Abstract
Context:
African American (AA) women have the highest rates of premenopausal breast cancer; however, it is unclear whether body size contributes to the hormonal patterns potentially associated with increased breast cancer risk in these women.
Objective:
To characterize the association between body size and serum levels of estradiol and sex hormone-binding globulin (SHBG) levels in a sample of premenopausal AA women.
Design:
A total of 164 premenopausal AA women who were not pregnant or breastfeeding were recruited for this study. Serum samples were collected during the early follicular phase, and trained staff collected body size measurements. Multiple linear regression models were performed to assess potential associations.
Main Outcome Measures:
Serum estradiol and SHBG levels.
Results:
Many (81%) of the women enrolled were overweight or obese. Both waist-to-hip ratio (WHR) (β = 2.68, P = .008) and waist circumference (WC) (β = 2.02, P = .046) were positively associated with higher levels of estradiol. All measures of body was significantly and inversely associated with SHBG levels (all P < .05).
Conclusions:
Premenopausal AA women with higher WHR or larger WC may have higher levels of estradiol and lower levels of SHBG. Thus, WHR or WC may be better indicators for assessing hormonal patterns implicated in breast cancer pathogenesis in these women.
Obesity is a known risk factor for breast cancer (1); however, the extent of the association varies according to several factors, including race/ethnicity and menopausal status (2). In African American (AA) women, the relationship between obesity and breast cancer risk has been inconsistent (3, 4). Thus, data related to the role of risk factors and breast cancer risk in AA women remains speculative.
Inconsistencies in reported associations between obesity and breast cancer risk may be attributed to the measurement of obesity. Historically, epidemiologic studies relied exclusively on body mass index (BMI) to approximate obesity, despite evidence that BMI is a poor proxy (5). Studies have proposed that measures of body fat distribution, such as abdominal obesity, may be more accurate (6). Abdominal obesity generally increases premenopausal breast cancer risk in all women and postmenopausal breast cancer risk in AA women (2, 3). In addition, abdominal obesity is associated with aggressive breast cancer subtypes (7). Thus, abdominal obesity in AA women may increase their risk for premenopausal breast cancer (8).
Obesity contributes to breast carcinogenesis by modulating metabolic and sex hormone pathways, which are known to promote breast carcinogenesis (9). Typically, obesity is associated with higher levels of estradiol, which stimulate the proliferation of breast epithelial cells (10), and lower levels of sex hormone-binding globulin (SHBG). SHBG is inversely associated with the risk of obesity and may be an important mediator of tumorigenesis because of its binding to estradiol and testosterone, which are biomarkers known to adversely affect breast cancer risk (10). Consistent with the hypothesis that obesity influences levels of sex hormones and binding proteins, previous studies have shown that AA women have higher plasma concentrations of estradiol and lower concentrations of SHBG than do non-Hispanic Caucasian (CA) women, independent of abdominal obesity (11).
Despite substantial evidence that AA women have patterns of risk factors (eg, hormone concentrations and obesity) that place them at a greater risk for premenopausal breast cancer than that of other racial and ethnic groups (2), few studies have sought to determine whether the associations between obesity and plasma concentrations of estradiol and SHBG differ according to indicators of body size. Thus, the purpose of this study was to characterize the associations between multiple measures of body size and plasma concentrations of total estradiol and SHBG in AA women. We hypothesized that significant associations between body size, serum estradiol, and SHBG levels may indicate potential hormonal abnormalities and provide the rationale for further research.
Materials and Methods
Serum samples were obtained from women participating in the African American Nutrition for Life intervention study (12). Premenopausal AA women who had no preexisting chronic illness and who consumed at least 28% of their calories from fat were eligible for participation. In addition, stringent exclusion criteria were applied: women were excluded if they were currently using hormone replacement therapy, oral contraceptives, or other lipid or endocrine hormone-altering medications; planning a pregnancy, currently pregnant, or breastfeeding; or had previous diagnosis of cancer (except nonmelanoma skin cancers and cervical carcinoma in situ) (12). The Institutional Review Board at The University of Texas MD Anderson Cancer Center approved the study.
