4060 (62.9) | 64.4 (13.2) | 10.9 (0.5) | 39.8 (12.3) |
| Possible PHPT | ||||
| Total | 452 (100.0) | 57.0 (17.6) | 10.9 (0.4) | |
| Gender | ||||
| Women | 287 (63.5) | 59.6 (17.9) | 10.9 (0.4) | |
| Men | 165 (36.5) | 52.6 (16.2) | 10.9 (0.4) | |
| Race | ||||
| Asian | 28 (6.2) | 52.9 (17.9) | 10.8 (0.2) | |
| Black | 61 (13.5) | 52.3 (15.6) | 10.9 (0.4) | |
| Hispanic | 93 (20.6) | 50.1 (16.7) | 10.9 (0.4) | |
| Other | 34 (7.5) | 49.8 (16.3) | 10.8 (0.3) | |
| White | 234 (51.8) | 62.7 (16.6) | 10.9 (0.4) |
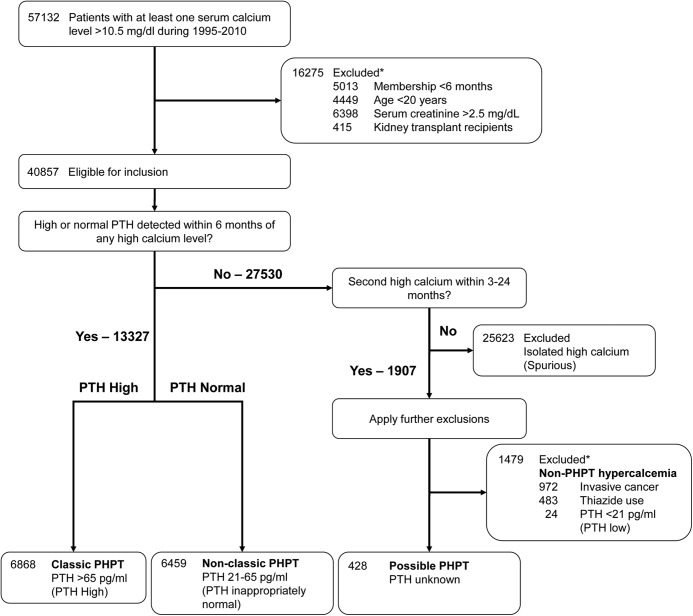
Initial case finding yielded 57 132 subjects with at least one elevated serum calcium level during the study period (Figure 1), of which 40 857 were eligible for inclusion. Of the 13 327 with documented high or normal PTH levels, 6868 were categorized as having classic PHPT (PTH > 65 pg/mL) and 6459 were categorized as having nonclassic PHPT (PTH 21–65 pg/mL). All of these patients had chronic hypercalcemia as defined by multiple instances of high serum calcium on different dates. Of the 27 530 patients without documented high or normal PTH levels, 25 623 were spurious cases with no additional episodes of hypercalcemia within 3 to 24 months of the index high calcium date. Additional exclusions were applied to the 1907 remaining patients with chronic hypercalcemia, 1479 of whom had non-PHPT hypercalcemia as explained by invasive cancer, thiazide diuretic use, or a documented low PTH level of less than 21 pg/mL. Unexplained chronic hypercalcemia was found in 428 patients with unknown PTH levels, and these patients were categorized as having possible PHPT.
Figure 1.
Case definitions. PHPT, primary hyperparathyroidism; PTH, parathyroid hormone. Normal PTH 21 to 65 pg/mL (2.2–6.8 pmol/L).
