Abstract
Background:
The ProSeal™ laryngeal mask (PLMA) is increasingly being used as an airway device for laparoscopic surgery. Its silicone cuff allows diffusion of nitrous oxide, carbon dioxide and other gases with resultant rise in its intracuff pressure during anesthesia. The present study was designed to investigate the intracuff pressure changes during anesthesia with and without nitrous oxide in patients undergoing laparoscopic surgery lasting up to two hours.
Materials and Methods:
One hundred patients, American Society of Anesthesiologists physical status 2 and 3, undergoing general anesthesia with muscle paralysis, were randomized into two groups of 50 patients each to receive an anesthetic gas mixture containing either oxygen and nitrous oxide (group N) or oxygen and air (group A). Following insertion of an appropriate size PLMA, its cuff was inflated with air to an intracuff pressure of 45 mm Hg. The cuff pressure was measured every 10 minutes for the entire course of anesthesia. The position of the device was also assessed fiberoptically and postoperative airway complications were recorded.
Results:
The maximum intracuff pressure recorded in group N was 103 ± 4.7 mm Hg vs. 45.5 ± 1.5 mm Hg in group A. The percentage rise in cuff pressure every 10 minutes was also highly significant (P < 0.001) being maximum in first 10 min in group N. The incidence of postoperative airway complications was comparable between the two groups.
Conclusion:
The results of this study demonstrate that the intracuff pressure of the PLMA increases progressively over time when the breathing gas mixture contains nitrous oxide.
Keywords: Anaesthetics, gases, nitrous oxide, equipment, laryngeal mask airway
Introduction
Several cuffed supraglottic airway devices (SADs) have been introduced into clinical practice since the introduction of classic laryngeal mask airway (cLMA). An ideal cuff of a SAD should provide good airway seal during positive pressure ventilation and protect against pulmonary aspiration without causing trauma to the surrounding structures. A recent survey reported that the use of a supraglottic airway as a primary airway management device for general anesthesia is as high as 56.2%.[1] The ProSeal™ laryngeal mask airway (PLMA), is a directional perilaryngeal sealer.[2–4] Its special cuff presses firmly into the periglottic tissues allowing an oropharyngeal seal (≥ 30 cmH2O) without increasing directly measured mucosal pressure.[3,5] Inflating the cuff to an intracuff pressure of 60 cmH2O (45 mmHg) is recommended to prevent leak. Excessive intracuff pressure can result in malposition, suboptimal seal and pharyngolaryngeal morbidity, including sore throat, dysphagia and nerve injury.[2] Nitrous oxide, carbon dioxide and other gases can diffuse into the cuff of airway devices and may further increase the intracuff pressure. There are several reports of the use of PLMA in laparoscopic surgery[6–9] but there is paucity of data on the measurement of intracuff pressure changes during these procedures. The present study was designed to investigate the intracuff pressure changes during anesthesia with and without nitrous oxide in patients undergoing laparoscopic surgery.
Materials and Methods
This randomized prospective study was conducted after obtaining approval from the hospital ethics committee and written informed consent from the patients. One hundred adult patients, of either sex, in American Society of Anesthesiologists physical status 1-2, undergoing elective laparoscopic surgery with an anticipated duration of 30-120 minutes were recruited for the study. Exclusion criteria included obesity (Body Mass Index > 35), oropharyngeal pathology, limited mouth opening (inter-incisor gap < 20 mm) and patients at risk of aspiration (full stomach, previous upper gastrointestinal surgery, hiatus hernia). The patients were randomized by computer generated numbers to one of two groups of 50 patients each. They were to receive an anesthetic gas mixture of oxygen and air (group A) or oxygen and nitrous oxide (group N). Patient enrollment was performed by an investigating anesthesiologist blinded to patient allocation. Anesthetic technique was standardized. After intravenous (IV) access, patients were premedicated with ranitidine 50 mg, metoclopramide 10 mg, glycopyrrolate 0.2 mg and midazolam 1 mg IV. Monitoring included pulse oximetry, electrokardiograph, non-invasive blood pressure, capnography and neuromuscular monitoring with train of four ratios.
