Abstract
Context:
Present knowledge about intraoperative management, morbidity, and mortality of patients with undiagnosed catecholamine-producing tumors is mostly based on published case reports and anecdotal evidence.
Aims:
The aim was to summarize the management and outcomes of reported cases and analyze for practice patterns, deduct useful management recommendations as applicable.
Settings and Design:
The Medline database was searched with specific keywords for the period of 1988-2010 for cases of incidental pheochromocytomas and paragangliomas.
Materials and Methods:
Case reports in the English language with a postoperative diagnosis of pheochromocytoma and paraganglioma by histopathology were included. Systematic data extraction from case reports was done.
Statistical analysis used:
Descriptive statistics were applied.
Results:
Of 823 retrieved records, 62 case reports met inclusion criteria. Hemodynamic instability occurred primarily during mass manipulation/intraoperatively (52%, n = 32) and induction/laryngoscopy (18%, n = 11). In cases reporting specific antihypertensive treatments, nitrates (67%, n = 30) represented the majority of medications used, followed by beta-blockers (47%, n = 21). Alpha receptor blockers were administered in 33% (n = 15). The perioperative mortality was 8% (n = 5), and none of these patients received intraoperative alpha blockade. A catecholamine-secreting tumor was suspected intraoperatively in 26% of cases.
Conclusions:
The perioperative mortality based on the reviewed cases of incidental catecholamine producing tumors was less than would traditionally be expected. Intraoperative alpha receptor blockade to treat hypertension was reported in 33% of cases, and none of the patients with a fatal outcome had received it. A higher intraoperative index of suspicion and a lower threshold to consider alpha blocking medications for severe intraoperative hypertension may improve outcomes.
Keywords: Adrenal gland neoplasms, adrenal incidentaloma, anesthesia – general, outcome assessment, paraganglioma
Introduction
Catecholamine-producing tumors originating from the entero-chromafin cells of the adrenal medulla are known as pheochromocytomas, whereas those arising from the extra-adrenal chromafin cells of the sympathetic ganglia are classified as paragangliomas. As the name implies, the latter may be distributed along the paravertebral axis and may be located in the bladder, the prostate and even the heart.[1,2] The majority of these neuroendocrine tumors (80-90%) occur in the adrenal medulla.[3] Signs and symptoms are generally related to catecholamine excess from the secreting tumor: Systemic hypertension, pallor, sweating, palpitations, headaches, and anxiety attacks.[4]
Intraoperative unpredictable paroxysmal release of catecholamines can result in catastrophic cardiovascular complications in the previously undiagnosed patient.[5] Even in medically prepared patients, surgery may still be associated with a 25 % incidence of sustained hypertensive events.[3,6]
The prevalence of incidental intraoperative pheochromocytomas and paragangliomas is unknown, but historically they have been associated with a mortality rate of up to 40%.[7–9] Knowledge about the intraoperative management of patients not previously diagnosed with a neuroendocrine tumor is largely limited to case reports. We theorized that aggregate information from these case reports may inform the clinician about intraoperative management choices in the event of hypertensive crisis, possibly beyond what is already known from patients with a preoperatively diagnosed catecholamine secreting tumor. Additionally postoperative outcomes of the reported cases might provide new clinical insights. Therefore we conducted a review of this literature in the English language over the past 22 years to study and summarize perioperative demographic, management, and outcome data of incidental pheochromocytomas and paragangliomas.
