Abstract
The contribution made by the private sector to health care in a low- or middle-income country may affect levels of physician emigration from that country. The increasing importance of the private sector in health care in the developing world has resulted in newfound academic interest in that sector’s influences on many aspects of national health systems. The growth in physician emigration from the developing world has led to several attempts to identify both the factors that cause physicians to emigrate and the effects of physician emigration on primary care and population health in the countries that the physicians leave. When the relevant data on the emerging economies of Ghana, India and Peru were investigated, it appeared that the proportion of physicians participating in private health-care delivery, the percentage of health-care costs financed publicly and the amount of private health-care financing per capita were each inversely related to the level of physician expatriation. It therefore appears that private health-care delivery and financing may decrease physician emigration. There is clearly a need for similar research in other low- and middle-income countries, and for studies to see if, at the country level, temporal trends in the contribution made to health care by the private sector can be related to the corresponding trends in physician emigration. The ways in which private health care may be associated with access problems for the poor and therefore reduced equity also merit further investigation. The results should be of interest to policy-makers who aim to improve health systems worldwide.
Résumé
La contribution apportée par le secteur privé aux soins de santé dans les pays à revenu faible ou intermédiaire peut modifier les taux d'émigration des médecins de ces pays. L'importance croissante du secteur privé dans les soins de santé dans les pays en voie de développement a suscité un regain d'intérêt académique dans les influences de ce secteur sur de nombreux aspects des systèmes de santé nationaux. La croissance de l'émigration des médecins des pays en voie de développement a conduit à plusieurs tentatives d'identifier à la fois les facteurs qui incitent les médecins à émigrer et les effets de l'émigration des médecins sur les soins primaires et la santé de la population dans les pays qu'ils quittent. Lorsque les données pertinentes sur les économies émergentes du Ghana, de l'Inde et du Pérou ont été étudiées, il est apparu que la proportion de médecins qui participent à la prestation des soins privés, le pourcentage de dépenses de santé financées publiquement et le montant du financement des soins de santé privés par habitant ont été chacun inversement proportionnels au taux d'expatriation des médecins. Ainsi, la prestation et le financement de soins de santé privés peuvent réduire l'émigration des médecins. Il existe clairement un besoin de recherches similaires dans d'autres pays à revenus faible et intermédiaire, ainsi que d'études pour voir si, au niveau du pays, les tendances temporelles de la contribution aux soins de santé par le secteur privé peuvent être liées aux tendances correspondantes de l'émigration des médecins. Les façons dont les soins de santé privés peuvent être associés à des problèmes d'accès pour les pauvres et, par conséquent l'équité réduite, méritent également une enquête plus approfondie. Les résultats devraient intéresser les décideurs politiques qui visent à améliorer les systèmes de santé à travers le monde.
Resumen
La aportación del sector privado a la atención sanitaria en un país de ingresos medios o bajos puede repercutir en los índices de emigración de médicos de dicho país. La importancia creciente del sector privado en la atención sanitaria en los países en desarrollo ha suscitado un nuevo interés entre los académicos respecto a las influencias de dicho sector sobre muchos aspectos de los sistemas sanitarios nacionales. El aumento de la emigración de médicos procedentes de países en desarrollo ha conducido a varios intentos de identificar, por un lado, los factores implicados en la emigración de médicos y, por otro lado, los efectos de la emigración de médicos sobre la atención primaria y la salud de la población de los países de donde parten los médicos. Tras investigar la información pertinente sobre las economías emergentes de Ghana, India y Perú, se halló una relación inversa entre el índice de médicos expatriados y cada uno de los siguientes factores: la proporción de médicos que prestan atención sanitaria dentro del sector sanitario privado, el porcentaje de los costes sanitarios financiados con fondos públicos y la cuantía de la financiación per cápita del sector sanitario privado. Por consiguiente, parece ser que la prestación de servicios sanitarios por parte del sector privado y la financiación pueden reducir la emigración de médicos. Resulta evidente la necesidad de realizar investigaciones similares en otros países de renta media y baja, así como estudios que esclarezcan si, a escala nacional, se pueden vincular las tendencias temporales de la contribución por parte del sector privado con las correspondientes tendencias de la emigración de médicos. Cómo la sanidad privada puede relacionarse con los problemas de acceso para los pobres y, por lo tanto, con la reducción de la equidad, merece asimismo mayor investigación. Los resultados podrían ser de interés para los responsables políticos que aspiren a mejorar los sistemas sanitarios a escala mundial.