Pre-use checkup and size selection of PLMA was done as recommended by the manufacturer.[2]
The transducer (Pressure Monitoring Kit, Edwards Life Sciences, US) to measure the cuff pressure was set up as follows. The transducer was fixed to the operating table by means of clamp (provided by manufacturer) mounted on a steel rod with its height adjusted 10 cm above the operating table top, corresponding to the level of the glottis with the patient lying supine. The transducer cable was attached to the monitor. Other end of transducer was attached to the PLMA cuff with the help of pressure monitoring line, 100 cm long and a three way stop-cock. Zeroing of the transducer was done by opening transducer to the atmosphere and was repeated every 30 minutes or whenever changes were made in patient's position. The entire set-up was filled with air only. The cuff was deflated and the cuff pressure was set at -25 mmHg with the help of a transducer connected to the monitor.
Anesthesia was induced with fentanyl citrate 1.5 mcg/kg and propofol 2 mg/kg IV. Neuromuscular blockade was achieved with vecuronium bromide 0.1 mg/kg IV. One anesthesiologist (out of two anesthesiologists in the study) well versed with PLMA use, inserted and fixed the device with the following two anesthesiologists well versed with PLMA use, inserted and fixed the device. A hand-held cuff manometer (Mallinckrodt Medical, Athlone, Ireland) was connected to the pilot balloon of the PLMA via a three-way stopcock and the cuff was inflated with air to an intracuff pressure of 45 mm Hg (60 cmH2O).
Anesthesia was maintained with 1-2% sevoflurane in oxygen/air or oxygen/nitrous oxide (FiO2 = 0.3). Aliquots of vecuronium bromide 0.02 mg/kg were given for maintenance of neuromuscular blockade, as and when required.
The PLMA was connected to the gas delivery circuit of the anesthesia machine (Prima SP, Penlon, Abingdon, UK). Proper placement of the PLMA was confirmed by; capnography, bilateral chest wall movements and absence of audible leak from the drain tube with the peak airway pressure <20 cmH2O. A maximum of three attempts were allowed. If insertion failed after 3 attempts, the airway was secured by a tracheal tube. Posterior folding of mask was ruled out by passing a gastric tube through the drain tube and its correct position confirmed by aspiration of gastric contents or by auscultating the epigastrium while injecting air. The patients were mechanically ventilated with a tidal volume of 8 ml/kg (volume control mode) with I:E ratio of 1:2. Respiratory rate was adjusted to maintain EtCO2 between 35-45 mmHg.
The oropharyngeal seal pressure (OSP) was measured by giving a fresh gas flow of 4 l/min, closing the expiratory valve of the circuit and noting the pressure at which there was an audible leak. The OSP was not allowed to exceed 40 cmH2O to avoid barotrauma. The position of the PLMA was evaluated by a flexible fiberoptic scope (Olympus LF-2, Japan) introduced into the airway tube, for viewing the laryngeal structures. The fiberoptic view was graded on the following scoring system; 4 = vocal cords only; 3 = vocal cords plus posterior epiglottis (PE); 2 = vocal cords plus anterior epiglottis (AE); 1 = vocal cords not seen.[10]
The peak airway pressure and cuff pressure were monitored. The cuff pressure was recorded every 10 minutes for the entire course of anesthesia, using a transducer which was zeroed every 30 minutes and with every change in patient's position. The measurements were made with the head and neck in neutral position. In both groups, the intra-abdominal pressure was held constant at 15 mmHg by an automatic, high flow insufflation unit (Olympus, UHI 3, Tokyo, Japan). If surgery lasted more than 2 hours, the anesthesiologist was allowed to adjust the intracuff pressure of the PLMA to 45 mmHg but the data collection was terminated at that point. After the completion of procedure, the neuromuscular block was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.02 mg/kg and the PLMA was removed with the cuff inflated. Post-operatively, the patients were assessed by an independent observer blinded to the technique, in the post-anesthesia care unit for sore throat (constant pain, independent of swallowing), dysphagia (difficulty in, or pain provoked by swallowing), hoarseness of voice, dysphonia (difficulty in or pain on speaking) and numbness of the tongue.
Based on a pilot study, the sample size was calculated to detect a difference of 55 % increase in the intracuff pressure in group N when compared to group A at 30 minutes duration of surgery to achieve 90% power at 5% level of significance. The primary variable was the cuff pressure. Statistical tests were performed using SPSS software (17.0 version; SPSS Inc., Chicago, IL, USA). Statistical techniques included quantitative and qualitative analysis. Continuous variables were presented as mean ± SD and categorical variables were expressed as frequencies. Unpaired t-tests were used for comparison of continuous variables between the two groups. Differences between groups were assessed with Chi-square or Fisher's exact test for categorical variables as appropriate. P value of < 0.05 was taken as significant.