Materials and Methods
We searched the Ovid Medline database and its In-Process Medline file including the years 1988-2010 for cases and case series of incidental pheochromocytoma and paraganglioma during surgery. We chose the starting year for the search as a time when pulse oximetry had been introduced and was now widely used as a surrogate, marking an era of “modern medicine.” A reference librarian assisted with compilation of the articles of interest using a medical subject heading (MeSH) search string. Terms used but not limited to the following included incidentaloma, intraoperative, pheochromocytoma, paraganglioma, neuroendocrine tumor, surgery, and anesthesia. Inclusion criteria were all articles in the English language describing intraoperative management of cases with a preoperatively unsuspected but postoperatively proven diagnosis of either pheochromocytoma or paraganglioma by histopathology. All identified abstracts were reviewed by one of the authors (SH) for eligibility. A second author (RS) was available to resolve uncertainties encountered during the primary review. Full text articles were assessed by both authors for eligibility, and those with a lack of a final histopathologic diagnosis of a catecholamine tumor, or insufficient intraoperative case management information were excluded. Of the remaining manuscripts, patient demographic data, perioperative management, and outcome data including perioperative timing of hemodynamic instability and use and type of vasoactive agents for treatment were extracted by both authors into an electronic database, compared for entry errors, and summarized. In manuscripts describing more than one case, each case with sufficient case detail was counted as a separate case report entry (see also Appendix) and analyzed accordingly. Because of the limited number of articles and their type – case reports and case series – and accordingly the relative simplicity of the data provided, risk of bias assessment or measures of consistency often typical for systematic study reviews were not possible. Descriptive statistics were used, and data were reported in mean ± standard deviation (SD).
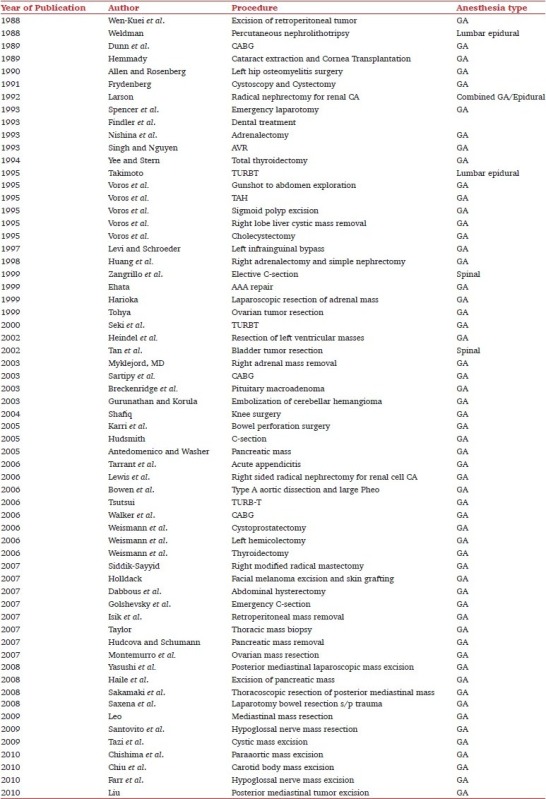
Results
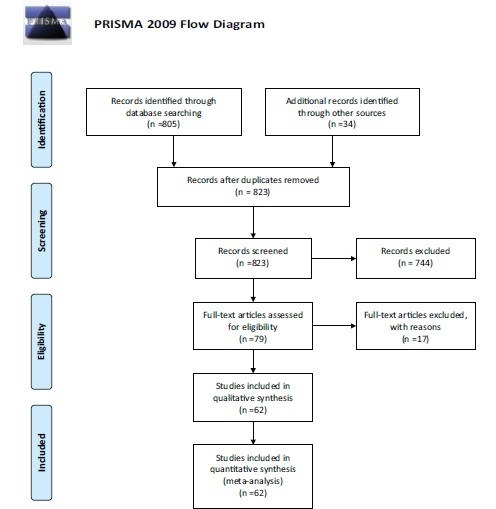
The literature search resulted in 839 abstracts. Sixteen duplicate records were removed, and 823 abstracts were screened. Of these, 744 cases did not report on incidental catecholamine secreting tumors. Seventy-nine full text articles were assessed for eligibility, and an additional 17 were subsequently excluded for reasons mentioned above (PRISMA diagram I). Sixty-two case reports and series met inclusion criteria (Appendix). Anesthetic management included 57 general anesthetics, two spinals, two epidurals, and one combined general/epidural technique. There were 36 men (58 %) and 24 women (39%) as well as two cases lacking gender identification (three percent). Of these patients 71% (n = 43) had a pheochromocytoma, 28 were in men, 14 in women, and two in cases with unreported gender. Paragangliomas were diagnosed in 29% (n = 18) of cases, 8 of whom were men and 10 were women. The patients presented at an age of 50 ± 16 yrs (range 11-87).