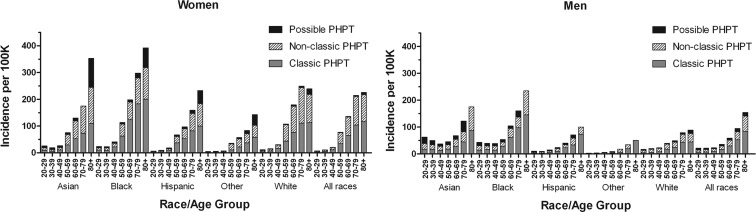
The age-adjusted incidence of PHPT (classic, nonclassic, and possible combined) fluctuated between 34.0 and 120.2 in women and 13.4 and 35.6 in men, with an average incidence of 65.5 and 24.7 over the entire study period for women and men, respectively (Figure 2). The incidence of classic PHPT ranged from 17.6 to 48.5 per 100 000 person-years among women, and from 7.2 to 20.9 per 100 000 person-years among men (Supplemental Table 1). (Please see Supplemental Table 1 published on The Endocrine Society's Journals Online web site at http://jcem.endojournals.org.) The incidence of nonclassic PHPT varied from 12.6 to 72.2 per 100 000 person-years among women and from 4.0 to 15.8 per 100 000 person-years among men. The incidence of possible PHPT was relatively low, ranging from one to eight cases per 100 000 person-years for both women and men. Over the 15-year period, the incidence of PHPT was consistently higher among women than men, with an incidence ratio ranging from 1.8 to 4.0 (mean incidence ratio 2.7).
Figure 2.
Age-adjusted incidence of primary hyperparathyroidism by year, women and men. PHPT, primary hyperparathyroidism.
The proportion of KPSC enrollees with at least one serum calcium test drawn per year grew steadily from 6.8% in 1995 to 12.7% in 2010 for women, and from 5.3% to 8.9% in men (Supplemental Table 1); this figure did not correlate with the incidence of PHPT in the population for either sex. We noted racial differences in the proportion of patients with at least one calcium test per year, with the black women having the highest rate of calcium testing (13.0%), followed by whites (12.9%), Asians (9.1%), Hispanics (7.7%), and other (4.2%; P < .0001). A similar pattern was observed among men, with blacks having the highest rate of calcium testing (11.9%), followed by whites (10.4%), Asians (8.8%), Hispanics (6.4%), and other (2.3%; P < .0001). These differences in the frequency of calcium testing did not correlate with race-specific PHPT incidence rates.
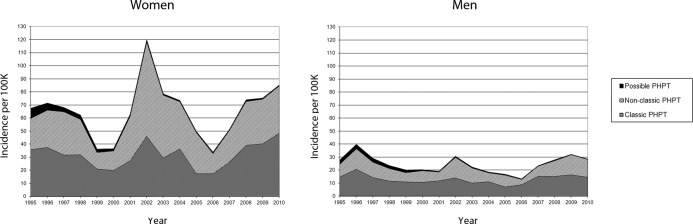
Incidence rates were analyzed separately according to sex, race, and age group by decade (Figure 3, Supplemental Table 2). For those younger than 50 years, incidence rates were generally low and similar across the sexes (incidence 12.1–24.4 per 100 000 person-years, all races). With advancing age, incidence increased and sex differences became pronounced. For patients 50–59 years, the incidence was 79.6 per 100 000 person-years for women and 35.6 per 100 000 person-years for men (all races). For patients 70–79 years, the incidence was 195.7 per 100 000 person-years for women and 94.6 per 100 000 person-years for men (all races).
Figure 3.
Incidence of primary hyperparathyroidism (crude) by race and age group, all years, women and men. PHPT, primary hyperparathyroidism.
The age-adjusted incidence of PHPT was highest among blacks (92.0 women; 46.0 men, P < .0001) followed by whites (81.0 women; 29.4 men), with rates for Asians (51.8 women, 27.9 men), Hispanics (48.6 women, 17.1 men), and other races (25.4 women, 5.9 men) being lower than that for whites (P < .0001). Racial differences also became more pronounced among older patients.
The age-adjusted prevalence of PHPT climbed from 76.3 to 232.7 per 100 000 among women, and from 29.5 to 85.2 per 100 000 among men during the study period (Figure 4, Supplemental Table 3). This growth was almost entirely attributable to an increase in the prevalence of classic PHPT. The prevalence ratio of female-to-male cases remained stable at approximately 2.5 to 1 when all age groups and races were considered together.
