Abstract
Background:
Oxytocin is routinely administered during cesarean delivery for uterine contraction. Adverse effects are known to occur after intravenous oxytocin administration, notably tachycardia, hypotension, and electrokardiogram (EKG) changes, which can be deleterious in high-risk patients.
Aims and Objectives:
To compare the hemodynamic changes and uterotonic effect of equivalent dose of oxytocin administered as an intravenous bolus versus intravenous infusion.
Study Design:
Randomized, double-blind, active controlled trial.
Materials and Methods:
Eighty parturients undergoing elective cesarean delivery, under spinal anesthesia, were randomly allocated to receive 3 IU of oxytocin either as a bolus intravenous injection over 15 seconds (group B, n = 40) or as an intravenous infusion over 5 minutes (group I, n = 40). Uterine tone was assessed as adequate or inadequate by an obstetrician. Intraoperative heart rate, non-invasive blood pressure, and EKG changes were recorded. These data were compared between the groups. Any other adverse events like chest pain, nausea, vomiting, and flushing were noted.
Results:
There was significant rise in heart rate and significant decrease in mean arterial pressure in bolus group compared to infusion group. Three patients in bolus group had EKG changes in the form of ST-T depression and 5 patients complained of chest pain. No such complications were found in infusion group.
Conclusion:
Bolus oxytocin (at a dose of 3 IU over 15 seconds) and infusion of oxytocin (at a dose of 3 IU over 5 minutes) have comparable uterotonic effect. However, the bolus regime shows significantly more adverse cardiovascular events.
Keywords: Cesarean delivery, hemodynamic change, oxytocin, uterine tone
Introduction
Oxytocin is the most commonly used uterotonic agent in obstetrics. It is routinely administered after both normal and operative delivery to initiate and maintain adequate uterine contractility for minimizing blood loss and preventing postpartum hemorrhage.[1] Several regimens of oxytocin have been tested during cesarean delivery (CD) with variable wanted (uterotonic) and unwanted (cardiovascular) effects.[2–8] It is a common practice to administer oxytocin as an intravenous (IV) bolus followed by IV infusion for adequate uterine contraction. Larger dose of oxytocin injected rapidly is known to produce various adverse effects such as hypotension, nausea, vomiting, chest pain, headache, flushing, myocardial ischemia, ST-T segment changes, pulmonary edema, severe water intoxication, and convulsion.[9]
We aimed to compare the hemodynamic effects (heart rate, mean arterial pressure, arrhythmias), uterine contraction, and adverse events (chest pain, flushing, nausea, and vomiting) of equivalent doses of oxytocin as IV bolus versus IV infusion.
Materials and Methods
This randomized, double-blind, active controlled trial was started after obtaining the clearance from the Institute's Ethics Committee and written informed consent from all patients. Eighty parturients of American Society of Anesthesiologists physical status I and II, aged between 20 and 30 years, scheduled for elective CD under spinal anesthesia (SA) were recruited. Based on a previous study,[8] the mean difference and the pooled standard deviation were calculated and the sample size was determined (40 in each group), with power of study being 80% and confidence interval being 99%. Patients with active labor pain, ruptured membrane, multiple gestation, cardiovascular instability, preeclampsia and eclampsia, diabetes mellitus, and placenta previa were excluded from this study.
The patients were instructed to avoid solid food for 6 hours and allowed to drink plain water up to 2 hours before the operation. After arriving in the operating room an IV line was established with an 18G cannula and preloading was done with 15 ml/kg Ringer's lactate solution over 30 minutes before SA, followed by infusion of same solution 5 ml/kg/hour. All the patients were premedicated with slow metoclopramide 10 mg and ranitidine 50 mg IV. Baseline maternal mean arterial pressure (MAP) and heart rate (HR) were recorded before administering SA. The procedure of SA was explained to all patients.
The patients were randomly allocated to receive 3 International units (IU) of oxytocin either as a bolus IV over 15 seconds (group B, n = 40) or as an infusion over 5 minutes (group I, n = 40). Randomization was done following a computer-generated random numbers. Allocation concealment was ensured with sealed opaque envelope. Patients concerned as well as data collector were blind to the mode of administration of oxytocin. Both the groups received infusion; one of them received oxytocin among it to make similarity between them.
Then 12 mg hyperbaric bupivacaine (0.5%) was administered through the L3-L4 intervertebral space with the patients in the sitting position with a 26-G pencil-point spinal needle. The patients were then made supine with left lateral uterine displacement using a wedge. Multichannel monitor was attached. Surgery was allowed to proceed after achieving a T6 sensory level to pinprick. Oxytocin was administered as per the group allocated after childbirth. Once again, the MAP and HR were recorded before giving the injection oxytocin.