Diagram 1.
Intraoperative Management of Patients with Incidental Catecholamine Producing Tumors: A Literature Review and Analysis
In 16 cases (26%), the diagnosis was subsequently suspected intraoperatively.
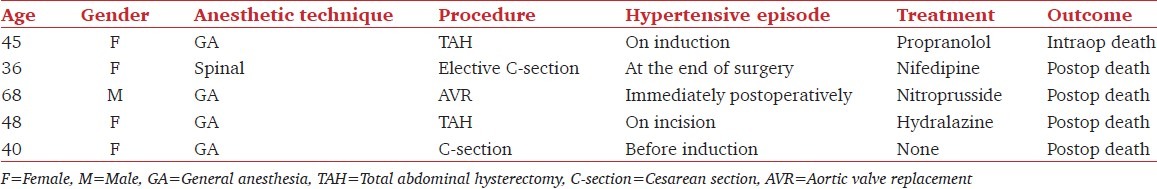
Perioperative mortality was 8% (n = five, Table 1). The publication years of case reports with fatal outcomes were 1993, 1995, 1999, 2005, and 2007. All patients who succumbed were treated with a single antihypertensive agent, and none of them received an alpha receptor blocker intraoperatively. Four of the five deceased patients (80%) required either obstetric (cesarean section, n = two) or gynecologic surgery (hysterectomy, n = two).
Table 1.
Perioperative mortality (n=5)
The mean hospital length of stay was 15 ± 13.3 days (n = 15).
Hemodynamic instability was described as hypertensive episodes, except for one case. Figure 1 shows the perioperative timing of these episodes. They were most frequent (n = 32, 53%) during mass manipulation or otherwise intraoperatively, or occurred at anesthetic induction and laryngoscopy (n = 11, 18%, Figure 1). The terms used to describe hemodynamic instability in the reviewed case reports, such as “hypertensive episode” or “hypertensive crisis” were not specifically defined by the respective authors, but rather used descriptively. However, the term “hypertensive crisis” has been defined in the literature as a systolic blood pressure of greater than 180 mmHg and/or a diastolic blood pressure of greater than 120 mmHg that necessitates immediate blood pressure reduction to prevent or limit end-organ damage.[10] In all our cases the blood pressure elevations described met these criteria for hypertensive crisis. A single patient, later diagnosed with bilateral pheochromocytomas, presented with perioperative hypotension requiring vasopressors. The catecholamine involved in these masses was not reported.
Figure 1.
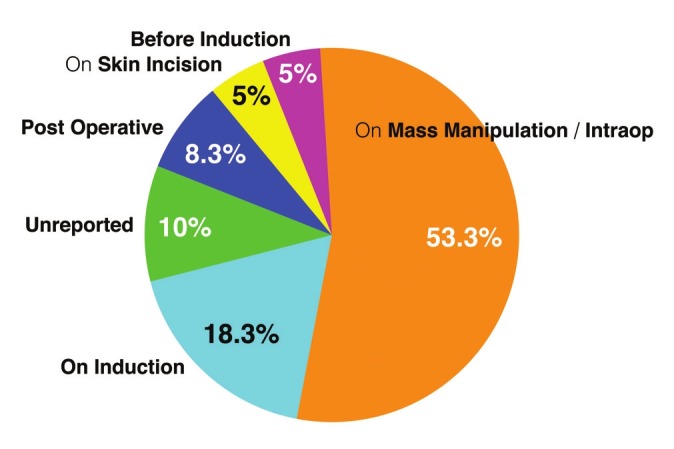
Proportion of the temporal occurrence of hemodynamic instability (n = 62)
In 45 of the 62 cases specific medication use for the treatment of hemodynamic instability was described. Between one and six different vasoactive agents were administered per reported case to treat hypertension [Figure 2]. Overwhelmingly, either one or two or three different agents were chosen to control hypertensive crisis and tachycardia. Use of more than three drugs was infrequent. The types of antihypertensives employed are summarized in Figure 3. Nitrates (67%, n = 30) followed by beta-blockers (47%, n = 21) were given most frequently. Alpha adrenergic receptor blocking agents were used in 33% (n = 15) of patients. Miscellaneous alternatives were chosen less frequently.