ملخص
قد يؤثر إسهام القطاع الخاص في الرعاية الصحية في بلد منخفض أو متوسط الدخل في مستويات هجرة الأطباء من هذا البلد. وقد أدى تزايد أهمية القطاع الخاص في الرعاية الصحية في العالم النامي إلى اهتمام أكاديمي مؤخراً بتأثيرات هذا القطاع على العديد من جوانب النظم الصحية الوطنية. وأدى تزايد هجرة الأطباء من العالم النامي إلى عدة محاولات لتحديد العوامل التي تتسبب في هجرة الأطباء وتأثيرات هجرة الأطباء على الرعاية الأولية وصحة السكان في البلدان التي يغادرها الأطباء. وعندما تم تحري المعطيات ذات الصلة في الاقتصاديات الناشئة لغانا والهند وبيرو، بدا أن نسبة الأطباء الذين شاركوا في إيتاء خدمات الرعاية الصحية الخاصة والنسبة المئوية لتكاليف الرعاية الصحية الممولة بالمال العام وحجم تمويل الرعاية الصحية الخاصة لكل فرد ترتبط عكسياً بمستوى هجرة الأطباء. وبناءً على ذلك، يبدو أن إيتاء خدمات الرعاية الصحية الخاصة وتمويلها قد يؤديان إلى التقليل من هجرة الأطباء. وثمة حاجة واضحة إلى إجراء بحوث مشابهة في البلدان المنخفضة والمتوسطة الدخل الأخرى، وإجراء دراسات لمعرفة ما إذا كانت الاتجاهات المؤقتة في إسهام القطاع الخاص في الرعاية الصحية، على صعيد البلدان، ذات صلة بالاتجاهات المقابلة في هجرة الأطباء. وتستحق الطرق التي قد ترتبط من خلالها الرعاية الصحية الخاصة بمشكلات الوصول إلى الفقراء، ومن ثم الإنصاف المنخفض مزيداً من التحري. وينبغي أن تحظى النتائج باهتمام لدى صناع السياسة الذين يهدفون إلى تحسين النظم الصحية في جميع أنحاء العالم.
摘要
私人部门对中低收入国家卫生保健做出的贡献可能影响该国医生移民的水平。发展中国家私人部门对卫生保健重要性日益提高,使该部门对国家卫生系统诸多方面的影响引起新的学术兴趣。发展中国家医生移民的增长,促使人们在确定造成医生移民的因素以及医生移民对医生所离开国家的初级保健和人口健康的影响这两个方面都进行了一些尝试。对加纳、印度和秘鲁新兴经济体相关数据的调查显示,医生参与私人医疗保健服务的比例、公共资金在医疗成本中的比例以及私人资金承担的人均医疗金额均与医师移居国外呈负相关。因此,似乎私人医疗保健服务和资金可能会减少医生移民数量。很明显,需要在其他中低收入国家进行类似的研究,还需要其他一些研究,在国家层面上了解私人部门对卫生保健贡献的时间趋势是否可能与医生移民方面相应的趋势相关。私人卫生保健可能与穷人看病难问题以及因此造成的不公平之间存在联系,其关联方式也值得进一步调查。调查结果将会引起旨在改善全球卫生系统的决策制定者的关注。
Резюме
Вклад, вносимый частным сектором в здравоохранение в странах с низким или средним уровнями доходов, может повлиять на уровни эмиграции врачей из страны. Возрастающее значение частного сектора в здравоохранении в развивающихся странах вызвало новый научный интерес к влиянию, оказываемому данным сектором на многие аспекты систем общественного здравоохранения. Рост эмиграции врачей из развивающихся стран вызвал стремление определить как факторы, провоцирующие эмиграцию врачей, так и влияние эмиграции врачей на первичную медицинскую помощь и здоровье населения в странах, которые покидают врачи. После изучения соответствующих данных по развивающимся экономикам Ганы, Индии и Перу выяснилось, что доля врачей, задействованных в оказании частной медицинской помощи, процентное отношение затрат на здравоохранение, финансируемых из государственного бюджета, и объем частного финансирования здравоохранения на душу населения были обратно пропорциональны уровню экспатриации врачей. Следовательно, оказание частной медицинской помощи и частное финансирование, по-видимому, могут уменьшить эмиграцию врачей. Очевидно, что необходимо проведение аналогичных научных изысканий в остальных странах с низким и средним уровнями доходов, а также исследований, устанавливающих возможность связи, на уровне страны, временных тенденций вклада, вносимого в здравоохранение частным сектором, с соответствующими тенденциями эмиграции врачей. Связь частного здравоохранения с проблемами доступа к здравоохранению неимущих слоев населения и, следовательно, со снижением уровня социальной справедливости также заслуживает дальнейшего исследования. Результаты должны быть интересны ответственным лицам, стремящимся улучшить системы здравоохранения по всему миру.