Results
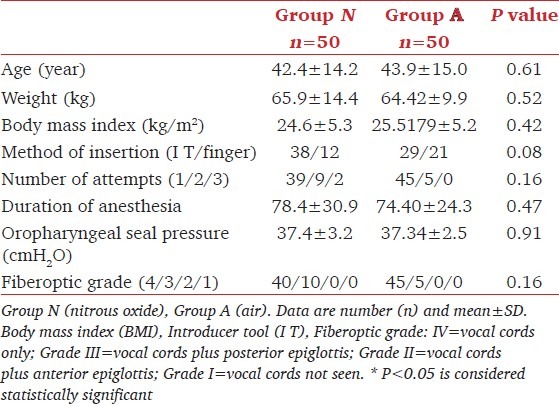
Complete data were obtained from all patients. Data collection was terminated in one patient of group N at 120 min and the cuff pressure was reset to 45 mmHg as the surgery lasted for 220 minutes. The patient characteristics, methods of insertion, and number of insertion attempts, anesthesia time, the mean OSP and fiberoptic position [Table 1] were comparable between the two groups.
Table 1.
Patients characteristics and anesthesia details
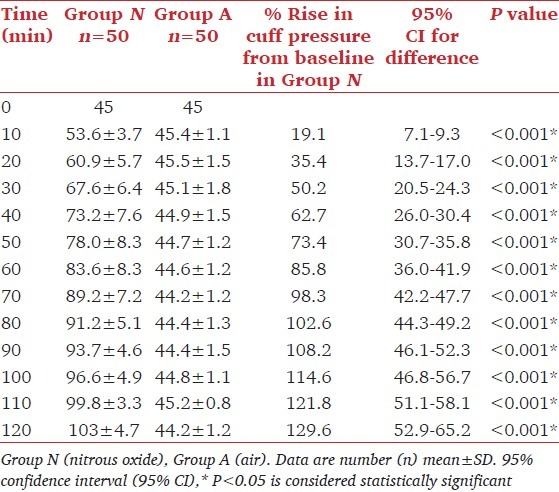
In group N, [Table 2] there was a consistent and significant increase in intracuff pressure over time (P < 0.001) while in group A, it remained stable throughout the procedure (maximum intracuff pressure of 45 mmHg). The maximum intracuff pressure recorded in group N was 103 mmHg which was 129% higher than the baseline (p < 0.001). The percentage rise in cuff pressure every 10 minutes was also highly significant (p < 0.001). It was highest (19%) in the first 10 min, decreasing over time to 5% at 120 minutes. The rise in peak airway pressure after carboperitoneum was comparable between the two groups. There was no evidence of displacement of device in either group.
Table 2.
Intracuff pressure (mmHg) changes of PLMA over time in groups N and A
In the post anesthesia period, five (10%) patients in Group N and one (2%) patient in group A complained of sore throat (p = 0.2). The incidence of sore throat increased with increased number of insertion attempts (p = 0.04) Hoarseness of voice was reported in one (2%) patient in group N. There was no incidence of dysphagia, dysphonia and numbness of tongue in either group.
Discussion
We observed a significant and progressive increase in intracuff pressure of the PLMA over time when nitrous oxide was used as a part of balanced anesthesia technique for laparoscopic surgery. However, the cuff pressure did not change when air was used instead of nitrous oxide (p < 0.001). The incidence of sore throat was comparable between the two groups.
