Abstract
Context:
Morbidly obese patients are prone for intraoperative hemodynamic disturbances and postoperative airway complications.
Aim:
Comparison of intraoperative hemodynamics and postoperative recovery characteristics of desflurane versus sevoflurane in morbidly obese patients undergoing laparoscopic bariatric surgery.
Settings and Design:
Randomized controlled trial
Materials and Methods:
After institutional ethics committee approval and written informed consent, 40 morbidly obese patients (BMI > 35 kg/m2) were randomized to receive desflurane or sevoflurane as part of a standardized general anesthesia technique. Volatile anesthetic concentration was titrated to maintain electroencephalographic bispectral index score (BIS) in the range of 40-60. Mean arterial pressure (MAP) and heart rate (HR) were recorded preoperatively, at induction and intubation, then at regular intervals. After extubation, early recovery was recorded by time to emergence and orientation to time and place. In post anesthesia care unit, intermediate recovery was assessed by modified Aldrete Score and Digit Symbol Substitution Test (DSST).
Results:
Intraoperative MAP and HR did not differ between the two groups (P > 0.05). The time to response to painful stimuli, obeying verbal commands and spontaneous eye opening was shorter (P = 0.001) and modified Aldrete Score was higher after desflurane anesthesia than after sevoflurane anesthesia (P = 0.049). DSST also returned towards normal faster after desflurane (28.50 ± 6.30 min vs. 35.0 ± 5.62 min, P = 0.03).
Conclusions:
Both desflurane and sevoflurane produce similar hemodynamic changes but the immediate and intermediate recovery was significantly faster after desflurane thus contributing to fast tracking and early discharge of patients.
Keywords: Anesthesia, morbidly obese, anesthetics volatile, sevoflurane, desflurane, recovery, early, intermediate
Introduction
Laparoscopic bariatric surgery offers the advantage of early mobilization and reduced hospital stay, but the associated carboperitoneum may lead to intraoperative cardiovascular instability.[1] Morbidly obese patients are also at increased risk of aspiration and acute upper airway obstruction after tracheal extubation. An ideal general anesthetic for bariatric procedures should provide intraoperative hemodynamic stability, and rapid recovery.[2]
Inhaled anesthetics, sevoflurane and desflurane, have low blood gas partition coefficients, and therefore share the advantage of faster onset and offset of anesthesia as compared with older inhaled anesthetics like halothane and isoflurane. Desflurane appears to yield a more rapid recovery because of its pharmacological properties.[3] The purpose of this study was to compare hemodynamic stability and recovery characteristics of desflurane and sevoflurane in bariatric surgery.
Materials and Methods
After approval from hospital ethics committee and written informed consent from patients, 40 morbidly obese patients (BMI > 35 kg/m2) belonging to American Society of Anesthesiologists grade II and III, and scheduled to undergo elective laparoscopic bariatric surgery were enrolled for the study. Patients were randomized by computer-generated random numbers table, into two groups of 20 patients each, to receive either desflurane (group D) or sevoflurane (group S) for maintenance of anesthesia. Exclusion criteria included history of allergy to the study drugs, chronic alcohol or narcotic drug abuse within 90 days of surgery, significant cardiopulmonary disease, hepatic and renal dysfunction and preoperative hematocrit values of less than 25%.
The pre anesthetic examination comprised of detailed history and systemic examination relevant to obesity. A thorough airway examination was conducted to evaluate for possible difficult intubation. Preoperative investigations included complete blood count (CBC), urine examination, blood sugar, serum electrolytes, coagulation indices, thyroid, liver, kidney and pulmonary function tests, electrokardiography and echokardiography or stress echokardiography as indicated. Patients were familiarized with the Digital Symbol Substitution Test (DSST) and baseline value was obtained. All patients were kept fasting for at least 12 h prior to surgery. Premedication included oral ranitidine hydrochloride 150 mg and metoclopramide 10 mg given the night before, and one hour before the surgery. Enoxaparin 40 mg was given subcutaneous for deep vein thrombosis prophylaxis, one hour before the surgery.