Introduction
There has been considerable academic interest in the growth of the private sector in the delivery and financing of health care in developing countries. In a recent editorial, Forsberg et al. drew attention to the “major role in financing and provision” that the private sector plays in low- and middle-income countries, and went on to state that “private health sector research has moved beyond classifying and counting providers and users, to the assessment of mechanisms for harnessing the private sector and identifying conditions for their successful application”.1
In the developing world in particular, research on health care is often hampered by a lack of standard definitions. For example, only clinicians with medical degrees are categorized as physicians in some studies, but traditional healers are also considered physicians in other investigations.2,3 Despite such problems with definitions, a growing body of literature now links private health-care financing and delivery in low- and middle-income countries with quality of care, drug availability, patient access and equity, provider training and provider knowledge, and changes in public-sector health care delivery in the same settings.4–7 Various interventions may further improve private health care provision in low- and middle-income countries.8
The private sector is making a growing contribution to health care in much of the developing world. In an analysis of data from 26 African countries by the World Bank, nearly half of the sick children from the poorest income quintile were found to have made use of private providers.9 Most (nearly 87%) of India’s health care is now privately funded10 and out-of-pocket payments from patients have been found to represent 40–70% of the gross domestic product spent on medical care in 20 developing countries.11 Various factors, including the traditional counterbalance between supply and demand, heavily influence the growth of private health care in the developing world and whether physicians choose to practise in the private sector, the public sector or both sectors and to stay in their home country or to emigrate.12
Physicians in low- and middle-income countries often emigrate because of the poor incomes and inadequate resources available in their home countries and the better professional prospects and higher standards of living available to them abroad.13,14 There is considerable recruitment of such physicians by high-income countries.15 Of the physicians working in Australia in 1999, Canada in 2002, the United Kingdom of Great Britain and Northern Ireland in 2002 and the United States of America in 2004, 23–28% were immigrants, mostly from Asia, the Caribbean and sub-Saharan Africa; India alone accounted for nearly 60 000 of the physicians.16 The emigration of physicians from numerous low- and middle-income countries drains skilled personnel from already weak health systems and reduces the success of existing primary care and public health activities.17
In an attempt to determine if countries with relatively large private health care sectors have relatively low rates of physician emigration, the relevant data from three countries with emerging economies were collected together and analysed.
Case studies
The three study countries, Ghana, India and Peru, were selected to give a wide range of physician emigration rates and to represent three different World Health Organization (WHO) regions. The data analysed came from the Organisation for Economic Co-operation and Development (OECD),18 which records the numbers and nationalities of immigrant physicians in each OECD country, and from reviews of the relevant published and “grey” literature. The expatriation rates for physicians were taken from a table published by the OECD18 and are estimates for the year 2000. Each rate was calculated, as a percentage, by dividing the number of physicians who were trained in a study country but were practising in any OECD country in 2000 by the sum of that number and the number of physicians practising in the same study country in 2000, and then multiplying the result by 100. The literature reviews were conducted using the PubMed, Google and SciELO search engines and the search facilities available via the web sites of the World Bank and WHO. The PubMed search strategy involved keywords and MeSH terms related to private health care and physician migration, combined with developing world, Ghana, India or Peru. Similar strategies were followed with the other search engines.
All of the search results were reviewed for relevance and the citations in the relevant articles were examined for other articles that might hold useful data. The final analysis included only data from articles that had been published within the previous 20 years in a peer-reviewed journal or by the World Bank or WHO. For this analysis, only individuals with biomedical training were considered to be physicians.
Ghana
Physicians from Ghana appear more likely to migrate abroad than physicians from India or Peru. The physicians who remain in Ghana mostly work for the public sector, although most (64%) of their income comes from out-of-pocket contributions from patients. A Ghanaian is much more likely to have public health insurance than an Indian or Peruvian. Private health insurance remains relatively rare in Ghana, although it has become more common in the last few years.
