Abstract
Background:
Transversus abdominis plane block is a safe, simple and effective technique of providing analgesia for lower abdominal surgeries with easily identifiable landmarks.
Aims:
To compare the analgesic efficacy of transversus abdominis plane block with that of direct infiltration of local anesthetic into surgical incision in lower abdominal procedures.
Settings and Design:
Prospective randomized controlled trial in lower abdominal surgeries done under general anesthesia.
Materials and Methods:
52 ASA I-II patients undergoing lower abdominal gynecological procedures under general anesthesia were divided randomly into two groups each after written informed consent. A bilateral TAP block was performed on Group T with 0.25% bupivacaine 0.6 ml/kg with half the volume on either side intra-operatively after skin closure before extubation using a short bevelled needle, whereas Group I received local infiltration intra-operatively after skin closure with the same amount of drug. The time taken for the first rescue analgesic and visual analog score (VAS) was noted, following which, the patient was administered intravenous morphine 0.1 mg/kg and connected to an intravenous patient controlled analgesia system with morphine for 24 hrs from the time of block administration. 24 h morphine requirement was noted. VAS and sedation scores were noted at 2, 4, 6 and 24 h postoperatively.
Statistical Analysis Used:
The results were analyzed with SPSS 16. A P value < 0.05 was considered significant. Duration of analgesia and 24 h morphine requirement was analysed by Student's t-test. VAS scores, with paired comparisons at each time interval, were performed using the t-test or Mann-Whitney U-test, as appropriate. Categorical data were analyzed using Chi square or Fisher's exact test.
Results:
In Group T, the time to rescue analgesic was significantly more and the VAS scores were lower (P = 0.001 and 0.003 respectively). The 24 hr morphine requirement and VAS at 2, 4, 6 and 24 h were less in the Group T (P = 0.001). Incidence of PONV was significant in Group I (P = 0.043), whereas Group T were less sedated at 2 and 4 h (P = 0.001 and 0.014).
Conclusions:
Transversus abdominis plane block proved to be an effective means of analgesia for lower abdominal surgeries with minimal side-effects.
Keywords: Transversus abdominis plane block, lower abdominal surgeries, local infiltration
Introduction
Gynecological surgeries are often associated with severe pain requiring a well-planned analgesia regimen to ensure adequate patient-comfort, satisfaction, early mobilization, and to decrease the hospital/post-anesthesia care unit (PACU) stay. Transversus abdominis plane (TAP) block was first described by Rafi[1] and works by blocking the thoraco-lumbar nerves (T6–L1) which supply sensory fibers to the anterior abdominal wall. It has been used to provide analgesia for various surgical procedures.[2–9] Local anesthetic infiltration into the surgical site relieves pain at the incision site and is used widely as part of multi-modal analgesia regimens. A comparison of both these methods in terms of duration and quality of analgesia is warranted as both help in alleviating the incisional pain.
We hypothesized that the TAP block would provide a longer duration and better quality of analgesia than that of direct infiltration of surgical incision with local anesthetic.
Materials and Methods
After approval by the Institute Ethics Committee and written informed patient consent, we studied 52 American Society of Anesthesiologists physical status I-II patients scheduled for various lower abdominal (gynecological) surgeries under general anesthesia, in a prospective, investigator-blinded randomized controlled clinical trial. Patients who had a history of relevant drug allergy and tolerance to opiates were excluded from this study.
Patients were randomized by means of a computer-generated random number to either undergo TAP block (Group T, n = 26) or to receive local anesthetic infiltration into surgical incision (Group I, n = 26), intra-operatively, after skin closure, before reversal of patient from general anesthesia.
The patients and the investigator who assessed the patient's parameters postoperatively were blinded to the group assignment. All the patients received a standardised general anesthetic as per the institute protocols. Standard monitoring included non-invasive blood pressure monitoring, arterial oxygen saturation, electrokardiogram and end-tidal carbon-dioxide monitoring. Anesthesia was induced with thiopentone 5-7 mg/kg, fentanyl 2 mcg/kg and atracurium 0.5 mg/kg intravenous (IV) and anesthesia was maintained with isoflurane and 40% oxygen in nitrous oxide. All patients received hourly boluses of fentanyl 0.5 mcg/kg (IV). Prophylactic antiemetics were not administered.
