Abstract
Rebreathing of carbon dioxide caused by incompetent ‘cage and disc’ unidirectional valves has been reported earlier. Some manufacturers have changed the design of unidirectional valves to ‘flexible leaflets’. We report a series of cases where a deformed membrane leaflet in expiratory unidirectional valves led to rebreathing of carbon dioxide.
Keywords: Anesthesia machine, circle breathing system, incompetent unidirectional valves
Introduction
Hypercapnia can occur when a circle breathing system is used.[1] It could result from hypoventilation due to leaks, exhausted soda lime, bypassing the absorber inadvertently, or due to a malfunction of unidirectional valves (UDVs). Incompetence of expiratory UDV, caused by a damaged disc or a disc stuck in an open position, has been reported earlier.[2–7] There have been many changes in the design of anesthesia workstations in recent years. Some manufacturers have changed the design of UDVs from the ‘cage and disc’ to the ‘flexible leaflet’ type. We report a series of cases where deformed ‘flexible leaflet’ of the expiratory UDV was the cause of hypercapnia, which resulted in the rebreathing of carbon dioxide.
Case Reports
An anesthesia workstation with a circle absorber (Signet-615, av+ulco Healthcare , Avasarala Technologies Limited, India) was used in all the cases reported. An anesthesia ventilator connected to a single flow sensor in the expiratory limb (eV-700, av+ulco Healthcare, Avasarala Technologies Limited, India) and a multiparameter anesthesia monitor (StarPlus, Larson and Toubro Limited, India) were used in all cases.
Case 1
A five-year-old girl was scheduled for surgical closure of an atrial septal defect under cardiopulmonary bypass. After routine preuse check, anesthesia was induced by inhalation of sevoflurane, using Jackson Rees’ modification of the Ayre's T-piece (JRMATP). Induction and tracheal intubation were uneventful. The lungs were ventilated using a circle breathing system and volume-controlled ventilation (VCV). The capnogram showed an increasing trend of end-tidal carbon dioxide (EtCO2; 45 mmHg) with high inspired carbon dioxide (FiCO2; 12 mmHg). Soda lime in the canister was fresh and did not show any change in color. Increasing the flow of fresh gas had no effect on FiCO2. As the source of the problem could not be identified, the breathing system was changed to JRMATP and anesthesia was continued. Later, the anesthesia machine was replaced and further management of the case was uneventful.
Case 2
A nine-year-old boy was scheduled for the release of a burn contracture in the leg. Anesthesia was induced with propofol and a size 2.5 laryngeal mask airway (LMA) was inserted. Anesthesia was maintained with isoflurane using a circle breathing system, with the patient breathing spontaneously. The capnogram showed a progressive increase in EtCO2 with elevated FiCO2 (up to 8 mmHg), not altered by increasing the flow of fresh gas. Soda lime appeared unaltered. When ventilation was assisted manually, EtCO2 decreased to normal levels and touched baseline during inspiration. The problem recurred whenever the child was allowed to breathe spontaneously without assistance. Anesthesia was continued with assisted ventilation and further management was uneventful. On close inspection, the flexible leaflet of the expiratory UDV appeared minimally deformed. After the end of the procedure, the UDV was tested and found to be incompetent.
Case 3
A four-year-old boy was scheduled for cleft palate repair, as the third patient on the list. After managing two adult patients earlier, the corrugated tubing of the circle breathing system was changed to the pediatric type and tested for leaks. Anesthesia was induced with sevoflurane using JRMATP. After tracheal intubation, the circle breathing system was used with pressure-controlled ventilation (PCV). After a few breaths, FiCO2 increased to 9 mmHg [Figure 1]. Soda lime was only partly discolored. The flow rate setting in the ventilator (i.e., the flow rate used to achieve the set inspiratory pressure, an equivalent of Pramp or ‘rise time’) was increased and FiCO2 became zero. With manual ventilation, FiCO2 increased whenever the tidal volume was delivered slowly and decreased with rapid delivery of tidal volume. We noted that the leaflet of the expiratory UDV was deformed and part of it remained open during inspiration [Figure 2]. The valve was closing fully with rapid delivery of tidal volume (or higher flow rate). The flow waveform on the ventilator showed minimal flow during inspiration [Figure 3]. The flow sensor was not direction sensitive, and was showing both the normal expiratory flow and the abnormal reverse flow on the same side of the Y-axis (the ventilator was not equipped with any alarm to indicate reverse flow). Later, the expiratory UDV was tested and found to be incompetent. The machine was used in subsequent patients after replacing the defective valve leaflet. The problem recurred after a few days and the new leaflet was also found to be deformed.
Figure 1.

Capnogram showing elevated baseline and higher end-tidal carbon dioxide
Figure 2.

Deformed ‘flexible leaflet’ of expiratory unidirectional valve (shown after removing the covering dome)
Figure 3.