Levels of physician emigration are relatively high in Ghana. Of the physicians who graduated from the University of Ghana between 1985 and 1994, 50% and 75% had emigrated within 4.5 and 9.5 years of their graduation, respectively.19 Although Ghana’s first private insurance scheme, the Nationwide Mutual Medical Insurance scheme, was launched in 1993, most physicians continued to be paid from the “public purse”. The private insurance scheme was soon struggling with fraudulent claims, inadequate premiums, a generally dissatisfied clientele and a claims backlog.20
In the 1990s, about 47% of the hospitals and 60% of the clinics in Ghana were government-managed. Private health-care facilities then, as today, were most commonly run by nongovernmental organizations on a no-profit basis or by faith organizations that charged patients small, nominal fees; for-profit delivery by the private sector remained rare.21 The quality of the health care delivered by the private sector varied greatly; although some urban facilities were well equipped and well managed, many private clinics in rural areas were run by “petty traders selling drugs, drug peddlers, quacks and injectionists”.22
The Ghanaians’ apparently small appetite for private insurance and private health care delivery led to the insolvency of the Nationwide Mutual Medical Insurance scheme in 1997.20 Physician emigration remained very common; between 1993 and 2001, 68% of Ghanaian medical graduates left Ghana.23
In the year 2000, 1469 physicians trained in Ghana were recorded as living in OECD countries. This represented an expatriation rate of 31.2%.18 In 2009, health care in Ghana was described as a mixture of private traditional systems and public, private for-profit and private not-for-profit non-traditional systems. Recent efforts have been made towards integrating the system based on traditional medicine with the private, not-for-profit, non-traditional system.24 Only 10% of the health-care providers working in Ghana in 2010 worked exclusively in the private sector.20 At this time, private insurance remained rare and was largely confined to unionized workers in the private sector, who had fought for such cover during their collective bargaining with their employers.20 Despite the predominance of the public sector in Ghanaian health-care delivery, 64% of the health-care financing in Ghana comes from the private sector and 80% of the private finances come from out-of-pocket contributions from patients.3 More than half of all Ghanaians are covered by public health insurance via the National Health Insurance scheme.20
India
India trains more physicians than almost any other country, provides the largest number of emigrant physicians, and has the largest private health-care system. About 11% of physicians practising in the United Kingdom and 5% of those practising in the United States of America were trained in India.14,25 India is the country from which the largest number of physicians of any given nationality living in OECD countries have emigrated.18 However, the number of physicians trained in India every year is so enormous that the 55 000 Indian physicians who live abroad make for an expatriation rate of only 8%.18
At the time of India’s independence, in 1947, only 8% of health care delivery was private. Today, however, 80–85% of the licensed physicians, 93% of the hospitals and 80% of the outpatient clinics in India operate, in whole or in part, within the for-profit private sector. Private physicians are remunerated on a fee-for-service basis. Out-of-pocket contributions from patients provide an estimated 87% of health-care finances.10 It has been estimated that only about 1% and 10–14% of the Indian population has public and private health insurance, respectively.26,27
Private physicians in India are categorized as rural medical providers, non-profit physicians or for-profit physicians. Rural medical providers are generally unqualified medical practitioners. Non-profit private physicians, who work for nongovernmental organizations or faith-based organizations, provide only 1.32% of the private consultations in India.10 Most private physicians in India work in the for-profit sector.10
The predominance of the private sector in health care in India is largely a consequence of the Indian government’s failure to keep pace with the growing health-care needs of the world’s second largest population. The government’s economic policies, the rapid influx of technology and the increasing number of Indians who have moderate (rather than poor) incomes have also encouraged expansion of the private sector.27 Although the growth of private-sector health care has generally increased access to health-care providers, there are concerns that private care is too expensive, poorly regulated and associated with inadequate training and a general lack of practice standards, particularly in the for-profit sector. The Indian government is making efforts to address these concerns by increasing public-insurance coverage28 and improving the regulation of the private sector.29
Why India has such a low rate of physician emigration, even though it has the largest absolute number of physicians migrating abroad, is unclear. It is possible that Indian physicians who have received poor training choose to remain in India, perhaps encouraged by work in the for-profit private sector that can provide reasonable incomes and little regulatory restriction. The recent growth in medical tourism to India, which has provided a fresh source of income for the for-profit sector, may well have improved physician retention. If the growing calls for increases in the public financing and delivery of health care in India30 are successful, levels of physician emigration from the country may increase.
Peru
Peruvian physicians only really began to emigrate following the civil unrest in the 1980s, but the trend continued into the 1990s in the midst of an economic recession. Over this period, health care was predominantly delivered by the public sector and public investments in health were seen as critical to national development.
