Abstract
Management of neuraxial anesthesia/analgesia in anticoagulated patient can be challenging. The shortest safe time to remove epidural catheter, after a patient receives long-acting dual antiplatelet agents (clopidogrel and aspirin), is unclear. American Society of Regional Anesthesiology (ASRA) guidelines recommend seven days interval for the epidural placement after clopidogrel administration. However ASRA Guideline did not specify the time for epidural catheter removal, and did not specify how much time elapse necessary after dual antiplatelet therapy with clopidogrel and aspirin. We report a case of safe removal of epidural catheter 72 hours after oral dose of clopidogrel and aspirin with a normal platelet function analysis and normal thromboelastography before removal.
Keywords: Anticoagulation, clopidogrel, epidural, thromboelastography
Introduction
Epidural Hematoma is a rare but potentially serious complication of neuraxial anesthesia/analgesia. The incidence of this condition is estimated to be in the range of <1 in 150,000 to 200,000 epidural anesthetics and <1 in 220,000 after spinal anesthetics in patients without additional risk factors.[1,2] The etiology of this complication is believed to be trauma to epidural vessels during catheter placement and/or removal. A review of the literature by Vandermeulen et al., suggested that catheter removal is nearly as risky for epidural hematoma as catheter insertion.[3,4] Puncture of epidural vessels is estimated to occur at a rate of 3-12% for each attempt at epidural placement.[1] Based on review of the case series and large inclusive surveys the principal risk factors for neuraxial bleeding complications include hemostatic defects and/or procedural difficulties with multiple puncture attempts. The American Society of Regional Anesthesia and Pain Medicine released their 3rd edition practice advisory in 2010 outlining evidence based recommendations regarding timing of catheter placement in relation to antithrombotic therapy, which is seven days after clopidogrel therapy and 24 hours after low molecular weight heparin.[5]
Case Report
A 62-years-old man with a palpable mass in the popliteal fossa was found on magnetic resonance imaging (MRI) to have a thrombus-containing popliteal aneurysm. The patient had history of coronary artery disease for which percutaneous coronary intervention with single bare metal stent placement was done. Patient also suffered from hypertension, obstructive sleep apnea, paroxysmal atrial fibrillation, and a small infrarenal abdominal aortic aneurysm. Angiography demonstrated complete occlusion of the right popliteal artery caused by the aneurysm. Review of a recent 2D transthoracic echocardiography revealed normal left ventricular wall motion with ejection fraction (EF) of 55% and mild mitral regurgitation. He had completed a one-month course of clopidogrel therapy following bare metal coronary artery stent placement and was currently on aspirin 325 mg daily, which he discontinued 72 hours prior to surgery. Pre-operative laboratory tests were unremarkable including a hematocrit of 41%, platelet count of 166,000, and normal PTT, PT and INR.
A lumbar epidural catheter was placed at the L3-L4 inter-space uneventfully on first attempt using an 18 G Tuohy needle with loss of resistance technique. A test dose of 3 mL of 1% lidocaine with epinephrine 1:200,000 was negative. The catheter was intermittently dosed to a total of 25 mL of 0.5% bupivacaine and a sensory blockade level of T6 was obtained. The patient underwent the resection of the thrombosed popliteal aneurysm with a saphenous vein graft interposition. He was hemodynamically stable throughout the procedure. Intra-operatively the patient received 10,000 units of heparin which was reversed after approximately 1 hour of anticoagulation with 75 mg of protamine. Following surgery he was transported to the ICU in stable condition. His pain was adequately managed postoperatively with Patient-Controlled Epidural Analgesia using a basal infusion of 0.2% ropivacaine at 10 mL/hour and a patient controlled bolus dose of 5 mL with a 30 minute lockout period. Immediately on arrival to the ICU he was started on enoxaparin 90 mg twice a day subcutaneously. The following morning he received one oral dose of clopidogrel 75 mg and Aspirin 325 mg accidentally.
