Abstract
Background:
Presence of major depressive syndrome (MDS) in chronic pain patients (CPPs) requires more attention from the clinicians because of its clinical nature, association of suicidal thoughts and their actual completion, and treatment difficulties. The prevalence of MDS among Indian CPPs is not well studied.
Aim:
To determine the prevalence of MDS among Indian CPPs visiting pain clinic.
Materials and Methods:
In this prospective study, 476 patients who attended a pain clinic in a metropolitan city of India for chronic pain (pain more than six months) were included. They were assessed by ‘PHQ-9 depression scale’ for presence of MDS. Intensity of pain was assessed by ‘Visual analogue scale’ (VAS). Patient details (viz. age, sex), duration and site of pain, and scores of PHQ-9 depression scale and VAS, were noted and statistically analyzed.
Results:
146 out of 476 CPPs (30.67%) were found to suffer from MDS. Women were more prone (F: M =3:2) to develop MDS while suffering from chronic pain. Among 146 CPPs who were suffering from MDS, 108 (73.97%) patients also had suicidal thought. The prevalence of suicidal thought among all CPPs was found to be 22.69%. The depression severity was found to be strongly associated with intensity of pain (P = 0.005 < 0.05) but not associated with the duration of pain (P = 0.159 > 0.05) and age of the patient (P = 0.24 > 0.05).
Conclusion:
We found a high prevalence of MDS among CPPs from India and majority of them also harbored suicidal thought. Therefore, for successful outcome in chronic pain management routine psychological assessment in CPPs should be done to exclude the presence of MDS and suicidal thought.
Keywords: Chronic pain, chronic pain patients, major depressive syndrome PHQ-9
Introduction
Pain which is often described as fifth vital sign is the leading reason for which patients seek medical care.[1,2] The prevalence of chronic pain among general population ranges from 10-46% depending upon the study population surveyed, survey method and definition of chronic pain used.[3,4] In a World Health Organization survey of primary care patients, the prevalence of chronic pain from India was reported as 19%.[5] Bihari et al., found the prevalence of musculoskeletal pain in Indian population to be 25.9%.[6]
Likewise, major depression is a common illness among the general population.[7] According to studies 2 to 4% of persons in the community, 5-10% of primary care patients, and 10-14% of medical inpatients suffer from major depression.[8] Studies done in primary care set up in India, however, have estimated the prevalence rate of depression as high as 21-40.45%.[7]
The co-occurrence of pain and depression is common.[9,10] Depression is more prevalent in chronic pain patients (CPPs) than in the general population as a consequence of the presence of chronic pain.[11,12] These group of patients are prone to suicidal ideation and their actual performance along with other psychological co-morbidity demanding immediate interference and close surveillance. The etiology of the co-occurrence of pain and depression is not clearly explained which may be causally related or may co-occur relatively independently. However, as the biological systems involving both pain and mood regulation are becoming more clearly apparent, it appears that the neural circuit, involved in the processing and regulation of pain and depression, overlaps to some extent; explaining the role of some antidepressants in alleviation of some forms of chronic pain.[13,14] Although, in the majority, pain is the source of depression; in a few, chronic pain is a manifestation of depression. Certain other factors such as financial burden due to chronicity of the disease, restricted physical movements, dependence on others, sleep disturbances, occupational issues, reduced sexual activities, social isolation, are also responsible for depression in these patients.
Prevalence of major depression among CPPs has been estimated to be between 1.5 to 100% depending upon various study settings.[9] However, the prevalence of major depressive syndrome (MDS) in Indian CPPs is not well studied. The purpose of this study was to determine the prevalence of MDS among Indian CPPs visiting pain clinic.
Materials and Methods
In this prospective study, 476 patients who attended pain clinic for chronic pain (e.g., joint pain, back pain, cervical pain, arm or leg pain, generalized body pain etc.) between December 2009 and August 2010 were included. The place of study was a pain clinic situated in a metropolitan city of eastern part of India. Written and explained consents were taken from the patients. Patients refusing to participate or those unable to comprehend for other reasons were excluded from the study. Patient with cancer, cardiovascular disease, diabetes were excluded from this study. The patients who were on antidepressants or on chronic medication due to other psychiatric disorder were also excluded from the study.