In 1984, the public sector held 78% of the hospital beds and 93% of the primary health-care facilities in Peru. However, the cuts made in the government’s health budget at about this time drove an expansion of private health care delivery. Throughout the 1980s and 1990s, physicians who were publicly employed in Peru fought for permission to develop and maintain private practices to mitigate the consequences of the budget cuts on their incomes.31 Although concerns were raised about how such “dual-sector practices” would affect patient access and various other aspects of health care delivery, the number of Peruvian physicians who work for both the private and public sectors continues to grow. So far, no relevant official policy or regulation has been developed and the general consensus seems to be that physicians should be allowed to supplement low public wages in this way.32
The General Health Law of 1997 required the Peruvian government to promote conditions that should, in principle, guarantee adequate and universal health service coverage throughout Peru.33 The result was a relaxation of the public monopoly on the delivery of medical services. Once this law was passed, beneficiaries of the public insurance provider – Peru’s Social Security Institute, formerly called the Instituto Peruano de Seguridad Social (IPSS) and now called the Seguro Social de Salud (EsSalud) – could receive care from private companies, which would then bill the insurance provider. In another attempt to promote adequate coverage, the government created the Seguro Integral de Salud (SIS) in 2001 to cover indigent rural and periurban populations, especially the impoverished women and children in such populations who had no other access to social assistance.
Of the health care received by patients treated by physicians in Peru in 1998, 55.1% was provided through publicly financed institutions, 20.8% (delivered either publicly or privately) was financed by the Seguro Social de Salud, 10.9% was provided through public non-specialized health-care services (e.g. armed forces, police and welfare institutions) and only 18.9% was provided by private providers supported by out-of-pocket contributions from patients.34 By the time the 2003 Second Infrastructure and Human Resources Census was conducted, however, these percentages had changed to 39.1%, 18.1%, 7.1% and 32.4%, respectively.31 Thus, between 1998 and 2003 the amount of health care provided by private providers supported by out-of-pocket contributions nearly doubled, partly as a consequence of the large number of physicians (nearly 50% of all of those in Peru) who were working in both the public and private sectors by 2003.31
Since the passage of the General Health Law in 1997, private insurance coverage and out-of-pocket payments have become significant financing mechanisms for health care in Peru. Today, 42% of Peruvians receive some form of public insurance: 20%, mostly urban workers, are covered by the Seguro Social de Salud, 18% are covered by the Seguro Integral de Salud, and 4% are covered directly by the government because they are politicians, members of the armed services or educators.35 Since only 2% of Peruvians have private health insurance, more than half (56%) of all Peruvians have to pay out of pocket for their health care.36 The uninsured Peruvians are mostly the working poor, who are ineligible for support from the Seguro Social de Salud because they have work and who earn too much to receive support from the Seguro Integral de Salud and too little to pay for private insurance.37 The decision to allow some richer Peruvians who are covered by public health insurance to contribute towards their own health care at expensive private facilities has been seen as a waste of the insurance, especially by the uninsured working poor.32 By 2008, 15% of Peruvians were receiving primary health care through private providers located in urban areas.38,39
While private-sector involvement in health-care financing and delivery has being growing in Peru, rates of physician emigration and expatriation have been declining. Only about 24% of the physicians who graduated in Peru between 1995 and 2005 chose to stay in Peru.40 However, in more recent studies in two Peruvian medical institutions, only 30%41 or 51%42 of recent graduates were found to have left Peru, to pursue medical residencies abroad.
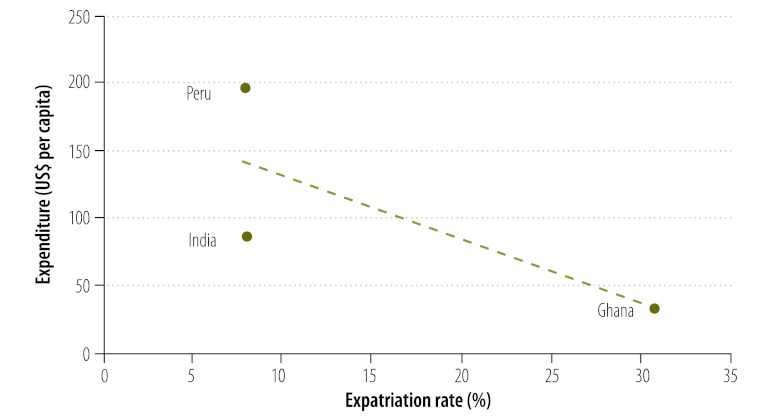
Of the three study countries, Peru has the lowest level of physician expatriation and the highest per-capita expenditure on private health care (Fig. 1).