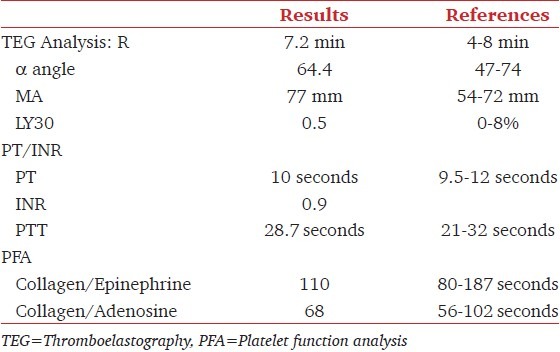
Several hours later anesthesia consult was sought to evaluate for epidural catheter removal. Aspirin and clopidogrel were then immediately discontinued in preparation for epidural catheter removal. Due to concerns for bleeding complications with epidural catheter removal in the setting of anticoagulation and antiplatelet therapy, the decision was made to remove epidural catheter 72 hours after the clopidogrel and aspirin dose contingent upon acceptable coagulation and platelet function parameters. The patient continued to receive subcutaneous enoxaparin 90 mg twice a day with the last dose being 24 hours before the planned epidural catheter removal. After approximately 72 hours had elapsed since receiving a dose of clopidogrel 75 mg and aspirin 325 mg, routine coagulation tests, platelet function assay (PFA) and thromboelastography (TEG) were obtained as shown in Table 1. The exact times medications were administered (last doses) relative to time of catheter removal are as following: Aspirin 325 mg orally at 0859 h on postoperative day 1; Clopidogrel 75 mg orally at 0859 h on postoperative day 1; Enoxaparin 90 mg subcutaneously at 0920 h on postoperative day 3 and epidural catheter removal at 0926 h on postoperative day 4.
Table 1.
TEG, PT INR and PFA results when removal of epidural catheter
After a thorough discussion was made with the patient regarding the risk of epidural hematoma and patient's consent was obtained, the catheter was removed uneventfully. He was monitored in the surgical intensive care for two hours following catheter removal and was discharged home that evening in stable condition. Following discharge the patient was contacted by phone daily for one week to evaluate for symptoms of epidural hematoma. He remained asymptomatic and was restarted on clopidogrel 75 mg daily as an outpatient.
Discussion
The increasingly realized benefits of neuraxial techniques in reducing surgical morbidity and mortality and improving patient-oriented outcomes[6] have led to the widespread use of neuraxial block in indicated surgical procedures. Prophylaxis of postoperative thromboembolic complications with various strategies (anticoagulations, antiplatelets, and thrombolytics) are also increasingly used by surgery teams. These lead to the inevitable overlap in some patients who will receive both at the same time. This combination of neuraxial catheter placement and antithrombotic therapy may potentially cause serious complication(s) postoperatively. Managing these patients involves a delicate balance of minimizing the incidence of bleeding into epidural/spinal space causing epidural/spinal hematoma and the risks of thromboembolic complications due to cessation of anticoagulation. It is necessary to consider the inherent risks associated with neuraxial techniques and evaluate for the presence of risk factors that may jeopardize the safety of regional anesthesia.
The ASRA Practice Guidelines serve as a guide for safely administering neuraxial anesthesia in the setting of antithrombotic therapy.[5] However these guidelines are based primarily on expert opinion, case reports and clinical series as opposed to higher levels of evidence obtained from randomized prospective clinical trials and meta-analysis. These guidelines are generally very conservative due to medicolegal concerns. Thus occasional variances from these recommendations may be acceptable based on the judgment of the individual practitioner.
Our patient had a smooth epidural placement prior to vascular surgery and uneventful intraoperative course. However immediately after the surgery the patient was administered high dose of enoxaparin subcutaneous by the surgical team. The ASRA Guidelines recommend delaying 24 hours for the first dose postoperatively and 24 hours after the last dose for epidural catheter removal. Our patient was placed at an increased risk of bleeding from a premature administration of high dose enoxaparin and received twice daily afterwards. The following morning, the patient received a dose of clopidogrel 75 mg and aspirin 325 mg. It is widely accepted that antiplatelet agents have synergistic effects in regards to risk for bleeding.[7] The ASRA Guidelines suggest a seven day interval between discontinuation of clopidogrel therapy and neuraxial blockade[5] and additionally obtain documentation of normalization of platelet function if neuraxial blockade is indicated between five and seven days after discontinuation, but ASRA Guideline did not specifically discuss how antiplatelet therapy affects timing of catheter removal. Our decision to remove epidural catheter at 72 hours instead of seven days after clopidogrel and aspirin dose was based on the following considerations: patient had only one oral dose of clopidogrel and aspirin, he did not have previous coagulopathy, twice daily enoxaparin dose will be stopped 24 hours prior the planned catheter removal, and most importantly, he had coronary artery disease with bare metal stents which necessitated resumption of antiplatelet therapy postoperatively as soon as possible. Obviously the decision of epidural removal 72 hours after last doses of clopidogrel and aspirin was not completely arbitrary, it was also a compromise between withholding anticoagulation in preparing for epidural removal and the necessity of preventing coronary thrombosis because this patient has bare metal coronary stent. The elimination half-life of enoxaparin, which is three to six hours after subcutaneous injection, is dose independent. The ASRA Guidelines also suggest at least a 24 hours delay following high dose enoxaparin therapy prior to epidural placement thus we applied this concept to epidural catheter removal. The patient was continued on enoxaparin therapy to prevent thromboembolic complications while cessation of antiplatelet therapy and enoxaparin therapy was subsequently discontinued 24 hours prior to the planned catheter removal. Measuring anti-Xa level to monitor the anticoagulant response to enoxaparin is not predictive of risk of bleeding[8] and thus was not obtained prior to catheter removal in our case.