In the operating room, standard monitoring devices, the TOF-Guard neuromuscular monitor and electroencephalographic Bispectral Index (BIS) monitor were applied. Difficult airway cart was kept ready for all patients. The patients were positioned on a ramp made up of blocks kept under the shoulders and head so as to bring the chin on level with the chest wall. After administration of midazolam 0.05 mg/kg and fentanyl citrate 1-2 mcg/kg intravenous (IV), the patients were pre-oxygenated for three minutes. Anesthesia was induced with propofol 1-1.5 mg/kg IV, followed by atracurium besylate 0.5 mg/kg IV to facilitate tracheal intubation with an appropriate sized endotracheal tube. Anesthesia was maintained in the two groups using oxygen-nitrous oxide along with sevoflurane or desflurane as per the group allocation. The concentration of volatile anesthetics was titrated to maintain a BIS value between 40 and 60. Lungs were ventilated with tidal volume and respiratory rate set to maintain end-tidal carbon dioxide (EtCO2) of 30-40 mm Hg and arterial blood gases within normal limits, using a closed circuit breathing system. Neuromuscular block was maintained with atracurium besylate infusion to maintain one twitch on Train of Four (TOF) monitoring. Radial artery and internal jugular vein were cannulated for sampling and monitoring.
Continuous monitoring of oxygen saturation, non-invasive and invasive blood pressure, end-tidal carbon dioxide, electrokardiogram, expired concentration of volatile anesthetic agent and central venous pressure (CVP) was done. The heart rate, systolic, diastolic and mean blood pressure and BIS values were recorded before and at induction of anesthesia, immediately after tracheal intubation and at predetermined intervals (2, 3, 4, 5, 10, 15, 20, 30, 45 and 60 minutes and half hourly thereafter). Arterial blood gases and blood sugar were estimated as indicated. Fluids were administered guided by CVP values. Atracurium besylate infusion was discontinued 30 minutes before completion of surgery and volatile anesthetic agents were discontinued after last skin stitch. The neuromuscular block was reversed with neostigmine bromide 0.05 mg/kg and glycopyrrolate 0.08 mg/kg IV. The tracheal tube was removed after recovery of the neuromuscular block and when the patient was fully conscious.
Early recovery was assessed by recording the time to return of consciousness and appropriate response to painful stimuli after discontinuation of the anesthetics. In addition, time of response to verbal commands, spontaneous eye opening, stating name, date of birth, place of stay, squeezing fingers and lifting limb was also recorded. In the post-anesthesia care unit (PACU), intermediate recovery was assessed with the help of modified Aldrete Score recorded on arrival, after 5 minutes and again after 10 minutes. The time to successful completion of DSST test was also recorded.
All statistical analysis was performed using SPSS package (version 17, SPSS Inc., Chicago, IL, USA) software for windows. Sample size of 40 patients was calculated to achieve statistical significant result with α = 0.05 and power of 80%. Data are reported as mean ± SD or median and range as appropriate. Student's t-test was applied to test the statistical significance between the desflurane and the sevoflurane groups for hemodynamic variables and early recovery characteristics. Mann-Whitney U-test was used for modified Aldrete scoring and DSST. P- value <0.05 were considered statistically significant.
Results
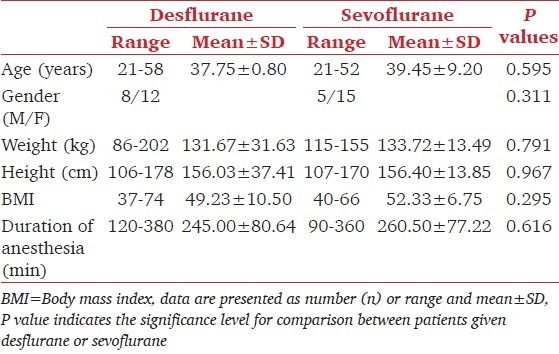
All 40 patients recruited for the study successfully completed the required assessments as per the protocol. The two study groups were comparable with respect to gender, age, weight, height, body mass index and the duration of anesthesia [Table 1].
Table 1.