Figure 4.
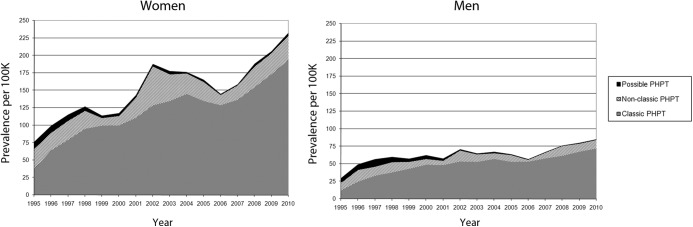
Age-adjusted prevalence of primary hyperparathyroidism by year, women and men. PHPT, primary hyperparathyroidism.
Prevalence rates were then analyzed separately according to sex, race, and age by decade (Figure 5, Supplemental Table 4). The prevalence of PHPT rose with increasing age, peaking at an average of 492.2 per 100 000 women aged 70–79 years and 264.1 per 100 000 men aged 80 years or older. PHPT was most prevalent among older blacks, affecting 921.5 per 100 000 black women aged 70–79 y (vs 630.3 per 100 000 in similarly aged whites, P < .0001), and 481.1 per 100 000 black men aged 80 years or older (vs 164.7 per 100 000 in similarly aged whites, P < .0001).
Figure 5.
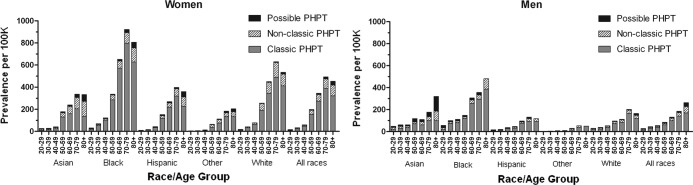
Prevalence of primary hyperparathyroidism (crude) by race and age group, all years, women and men. PHPT, primary hyperparathyroidism.
Because prevalence rates tripled over the study period, the year 2010 was analyzed separately to provide a reflection of the present (Supplemental Table 5). The highest age-adjusted prevalence rates during that year remained in black women (447.9 per 100 000), followed by whites (312.0), Asians (183.7), Hispanics (169.4), and other (46.2). The same pattern was observed among men, with black men having the highest age-adjusted prevalence of 177.5 per 100 000, followed by whites (103.1), Asians (71.8), Hispanics (54.8), and other (12.0) The highest overall prevalence rate found in the study was 1408.9, representing black women aged 70–79 years in 2010.
Vitamin D levels were available in 30% of subjects (Supplemental Table 6). Rates of vitamin D deficiency (as defined by a 25-hydroxy vitamin D level < 20 ng/mL) were lowest among whites (11.3%) and Asians (11.3%) and highest among blacks (30.9%, P = .004).
Discussion
The current study, encompassing 13 779 patients with PHPT, is the largest such series reported to our knowledge. Previously published series have included as many as 9782 patients in Europe (4, 11, 12) and 475 patients in the United States (3). We have described racial differences in the incidence and prevalence of PHPT, something not previously achievable because all previous studies have examined populations comprised of 90% or more white individuals. We believe that our findings are reflective of the larger US population.
The large sample size has allowed us to calculate incidence and prevalence rates split along the three axes of sex, race, and age by decade, while maintaining adequate statistical power to make intergroup comparisons. Previously, the most frequently reported statistic on PHPT incidence in the United States was 21.6 cases per 100 000 person-years, as calculated from an analysis of residents of Rochester, Minnesota (6). We found that the incidence of PHPT fluctuated between 36.3 and 120.2 in women and 13.4 and 35.6 in men, with an average incidence of 65.5 and 24.7 over the entire study period for women and men, respectively. Similar fluctuations in incidence have been observed in other studies (3, 4) and remain unexplained. The fluctuations we observed did not correlate with the frequency of calcium testing, which increased steadily during the study period across all sex, race, and age groups. Most European studies have reported relatively low incidence rates of less than 6 per 100 000 person-years (12, 13). One study examining residents of Tayside, Scotland, reported slightly higher incidence rates of 57.8 to 146.0 per 100 000 person-years for women and 22.8 to 79.5 per 100 000 person-years for men, figures that parallel our findings.