Measures
Biochemical analysis
A fasting, early follicular phase blood sample was obtained at baseline from each participant within 5 days of cessation of menses. The blood samples collected were then centrifuged, the serum collected, aliquoted into a light-protected amber tubes, and stored at −80°C until the time of analysis. Circulating estradiol and SHBG levels were assessed using commercial enzyme-linked immunosorbent assay kits from BioCheck, Inc (Foster City, California) and ALPCO Diagnostics (Salem, New Hampshire), respectively, per the manufacturers' instructions. Briefly, 25 μL standard, sample, or control sera were added to the appropriate wells followed by the addition of 100 μL estradiol-horseradish peroxidase conjugate reagent and 50 μL rabbit antiestradiol reagent. A tetramethylbenzidine reagent was then added, and the reaction was stopped with 100 μL of 1 N sulfuric acid. The plate was then read at an absorbance level of 450 nm. Total estradiol and SHBG levels were calculated on the basis of the standard linear curve. All samples were diluted 1:10 before analysis of SHBG levels. The intra- and interassay variations for estradiol were 5.3% and 9.0%, respectively, and 7.1% and 12.0%, respectively for SHBG.
Anthropometric indicators
Participants in this study underwent whole-body scans using dual-energy x-ray absorptiometry (DPX-L 2288 densitometer; Lunar Corp, Madison, Wisconsin). Participants' height, weight, waist circumference (WC), hip circumference (HC), and percentage of body fat were also recorded by a study dietitian upon the participants' enrollment. Height was measured to the nearest centimeter, and weight was measured to the nearest 0.1 kg on an electric scale while participants were wearing lightweight clothing. WC and HC were measured in a horizontal line at the narrowest circumference above the umbilicus and at the largest circumference of the hips, respectively. BMI (weight in kilograms/height in meters squared [kg/m2]) and waist-to-hip ratio (WHR) also were calculated.
Lifestyle characteristics
Participants self-reported their current age, age at menarche, age at first live birth, socioeconomic status (ie, education), smoking status, marital status, and dietary intake during the first clinic visit. Dietary intake was assessed with the Arizona Food Frequency Questionnaire (13). Total caloric intake was used to approximate diet.
Statistical analysis
Descriptive statistics were used to summarize study population data. Serum levels of estradiol and SHBG were summarized using geometric means and 95% confidence intervals due to the skewed nature of their distributions. Estradiol was square-root transformed before its relationship with body size indicators was assessed. SHBG was left on its original scale. Multiple linear regression models were used to assess the association between body size indicators and serum hormone levels while adjusting for the following covariates: current age, age at menarche, parity, smoking status, and total caloric intake. Subsequent models testing for interactions between body size and age at menarche, current age, and age at first live birth were examined. P values < .05 set the criteria for considering statistical significance.
Results
Medical, anthropometric, and demographic characteristics
The study population included 164 participants, most of whom were 36 to 45 years old, single, nonsmokers, college educated, and obese (Table 1). The average age at first live birth was 24 years, and most women had at least one child.
Table 1.
Descriptive Characteristics of Study Participants
| Characteristics | % Difference | n (%) | |
|---|---|---|---|
| Age, y | |||
| Mean ± SD | 36.7 ± 5.2 | 164a | |
| Age groups | |||
| 25–35 y | 62 (38) | ||
| 36–45 y | 102 (62) | ||
| Age at menarche, y | |||
| Mean ± SD | 12.5 ± 1.7 | 147a | |
| Age at first live birth, y | |||
| Mean ± SD | 23.6 ± 6.0 | 107a | |
| Parity | |||
| No children | 49 (31) | ||