Patient characteristics
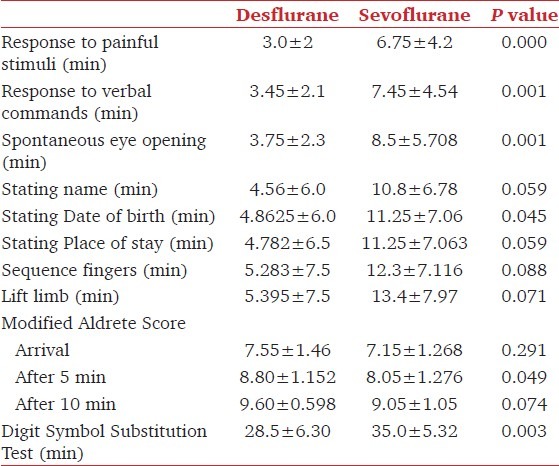
Intraoperative hemodynamic parameters did not differ in the two groups during the course of anesthesia and were successfully maintained within 20% of baseline values with both anesthetics [Figure 1]. After discontinuation of volatile anesthetic, the time to recovery of parameters like reaction to painful stimuli, obeying verbal commands and spontaneous eye opening was significantly shorter in patients given desflurane than in patients given sevoflurane (P = 0.001, Table 2). Although the intermediate recovery, as assessed by the modified Aldrete Score was comparable between the two groups on arrival to the PACU and at 10 minutes, the score at 5 minutes was significantly higher in the desflurane group (P < 0.05). The time taken to complete DSST in the desflurane group was significantly shorter as compared to the sevoflurane group, being 28.5 ± 6.30 min and 35.0 ± 5.32 min respectively, (P = 0.003).
Figure 1.
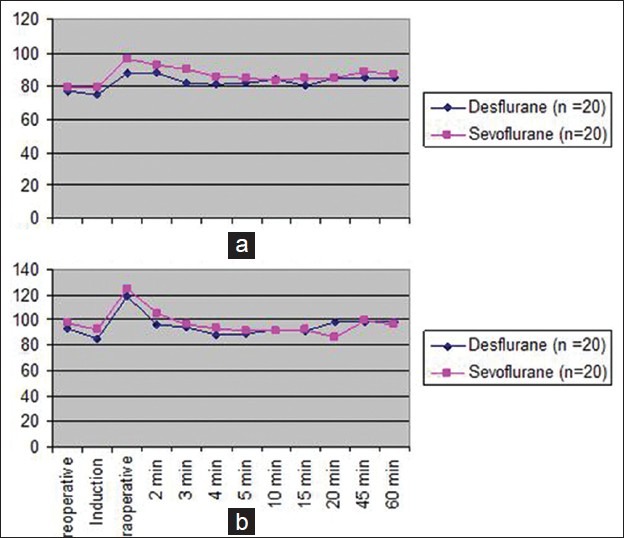
Changes in intraoperative hemodynamic parameter (a) Mean arterial pressure, (b) Heart rate. Result are presented as mean ± SD. P < 0.005
Table 2.
Early and intermediate recovery
Discussion
The laparoscopic approach to bariatric surgical procedures are preferred to open bariatric procedures, as they are known to cause less morbidity and allows a much earlier return to normal activities because of decreased postoperative discomfort. There is less need for intraoperative and postoperative narcotic drug administration, leading to improved oxygenation and decreased incidence of postoperative nausea and vomiting, especially during the early postoperative period.
Higher intra-abdominal pressure following carboperitoneum tends to collapse the major abdominal veins and decreases venous return, thus leading to a drop in preload and cardiac output.[4] Sevoflurane and desflurane provided similar intraoperative conditions during the maintenance period.[5] The present study also demonstrates that both, desflurane and sevoflurane, provide comparable hemodynamic stability in morbidly obese patients for prolonged laparoscopic surgical procedures. Mean arterial blood pressure and heart rate did not differ between the two groups, and were maintained within 20% of baseline values during the course of anesthesia.