Fig. 1.
Relationship between expenditure on private health care in Ghana, India and Peru and physician expatriation from the same countries
US$, United States dollar.
Note: The expenditures shown are the per capita values in United States dollars for 2008. The expatriation rates shown are estimates for 2000.
Overview
The main results from the data review are summarized in Table 1. In each of the three study countries, private expenditure on health per capita was calculated from data collected by WHO43 by multiplying the proportion of total health expenditure spent on private health care by the total health expenditure per capita. When the per capita private expenditures on health in Ghana, India and Peru were plotted against the most recent estimates of the rates of physician emigration from the three countries, the two variables appeared to be inversely related (Fig. 1).
Table 1. The most recent estimates of physician expatriation and other features of the health systems of Ghana, India and Peru, 2000–2010.
| Variable | Ghana | India | Peru |
|---|---|---|---|
| No. of physicians living abroad | 1469 | 55 794 | 2807 |
| Physician expatriation rate (%) | 31.2 | 8.0 | 7.9 |
| Out-of-pocket contributions (% of health expenditure) | 65.9 | 87.0 | 75.3 |
| Health insurance coverage (% of population) | |||
| public | 56 | 11–15a | 42 |
| private | 18 | 1 | 2 |
| Physicians working in private sector (%) | 10.0 | 51.9 | 50.0 |
| Main source of physician income from private sector | Fees for services | Fees for services | Fees for services |
| Universal health-care coverage guaranteed by government? | No | No | Yesb |
| Annual expenditure on private health care (United States dollars per capita) | 33 | 86 | 197 |
a The range shown indicates the variation in recent estimates.
b In principle.
Discussion
For the health systems of Ghana, India and Peru, data on the private sector were rarer and harder to obtain than the corresponding information on the public sector; there is clearly a need for better monitoring and evaluation of private health-care financing and delivery in the three countries. Despite this limitation, it is clear that, over the last few decades, Ghana, India and Peru have seen growth in private-sector financing and delivery of health care, in parallel with economic growth, increasing population demand and changing policy environments.
Of the three countries investigated, Ghana had the lowest per capita expenditure on private health care and the highest level of physician expatriation. Peru, on the other hand, had the highest per capita expenditure on private health care and the lowest level of physician expatriation.
Our primary hypothesis was that physicians working in systems structured towards private delivery and financing may be less inclined to migrate than other physicians. This may well be the case if physicians can offer their services at private rates that exceed the corresponding public-sector remuneration. Peru’s growth in dual-sector practices has not only led to growth in the private-sector delivery of health care, but has also, according to the data available on physician expatriation, improved physician retention. Although the data discussed here indicate a negative correlation between per-capita expenditure on health care and physician emigration, they give only three points on a graph (Fig. 1). This relationship needs to be explored much further, with more extensive models that consider many more countries while controlling for factors (other than the level of private-sector involvement) that may persuade physicians to emigrate or to remain in the country where they were trained.
If it can be proven that growth in private sector participation does improve physician retention, then we need to know if the benefits of retaining physicians in the private sector outweigh the problems of patient access associated with the private sector, particularly in the developing world. Many emerging economies have populations that not only have little health insurance but are also frequently too poor to make the out-of-pocket contributions demanded by the private health-care sector.
In future research, all of the “push” and “pull” factors related to private sector and public sector health care delivery and financing that could drive physician emigration need to be investigated. In India, for example, the poor training of some physicians may prevent their employment in other countries.
Conclusion
Rapid economic development, limitations on public spending and health service regulation continue to drive the growth of private health care in the developing world. As the contribution made to health-care delivery and financing by the private sector increases, physicians in the developing world may become less inclined to emigrate. Much more research on this topic needs to be conducted. In the present analysis it proved impossible to distinguish physicians who worked in both the public and private sectors from those who worked only in the private sector. Better data need to be collected from many low- and middle-income countries, particularly on the private sector. The possibly adverse effects of private-sector growth on attempts to achieve universal health-care coverage also need to be investigated. Careful consideration should therefore be given to any policies designed to regulate private sector growth or physician emigration.
Acknowledgements
We gratefully acknowledge the comments and feedback provided by WHO’s Human Resources for Health team.
Competing interests:
None declared.