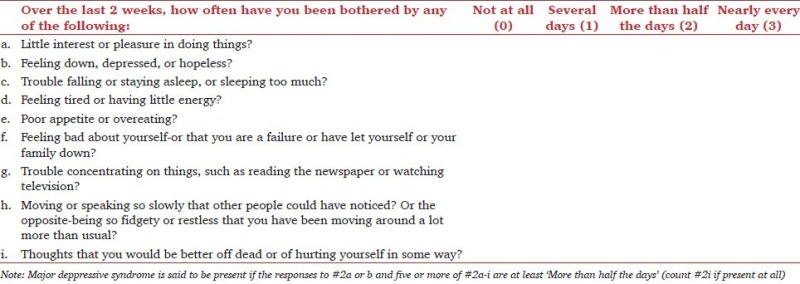
Chronic pain was defined as pain persisting for more than six months. Intensity of pain was assessed by ‘Visual analogue scale’ (VAS). Depression was assessed by the depression module of the ‘Patient Health Questionnaire’ (PHQ), a self-administered version of the mental disorder assessing tool ‘PRIME-MD’, called the ‘Patient Health Questionnaire 9’ (PHQ-9) depression scale.[15,16] A preformed questionnaires comprising nine items, each of which is scored 0 to 3, and thus providing a severity score ranging between 0 to 27, was given to the patients suffering from chronic pain.[16] For diagnosis of MDS we used the diagnostic algorithms [Appendix] given by the PHQ-9 scale i.e., MDS was said to be present if the answers to the questions #2a or b and five or more of #2a to 2i were at least “More than half the days” in the past 2 weeks.[16] Question 2i (“thoughts that you would be better off dead or of hurting yourself in some way”) counts if present at all, regardless of duration.[16] The scores 0, 1, 2, and 3, are assigned to the response categories of “not at all”, “several days”, “more than half the days”, and “nearly every day” respectively. The response categories are based upon the frequency of a particular symptom over the last two weeks. The severity of depression was assessed by PHQ-9 depression severity score (DSS) and graded as none/minimal (0-4), mild (5-9), moderate (10-14), moderately severe (15-19) severe (20-27).
All the participants were first screened for presence of chronic pain as defined in our study i.e., any pain or discomfort that persists continuously or intermittently for longer than 6 months, following which, the pain intensity was assessed using VAS and the depression was assessed using the predefined questionnaire in PHQ-9 scale. The PHQ-9 questionnaire in different languages (Bengali, Hindi and English) was used for different linguistic people. Patient details (viz. age, sex), duration and site of pain, and scores of PHQ-9 depression scale and VAS, were noted. Patients were also grouped according to the depression severity.
Microsoft Excel and SPSS statistical package were used for statistical calculation. The value of ‘p’ less than 0.05 was considered as statistically significant. Fisher's F-test, Student's t-test and Pearson correlation analysis test were used for statistical calculation other than simple mathematical calculations.
Results
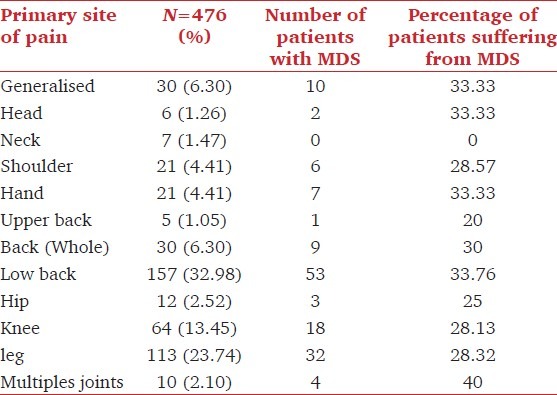
There were a total of 476 patients comprising 281 female (59.03%) and 195 male (40.97%) patients in the sample who were suffering from chronic pain. The average age of the patients was 49.57 years with a range of 18 to 90 years. The average duration of symptoms was 49.35 months with a minimum of six months and a maximum of 35 years. Among the 476 CPPs, 146 were found to suffer from MDS and 108 patients out of those 146 patients were also found to carry suicidal thoughts. Therefore, the prevalence of MDS was 30.67% among patients suffering from chronic pain for more than six months and 73.97% of them (MDS patients) had suicidal thoughts. Demographic characteristics, average duration of pain and average VAS score of CPPs suffering from MDS and those not suffering from MDS were shown in Table 1. CPPs of both the groups, with and without MDS, had similar average age and average duration of pain without any statistical difference (P = 0.269 > 0.05 and 0.257 > 0.05 respectively). However, CPPs with MDS suffered from more intense pain than the CPPs without MDS which is statistically significant (P = 0.018 < 0.05). Female patients with chronic pain suffered more frequently from MDS than the male patients (F:M =1.92:1 and 1.28:1 for patients with and without MDS respectively). Distribution of CPPs according to the primary site of pain revealed that 157 (32.98%) patients were suffering from low back pain which is highest in frequency followed by 113 (23.74%) patients suffering from leg pain [Table 2]. Pain involving multiple joints, low back pain, generalized body ache, pain involving head and hand regions are more commonly associated with MDS.