The prevalence of PHPT increased by a factor of 3.05 in women and 2.89 in men over the study period. We attribute this growth to the accumulation of cases through routine calcium testing; annual biochemical monitoring of patients with classic PHPT, which ensures retention within the cohort; and a relatively low rate of exit through surgical treatment. We have documented previously that 28% of patients with PHPT undergo surgery (14). The age and gender distribution of our cohort remained stable over the study period.
We have discovered substantial racial differences in the incidence and prevalence of PHPT, with the highest rates observed consistently in older black women. This finding raises a series of questions that have been altogether unexplored, most notably, do blacks therefore experience the adverse health effects of PHPT more commonly than do other races? Black American physiology is characterized by higher PTH levels, lower vitamin D levels, and a reduced risk of osteoporotic fracture compared with those of other races (15–18). These distinctive features of calcium homeostasis in this racial group have raised questions regarding whether the established normal range for vitamin D is appropriate for blacks (19).
Our study has a number of other salient findings. Although PHPT is acknowledged to be the most common cause of hypercalcemia in ambulatory patients (20), our ability to electronically identify all elevated calcium levels has led to the discovery that 90% of all chronic hypercalcemia is attributable to PHPT. This remarkably high proportion serves as a reminder that all patients with hypercalcemia should have their PTH levels measured because heightened attention to this diagnosis may yield opportunities for fracture prevention. We also found that, of patients with PHPT, only half have the classic form of the disease, characterized by elevations of both serum calcium and PTH. The remaining half represent nonclassic cases with high serum calcium and inappropriately normal or nonsuppressed PTH levels. In principle, the distinction between the two is artificial because both forms of the disease are characterized by inappropriate PTH excess and follow the same demographic patterns. However, in clinical practice we have observed considerable confusion regarding nonclassic PHPT cases. Patients with classic PHPT were closely monitored with annual calcium testing, which was responsible for the steady increase in the prevalence of these cases; they also commonly underwent bone mineral density measurement as recommended by consensus guidelines (21). In contrast, patients with nonclassic PHPT were inconsistently monitored, rarely underwent bone density measurement, and very rarely were referred for surgery, despite usually having hypercalcemia of a degree similar to that of patients with classic PHPT. This large group of patients merits clinical attention and further characterization in the literature.
Unique to our study is the strictly biochemical algorithm of identifying PHPT cases, which carries numerous strengths and several weaknesses. Previous epidemiologic studies have captured cases using a combination of biochemical, histopathologic, radiologic, and clinical data sources (1, 3, 4, 12, 13, 22), likely because the biochemical data may have been less broadly available in these study settings than in ours. PHPT is fundamentally a biochemical disease; establishing the diagnosis hinges entirely on demonstration of inappropriate PTH excess, and confirmation of surgical cure rests entirely on demonstration of having appropriate PTH levels restored. All other data sources carry considerable ascertainment bias. Histopathologic data would yield a higher detection rate for the minority of patients treated surgically. Furthermore, histopathologic evidence of parathyroid adenomas can be found incidentally in eucalcemic individuals undergoing thyroidectomy; these patients cannot be considered to have PHPT (23). Radiologic studies have sensitivities and specificities that are far from 100%; there is consensus that imaging is not an appropriate method of diagnosing PHPT (24). Clinical data would rely upon the skill of the physician and his or her attentiveness to the diagnosis of PHPT, which is highly variable (14).