Airway devices have cuffs which are permeable to a variety of gases depending on their partial pressure, and solubility. The composition and thickness of the cuff material (latex, silicone or polyvinyl chloride) play a significant role in the intracuff pressure changes during anesthesia. Nitrous oxide and other gases diffuse into air filled cuffs of tracheal tubes and supraglottic devices, increasing their volume and pressure.[11–13] The addition of plasticizers to the polyvinyl chloride cuff material of the tracheal tubes and disposable LMAs softens it and renders it less permeable to nitrous oxide.[14,15]
The reusable cLMA and PLMA cuffs are made up of silicone. The elastance for the ProSeal™ has been reported to be lower than that of the cLMA, probably due to its larger cuff size.[5] In a case report of a 5h general anesthesia, with gas mixture containing 57-63% nitrous oxide, it was observed that the intracuff pressure of PLMA increased from base line of 45 mmHg to approximately 76 mmHg after one hour, 87 mmHg after two hours, and remained stable thereafter.[12] A similar increase in intracuff pressure from 45 mmHg to 91 mmHg within two hours of surgery has been reported using the laryngeal tube with a silicone cuff.[13] In our study too, the intracuff pressure remained around 45 mmHg in group A while in group N, the percentage rise in cuff pressure every 10 minutes from the baseline was significantly higher (P < 0.001), reaching 103 mmHg, i.e. an increase of 129% from baseline at the end of the 120 min study period. The maximum increase, at first 10 min was due to the increased pressure gradient at initial low intracuff volume. With the passage of time, it declined as the pressure gradient decreased with further diffusion of nitrous oxide into the PLMA cuff.
The rise in the intracuff pressure of the tracheal tubes and supraglottic devices is known to increase the ischemic damage to the surrounding pharyngolaryngeal mucosa.[16–20] Unlike the tracheal tube cuff which expands within the rigid confines of the tracheal rings, the PLMA cuff inflates in the compliant potential space of the pharynx allowing the cuff walls to match the contours of pharyngeal and laryngeal surfaces.[21]
A progressive reduction in the pharyngeal mucosal perfusion has been reported when mucosal pressure increases from 25 to 60 mmHg while using a cuffed oropharyngeal airway.[18] The cuffs of cLMA and PLMA exert pressure on the pharyngeal mucosa causing a concomitant decrease of pharyngeal perfusion and increase in the incidence of post-operative complications including sore throat, dysphonia, and nerve damage.[18–20] Recurrent laryngeal nerve neuropraxia resulting from high cuff pressure due to nitrous oxide influx during anesthesia has been reported following the use of PLMA in a patient with CREST syndrome (Calcinosis, Raynaud's syndrome, Esophageal Dysmotility, Sclerodactyly, Telangiectasia).[22] However, another study with the PLMA suggested that directly measured mucosal perfusion pressure rarely exceeded 25 mmHg[19] and therefore, did not increase pharyngeal mucosal injury, while others recommend reducing the cuff volume until it just seals the leak.[23,24]
A cadaveric study comparing the mucosal pressure induced by cuffs of seven airway devices reported that the cuff of PLMA inflated with maximum recommended cuff volumes, exerted lower pressures (predominantly below 15 mm Hg) on the pharyngeal and hypopharyngeal mucosa than the cuff of cLMA. It was also reported that PLMA along with easy tube, induced significantly higher pharyngeal pressures in the posterior location when compared to other devices. This may be because of the additional cuff on the posterior part of the PLMA.[25]
Higher cuff pressure and higher incidence of postoperative sore throat has also been reported after use of PLMA in children while breathing 50% nitrous oxide and oxygen mixture in comparison to patients whose breathing gases were composed of oxygen and air.[26] Tekin et al. recommended inflating the PLMA cuff with nitrous oxide and oxygen mixture to avoid further increase in cuff pressure when nitrous oxide was a part of general anesthesia technique.[27]
Carbon dioxide used during the laparoscopic procedures gets absorbed into the blood to increase the PaCO2 as well as the end-tidal carbon dioxide, and may diffuse into the cuff to increase intracuff pressure. However, it does not contribute to rise in intracuff pressure as the cuff pressure remained unchanged in group A. The rise in intracuff pressure in group N can be attributed to the diffusion of nitrous oxide which is more diffusible than carbon dioxide.[28] Moreover, the inspired/expired concentration of carbon dioxide was low (4-6.5% vs. 66% for nitrous oxide).
The reported incidence of sore throat with the PLMA is 14-23%.[8,29] In our study, the incidence of sore throat was low and comparable between the two groups. Since we had limited our study to two hours duration, no conclusion can be drawn regarding the incidence of sore throat being related to the duration of anesthesia. As the device is being increasingly used for procedures longer than two hours, vigilance is required during its use and excessive gas should be regularly removed from the cuff.
Our study has a few limitations. We did not record the pharyngeal mucosal pressure or analyze the intracuff gas mixture due to the non-availability of the appropriate equipment (microchip sensors or gas analyzer). Since the number of attempts at insertion also has a significant relationship with the incidence of postoperative sore throat, the study cannot exclusively relate sore throat with rise in intra-cuff pressures.