A single investigator, experienced in performing the blocks, administered the TAP block as well as skin infiltration. Bilateral TAP blocks were performed using 18G Tuohy needle using the mid-axillary landmark, piercing the skin two inches cephalad to the iliac crest with a “double-pop” technique. After negative aspiration to exclude vascular puncture, a test dose of 1ml was injected. In case of resistance, indicating that the needle is not between the fascial planes, the needle was repositioned and the tests repeated. A volume of 0.6 ml/kg of 0.25% bupivacaine in two divided doses i.e. 0.3 ml/kg on either side is administered. Group I patients received infiltration of surgical incision with 0.6 ml/kg of 0.25% bupivacaine.
Postoperatively the patients were observed in PACU with standard monitoring. The time for the first request for analgesia in minutes (T-rescue), as well as visual analog scale (VAS) at that time (VAS T-rescue) were noted. Patients were administered morphine 0.1 mg/kg IV in increments on request for analgesia and then connected to intravenous patient-controlled analgesia (IVPCA) system with morphine 1 mg/ml (bolus 1 ml, 5-minute lockout interval, 0.2 mg/kg four hourly dose limit) in both the groups which was continued for 24 h from the time of block administration. Secondary outcomes were 24 h morphine requirement, VAS and sedation scores at 2, 4, 6 and 24 hrs postoperatively. Rescue antiemetics requirement was noted if any. Ondansetron 0.1 mg/kg IV was given as rescue entiemetic. Pain severity was measured using VAS score (0 = no pain and 10 = worst imaginable pain). Sedation was measured using a categorical scoring system (awake and alert = 0, quietly awake = 1, asleep but easily roused-2, deep sleep = 3).
We calculated the sample size based on a pilot study done previously in our hospital. We determined that a study with 22 patients per group would have an 80% power (α = 0.05 and β = 0.2) for a 50% absolute reduction in the mean time for the first request for rescue analgesia. To minimize effect of any data loss, we elected to recruit 26 patients per group into the study.
Statistical analysis was performed using Statistical Package for the Social Sciences 16 (SPSS 16). Demographic data were analyzed using Student's t-test or Fisher's exact test as appropriate. Duration of analgesia and 24 h morphine requirement were analyzed by Student's t-test. VAS scores, with paired comparisons at each time interval, were performed using the t-test or Mann-Whitney U-test as appropriate. Categorical data were analysed using Chi square or Fisher's exact test. Normally distributed data are presented as mean ± SD. The α level for analysis was set at P ≤ 0.05.
Results
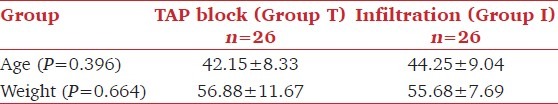
52 subjects entered into the study. All patients who entered randomisation completed the study. Both the groups were comparable in age and weight [Table 1].
Table 1.
Patient characteristics data comparison Group T and Group I
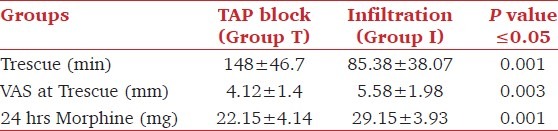
Patients who underwent TAP block took a longer time to request for the first rescue analgesic (P = 0.001), with reduced VAS at T-rescue (P = 0.003) and also reduced 24 h morphine requirement (P = 0.001) [Table 2].
Table 2.
Comparison of time to first rescue analgesic (Trescue), VAS at first request of analgesic (VAS Trescue) and 24h-morphine requirement between Group T and Group I
Postoperative VAS scores in Group T were significantly reduced at 2, 4, 6 and 24 h [Figure 1]. Sedation scores were significantly less at 2 and 4 h (P = 0.001 and 0.014 respectively) [Figure 2]. Post-operative nausea and vomiting (PONV) incidence was significant (P = 0.043) in Group I and required antiemetic administration.
Figure 1.