Although our algorithm was designed to be highly sensitive, the priority was specificity, that is, avoidance of sample contamination with non-PHPT cases. Thus, we may have slightly underestimated the incidence and prevalence of PHPT by excluding the following types of patients: those with PHPT and renal impairment (serum creatinine >2.5 mg/dL), those with PHPT who are also taking a thiazide diuretic, and those with PHPT and a history of invasive cancer. In fact, because hypercalcemia is an uncommon complication of malignancy, it is likely that most patients we excluded using the invasive cancer criterion actually had PHPT (25). Because urine calcium measurements were available only in a minority of subjects, we acknowledge that our sample may be contaminated with a small number of patients with familial hypocalciuric hypercalcemia, which has an estimated prevalence of 1 in 78,000 (26). The small population of patients with possible PHPT may be contaminated with a few patients with non-PHPT hypercalcemia of uncommon origin, such as hypervitaminosis D, milk-alkali syndrome, thyroid dysfunction, or sarcoidosis (20). It is important to note that our population is completely covered by private health insurance and thus unaffected by biases related to access to care. For these reasons, we believe our incidence and prevalence figures are as objective and unbiased as possible.
In conclusion, we have identified the largest population-based cohort of patients with PHPT described to date and have documented racial differences in the incidence and prevalence of PHPT for the first time. Given that published longitudinal series on the long-term effects of this disease have involved relatively low sample sizes, additional study of this cohort should shed light on the natural history of PHPT and the effectiveness of different management strategies on long-term skeletal and extraskeletal outcomes. Moreover, additional study regarding racial differences in the biochemical and clinical manifestations of this disease is warranted.
Supplementary Material
Acknowledgments
Annette L. Adams had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was approved by the Institutional Review Boards of both UCLA David Geffen School of Medicine and Kaiser Permanente Southern California.
This study was supported by the National Institutes of Health/National Institute on Aging (RFA-AG-11-007), the American Geriatrics Society, and the Earl Gales Family Foundation.
Disclosures: The authors have no conflicts of interest to disclose.
Footnotes
- KPSC
- Kaiser Permanente Southern California
- PHPT
- primary hyperparathyroidism
- PTH
- parathyroid hormone.
References
- 1. Adami S, Marcocci C, Gatti D. Epidemiology of primary hyperparathyroidism in Europe. J Bone Miner Res. 2002;17:N18–N23 [PubMed] [Google Scholar]
- 2. Christensson T, Hellström K, Wengle B, Alveryd A, Wikland B. Prevalence of hypercalcaemia in a health screening in Stockholm. Acta Med Scand. 1976;200:131–137 [DOI] [PubMed] [Google Scholar]
- 3. Wermers RA, Khosla S, Atkinson EJ, et al. The rise and fall of primary hyperparathyroidism: a population-based study in Rochester, Minnesota, 1965–1992. Ann Intern Med. 1997;126(6):433–440 [DOI] [PubMed] [Google Scholar]
- 4. Yu N, Donnan PT, Murphy MJ, Leese GP. Epidemiology of primary hyperparathyroidism in Tayside, Scotland, UK. Clin Endocrinol. 2009;71(4):485–493 [DOI] [PubMed] [Google Scholar]
- 5. Fraser WD. Hyperparathyroidism. Lancet. 2009;374(9684): 145–58 [DOI] [PubMed] [Google Scholar]
- 6. Wermers RA, Khosla S, Atkinson EJ, et al. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: An update on the changing epidemiology of the disease. J Bone Miner Res. 2006;21(1):171–177 [DOI] [PubMed] [Google Scholar]
- 7. Writing Group for the SEARCH for Diabetes in Youth Study Group, Dabelea D, Bell RA, et al. Incidence of diabetes in youth in the United States. JAMA. 2007;297(24):2716–2724 [DOI] [PubMed] [Google Scholar]