| 1 or more children | 107 (69) | ||
| Marital status | |||
| Single | 56 (34) | ||
| Married | 87 (53) | ||
| Other | 21 (13) | ||
| Education | |||
| ≤ High school | 25 (15) | ||
| Some college or technical school | 21 (13) | ||
| ≥ College graduate | 118 (72) | ||
| Current Smoker | |||
| No | 138 (85) | ||
| Yes | 25 (15) | ||
| BMI, kg/m2 | |||
| Mean ± SD | 32.0 ± 8.1 | 150a | |
| BMI categories | |||
| Normal (<25 kg/m2) | 28 (19) | ||
| Overweight (between 25 and 30 kg/m2) | 42 (28) | ||
| Obese (>30 kg/m2) | 80 (53) | ||
| Serum SHBG levels, nmol/L | |||
| GeoMean (95% CI) | 97.1 (88.2, 106.9) | 154a | |
| In categories of WC | |||
| Category 1 (<81.34 cm) | 143.1 (126.3, 162.2) | 37a | |
| Category 2 (81.34–89.80 cm) | 98.6 (81.6, 119.1) | 36.8% | 35a |
| Category 3 (89.80–104.90 cm) | 92.9 (80.2, 107.6) | 42.5% | 36a |
| Category 4 (>104.90 cm) | 63.8 (49.8, 81.7) | 76.7% | 35a |
| In categories of WHR | |||
| Category 1 (<0.74) | 121.3 (103.9, 141.6) | 35a | |
| Category 2 (0.74–0.80) | 106.7 (91.1, 124.9) | 12.8% | 36a |
| Category 3 (0.80–0.86) | 89.8 (74.0, 109.1) | 29.8% | 36a |
| Category 4 (>0.86) | 74.0 (57.0, 96.0) | 48.4% | 36a |
| Serum total estradiol (pg/mL) | |||
| GeoMean (95% CI) | 151.2 (127.9, 178.6) | 135a | |
| In categories of WC | |||
| Category 1 (<81.34 cm) | 135.6 (99.4, 185.1) | 32a | |
| Category 2 (81.34–89.80 cm) | 158.9 (114.0, 221.4) | 15.8% | 30a |
| Category 3 (89.80–104.90 cm) | 151.6 (109.8, 209.4) | 11.4% | 31a |
| Category 4 (>104.90 cm) | 165.9 (119.6, 230.1) | 20.1% | 32a |
| In categories of WHR | |||
| Category 1 (<0.74) | 108.4 (72.8, 161.3) | 31a | |
| Category 2 (0.74–0.80) | 142.7 (105.5, 193.2) | 27.3% | 29a |
| Category 3 (0.80–0.86) | 213.2 (165.8, 274.1) | 65.2% | 31a |
| Category 4 (> 0.86) | 162.3 (122.0, 216.0) | 39.8% | 34a |
Abbreviations: CI, confidence interval; GeoMean, geometric mean.
Number of responses used to compute summary statistics. “Other” category consists of participants who were divorced, separated, or widowed. Women were excluded from the study if they reported oral contraceptive use or anovulatory cycles.
Anthropometric indicators, estradiol, and SHBG
For serum SHBG, differences of 76.7% and 48.4% for WC and WHR, respectively, were observed when considering lowest and highest categories. In addition, for serum estradiol differences of 20.1% and 39.8% for WC and WHR, respectively, were observed (Table 1).
A positive linear relationship was observed between WHR and total estradiol levels (β = 2.68, P = .008) and WC and total estradiol levels (β = 2.02, P = .046) after adjusting for key covariates of interest (Table 2; Figure 1). No other significant associations were observed between body size and serum measures of estradiol. In general, the anthropometric indicators and serum SHBG levels had a significant inverse relationship after adjusting for key covariates of interest (Table 2). No significant interaction effects were observed between the covariates (current age, age at menarche, parity, smoking status, and total caloric intake) and body size indicators.
Table 2.
Adjusted Associations Between Anthropometric Indicators and Serum Measures of Estrogen and SHBG
| Indicator | Estradiol, pg/mL |
SHBG, nmol/L |
||
|---|---|---|---|---|
| β | P Value | β | P Value | |
| Hip circumference in cm | 0.69 | .489 | −4.48 | <.001 |
| BMI, kg/m2 | 0.78 | .438 | −5.12 | <.001 |
| WHR | 2.68 | .008 | −3.48 | .001 |
| WC, cm | 2.02 | .046 | −5.43 | <.001 |
| Percentage of body fat | 1.19 | .236 | −4.24 | <.001 |
| Weight, kg | 1.18 | .253 | −4.49 | <.001 |
Abbreviations: β, standardized β coefficient (point estimate/SE). Estradiol measures are square-root transformed. All analyses were adjusted for current age, age at menarche, age at first pregnancy, smoking status, and total caloric intake.
Figure 1.
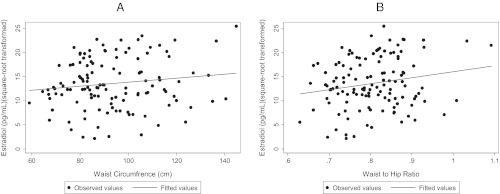
Scatter plots displaying the association between WC (A), WHR (B), and serum concentrations of estradiol.