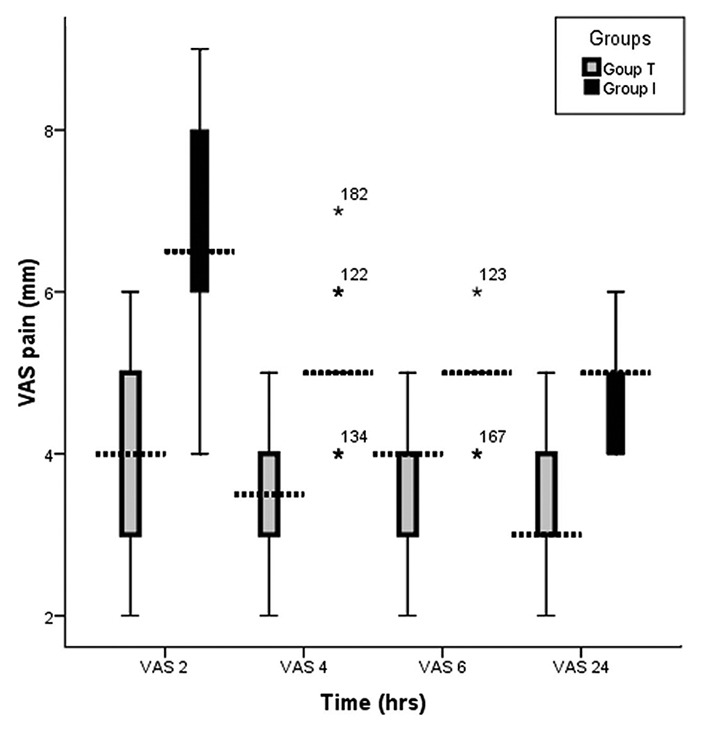
Postoperative VAS scores comparison between Group T and Group I
Figure 2.
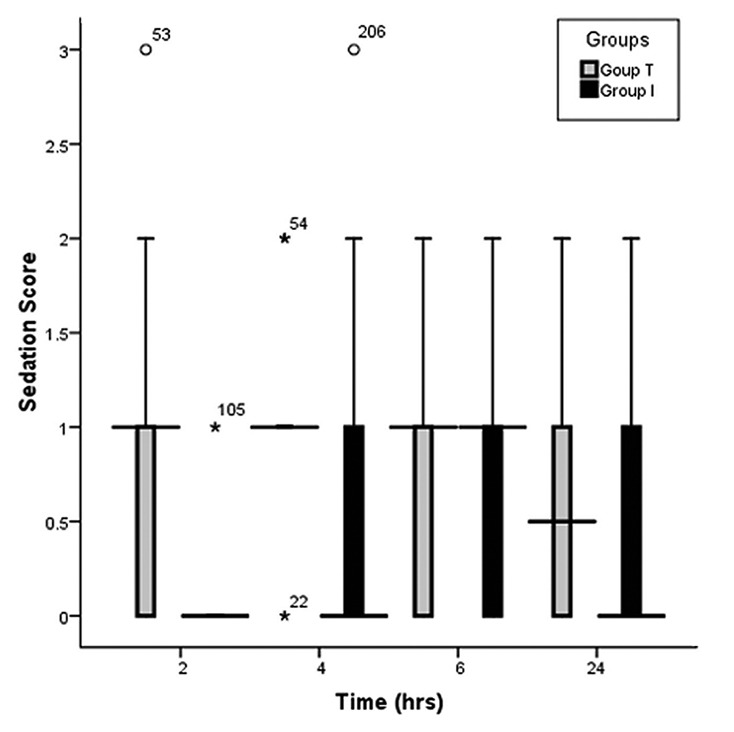
Sedation scores comparison between Group T and Group I
Discussion
The aims of this study were primarily to determine the duration of analgesia of TAP block, the quality of analgesia (as assessed by VAS scores and 24 h morphine requirement) and to note the incidence of side effects - sedation score and PONV which follow opioid usage.
TAP block provided a longer duration and better quality of analgesia as compared to local anesthesia infiltration of surgical incision with lesser sedation and decreased incidence of PONV.