Recovery is a continual and ongoing process and is divided into three phases: Early recovery, as the patient emerges from anesthesia and regains vital reflexes; intermediate recovery, when the patient achieves criteria for discharge from the PACU; and late recovery, when the patient returns to his or her preoperative physiological state. Early and complete recovery after general anesthesia is desirable in all patients, more so in the morbidly obese patients. All volatile anesthetics accumulate, over time, in adipose tissue. Such accumulation may delay recovery from anesthesia. The impact of anesthetic stored in fat may be exaggerated in morbidly obese patients, particularly after prolonged anesthesia.[6] In our study, the early postoperative recovery was significantly rapid after desflurane anesthesia and the patients could be transferred to PACU earlier. The intermediate recovery as evaluated by modified Aldrete Score at 5 minutes and the DSST also occurred earlier in the desflurane group.
The pharmacokinetic properties of desflurane and sevoflurane favor better intraoperative control of anesthesia and a rapid postoperative recovery. They have significantly lower blood/gas partition coefficients (0.45 and 0.65 respectively) than isoflurane (1.4) or halothane (2.4). The lower fat/blood partition coefficient of desflurane, 27 vs. 48 for sevoflurane, should favor its early elimination from the body resulting in early recovery.[7] A study comparing recovery characteristics of desflurane and sevoflurane in healthy male volunteers of normal weight, and observed earlier recovery after desflurane anesthesia. They postulated that delayed recovery after sevoflurane could also be attributed to additional factors such as effects of its degradation products after prolonged anaesthesia.[8]
Studies comparing the recovery profile after desflurane and sevoflurane anesthesia have shown conflicting results. In our study, the early recovery parameters were achieved much faster in patients anesthetized with desflurane than with sevoflurane (P = 0.001). In morbidly obese patients undergoing open bariatric procedures, one study observed that response to command and orientation took about half the time after desflurane than after sevoflurane.[4] Other studies however did not observe any difference in emergence parameters like times to eye opening, handgrip and recall of name and date of birth, after desflurane or sevoflurane anesthesia in morbidly obese patients undergoing laparoscopic bariatric surgeries.[9–11] However, unlike our study, these investigators used MAC equivalents of the two inhalational agents. The use of MAC as a guide to titrate volatile anesthetics can result in either under or over dosing. Multiple confounding factors can also affect the MAC in individual patients. Instead of using MAC equivalent doses of sevoflurane or desflurane, we used BIS, which is quantifiable measure of sedative and hypnotic effects of inhaled anesthetics, as an indicator of adequate anesthesia. BIS values between 40 and 60, correlate well with clinical endpoints of sedation and loss of consciousness and is relatively agent independent.[12] BIS use also improves recovery and reduces cost by reducing drug consumption.
Morbidly obese patients are at risk for airway complications, sleep apnea and hypoxia during the postoperative period. Faster emergence, extubation with a secure airway and maintenance of spontaneous ventilation facilitates recovery, provides better patient comfort, allow a more rapid return to baseline cardiovascular function and permits earlier departure from the operation theater.[13] In our study, early recovery was assessed by recording the response to painful stimuli, response to verbal commands and spontaneous eye opening. Intermediate recovery was assessed using modified Aldrete Score and DSST. DSST is well known standard test which have been used to measure return of consciousness, perception, orientation, coherence, memory and motor activity.[4]
Our results show a statistical and clinical difference between the recovery profiles of patients who received desflurane versus sevoflurane. The data is consistent with the faster kinetic profile of desflurane and its faster wash out from the body. Faster washout and recovery times have been demonstrated with desflurane using inhalation bolus technique to optimize anesthetic administration to morbidly obese patient.[14] Use of desflurane is also associated with a more rapid initial awakening, less depression of cognitive function and less impairment of psychomotor performance.[15]