- 8. Lawrence JM, Lukacz ES, Nager CW, Hsu JW, Luber KM. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet Gynecol. 2008;111(3):678–685 [DOI] [PubMed] [Google Scholar]
- 9. Pagano M, Gauvreau K. Principles of Biostatistics. Belmont, CA: Duxbury Press; 1993 [Google Scholar]
- 10. Sahai H, Khurshid A. Confidence intervals for the mean of a Poisson distribution: A review. Biometrical J. 1993;35(7):857–867 [Google Scholar]
- 11. Nilsson I-L, Wadsten C, Brandt L, Rastad J, Ekbom Mortality in sporadic primary hyperparathyroidism: Nationwide cohort study of multiple parathyroid gland disease. Surgery. 2004;136(5):981–987 [DOI] [PubMed] [Google Scholar]
- 12. Vestergaard P, Mosekilde L. Cohort study on effects of parathyroid surgery on multiple outcomes in primary hyperparathyroidism. BMJ. 2003;327(7414):530–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Richert L, Trombetti A, Herrmann FR, et al. Age and gender distribution of primary hyperparathyroidism and incidence of surgical treatment in a European country with a particularly high life expectancy. Swiss Med Wkly. 2009;139(27–28):400–404 [DOI] [PubMed] [Google Scholar]
- 14. Yeh MW, Wiseman JE, Ituarte PH, et al. Surgery for primary hyperparathyroidism: are the consensus guidelines being followed? Ann Surg. 2012;255(6):1179–1183 [DOI] [PubMed] [Google Scholar]
- 15. Aloia JF. African Americans, 25-hydroxyvitamin D, and osteoporosis: a paradox. Am J Clin Nutr. 2008;88(2):545S–550S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Aloia JF, Chen DG, Chen H. The 25(OH)D/PTH threshold in black women. J Clin Endocrinol Metab. 2010;95(11):5069–5073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cauley JA, Danielson ME, Boudreau R, et al. Serum 25-hydroxyvitamin D and clinical fracture risk in a multiethnic cohort of women: the Women's Health Initiative (WHI). J Bone Miner Res. 2011;26(10):2378–2388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Golden SH, Brown A, Cauley JA, et al. Health disparities in endocrine disorders: biological, clinical, and nonclinical factors—an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2012;97:E1579–E1639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wright N, Chen L, Niu J, et al. Defining physiologically ‘normal’ vitamin D in African Americans. Osteoporos Int. 2012;23:2283–2289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lafferty FW. Differential diagnosis of hypercalcemia. J Bone Miner Res. 1991;6(S2):S51–S59 [DOI] [PubMed] [Google Scholar]
- 21. Bilezikian JP, Khan AA, Potts JT, Jr, the Third International Workshop on the Management of Asymptomatic Primary Hyperthyroidism Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Third International Workshop. J Clin Endocrinol Metab. 2009;94(2):335–339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dedov II, Mokrysheva NG, Mirnaya SS, et al. Epidemiology of primary hyperparathyroidism in Russia (the first results from the database of federal state institution ‘Endocrinological Research Centre’). Problemy Endokrinologii. 2011;57(3):3–10 [Google Scholar]
- 23. Carnaille BM, Pattou FN, Oudar C, Lecomte-Houcke MC, Rocha JE, Proye CA. Parathyroid incidentalomas in normocalcemic patients during thyroid surgery. World J Surg. 1996;20(7):830–834 [DOI] [PubMed] [Google Scholar]
- 24. Udelsman R, Pasieka JL, Sturgeon C, Young JEM, Clark OH. Surgery for asymptomatic primary hyperparathyroidism: proceedings of the Third International Workshop. J Clin Endocrinol Metab. 2009;94(2):366–372 [DOI] [PubMed] [Google Scholar]
- 25. Vassilopoulou-Sellin R, Newman BM, Taylor SH, Guinee VF. Incidence of hypercalcemia in patients with malignancy referred to a comprehensive cancer center. Cancer. 1993;71(4):1309–1312 [DOI] [PubMed] [Google Scholar]
- 26. Glendenning P, Stuckey BG. The estimated prevalence of familial hypocalciuric hypercalcemia (FHH). Calcif Tissue Int. 2002;70(6):512. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.