Conclusion
In conclusion, the results of this study demonstrate that the intracuff pressure of PLMA increases progressively over time when the breathing gas mixture contains nitrous oxide. Use of cuff pressure monitor is recommended for initial cuff inflation as well as for intraoperative monitoring during prolonged surgery when using a nitrous oxide based anesthesia technique. Further studies confined to single attempt of PLMA insertion would be necessary to evaluate the relationship of sore throat with prolonged duration of nitrous oxide based anesthesia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Woodall NM, Cook TM. National census of airway management techniques used for anaesthesia in the UK: first phase of the fourth national audit project at the royal college of anaesthetists. Br J Anaesth. 2011;106:266–71. doi: 10.1093/bja/aeq339. [DOI] [PubMed] [Google Scholar]
- 2.Northfield House, Northfield End, Henley on Thames, Oxon, UK: The Laryngeal Mask Company Limited; 2002. [Last accessed on 2012 Sep 16]. LMA-ProSeal™ Instruction Manual. Available from: http://www.lmaco.com/viewifu.php?ifu=19 . [Google Scholar]
- 3.Brain AJ, Verghese C, Strube PJ. The LMA ‘Proseal’- a laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 4.Miller DM. A proposed classification and scoring system for supraglottic sealing airways: A brief review. Anesth Analg. 2004;99:1553–9. doi: 10.1213/01.ANE.0000134798.00069.2B. [DOI] [PubMed] [Google Scholar]
- 5.Keller C, Brimacombe J. Mucosal pressure and oropharyngeal leak pressure with the ProSeal vs laryngeal mask airway in anaesthetized paralysed patients. Br J Anaesth. 2000;85:262–6. doi: 10.1093/bja/85.2.262. [DOI] [PubMed] [Google Scholar]
- 6.Lu PP, Brimacombe J, Yang C, Shyr M. ProSeal versus the classic laryngeal mask airway for positive pressure ventilation during laparoscopic cholecystectomy. Br J Anaesth. 2002;88:824–7. doi: 10.1093/bja/88.6.824. [DOI] [PubMed] [Google Scholar]
- 7.Maltby JR, Beriault MT, Watson NC, Liepert D, Fick GH. The LMA-ProSeal is an effective alternative to tracheal intubation for laparoscopic cholecystectomy. Can J Anaesth. 2002;49:857–62. doi: 10.1007/BF03017420. [DOI] [PubMed] [Google Scholar]
- 8.Natalini G, Lanza G, Rosano A, Dell’Agnolo P, Bernardini A. Standard laryngeal mask airway and LMA-ProSeal during laparoscopic surgery. J Clin Anesth. 2003;15:428–32. doi: 10.1016/s0952-8180(03)00085-0. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Aquado R, Vivo Benlloch M, Zaragoza Fernandez C, Garcia Solbes JM. ProSeal Laryngeal Mask for Laparoscopic Cholecystectomy. Rev Esp Anestesiol Reanim. 2003;50:55–7. [PubMed] [Google Scholar]
- 10.Keller C, Brimacombe J, Puhringer F. A fiber optic scoring system to assess the position of laryngeal mask devices.Interobserver variability and a comparison between the standard, flexible and intubating laryngeal mask airway. Anasthesiol Intensivmed Notfallmed Schmerzther. 2000;35:692–4. doi: 10.1055/s-2000-8164. [DOI] [PubMed] [Google Scholar]
- 11.Bernhard WN, Yost LC, Turndorf H, Conttrell JE, Peagle RD. Physical characteristics of and rates of nitrous oxide diffusion into tracheal tube cuffs. Anesthesiology. 1978;48:413–7. doi: 10.1097/00000542-197806000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Nicholls M. ProSeal laryngeal mask airway for prolonged middle ear surgery. Br J Anaesth. 2001;87:323–4. [PubMed] [Google Scholar]
- 13.Asai T, Shingu K. Time-related cuff pressures of the laryngeal tube with and without the use of nitrous oxide. Anesth Analg. 2004;98:1803–6. doi: 10.1213/01.ANE.0000117143.75341.A3. [DOI] [PubMed] [Google Scholar]