The antiplatelet effect from clopidogrel results from inhibition of adenosine diphosphate-induced platelet aggregation and interference with platelet-fibrinogen binding. Without a loading dose, steady state levels are achieved within seven days of therapy. The degree of platelet function inhibition following a single dose of clopidogrel and prior to obtaining steady state drug levels is not clear. However it is widely accepted that a combination of antiplatelet drugs, like aspirin and clopidogrel, together evoke a higher risk of bleeding complications than either agent alone.[7] Following a 72-hours time interval assays of platelet function were obtained to assess residual clopidogrel effect. Thromboelastography was also performed to provide a global assessment of hemostasis prior to catheter removal.
Following epidural catheter removal it is critical to monitor these patients closely for signs and symptoms suggesting cord compression from a spinal hematoma. Patient usually complains of severe back pain and loss of sensory and motor function. Surgical decompression within 8 hours of onset of neurologic dysfunction results in maximal neurologic recovery. Delayed surgical intervention will likely lead to permanent neurological deficits.
In summary, platelet functional analysis and thromboelastography offer potentially reliable guidance for epidural catheter removal in patient who had received double antiplatelet therapy and 72 hours after single dose of clopidogrel and aspirin is safe for the removal of epidural catheter. However, we are not sure what is the shortest time after oral dual agents (aspirin and clopidogrel) for epidural catheter removal and placement. Considering a reasonable balance of minimizing the risk of epidural hematoma and the risks of thromboembolic events, it may very likely be less than 72 hours.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Horlocker TT. Regional anaesthesia in the patient receiving antithrombotic and antiplatelet therapy. Br J Anaesth. 2011;107:i96–106. doi: 10.1093/bja/aer381. [DOI] [PubMed] [Google Scholar]
- 2.Tryba M. European practice guidelines: Thromboembolism prophylaxis and regional anesthesia. Reg Anesth Pain Med. 1998;23:178–82. doi: 10.1016/s1098-7339(98)90144-4. [DOI] [PubMed] [Google Scholar]
- 3.Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165–77. doi: 10.1213/00000539-199412000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Vandermeulen E. Regional anaesthesia and anticoagulation. Best Pract Res Clin Anaesthesiol. 2010;24:121–31. doi: 10.1016/j.bpa.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Horlocker TT, Wedel DJ, Rowlingson JC, Enneking FK, Kopp SL, Benzon HT, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition) Reg Anesth Pain Med. 2010;35:64–101. doi: 10.1097/aap.0b013e3181c15c70. [DOI] [PubMed] [Google Scholar]
- 6.Liu SS, Carpenter RL, Neal JM. Epidural anesthesia and analgesia.Their role in postoperative outcome. Anesthesiology. 1995;82:1474–506. doi: 10.1097/00000542-199506000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Payne DA, Haynes PD, Jones CI, Belham P, Naylor AR, Goodall AH. Combined therapy with clopidogrel and aspirin significantly increase the bleeding time through a synergistic antiplatelet action. J Vasc Surg. 2002;35:1204–9. doi: 10.1067/mva.2002.122027. [DOI] [PubMed] [Google Scholar]
- 8.Paige JT, Gouda BP, Gaitor-Stampley V, Scalia PG, Klainer TE, Raum WJ, et al. No correlation between anti-factor Xa levels, low-molecular-weight heparin, and bleeding after gastric bypass. Surg Obes Relat Dis. 2007;3:469–75. doi: 10.1016/j.soard.2006.12.012. [DOI] [PubMed] [Google Scholar]