References
- 1.Forsberg BC, Montagu D, Sundewall J. Moving towards in-depth knowledge on the private health sector in low- and middle-income countries. Health Policy Plan. 2011;26(Suppl 1):i1–3. doi: 10.1093/heapol/czr050. [DOI] [PubMed] [Google Scholar]
- 2.Hanson K, Berman P. Private health care provision in developing countries: a preliminary analysis of levels and composition. Health Policy Plan. 1998;13:195–211. doi: 10.1093/heapol/13.3.195. [DOI] [PubMed] [Google Scholar]
- 3.Private health sector assessment in Ghana Washington: World Bank; 2011. Available from: http://issuu.com/world.bank.publications/docs/9780821386248 [accessed 16 January 2013].
- 4.Cameron A, Roubos I, Ewen M, Mantel-Teeuwisse AK, Leufkens HG, Laing RO. Differences in the availability of medicines for chronic and acute conditions in the public and private sectors of developing countries. Bull World Health Organ. 2011;89:412–21. doi: 10.2471/BLT.10.084327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mills A, Brugha R, Hanson K, McPake B. What can be done about the private health sector in low-income countries? Bull World Health Organ. 2002;80:325–30. [PMC free article] [PubMed] [Google Scholar]
- 6.Prinja S, Bahuguna P, Pinto AD, Sharma A, Bharaj G, Kumar V, et al. The cost of universal health care in India: a model based estimate. PLoS One. 2012;7:e30362. doi: 10.1371/journal.pone.0030362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sengupta A, Nundy S. The private health sector in India. BMJ. 2005;331:1157–8. doi: 10.1136/bmj.331.7526.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah NM, Brieger WR, Peters DH. Can interventions improve health services from informal private providers in low and middle-income countries? A comprehensive review of the literature. Health Policy Plan. 2011;26:275–87. doi: 10.1093/heapol/czq074. [DOI] [PubMed] [Google Scholar]
- 9.Marek T, O’Farrell C, Yamamoto C, Zable I. Trends and opportunities in public–private partnerships to improve health service delivery in Africa Washington: World Bank; 2005. [Google Scholar]
- 10.Radwan I. India – private health services for the poor Washington: World Bank; 2005. [Google Scholar]
- 11.Pauly MV, Zweifel P, Scheffler RM, Preker AS, Bassett M. Private health insurance in developing countries. Health Aff (Millwood) 2006;25:369–79. doi: 10.1377/hlthaff.25.2.369. [DOI] [PubMed] [Google Scholar]
- 12.Berman P, Nwuke K, Rannan-Eliya R, Mwanza A. Zambia: non-governmental health care provision. Boston: Harvard School of Public Health; 1995. [Google Scholar]
- 13.Stilwell B, Diallo K, Zurn P, Vujicic M, Adams O, Dal Poz M. Migration of health-care workers from developing countries: strategic approaches to its management. Bull World Health Organ. 2004;82:595–600. [PMC free article] [PubMed] [Google Scholar]
- 14.Kaushik M, Jaiswal A, Shah N, Mahal A. High-end physician migration from India. Bull World Health Organ. 2008;86:40–5. doi: 10.2471/BLT.07.041681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nullis-Kapp C. Efforts under way to stem “brain drain” of doctors and nurses. Bull World Health Organ. 2005;83:84–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Mullan F. The metrics of the physician brain drain. N Engl J Med. 2005;353:1810–8. doi: 10.1056/NEJMsa050004. [DOI] [PubMed] [Google Scholar]
- 17.Nullis-Kapp C. Health worker shortage could derail development goals. Bull World Health Organ. 2005;83:5–6. [PMC free article] [PubMed] [Google Scholar]
- 18.International migration outlook Paris: Organisation for Economic Co-operation and Development; 2007. [Google Scholar]
- 19.Dovlo D, Nyonator F. Migration by graduates of the University of Ghana Medical School: a preliminary rapid appraisal. Hum Resour Dev J. 1999;3:1–16. doi: 10.1056/NEJMsa050004. [DOI] [PubMed] [Google Scholar]
- 20.Atim C, Grey S, Apoya P, Anie SJ, Aikins M. A survey of health financing schemes in Ghana Bethesda: Partners for Health Reformplus; 2001. [Google Scholar]
- 21.Canagarajah S, Ye X. Public health education and spending in Ghana in 1992–98. Washington: World Bank; 2001. [Google Scholar]
- 22.Agyepong IA. Reforming health service delivery at district level in Ghana: the perspective of a district medical officer. Health Policy Plan. 1999;14:59–69. doi: 10.1093/heapol/14.1.59. [DOI] [PubMed] [Google Scholar]
- 23.Kirigia JM, Gbary AR, Muthuri LK, Nyoni J, Seddoh A. The cost of health professionals’ brain drain in Kenya. BMC Health Serv Res. 2006;6:89. doi: 10.1186/1472-6963-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salisu A, Prinz V. Health care in Ghana: March 2009. Vienna: Austrian Centre for Country of Origin and Asylum Research and Documentation; 2009.