Figure 2.
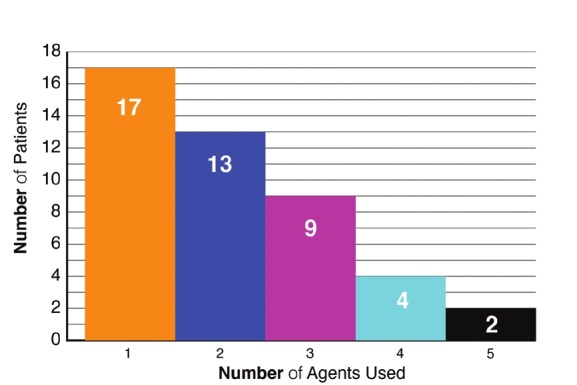
Number of vasoactive agents used per patient (n = 45). Up to five medications were given to treat hemodynamic instability, but in the majority of cases, either 3 agents or less were administered intraoperatively
Figure 3.
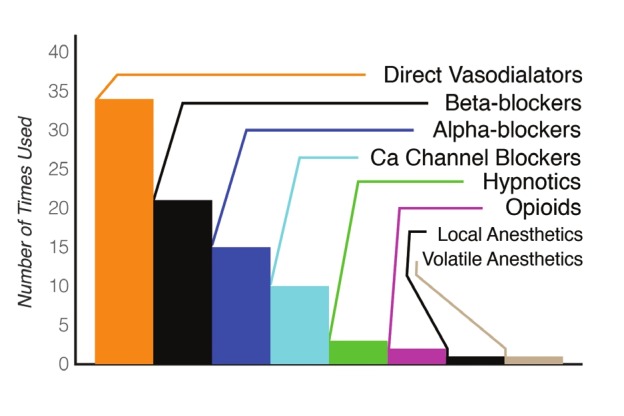
Frequency of treatments with different vasoactive agents during hemodynamic instability. Direct vasodilators: Nitroprusside (n = 18), nitroglycerin (n = 12), hydralazine (n = 4)
Discussion
The true incidence of unsuspected intraoperative catecholamine producing neuroendocrine tumors remains unknown. We report a collective experience of 62 case reports published between 1988 and 2010 according to a Medline search. Although considered rare tumors with a prevalence of 0.1-0.5% in the general population,[11,12] they are diagnosed in only half of the patients on whom a pheochromocytoma is found on autopsy.[13] When diagnosed prior to surgery, preoperative medical preparation emphasizing alpha before beta adrenergic blockade–to prevent unopposed alpha receptor mediated vasoconstriction from catecholamine release-and reversal of volume depletion is recommended.[3] The near 0% perioperative mortality rate for elective pheochromocytoma removal is largely attributed to improved medical preparation and perioperative management.[14] This concept however has been challenged by some, because of the availability of ultrashort acting vasoactive agents for intraoperative use.[15,16] Patients with undiagnosed vasoactive neuroendocrine tumors may be an extraordinary challenge to the intra- and perioperative care team, and the procedure is usually not curative for the mass, so that risks of continued unpredictable catecholamine surges persist following surgery.
In this series, incidental intraoperative catecholamine-producing neuroendocrine tumors have been reported during general, regional, and combined anesthetics. The great majority of these incidental tumors were pheochromocytomas occurring in men. Interestingly, in 30% of the cases, intraoperative hemodynamic instability (hypertension) was unrelated to direct tumor manipulation/intraoperative events or anesthetic induction and laryngoscopy. Hypertensive events were also reported immediately pre- and postoperatively, without further definition of triggers, such as perioperative anxiety or pain.