Uterine tone was assessed by obstetrician (same obstetrician for all cases) and designated as adequate or inadequate. Intraoperative HR, MAP, and electrokardiogram (EKG) changes were recorded. These data were compared between the groups. Any other adverse events like chest pain, nausea, vomiting, and flushing were noted. Patients having a fall in MAP before the administration of oxytocin were treated with IV bolus of 100 mcg phenylephrine and were excluded from the study.
HR was measured at 30-second interval up to 2.5 minutes, then at 5 and 10 minutes. MAP was measured at 1-minute interval up to 5 minutes, then at 7 and 10 minutes. Any EKG changes were monitored. Obstetricians were asked about the adequacy of uterine contraction 3 minutes after the start of injection oxytocin and noted as either “adequate” or “inadequate.” Any adverse events like chest pain, flushing, and vomiting was also observed.
If uterus was not adequately contracted after 3 minutes, oxytocin 3 IU IV was given as rescue dose. A maximum of 2 rescue doses were given. If still the uterus was not contracted, carboprost tromethamine 0.25 mg intramuscular was given. After the study period patients received a maintenance IV infusion of oxytocin (0.16 IU/min).
Patient characteristics and obstetric and intraoperative data were presented as mean ± SD. Numerical data were analyzed with Student's t-test and categorical data were analyzed with Chi-square test. A P value of <0.05 was considered to be statistically significant. The data collected were entered into a Microsoft Excel database and analyzed using Statistical Product for the Social Sciences (SPSS) for Windows, version 12.0.
Results
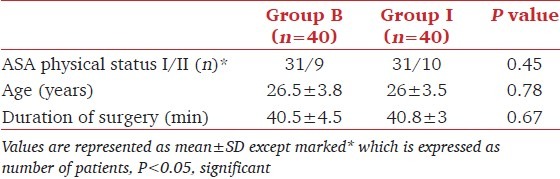
The study was conducted from January 2011 to June 2011. Eighty patients were recruited for the study. Both the groups were comparable demographic data [Table 1]. There was a failure of spinal anesthesia procedure in 3 patients and so they received general anesthesia. Three patients developed significant hypotension and required vasopressor prior to oxytocin administration; four patients required rescue uterotonic other than oxytocin. Ten patients violated the study protocol thus and were excluded from analysis.
Table 1.
Demographic data
The heart rate increased by 25-30 beats/minute in bolus group at 30 seconds, remained almost same up to 120 seconds and gradually decreased but did not touch the basal value even at 10 minutes. In case of infusion group heart rate increased by about 10 beats per minute at 60 seconds of starting infusion, gradually decreased to almost basal level at 10 minutes. All the values of mean heart rate of bolus group were higher compared to infusion group and differences were statistically significant [Table 2 and Figure 1].
Table 2.
Comparison of mean heart rate between two groups at different timings
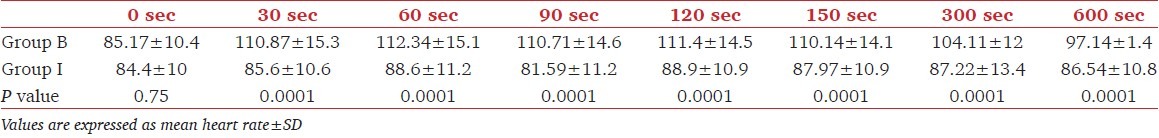
Figure 1.
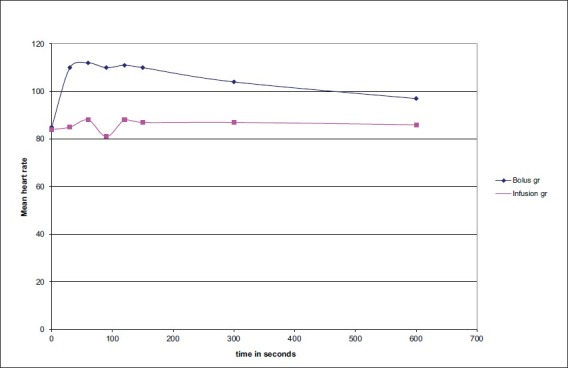
Mean heart rate at different timings in two groups
The fall in MAP (mean arterial pressure) was maximum at 3 minutes in bolus group, but no significant change was found regarding MAP in infusion group. The fall in MAP in bolus group was higher and statistically significant in comparison to infusion group [Table 3 and Figure 2].
Table 3.