Discussion
Our results show abdominal obesity, as indicated by higher WHR and WC, was significantly associated with serum concentrations of estradiol and SHBG. The association between WHR and WC with serum concentrations of estradiol is consistent with the findings of another study conducted among premenopausal AA women (14). However, our data differ from those of previous studies that reported nonsignificant or significant inverse associations between body size and estradiol (15–18). For example, among studies measuring abdominal obesity, WHR was not significantly associated with serum estradiol levels (18, 19). Of note, published serum estradiol levels were in a range similar to that of our study findings. The differences in our data may be attributed to the self-reported lifestyle characteristics. In particular, more than half (53%) of the women in our sample were obese and consumed high-fat and low-fiber, energy-dense diets. The coupling of these lifestyle characteristics could have resulted in higher serum estradiol levels (14).
We speculate that there may be several biological rationales to explain the relationship between abdominal obesity and higher serum estradiol levels. AA and CA women have different hormonal patterns (5, 11). Early age of menarche, when coupled with adult obesity previously was associated with higher estradiol levels (20). In addition, a recent study found that AA women have significantly higher levels of estradiol throughout the entire menstrual cycle (11). Marsh et al (11) speculated that AA women may have higher ovarian aromatase activity than do CA women, which may be a direct result of polymorphisms (ie, CYP19) and biological factors (ie, leptin and anti-Müllerian hormone). Future studies are needed to determine whether these factors moderate the relationship between abdominal obesity and serum estradiol levels.
All measures of body size were significantly and inversely associated with SHBG, which is a consistent finding in women (15, 18). The association between abdominal obesity and SHBG levels appeared to be stronger for WC than WHR, which differs from the associations we observed with estradiol. It is postulated that abdominal obesity elevates insulin levels (ie, hyperinsulinemia), which then lowers SHBG production and results in higher levels of sex hormones (9).
Previous studies have shown conflicting results with the use of BMI to assess sex hormone levels. Our data provide preliminary evidence that premenopausal AA women with high levels of abdominal obesity have higher serum concentrations of estradiol and lower concentrations of SHBG. Findings from this study contribute to the literature, suggesting that indicators of body fat distribution may be a better determinant of hormonal concentrations in at-risk populations. We speculate that abdominal obesity when coupled with other conditions (eg, early age of menarche and poor diet) may elevate serum estradiol levels.
Our study has a number of strengths, including the collection of all samples during the follicular phase, as well as objective measures of body size. However, our study is limited to capturing hormone levels at only one time point and may not be indicative of AA women's lifetime exposure to estrogen. We also report only total estradiol and not free estradiol. The modest sample size and the reliance on only two sex hormone outcomes suggest the need for future studies designed to assess the patterns of multiple sex hormones with body fat distribution indicators. In addition, because our sex hormone samples were obtained from a dietary intervention that required study participants to consume at least 28% of calories from fat, most of the participants in this study were considered overweight or obese. Thus, our results cannot be generalized to premenopausal women of normal weight. Lastly, the use of immunoassays is associated with a number of limitations. Nonetheless, these data support the need for lifestyle interventions emphasizing weight reduction and particular strategies that focus on reducing abdominal fat in AA premenopausal women.
Acknowledgments
The authors thank the A NULIFE Study participants, individuals who were involved in patient recruitment and data collection, and the staff of the Dorothy B. Height Center for Health Equity and Evaluation Research (formerly the Center for Research on Minority Health). The authors also express gratitude to the R25T program at MD Anderson Cancer Center for providing the resources to conduct the biochemical analysis and Dr. Peng Huang for his scientific expertise and guidance. The authors also thank Markeda Wade of the MD Anderson Cancer Center's Department of Scientific Publications for editorial assistance.
This work was supported in part by National Cancer Institute Grants K01CA158000 and R25 CA57730; National Institute on Minority Health and Health Disparities Grants 5P60MD000503 and 5RC2MD004783; American Cancer Society Grant TURSG-01-247-01-PBP; and National Institutes of Health Grant CA016672.
Disclosure Summary: The authors have no conflicts of interest to disclose.
Footnotes
- AA
- African American
- BMI
- body mass index
- CA
- Caucasian
- HC
- hip circumference
- SHBG
- sex hormone-binding globulin
- WC
- waist circumference
- WHR
- waist-to-hip ratio.