- 14.Asai T. Difficulty in insertion of the laryngeal mask. In: Latto IP, editor. Difficulties in Tracheal Intubation. 2nd ed. London: W.B. Saunders Company Ltd; 1997. pp. 197–214. [Google Scholar]
- 15.Asai T, Brimacombe J. Cuff volume and size selection with the laryngeal mask. Anaesthesia. 2000;55:1179–84. doi: 10.1046/j.1365-2044.2000.01624.x. [DOI] [PubMed] [Google Scholar]
- 16.Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: Endoscopic study of effects of four large volume cuffs. Br Med J. 1984;288:965–8. doi: 10.1136/bmj.288.6422.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brimacombe J, Berry A. Laryngeal mask airway cuff pressure and position during anaesthesia lasting one to two hours. Can J Anaesth. 1994;41:589–93. doi: 10.1007/BF03009998. [DOI] [PubMed] [Google Scholar]
- 18.Brimacombe J, Keller C, Puhringer F. Pharyngeal mucosal pressure and perfusion: Afiberoptic evaluation of the posterior pharynx in anesthetized adult patient with a modified cuff oropharyngeal airway. Anesthesiology. 1999;91:1661–5. doi: 10.1097/00000542-199912000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Marjot R. Pressure exerted by the laryngeal mask airway cuff upon the pharyngeal mucosa. Br J Anaesth. 1993;70:25–9. doi: 10.1093/bja/70.1.25. [DOI] [PubMed] [Google Scholar]
- 20.O’Kelly SW, Heath KJ, Lawes EG. A study of laryngeal mask inflation.Pressures exerted on the pharynx. Anaesthesia. 1993;48:1075–8. [PubMed] [Google Scholar]
- 21.Brimacombe J, Clarke G, Keller C. Lingual nerve injury associated with ProSeal laryngeal mask airway: A case report and review of literature. Br J Anaesth. 2005;95:420–3. doi: 10.1093/bja/aei187. [DOI] [PubMed] [Google Scholar]
- 22.Kawauchi Y, Nakazawa K, Ishibashi S, Kaneko Y, Ishikawa S, Makita K. Unilateral recurrent laryngeal nerve neuropraxia following placement of a ProSeal laryngeal mask airway in a patient with CREST syndrome. Acta Anaesthesiol Scand. 2005;49:576–8. doi: 10.1111/j.1399-6576.2005.00616.x. [DOI] [PubMed] [Google Scholar]
- 23.Abud TM, Braz JR, Martins RH, Gregorio EA, Saldanha JC. High laryngeal mask airway pressures resulting from nitrous oxide do not increase pharyngeal mucosal injury in dogs. Can J Anaesth. 2001;48:800–6. doi: 10.1007/BF03016698. [DOI] [PubMed] [Google Scholar]
- 24.Reiger A, Brunne B. Is the laryngeal mask a minimally invasive instrument for securing the airway? Anaesthesist. 1999;48:399–402. doi: 10.1007/s001010050805. [DOI] [PubMed] [Google Scholar]
- 25.Ulrich-Pur H, Hrska F, Krafft P, Friehs H, Wulkersdorfer B, Kostler WJ, et al. Comparison of mucosal pressures induced by cuffs of different airway devices. Anesthesiology. 2006;104:933–8. doi: 10.1097/00000542-200605000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Ben-zhen Chen, Li-hui Luo, Lu Jiang, Ru-rong Wang, Jingxia Li, Ling Tan. The effect of nitrous oxide on intracuff pressure of the size 2 ProSeal Laryngeal Mask Airway. J Clin Anesth. 2011;23:214–7. doi: 10.1016/j.jclinane.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Tekin M, Kati I, Tomak Y, Yuca K. Comparison of the effects of room air and N2O+O2 used for ProSeal LMA cuff inflation on cuff pressure and oropharyngeal structure. J Anesth. 2008;22:467–70. doi: 10.1007/s00540-008-0654-y. [DOI] [PubMed] [Google Scholar]
- 28.Lumb AB, Wrigley MW. The effect of nitrous oxide on laryngeal mask cuff pressure in vitro and in vivo studies. Anaesthesia. 1992;47:320–3. doi: 10.1111/j.1365-2044.1992.tb02173.x. [DOI] [PubMed] [Google Scholar]
- 29.Evans NR, Gardner SV, James MF, King JA, Roux P, Bennett P, et al. The ProSeal laryngeal mask: results of a descriptive trial with experience of 300 cases. Br J Anaesth. 2002;88:534–9. doi: 10.1093/bja/88.4.534. [DOI] [PubMed] [Google Scholar]