Table 1.
Demographic characteristics, average duration of pain and average VAS score of the chronic pain patients
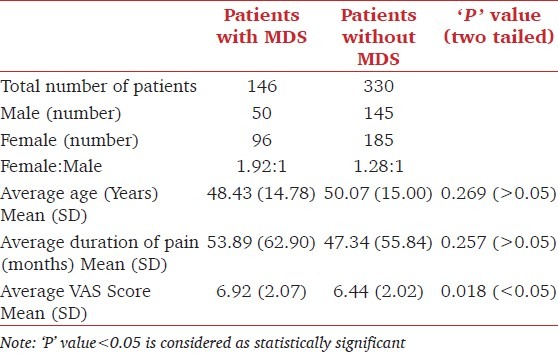
Table 2.
Distribution of the chronic pain patients according to the primary site of pain
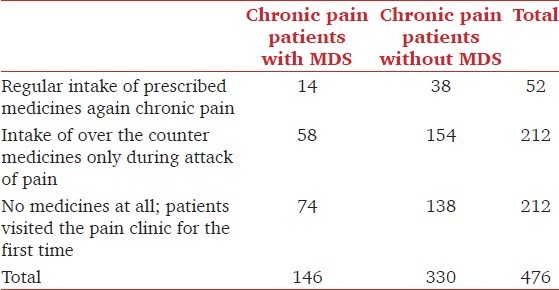
Among all the (N=476) CPPs only 52 patients (10.92%) were on regular medications for pain relief prescribed by physicians and 212 (44.54% of all patients) patients were taking over the counter medication for their pain. Among 146 CPPs who developed MDS, 14 (9.58%) were on regular medicines and 58 (39.73%) were on over the counter medication for their pain. Regular intake of properly prescribed medicines for chronic pain would reduce the risk of developing MDS by 40.4%; whereas, intake of medicines for pain, be it regularly taken and properly prescribed or taken irregularly from over the counter, would decrease the risk of MDS by 22% [Table 3].
Table 3.
Treatment history of the chronic pain patients at the time of visiting the pain clinic
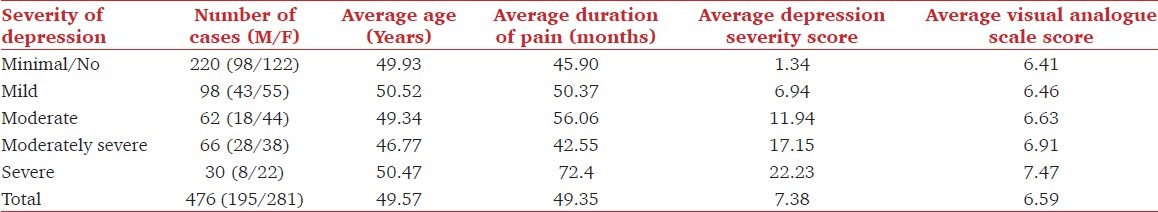
The CPPs were divided into groups on the basis of DSS according to PHQ-9 scale [Table 4]. It was found that among all patients (n = 476), 220 patients (46.22%) had no/minimal depression (score 0-4), 98 patients (20.59%) had mild depression (score 5-9), 62 patients (13.03%) had moderate depression (score 10-14), 66 (13.87%) patients had moderately severe depression (score 15-19), and 30 patients (6.30%) had severe depression (score 20-27). Patient characteristics among different depression severity groups are shown in Table 4. The DSS was found to be increasing with the higher VAS scores. The association of VAS score with DSS was assessed by Pearson correlation test where ‘Pearson correlation coefficient’ value (r) and, the ‘P’ value (two-tailed probability) were found to be 0.128 and 0.005 (<0.05) respectively. This shows a strong association between pain intensity and depression severity. The association between the duration of pain and DSS was also assessed by Pearson correlation test which yielded ‘r’ value and ‘p’ value (two-tailed probability) as 0.065 and 0.159 (>0.05) respectively; implying absence of any relationship between them. The association between the age and DSS was also assessed by Pearson correlation test which also did not reveal presence of any association between the two (‘r’ = -0.054, ‘P’ = 0.24 > 0.05).