The majority of the cases report nitrates as the intraoperative antihypertensives used, followed by beta-blockers and limited use of some form of alpha receptor blockade (33%). Rarely were more than three agents employed during one case. It is unclear if additional agents were not needed during the procedure or not readily available at the time.
The 8% mortality in our study was lower than the historically reported 40% incidence for unsuspected intraoperative catecholamine secreting tumors.[4–6] Improved monitoring, better availability of intravenous antihypertensives, and advances in anesthesiology may partially explain this finding. On the other hand, fatal outcomes may not have been reported with a representative frequency. In all five fatal cases of this series, single antihypertensive management without alpha blockers was used. It is undetermined whether multimodal antihypertensive therapy including an alpha blocker could have improved these outcomes. Furthermore four of the five deaths occurred postoperatively, emphasizing the challenge of seamless transition from intraoperative management to postoperative care. Four of these five patients presented either for a hysterectomy or a caesarean section raising questions about the possibility of an increased morbidity or mortality of this particular patient population when an incidental catecholamine producing tumor is present. Certainly during pregnancy, these tumors may be extremely confusing, mimicking pre-eclampsia.[17] While the female gender prevalence for mortality in our study could be a cause for concern, the sample size in this review prevents any generalizability of this finding. Although our literature search spanned 22 years which include improvements in anesthetic technology and pharmacology, the most recent year of a perioperative fatality indicates the persistence of this risk up to today.
Seventeen patients (38%) received a single-agent therapy, the effectiveness of which was often not reported. A diagnosis of pheochromocytoma was suspected intraoperatively only in 26% of patients.
A literature review of case reports such as ours is limited by the available literature, which is biased in at least two ways: that of clinicians selecting their clinical case for manuscript preparation, and that of the journals selecting a submitted manuscript as meeting their publication criteria. Another limitation is the nature of case reports themselves, which do not constitute actual studies that could be further systematically analyzed. Finally, the search was limited to the Medline database, and multiple additional databases may have provided a higher article yield albeit of a potentially different quality.
In instances of rare but worldwide recurring diagnostic and management dilemmas such as those described here, collection and analysis of single reports may still be a way to detect trends and offer otherwise unavailable insights, possibly with practical implications. An organized review such as this one is therefore reminiscent of the American Society of Anesthesiologists closed claims analysis project. Although the source of the data is different, they are inherently incomplete in both instances, yet still interesting, meaningful and sometimes suggesting best practices.
In conclusion, the collective experience extracted from case reports and case series of incidental catecholamine producing neuroendocine tumors suggests a lower than historically reported perioperative mortality. A higher index of suspicion intraoperatively may improve outcomes for patients with such tumors by promoting earlier and more aggressive hemodynamic management. Multiagent antihypertensive therapy including the use of an alpha adrenergic blocker or a combination antihypertensive medication containing an alpha receptor blocking component should be given early consideration for the treatment of unexplained perioperative hypertensive crisis. The benefits of a low threshold to institute invasive hemodynamic monitoring in these situations likely outweigh their risks. Attention to the postoperative care of patients with unexplained intraoperative hypertensive crisis is warranted. Several questions remain, and prospective research or at least data collection is needed. It may be desirable to establish a national or a worldwide prospective data repository of these-and other rare-cases, to ultimately provide evidence-based practice recommendations for patients with unexplained intraoperative hypertensive crisis. It remains to be determined as to how recent national efforts, such as the Multicenter Perioperative Outcomes Group or the Anesthesia Quality Institute in the USA and similar outcome repositories in the UK and other countries using prospectively collected electronic medical data will be able to contribute to such an effort.
Acknowledgments
The authors wish to thank Elizabeth J. Richardson, MLS, MED, Associate Librarian at the Hirsh Health Sciences Library at Tufts University School of Medicine for her invaluable assistance in the literature search.