Comparison of mean arterial pressure at various specified timings between two groups
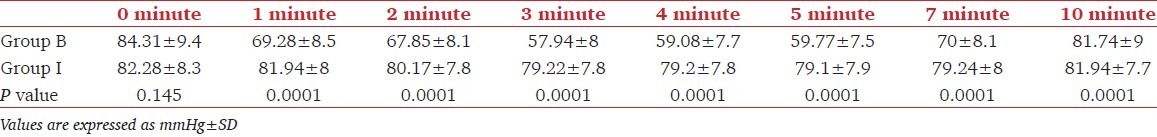
Figure 2.
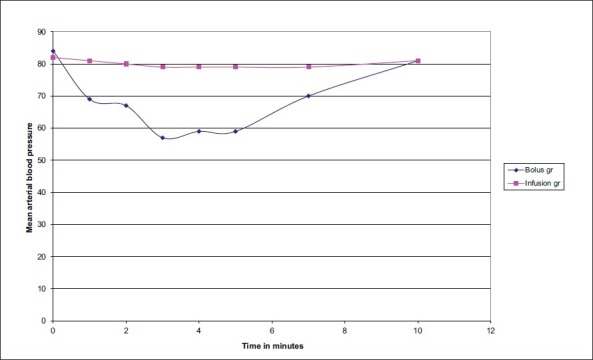
Mean arterial blood pressure at different time points in two groups
Three patients had ST-T depression and 5 patients had chest pain in bolus group. No adverse effect was found in patients of infusion group. Uterine contraction was adequate in both the groups.
Discussion
Pregnant women undergoing CD are at increased risk of obstetric hemorrhage, mainly due to uterine atony. Oxytocin is the mainstay of treatment of uterine atony.[1] Prophylactic routine use of oxytocin has been shown to reduce the incidence of postpartum hemorrhage by up to 40%.[10] Despite widespread use there is limited data to guide the optimal oxytocin dosing in patients undergoing elective CD.
Uterine oxytocin receptors population increases progressively during pregnancy and reaches peak at term. In late pregnancy, before the onset of labor, oxytocin receptors are on average 12 times higher than in early pregnancy and about 80 times higher than in non-pregnant uterus. As the non-laboring uterus at term remains more sensitive to oxytocin, low dose of oxytocin might have an optimum efficacy while not inviting the deleterious effects of high dose of oxytocin.[9] In this study, we selected mothers undergoing elective CD not in labor expecting a good response with low dose of oxytocin.
During the onset of labor, uterine sensitivity to oxytocin increases and oxytocin receptors express diffusely and heterogeneously.[9] It is a usual practice to increase the dose of oxytocin, assuming that higher doses will result in more effective uterine contraction. The higher doses of oxytocin are unlikely to improve uterine contractions further during CD in laboring mothers who are already receiving oxytocin. In-vitro and in-vivo studies find that prior exposure to oxytocin induces myometrial oxytocin receptor desensitization.[1] The oxytocin induced desensitization is dependent upon the duration of oxytocin exposure and occurs over a clinically relevant time frame of approximately 4.2 hours.[11] This can influence the optimum oxytocin dosing for adequate uterine tone following cesarean delivery in mothers who are already receiving oxytocin. The dose of oxytocin required is nine times higher in laboring women than non-laboring women.[5] It is suggested that excessive doses of oxytocin to achieve adequate uterine tone during elective CD needs re-evaluation.[7] It is observed that adequate uterine tone can be achieved with small bolus doses like 0.5-3 IU of oxytocin,[4] but the incidence of hypotension increases significantly after 5 IU. Increasing the bolus dose of oxytocin to above 5 IU during elective CD does not offer any advantage.[6] We used oxytocin either as 3 IU bolus over 15 seconds or as 3 IU infusion over 5 minutes. Only 3 patients needed rescue uterotonic other than oxytocin (injection carboprost). Rest of the patients in both the groups had adequate amount of uterine contraction as stated by the surgeon.
The present study finds a higher increase in HR (approximate 25-30 beats/min) in bolus group at 30 seconds which did not return to base line even after 10 minutes whereas in the infusion group the rise in heart rate was only by10 beats/min and gradually touched the baseline value. The decrease in MAP was found in bolus group only. Three patients (7.5%) had ST-T changes and 5 patients (12.5%) had chest pain in bolus group. No such adverse events were observed in the infusion group.