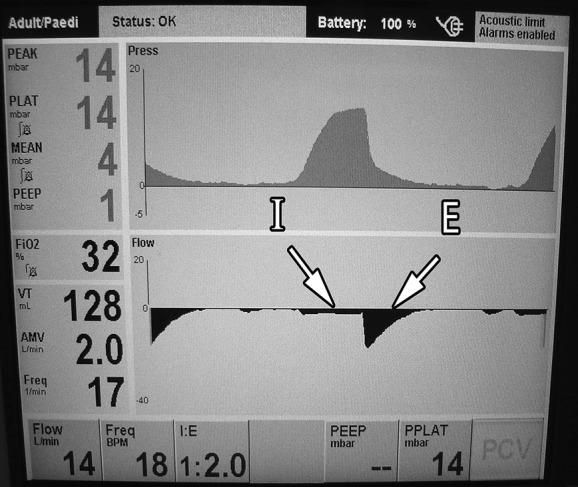
Ventilator display showing the abnormal reverse flow through expiratory unidirectional valve during inspiratory phase (I) and the normal flow during expiration (E)
On checking all anesthesia machines with similar UDVs, the inspiratory UDVs were found to be deformed and incompetent in some machines, although no problem was reported during clinical use. The matter was reported to the manufacturer and they concluded that the problem was caused by the thinness of the valve leaflet (0.3 mm). All the leaflets in UDVs were replaced with thicker ones (0.5 mm). No similar problems have been reported since then.
Discussion
The UDV leaflets in question were made of silicon and were too thin. Each time the valve opened, only a portion of the leaflet was lifted, allowing movement of gas, and after repeated use, this portion of the leaflet remained deformed in an open position. The deformed portion closed only at higher flow rates (or a higher upstream pressure). Low flow rates and smaller tidal volumes used in children were probably not generating sufficient upstream pressure to close the deformed portion of the leaflet, thereby causing rebreathing of carbon dioxide.
Incompetent expiratory UDV can be detected by ventilators with a reverse flow alarm.[1] Standard flow sensors should be able to identify the direction of flow and be able to give an alarm if the flow is reversed due to incompetent valves. The flow sensors used in the above patients were not direction sensitive and did not have a reverse flow alarm.
Although inspiratory UDVs in some machines were found to be incompetent during testing, the same had not been detected during clinical use. An incompetent inspiratory UDV results in the prolongation of the alveolar plateau of the capnogram which might be indistinguishable from a normal waveform and can be missed easily.[8]
The commonly used anesthesia preuse check protocols cannot identify an incompetent UDV reliably. Special tests to identify problems with UDVs may not be practically possible given the time constraints in modern operating rooms.[9–12]
Continuous revision of acceptable machine standards (e.g., making reverse flow alarm mandatory for flow sensors in the circle breathing system) and quality control of medical equipment must be undertaken, to ensure standards of anesthesia delivery systems.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Dorsch JA, Dorsch SE. Hazards of anesthesia machines and breathing systems. In: Dorsch JA, Dorsch SE, editors. Understanding anesthesia equipment. 5th ed. Philadelphia, Pennsylvania: Lippincott Williams and Wilkins; 2008. pp. 404–30. [Google Scholar]
- 2.Thorning GP, Groba CB. Critical incident due to a corroded expiratory valve. Anaesthesia. 2005;60:823–4. doi: 10.1111/j.1365-2044.2005.04310.x. [DOI] [PubMed] [Google Scholar]
- 3.Yew WS, Hwang NC. Faulty unidirectional expiratory valve as a cause of rebreathing. Anaesthesia. 2003;58:1239–40. doi: 10.1046/j.1365-2044.2003.03536.x. [DOI] [PubMed] [Google Scholar]
- 4.Dawood AM, Digger T. An apparently normal looking valve as a cause of rebreathing. Anaesthesia. 2002;57:929–30. doi: 10.1046/j.1365-2044.2002.27936.x. [DOI] [PubMed] [Google Scholar]
- 5.Cozanitis DA. Damage to an OHMEDA expiratory valve. Anaesth Intensive Care. 2000;28:585–6. [PubMed] [Google Scholar]
- 6.Findlay GP, Spittal MJ. A subtle cause of circle system failure. Br J Anaesth. 1995;75:667–8. doi: 10.1093/bja/75.5.667. [DOI] [PubMed] [Google Scholar]
- 7.Hornbein TF, Glauber DT. Inadvertent inspiration of carbon dioxide. Anesthesiology. 1984;61:114–5. [PubMed] [Google Scholar]
- 8.Breen P, Jacobsen B. Carbon dioxide spirogram (but not capnogram) detects leaking inspiratory valve in a circle circuit. Anesth Analg. 1997;85:1372–6. doi: 10.1097/00000539-199712000-00035. [DOI] [PubMed] [Google Scholar]
- 9.Kim JM, Kovac AL, Mathewson HS. A method for detection of incompetent unidirectional dome valves: A prevalent malfunction. Anesth Analg. 1985;64:745–7. [PubMed] [Google Scholar]
- 10.Kitagawa H, Sai Y, Nosaka S, Amakata Y, Oku S. A new leak test for specifying malfunctions in the exhalation and inhalation check valve. Anesth Analg. 1994;78:611. doi: 10.1213/00000539-199403000-00051. [DOI] [PubMed] [Google Scholar]
- 11.Eappen S, Corn SB. The anesthesia machine valve tester: A new device and method for evaluating the competence of unidirectional anesthetic valves. J Clin Monit. 1996;12:305–9. doi: 10.1007/BF02221751. [DOI] [PubMed] [Google Scholar]
- 12.Weigel WA, Murray WB. Detecting unidirectional valve incompetence by the modified pressure decline method. Anesth Analg. 2005;100:1723–7. doi: 10.1213/01.ANE.0000150969.30661.B7. [DOI] [PubMed] [Google Scholar]