The benefit of TAP block in patients undergoing various procedures such as abdominal hysterectomy,[2] Cesarean section,[3,4] large bowel resection,[5] open retropubic prostatectomy,[6] laparoscopic cholecystectomy[7,8] and appendicectomy[9] has been demonstrated. Most studies compared TAP block with placebo but none compared TAP block with local anesthesia infiltration, athough both take care of the incision pain (parietal component of surgical pain).
McMorrow et al,[4] reported no analgesic benefit with TAP block (with 0.375% bupivacaine) as compared to spinal morphine (100 mcg morphine) in patients undergoing Cesarean section which was possibly due to the analgesic effect of intradural morphine both at the visceral and parietal components of pain, whereas TAP block acts only on the nerves supplying the anterior abdominal wall and thereby subdues parietal component of pain only. No analgesic benefit from ultrasound-guided TAP block (with 0.375% ropivacaine 20 ml on each side) has also been reported in patients undergoing Cesarean section under spinal anesthesia with morphine.[10] However when the opioid sparing effect of ultrasound-guided TAP block after Cesarean delivery (with 0.5% ropivacaine 20 ml on each side) was investigated by another study, opioid consumption was found to be decreased in the first six hours, with lesser 24 h morphine requirement.[11]
We found that incidence of PONV in Group T was significantly lower. This is in contrast to the results of Carney et al,[2] who did not observe any reduction in the incidence or severity of PONV in the TAP block group as compared to placebo group in patients undergoing total abdominal hysterectomy.
Three approaches for the TAP block, subcostal, mid-axillary and lumbar triangle of Petit, were compared.[12] The subcostal approach was associated with a larger area of spread (T7-L1), whereas it was only T10-L1 was achieved with the other two approaches. We used the mid-axillary approach as the level T10-L1 would suffice the incisional pain in lower abdominal procedures reliably. Moreover its landmarks are much clearer and the drug has a paravertebral spread when administered at this location.
We did not use ultrasound for performing TAP block as wider applicability and merit has been shown by previous studies with the landmark technique. The mid-axillary point approach, despite its ill-defined sonoanatomy, has a paravertebral spread, blocking the lateral cutaneous afferents which is not the case with the more sonoanatomically clear anterior approach of the ultrasound-guided block.[4] The local anesthetic distribution might vary with the two approaches. The transversus abdominis neuro-fascial plane, with its contents can act as a depot for prolonged duration of action as compared to a surgical incision, which is highly vascular and probably leads to faster local anesthetic absorption followed by metabolism, which probably explains the lesser duration of action. T-rescue in Group T is 148 ± 46.7 minutes as compared to Group I, which is 85.4 ± 38.1 minutes.
Rozen et al,[13] demonstrated that the nerves located between the costal margin and inguinal ligament in the anterior axillary line have segmental origin from T9-L1 (TAP plexus) and the presence of a fascial layer within the TAP demands the anesthetic be placed between this layer and the transversus abdominis muscle layer. We had used a “double-pop” technique with a large-bore (18G) needle which should reliably deposit the drug beyond the external and internal oblique muscles into the TAP.
A review of incisional local anesthesia for postoperative pain relief after abdominal operations concluded that except for herniotomy, it was not an effective method for postoperative analgesia (appendicectomy, major abdominal surgeries, Caesarean section, abdominal hysterectomy, open cholecystectomy).[14] A meta-analysis on the effectiveness of TAP block concluded that TAP block is comparable to morphine for postoperative analgesia, reduces the requirement of postoperative opioid use, increases time to first request for further analgesia, offers better pain relief and has lesser side effects.[15] The meta-analysis analyzed studies comparing either placebo or no placebo. We compared two standard methods of analgesia for parietal pain - TAP block and local infiltration instead of placebo.
Our study has certain limitations. We did not assess pain on movement, as our primary aim was to find the duration of action of the two techniques, and assessing pain on movement which includes both visceral and parietal components of pain would have influenced the duration of analgesia. Both the techniques studied block only the parietal component of pain originating from the anterior abdominal wall due to the surgical incision and not the visceral component of pain, which may be a major part of pain on movement. Blinding of performer of blocks is not possible due to the varying techniques of both the groups, but, the investigator who assessed the patient postoperatively is blinded to which group the patient belongs. The patient too could not be blinded as there is appreciable loss of sensation or paresthesia with the TAP block, so true blinding may not have been possible.