Table 4.
Patient characteristics among different depression severity groups
The prevalence of suicidal ideation among CPPs with MDS was 73.97% and among all CPPs was 22.69%. Again, female patients were found to be more affected by suicidal ideation (F:M =2.18:1). The median age for male and female CPPs with suicidal thought was 40 and 46 years respectively. However, the parameters such as age, duration of pain, VAS score; DSS were similar between male and female patients without any statistical difference [Table 5]. The female patients outnumbered the male patients in all the age groups except below 40 years where they were equal to male patients in number [Figure 1].
Table 5.
Characteristics of the chronic pain patients (n = 108) with suicidal ideation
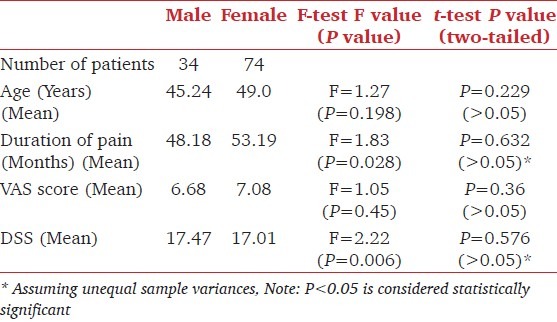
Figure 1.
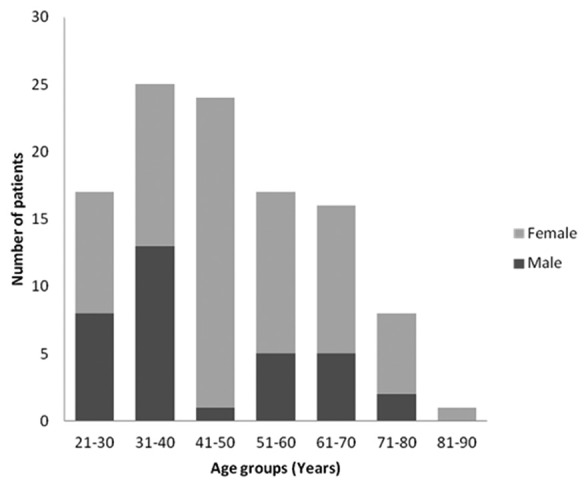
Number of patients with suicidal ideation among different age groups
Discussion
The link behind the association between pain and depression was investigated in various researches and was found to be heterogeneous with considerable overlap in the areas of genetic, structural, functional, neuroendocrine and neurotransmitter functionality.[17] A common theory postulates that depression and painful symptoms follow the same descending pathways of the central nervous system. The most completely described pain modulating circuit includes the amygdala, periaqueductal gray, dorsolateral pontine tegmentum and rostral-ventromedial medulla in the brainstem.[18] Through descending projections, this circuit controls both spinal and trigeminal dorsal horn pain transmission neurons. Several different neurotransmitters such as serotonin and norepinephrine are involved in the modulatory actions of this circuit, which exerts bi-directional control of pain through ‘On cells’ that facilitate and ‘Off cells’ that inhibit dorsal horn nociceptive neurons.[19] With depletion of serotonin and norepinephrine, as occurs in depression, this system may lose its modulatory effect such that minor signals from the body are amplified, and more attention and emotion are focused on them. This explains the multiple pain symptoms in patients with depression, and frequent association of pain with increased attention, focus and negative affect. Antidepressants, belonging to tricyclic antidepressants such as amitriptyline, imipramine and selective serotonin-norepinephrine reuptake inhibitors such as duloxetine, venlafaxine were shown to alleviate some forms of chronic pain.[14,20] They increase the availability of serotonin and norepinephrine by inhibiting their reuptake and thereby increasing their levels in key brain areas they modulate pain sig nals.[14] This pathophysiological correlation explains the frequent coexistence of major depression and chronic pain.[9,13]
The prevalence of major depression among CPPs differs according to the study settings. Bair et al., reviewed the literatures on prevalence rate of major depression among CPPs and found the prevalence rate to be varying within a wide range of 1.5% to 100% which included studies from pain clinic, psychiatric clinic, orthopedic clinic, dental clinic, gynecologic clinic, surgical patients and primary care settings.[9] They found the mean prevalence rate of major depression in CPPs from pain clinics to be 52% which included 15 studies. Our study demonstrated a prevalence rate of 30.67% for MDS in CPPs which is lower than the mean prevalence rate in other pain clinics. Other social, psychological, and biological factors could have accounted for this difference because major depression is a multifactorial disease.