The limitation of our study was a lack of investigator blinding to the use of study drugs and in the assessment of early recovery status. However, all patients underwent identical surgical procedures which were performed by the same anesthesiologist and the same surgeon. The use of BIS values to titrate volatile anesthetic concentration minimized investigator bias. The recovery was assessed by using objective end points. Obese patients are particularly at risk of early postoperative respiratory complications, so even slight improvements in early or intermediate recovery may be beneficial.[13]
In summary, we found that both desflurane and sevoflurane provide similar intraoperative hemodynamic stability but desflurane is associated with faster emergence and recovery in morbidly obese patients. The more predictable and rapid recovery after desflurane might have a significant beneficial effect on postoperative morbidity in the obese population.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Passannante AN, Rock P. Anesthetic management of patients with obesity and sleep apnea. Anesthesiol Clin North America. 2005;23:479–91. doi: 10.1016/j.atc.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Abernethy DR, Greenblatt DJ. Drug disposition in obese humans. An update. Clin Pharmacokinet. 1986;11:199–213. doi: 10.2165/00003088-198611030-00002. [DOI] [PubMed] [Google Scholar]
- 3.Cheymol G. Clinical pharmacokinetics of drugs in obesity. An update. Clin Pharmacokinet. 1993;25:103–14. doi: 10.2165/00003088-199325020-00003. [DOI] [PubMed] [Google Scholar]
- 4.Strum EM, Szenohradszki J, Kaufman WA, Anthone GJ, Manz IL, Lumb PD. Emergence and recovery characteristics of desflurane versus sevoflurane in morbidly obese adult surgical patients. Anesth Analg. 2004;99:1848–53. doi: 10.1213/01.ANE.0000136472.01079.95. [DOI] [PubMed] [Google Scholar]
- 5.Nathanson MH, Fredman B, Smith I, White PF. Sevoflurane versus Desflurane for outpatient Anaesthesia: A comparison of maintenance and recovery profiles. Anesth Analg. 1995;81:1186–90. doi: 10.1097/00000539-199512000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Eger EI, Gong D, Koblin D, Bowland T, Ionescu P, Laster MJ, et al. The effect of anesthetic duration on kinetic and recovery characteristics of desflurane versus sevoflurane, and on the kinetic characteristics of compound A, in volunteers. Anesth Analg. 1998;86:414–21. doi: 10.1097/00000539-199802000-00037. [DOI] [PubMed] [Google Scholar]
- 7.Eger EI., II New inhaled anesthetics. Anesthesiology. 1994;80:906–22. doi: 10.1097/00000542-199404000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Eger EI, Bowland T, Ionescu P, Laster MJ, Fang Z, Gong D, et al. Recovery and kinetic characteristics of desflurane and sevoflurane in volunteers after 8-h exposure, including kinetics of degradation products. Anesthesiology. 1997;87:517–26. doi: 10.1097/00000542-199709000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Romeo RC, Bettencourt AB, Vallejo MC. Desflurane vs sevoflurane wake up times in laparoscopic gastric patients. Anesthesiology. 2004;101:A128. [Google Scholar]
- 10.La Colla L, Albertin A, La Colla G, Mangano A. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth. 2007;99:353–8. doi: 10.1093/bja/aem197. [DOI] [PubMed] [Google Scholar]
- 11.Vallejo MC, Sah N, Phelps AL, O’Donnell J, Romeo RC. Desflurane versus sevoflurane for laparoscopic gastroplasty in morbidly obese patients. J Clin Anesth. 2007;19:3–8. doi: 10.1016/j.jclinane.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Sandlr NA. The use bispectral analysis to monitor outpatient sedation. Anesth Prog. 2000;47:72–83. [PMC free article] [PubMed] [Google Scholar]
- 13.Gergin S, Cevik B, Yildirim GB, Ciplakligil E, Colakoglu S. Sevoflurane Vs Desflurane: Haemodynamic Parameters And Recovery Characteristics. Internet J Anesthesiol. 2005;9:1. [Google Scholar]
- 14.De Baerdemaeker LE, Struys MM, Jacobs S, Den Blauwen NM, Bossuyt GP, Pattyn P, et al. Optimization of desflurane administration in morbidly obese patients: A comparison with sevoflurane using an inhalation bolus technique. Br J Anaesth. 2003;91:638–50. doi: 10.1093/bja/aeg236. [DOI] [PubMed] [Google Scholar]
- 15.Fletcher JE, Sebel PS, Murphy MR, Smith CA, Mick SA, Flister MP. Psychomotor performance after desflurane anesthesia: A comparison with isoflurane. Anesth Analg. 1991;73:260–5. doi: 10.1213/00000539-199109000-00005. [DOI] [PubMed] [Google Scholar]