- 25.Knox R. India’s doctors returning home Washington: NPR; 2007. Available from: http://www.npr.org/templates/story/story.php?storyId=16774871 [accessed 14 December 2012].
- 26.Pate RC, Purandare J, Oosterom W, Hall TW, Sengupta R, Schulman C. Health care in India. London: PricewaterhouseCoopers; 2007. [Google Scholar]
- 27.Bhat R. Characteristics of private medical practice in India: a provider perspective. Health Policy Plan. 1999;14:26–37. doi: 10.1093/heapol/14.1.26. [DOI] [PubMed] [Google Scholar]
- 28.Reddy KS, Patel V, Jha P, Paul VK, Kumar AK, Dandona L, Lancet India Group for Universal Healthcare Towards achievement of universal health care in India by 2020: a call to action. Lancet. 2011;377:760–8. doi: 10.1016/S0140-6736(10)61960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhat R. Regulating the private health care sector: the case of the Indian Consumer Protection Act. Health Policy Plan. 1996;11:265–79. doi: 10.1093/heapol/11.3.265. [DOI] [PubMed] [Google Scholar]
- 30.Prinja S, Bahuguna P, Pinto AD, Sharma A, Bharaj G, Kumar V, et al. The cost of universal health care in India: a model based estimate. PLoS One. 2012;7:e30362. doi: 10.1371/journal.pone.0030362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nigenda G, Machado MH, Castrillón MC, Arroyo J. The impact of health care reform on the professional regulation of physicians in Latin America. In: Söderlund N, Mendoza-Arana P, Goudge J, editors. The new public/private mix in health: exploring the changing landscape Geneva: Alliance for Health Policy and Systems Research; 2003. pp. 13–34. [Google Scholar]
- 32.Jumpa M, Jan S, Mills A. Dual practice of public sector health care providers in Peru London: London School of Hygiene and Tropical Medicine; 2003. [Google Scholar]
- 33.Zschock DK, editor. Health care in Peru: resources and policy Boulder: Westview Press; 1988. [Google Scholar]
- 34.Demanda de atención en servicios de salud. Lima: Instituto Nacional de Estadística e Informática; 1998. Spanish. Available from: http://www.inei.gob.pe/biblioineipub/bancopub/Est/Lib0035/indice.htm[accessed 16 January 2013].
- 35.Alcalde-Rabanal JE, Lazo-González O, Nigenda G. Sistema de salud de Perú. Salud Publica Mex. 2011;53(Suppl 2):s243–54. [PubMed] [Google Scholar]
- 36.Bardalez del Aguila C. La salud en El Perú: Lima: Peruvian Health Observatory; 2002. Spanish. [Google Scholar]
- 37.Maguiña C, Galán-Rodas E.Situación de la salud en el Perú: la agenda pendiente. Rev Peru Med Exp Salud Publica 201128569–70.Spanish 10.1590/S1726-46342011000300029 [DOI] [PubMed] [Google Scholar]
- 38.Peru: country health profile. Washington: Pan American Health Organization; 2011. Available from: http://www.paho.org/english/sha/prflper.htm [accessed 16 January 2013].
- 39.Health of Nations [Internet]. Peru. Fairfield: General Electric Company; 2011. Available from: http://www.healthofnations.com/countries/profile/peru [accessed 16 January 2013].
- 40.Fraser B. Human resources for health in the Americas. Lancet. 2007;369:179–80. doi: 10.1016/S0140-6736(07)60091-9. [DOI] [PubMed] [Google Scholar]
- 41.Leon JR, Luis R, Ojeda H, Wendel CS.Comparación de la calidad de vida entre médicos graduados en el Perú que migraron al extranjero y los que permanecieron en el país. Rev Med Hered 201021187–96.Spanish [Google Scholar]
- 42.Mayta-Tristán P, Mejia CR, Riega-Lopez P, Rojas-Mezarina L, Posso M, Mezones-Holguín E.Proyección de trabajo en el interior del país y factores asociados en médicos recién colegiados de Lima, Perú 2010. Rev Peru Med Exp Salud Publica 201128186–93.Spanish 10.1590/S1726-46342011000200004 [DOI] [PubMed] [Google Scholar]
- 43.World health statistics 2012 Geneva: World Health Organization; 2012. [Google Scholar]