References
- 1. Stephenson GD, Rose DP. Breast cancer and obesity: an update. Nutr Cancer. 2003;45:1–16 [DOI] [PubMed] [Google Scholar]
- 2. Rose DP, Haffner SM, Baillargeon J. Adiposity, the metabolic syndrome, and breast cancer in African-American and white American women. Endocr Rev. 2007;28:763–777 [DOI] [PubMed] [Google Scholar]
- 3. Hall IJ, Newman B, Millikan RC, Moorman PG. Body size and breast cancer risk in black women and white women: the Carolina Breast Cancer Study. Am J Epidemiol. 2000;151:754–764 [DOI] [PubMed] [Google Scholar]
- 4. Adams-Campbell LL, Kim KS, Dunston G, Laing AE, Bonney G, Demenais F. The relationship of body mass index to reproductive factors in pre- and postmenopausal African-American women with and without breast cancer. Obes Res. 1996;4:451–456 [DOI] [PubMed] [Google Scholar]
- 5. Ewertz M, Jensen MB, Gunnarsdóttir KÁ, et al. Effect of obesity on prognosis after early-stage breast cancer. J Clin Oncol. 2010;29:25–31 [DOI] [PubMed] [Google Scholar]
- 6. Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–578 [DOI] [PubMed] [Google Scholar]
- 7. Yang XR, Chang-Claude J, Goode EL, et al. Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst. 2011;103:250–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moorman PG, Jones BA, Millikan RC, Hall IJ, Newman B. Race, anthropometric factors, and stage at diagnosis of breast cancer. Am J Epidemiol. 2001;153:284–291 [DOI] [PubMed] [Google Scholar]
- 9. Bernstein L. Epidemiology of endocrine-related risk factors for breast cancer. J Mammary Gland Biol Neoplasia. 2002;7:3–15 [DOI] [PubMed] [Google Scholar]
- 10. Key T, Appleby P, Barnes I, Reeves G. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst. 2002;94:606–616 [DOI] [PubMed] [Google Scholar]
- 11. Marsh EE, Shaw ND, Klingman KM, et al. Estrogen levels are higher across the menstrual cycle in African-American women compared with Caucasian women. J Clin Endocrinol Metab. 2011;96:3199–3206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. King DW, Duello TM, Miranda PY, et al. Strategies for recruitment of healthy premenopausal women into the African American Nutrition for Life (A NULIFE) Study. J Womens Health (Larchmt). 2010;19:855–862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Thomson CA, Giuliano A, Rock CL, et al. Measuring dietary change in a diet intervention trial: comparing food frequency questionnaire and dietary recalls. Am J Epidemiol. 2003;157:754–762 [DOI] [PubMed] [Google Scholar]
- 14. Barnett JB, Woods MN, Rosner B, et al. Sex hormone levels in premenopausal African-American women with upper and lower body fat phenotypes. Nutr Cancer. 2001;41:47–56 [DOI] [PubMed] [Google Scholar]
- 15. Freeman EW, Sammel MD, Lin H, Gracia CR. Obesity and reproductive hormone levels in the transition to menopause. Menopause. 2010;17:718–726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nagata C, Wada K, Nakamura K, Hayashi M, Takeda N, Yasuda K. Associations of body size and reproductive factors with circulating levels of sex hormones and prolactin in premenopausal Japanese women. Cancer Causes Control. 2011;22:581–588 [DOI] [PubMed] [Google Scholar]
- 17. Tworoger SS, Eliassen AH, Missmer SA, et al. Birthweight and body size throughout life in relation to sex hormones and prolactin concentrations in premenopausal women. Cancer Epidemiol Biomarkers Prev. 2006;15:2494–2501 [DOI] [PubMed] [Google Scholar]
- 18. Verkasalo PK, Thomas HV, Appleby PN, Davey GK, Key TJ. Circulating levels of sex hormones and their relation to risk factors for breast cancer: a cross-sectional study in 1092 pre- and postmenopausal women (United Kingdom). Cancer Causes Control. 2001;12:47–59 [DOI] [PubMed] [Google Scholar]
- 19. Ivandiæ A, Prpiæ-Krizevac I, Suciæ M, Juriæ M. Hyperinsulinemia and sex hormones in healthy premenopausal women: relative contribution of obesity, obesity type, and duration of obesity. Metabolism. 1998;47:13–19 [DOI] [PubMed] [Google Scholar]
- 20. Emaus A, Espetvedt S, Veierød MB, et al. 17-beta-estradiol in relation to age at menarche and adult obesity in premenopausal women. Hum Reprod. 2008;23:919–927 [DOI] [PubMed] [Google Scholar]