PHQ-9 was taken as the diagnostic tool because it is brief, simple and quick to perform with relatively high positive predictive value and its ability to inform the clinician on both depression severity and diagnostic criteria.[21,22] The nine items of this depression scale are based on the diagnostic criteria for major depressive disorder in the Diagnostic and Statistical Manual Fourth Edition.[16] However, the scoring system based on the duration of symptoms, are modified. It assesses symptoms and functional impairment to make a tentative depression diagnosis, and derives a severity score to help select and monitor treatment. A PHQ-9 score ≥10 has a sensitivity of 88% and a specificity of 88% for diagnosing major depression.[23] This screening tool has been validated in Indian patients for diagnosing major depression.[24] This well validated self-reporting depression screening tool is the best available scale for detecting and monitoring depression in primary care settings.[21,22,25,26] Diagnosis of major depressive disorder (MDD) requires absence of history of a manic episode, absence of any physical disorder, medication or any other drug that may lead to depression as biological cause and absence of normal bereavement symptoms for a duration less than two months as additional criteria to the existing diagnostic criteria for MDS.[16] To keep the investigation procedure simple and comprehensible to all class of people, we considered MDS as a measure of depression which included nine questions as a diagnostic criteria.
Using the PHQ-9 scale patients can be allotted into different groups according to the depression severity. This can help in triage of the patients and thereby helps in administering the type of treatment needed. Kroenke and Spitzer suggested treatment plans according to the various levels of PHQ-9 depression severity.[16] They proposed immediate initiation of pharmacotherapy and/or psychotherapy when the depression severity is moderately severe (score of 15-19), and immediate initiation of pharmacotherapy and quick referral to a psychiatry consultant on poor response to the pharmacotherapy when the depression severity is severe (score of 20-27). When the depression severity is moderate (score of 10-14), treatment is directed to counseling and/or pharmacotherapy. Watchful waiting and follow-up by repeat PHQ-9 screening have been advocated for mild depression (score 5-9).
Despite being used frequently in clinical contexts, chronic pain is not a formal diagnosis. American chronic pain association defines ‘Chronic Pain’ as ongoing or recurrent pain, lasting beyond the usual course of acute illness or injury or more than three to six months, and which adversely affects the individual's well-being. Traditionally chronic pain has been determined by an arbitrary interval of time since onset; with continuation beyond three months and six months since onset are the two most commonly used criteria for diagnosing chronic pain in different studies.[27–29] For the purpose of this study we have included those patients suffering from pain for more than 6 months.
Like other studies, we too found that depression severity increases with the severity of perceived pain (r = 0.931).[30,31] We, however, did not find any association between depression severity and duration of pain (r = 0.065) or age of the individual (r = -0.054). From the results of our study it is evident that intensity of pain rather than duration of pain are responsible for development of MDS in CPPs. We found low back pain as the most frequent cause of chronic pain and also more frequently associated with MDS. Pain involving multiple joints, generalized body ache, pain involving head and hand regions were the other sites which were more commonly associated with MDS. The findings are similar to other studies.[3,4]
We found that large number of patients (89.08%) ignored routine therapy for pain prescribed by physicians despite the sufferings. A half of them, however, took over the counter medicines during acute phase of chronic pain. It can be found that patients on regular treatment had less chance (40.4% reduction of risk) of developing MDS.