A significant fall of MAP 30 seconds after administration of a 10 IU bolus oxytocin, but a significant increase in HR and cardiac output (CO), occurred 1 minute after 5 IU administration has been reported earlier.[12] When 5 IU bolus IV was compared with 5 IU infusion, MAP decreased up to 27 mm of Hg and HR increased by 7/minute at 35 seconds in the bolus group, which recovered to baseline at 110 seconds. The infusion group in contrast had a decrease in MAP of only 8 mm Hg and HR increased by 10 beats/minute.[7] The reduction in MAP and speed of recovery are dose dependent.[12]
Rapidly injected large doses of oxytocin are known to produce various adverse effects such as hypotension, nausea, vomiting, chest pain, headache, flushing, myocardial ischemia, ST-T segment changes, pulmonary edema, and severe water intoxication with convulsions.[9] ED90 of oxytocin reported to prevent uterine atony and PPH after an elective CD is 0.29 IU/minute, or approximately 15 IU of oxytocin in one liter of IV fluid administered over one hour period.[11] This dose of oxytocin infusion is 30% less than the infusion dose currently in use.
Conclusion
To conclude, in elective cesarean delivery, administration of oxytocin IV infusion is better, than the same dose administered as a bolus IV dose, to produce adequate uterine contraction and is associated with less adverse hemodynamic changes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Dyer RA, Butwick AJ, Carvalho B. Oxytocin for labour and caesarean delivery: Implications for the anaesthesiologist. Curr Opin Anaesthesiol. 2011;24:255–61. doi: 10.1097/ACO.0b013e328345331c. [DOI] [PubMed] [Google Scholar]
- 2.Marcus HE, Fabian A, Lier H, Dagtekin O, Böttiger BW, Teschendorf P, et al. Survey on the use of oxytocin for caesarean section. Minerva Anestesiol. 2010;76:890–5. [PubMed] [Google Scholar]
- 3.Carvalho JC, Balki M, Kingdom J, Windrim R. Oxytocin requirements at elective cesarean delivery: A dose-finding study. Obstet Gynecol. 2004;104:1005–10. doi: 10.1097/01.AOG.0000142709.04450.bd. [DOI] [PubMed] [Google Scholar]
- 4.Butwick AJ, Coleman L, Cohen SE, Riley ET, Carvalho B. Minimum effective bolus dose of oxytocin during elective Caesarean delivery. Br J Anaesth. 2010;104:338–43. doi: 10.1093/bja/aeq004. [DOI] [PubMed] [Google Scholar]
- 5.Balki M, Ronayne M, Davies S, Fallah S, Kingdom J, Windrim R, et al. Minimum oxytocin dose requirement after caesarean delivery for labour arrest. Obstet Gynecol. 2006;107:45–50. doi: 10.1097/01.AOG.0000191529.52596.c0. [DOI] [PubMed] [Google Scholar]
- 6.Sarna MC, Soni AK, Gomez M, Oriol NE. Intravenous oxytocin in patient undergoing elective cesarean section. Anesth Analg. 1997;84:753–6. doi: 10.1097/00000539-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Thomas JS, Koh SH, Cooper GM. Haemodynamic effects of oxytocin given as i.v. bolus or infusion on women undergoing Caesarean section. Br J Anaesth. 2007;98:116–9. doi: 10.1093/bja/ael302. [DOI] [PubMed] [Google Scholar]
- 8.Sartain JB, Barry JJ, Howat PW, McCormack DI, Bryant M. Intravenous oxytocin bolus of 2 units is superior to 5 units during elective Caesarean section. Br J Anaesth. 2008;101:822–6. doi: 10.1093/bja/aen273. [DOI] [PubMed] [Google Scholar]
- 9.Devikarani D, Harsoor SS. Are we using right dose of oxytocin? Indian J Anaesth. 2010;54:371–3. doi: 10.4103/0019-5049.71020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nordström L, Fogelstam K, Fridman G, Larsson A, Rydhstroem H. Routine oxytocin in the third stage of labour: A placebo controlled randomised trial. Br J Obstet Gynaecol. 1997;104:781–6. doi: 10.1111/j.1471-0528.1997.tb12020.x. [DOI] [PubMed] [Google Scholar]
- 11.George RB, McKeen D, Chaplin AC, McLeod L. Up-down determination of the ED (90) of oxytocin infusions for the prevention of postpartum uterine atony in parturients undergoing. Can J Anaesth. 2010;57:578–82. doi: 10.1007/s12630-010-9297-1. [DOI] [PubMed] [Google Scholar]
- 12.Pinder AJ, Dresner M, Calow C, Shorten GD, O’Riordan J, Johnson R. Haemodynamic changes caused by oxytocin during caesarean section under spinal anaesthesia. Int J Obstet Anesth. 2002;11:156–9. doi: 10.1054/ijoa.2002.0970. [DOI] [PubMed] [Google Scholar]