Further studies are warranted with other local anesthetics, in varying concentrations, doses, with additives, with ultrasound-guided technique, in other surgeries, and also comparing pain on movement. We did not place a continuous block with a catheter, as we wanted to assess the duration of analgesia with a single injection on each side, as well as the procedural considerations of placing bilateral continuous infusions not exceeding the toxic dose limit. We also wanted to study the opioid requirement in the first 24 h postoperatively, which would have been biased by a continuous block.
TAP block is a promising technique in alleviating postoperative pain in patients undergoing lower abdominal gynecological surgeries especially when used as part of multi-modal analgesia regimen. The procedural simplicity of this block, along with reliable level of analgesia (T10-L1), longer duration as well as quality, with lesser opioid requirement and their side-effects makes the TAP block makes a good option for lower abdominal gynecological surgeries.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 2.Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–60. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 3.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after caesarean delivery: A randomized controlled trial. Anesth Analg. 2008;106:186–91. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 4.McMorrow RC, Mhuircheartaigh RJ, Ahmed KA, Aslani A, Ng SC, Conrick-Martin I, et al. Comparison of transversus abdominis plane block vs spinal morphine for pain relief after Caesarean section. Br J Anaesth. 2011;106:706–12. doi: 10.1093/bja/aer061. [DOI] [PubMed] [Google Scholar]
- 5.McDonnell JG, O’Donnell BD, Curley G, Hefferman A, Power C, Laffey JG. Analgesic efficacy of transversus abdominis plane (TAP) block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 6.O’Donnell BD, McDonnell JG, McShane AG. The transversus abdominis plane (TAP) block in open retropubic prostatectomy. Reg Anesth Pain Med. 2006;3:91. doi: 10.1016/j.rapm.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 7.El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, et al. Ultrasound-guided transversus abdominis plane block: Description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–7. doi: 10.1093/bja/aep067. [DOI] [PubMed] [Google Scholar]
- 8.Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58:362–8. doi: 10.4097/kjae.2010.58.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niraj G, Searle A, Mathews M, Misra V, Baban M, Kiani S, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103:601–5. doi: 10.1093/bja/aep175. [DOI] [PubMed] [Google Scholar]
- 10.Costello JF, Moore AR, Wieczorek PM, Macarthur AJ, Balki M, Carvalho JC. The transversus abdominis plane block, when used as part of a multi-modal regimen inclusive of intrathecal morphine, does not improve analgesia after caesarean delivery. Reg Anesth Pain Med. 2009;34:586–9. doi: 10.1097/aap.0b013e3181b4c922. [DOI] [PubMed] [Google Scholar]
- 11.Belavy D, Cowlishaw PJ, Howes M, Phillips F. Ultrasound-guided transversus abdominis plane block for analgesia after Caesarean delivery. Br J Anaesth. 2009;103:726–30. doi: 10.1093/bja/aep235. [DOI] [PubMed] [Google Scholar]
- 12.Milan Z, Tabor D, McConnell P, Pickering J, Kocarev M, du Feu F, et al. Three different approaches to Transversus abdominis plane block: A cadaveric study. Medicinski Glasnik. 2011;8:181–4. [PubMed] [Google Scholar]
- 13.Rozen WM, Tran TMN, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: A new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21:325–33. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 14.Moiniche S, Mikkelsen S, Wetterslev J, Dahl JB. A qualitative systematic review of incisional local anesthesia for postoperative pain relief after abdominal operations. Br J Anaesth. 1998;81:377–83. doi: 10.1093/bja/81.3.377. [DOI] [PubMed] [Google Scholar]
- 15.Siddiqui MRS, Sajid MS, David R, Uncles MB, Cheek L, Baig MK. A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anesth. 2011;23:7–14. doi: 10.1016/j.jclinane.2010.05.008. [DOI] [PubMed] [Google Scholar]