Appendix
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Young WF., Jr Paragangliomas.Clinical Overview. Ann NY Acad Sci. 2006;1073:21–9. doi: 10.1196/annals.1353.002. [DOI] [PubMed] [Google Scholar]
- 2.Al-Githmi I, Baslaim G, Batawil N. Primary cardiac paraganglioma with dual coronary blood supply presenting with angina chest pain. Can J Cardiol. 2010;26:e278–9. doi: 10.1016/s0828-282x(10)70426-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams DT, Dann S, Wheeler MH. Phaeochromocytoma—views on current management. Eur J Surg Oncol. 2003;29:483–90. doi: 10.1016/s0748-7983(03)00071-4. [DOI] [PubMed] [Google Scholar]
- 4.McClellan MW. Pheochromocytoma: evaluation, diagnosis, and treatment. World J Urol. 1999;17:35–9. doi: 10.1007/s003450050102. [DOI] [PubMed] [Google Scholar]
- 5.Pacak K. Approach to the patient.Preoperative Management of the Pheochromocytoma Patient. J Clin Endocrinol Metab. 2007;9:4069–79. doi: 10.1210/jc.2007-1720. [DOI] [PubMed] [Google Scholar]
- 6.Kinney MA, Warner ME, vanHeerden JA, Horlocker TT, Young WF, Jr, Schroeder DR, et al. Perianesthetic risks and outcomes of pheochromocytoma and paraganglioma resection. Anesth Analg. 2000;91:1118–23. doi: 10.1097/00000539-200011000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Sutton MG, Sheps SG, Lie JT. Prevalence of clinically unsuspected pheochromocytoma.Review of a 50-year autopsy series. Mayo Clin Proc. 1981;56:354–60. [PubMed] [Google Scholar]
- 8.Apgar V, Papper EM. Pheochromocytoma.Anesthetic management during surgical treatment. AMA Arch Surg. 1951;62:634–48. [PubMed] [Google Scholar]
- 9.Welbourn RB. The adrenal glands. In: Welbourn RB, editor. The history of endocrine surgery. New York: Praeger; 1990. pp. 147–15. [Google Scholar]
- 10.Fontes ML, Varon J. Perioperative hypertensive crisis: newer concepts. Int Anesthesiol Clin. 2012;50:40–58. doi: 10.1097/AIA.0b013e31825430fd. [DOI] [PubMed] [Google Scholar]
- 11.Anderson GH, Blakeman N, Streeten DH. The effect of age on prevalence of secondary forms of hypertension in 4429 consecutively referred patients. J Hypertens. 1994;12:609–15. doi: 10.1097/00004872-199405000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Wilhelmsen L, Berglund G. Prevalence of primary and secondary hypertension. Am Heart J. 1977;94:543–6. doi: 10.1016/s0002-8703(77)80120-8. [DOI] [PubMed] [Google Scholar]
- 13.Lo CY, Lam KY, Wat MS, Lam KS. Adrenal pheochromocytoma remains a frequently overlooked diagnosis. Am J Surg. 2000;179:212–5. doi: 10.1016/s0002-9610(00)00296-8. [DOI] [PubMed] [Google Scholar]
- 14.Van Braeckel P, Carlier S, Steelant PJ, Weyne L, Vanfleteren L. Perioperative management of phaeochromocytoma. Acta Anaesthesiol Belg. 2009;60:55–66. [PubMed] [Google Scholar]
- 15.Ulchaker JC, Goldfarb DA, Bravo EL, Novick AC. Successful outcomes in pheochromocytoma surgery in the modern era. J Urol. 1999;161:764–7. [PubMed] [Google Scholar]
- 16.Bravo EL, Tagle R. Pheochromocytoma: state-of-the-art and future prospects. Endocr Rev. 2003;24:539–53. doi: 10.1210/er.2002-0013. [DOI] [PubMed] [Google Scholar]
- 17.Londhey VA, Kulkarni VK. Pheochromocytoma presenting as hypertension in pregnancy. J Assoc Physicians India. 2010;58:508–10. [PubMed] [Google Scholar]