Women outnumber men in developing both chronic pain and major depression.[4,32–34] According to the epidemiological studies, the lifetime prevalence of a MDD in women is almost twice that in men, which, however, varies depending upon different ethnic groups.[35] Similarly, in our study the female to male ratio in patients with MDS (F:M-1.92:1) is distinctly higher than patients without MDS (F:M-1.28:1). Several biological processes and social factors are thought to be responsible for the predisposition of women to depression.[35]
Patients with chronic pain frequently go through suicidal ideation, suicide attempts, and suicide completions as a direct consequence of MDS. However, along with other risk factors, chronic pain itself can act as risk factor as was seen in various studies.[36] Pain type, intensity and duration among CPPs act as risk factors for suicidal ideation, independent from the effects of depression severity.[37,38] Tang and Crane in their review article reported the prevalence of suicidal ideation among CPPs to be approximately 20%.[38] This is similar to our findings where we got the prevalence for the same as 22.69%. Tang and Crane also reported the lifetime prevalence of suicide attempts to be between 5 and 14% among CPPs implying a high conversion rate among those patients with suicidal ideation.[38] This warrants the necessity of implementing measures to prevent self-harm and treating the depression aggressively along with the treatment of chronic pain. In our study the mean age of both male and female CPPs with suicidal ideation were 45.24 and 49.0 years respectively. 49 out of 108 CPPs (45.37%) with suicidal ideation belong to an age range of 31 to 50 years. Socioeconomical factors other than chronic pain such as unemployment, economic burden, marital issues, living alone, alcohol and substance abuse etc., could be responsible for this predilection towards the middle age.
MDS is one of the most common psychiatric disorder found in CPPs with a high risk of developing suicidal ideation. Therefore, detection of MDS in its early stage can prevent the development of suicidal ideation and their actual completion. The initial screening for MDS in the outdoor setting can be done using the PHQ-9 scale which also measures the depression severity. The success of treatment for chronic pain not only depends on application of modern therapies including interventional pain management but also depends on early detection of MDS and its timely intervention and referral to psychiatrist if necessary, because both chronic pain and major depression affects each other in a viscious way.[39]
Appendix: PHQ depression module for both diagnostic and severity purposes
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lorenz KA, Sherbourne CD, Shugarman LR, Rubenstein LV, Wen L, Cohen A, et al. How reliable is pain as the fifth vital sign? J Am Board Fam Med. 2009;22:291–8. doi: 10.3122/jabfm.2009.03.080162. [DOI] [PubMed] [Google Scholar]
- 2.Shi Q, Langer G, Cohen J, Cleeland CS. People in pain: How do they seek relief? J Pain. 2007;8:624–36. doi: 10.1016/j.jpain.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Neville A, Peleg R, Singer Y, Sherf M, Shvartzman P. Chronic pain: A population-based study. Isr Med Assoc J. 2008;10:676–80. [PubMed] [Google Scholar]
- 4.Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, et al. Common chronic pain conditions in developed and developing countries: Gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9:883–91. doi: 10.1016/j.jpain.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Gureje O, Von Korff M, Smion GE, Gater R. Persistent pain and well-being.A World Health Organization study in primary care. JAMA. 1998;280:147–51. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 6.Bihari V, Kesavachandran C, Pangtey BS, Srivastava AK, Mathur N. Musculoskeletal pain and its associated risk factors in residents of National Capital Region. Indian J Occup Environ Med. 2011;15:59–63. doi: 10.4103/0019-5278.90375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grover S, Dutt A, Avasthi A. An overview of Indian research in depression. Indian J Psychiatry. 2010;52:S178–88. doi: 10.4103/0019-5545.69231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry. 1992;14:237–47. doi: 10.1016/0163-8343(92)90094-q. [DOI] [PubMed] [Google Scholar]
- 9.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med. 2003;163:2433–45. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 10.Lépine JP, Briley M. The epidemiology of pain in depression. Hum Psychopharmacol. 2004;19:S3–7. doi: 10.1002/hup.618. [DOI] [PubMed] [Google Scholar]
- 11.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: Antecedent or consequence of chronic pain.A review? Clin J Pain. 1997;13:116–37. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Manchikanti L, Fellows B, Pampati V, Beyer C, Damron K, Barnhill RC. Comparison of psychological status of chronic pain patients and the general population. Pain Physician. 2002;5:40–8. [PubMed] [Google Scholar]
- 13.Gambassi G. Pain and depression: The egg and the chicken story revisited. Arch Gerontol Geriatr. 2009;49:103–12. doi: 10.1016/j.archger.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Briley M, Moret C. Treatment of comorbid pain with serotonin norepinephrine reuptake inhibitors. CNS Spectr. 2008;13:22–6. doi: 10.1017/s1092852900028285. [DOI] [PubMed] [Google Scholar]
- 15.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–21. [Google Scholar]
- 17.Narasimhan M, Campbell N. A tale of two comorbidities: Understanding the neurobiology of depression and pain. Indian J Psychiatry. 2010;52:127–30. doi: 10.4103/0019-5545.64586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fields HL. Pain modulation: Expectation, opioid analgesia and virtual pain. Prog Brain Res. 2000;122:245–53. doi: 10.1016/s0079-6123(08)62143-3. [DOI] [PubMed] [Google Scholar]
- 19.Fields HL, Heinricher MM, Mason P. Neurotransmitters in nociceptive modulatory circuits. Annu Rev Neurosci. 1991;14:219–45. doi: 10.1146/annurev.ne.14.030191.001251. [DOI] [PubMed] [Google Scholar]
- 20.Jann MW, Slade JH. Antidepressant agents for the treatment of chronic pain and depression. Pharmacotherapy. 2007;27:1571–87. doi: 10.1592/phco.27.11.1571. [DOI] [PubMed] [Google Scholar]
- 21.Nease DE, Jr, Maloin JM. Depression screening: A practical strategy. J Fam Pract. 2003;52:118–24. [PubMed] [Google Scholar]
- 22.Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: A systematic review. Gen Hosp Psychiatry. 2007;29:388–95. doi: 10.1016/j.genhosppsych.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kochhar PH, Rajadhyaksha SS, Suvarna VR. Translation and validation of brief patient health questionnaire against DSM IV as a tool to diagnose major depressive disorder in Indian patients. J Postgrad Med. 2007;53:102–7. doi: 10.4103/0022-3859.32209. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen Hosp Psychiatry. 2010;32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Löwe B, Unützer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004;42:1194–201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Turk DC, Okifuji A. Pain terms and taxonomies of pain. In: Loeser JD, Butler SH, Chapman CR, Turk DC, editors. Bonica's management of pain. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 18–25. [Google Scholar]
- 28.Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry. 2003;60:39–47. doi: 10.1001/archpsyc.60.1.39. [DOI] [PubMed] [Google Scholar]
- 29.Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68:262–8. doi: 10.1097/01.psy.0000204851.15499.fc. [DOI] [PubMed] [Google Scholar]
- 30.Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G. Predictors of depression in a sample of 1,021 primary care patients with osteoarthritis. Arthritis Rheum. 2007;57:415–22. doi: 10.1002/art.22624. [DOI] [PubMed] [Google Scholar]
- 31.Muñoz RA, McBride ME, Brnabic AJ, López CJ, Hetem LA, Secin R, et al. Major depressive disorder in Latin America: The relationship between depression severity, painful somatic symptoms, and quality of life. J Affect Disord. 2005;86:93–8. doi: 10.1016/j.jad.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein RD, Gruenberg AM. Major Depressive Disorder in the older adult: Implications for women. J Women Aging. 2007;19:63–77. doi: 10.1300/J074v19n01_05. [DOI] [PubMed] [Google Scholar]
- 33.Accortt EE, Freeman MP, Allen JJ. Women and major depressive disorder: Clinical perspectives on causal pathways. J Womens Health (Larchmt) 2008;17:1583–90. doi: 10.1089/jwh.2007.0592. [DOI] [PubMed] [Google Scholar]
- 34.Chin ML, Rosenquist R. Sex, gender, and pain: “Men are from Mars, women are from venus.”. Anesth Analg. 2008;107:4–5. doi: 10.1213/ane.0b013e3181788ca3. [DOI] [PubMed] [Google Scholar]
- 35.Noble RE. Depression in women. Metabolism. 2005;54:49–52. doi: 10.1016/j.metabol.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 36.Fishbain DA. The association of chronic pain and suicide. Semin Clin Neuropsychiatry. 1999;4:221–7. doi: 10.153/SCNP00400221. [DOI] [PubMed] [Google Scholar]
- 37.Smith MT, Perlis ML, Haythornthwaite JA. Suicidal ideation in outpatients with chronic musculoskeletal pain: An exploratory study of the role of sleep onset insomnia and pain intensity. Clin J Pain. 2004;20:111–8. doi: 10.1097/00002508-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Tang NK, Crane C. Suicidality in chronic pain: A review of the prevalence, risk factors and psychological links. Psychol Med. 2006;36:575–86. doi: 10.1017/S0033291705006859. [DOI] [PubMed] [Google Scholar]
- 39.Sharp J, Keefe B. Psychiatry in chronic pain: A review and update. Curr Psychiatry Rep. 2005;7:213–9. doi: 10.1007/s11920-005-0056-x. [DOI] [PubMed] [Google Scholar]


