Abstract
Background:
The complicated concept of quality of life (QOL) has been considered as an important criterion for health outcomes in chronic diseases, such as heart disease, in recent years. The aim of this study was to evaluate the QOL of patients with angina pectoris after treatment with enhanced external counterpulsation (EECP).
Materials and Methods:
This quasi-experimental study was conducted on 64 patients with angina pectoris undergoing EECP who came to Shahid Chamran and Sina Hospitals in Isfahan. Sampling was performed by the convenient method. Data were collected using a questionnaire containing socio-demographic and clinical data. A standard questionnaire called 36-item Short-Form Health Survey was also used. Questionnaires were completed through interviews and phone calls in three stages (before, immediately and three months after the treatment). The results were analyzed using descriptive statistics (frequency, mean, and standard deviation) and analytical statistics (paired t-test and repeated measures test) in SPSS11.5.
Findings:
The obtained results demonstrated that the majority of patients were men (59.4%) and aged 56-71 years. In addition, 57.8% had hypertension and 56.3% had hyperlipidemia. A history of myocardial infarction was found in 70.3% of the subjects and the familial history of coronary artery disease was detected in73.4%. Although QOL evaluations showed improvements in all subscales immediately and three months after the treatment, the changes were not statistically significant in case of general health, role limitations due to physical problems and role limitations due to mental problems
Conclusions:
Similar to previous research, this study showed QOL to improve in patients who undergo EECP. This improvement will remain stable three months after the treatment in all subscales. Therefore, EECP is an efficient noninvasive method in treating patients with angina pectoris and in developing their QOL.
Keywords: Angina pectoris, health-related quality of life, enhanced external counterpulsation
INTRODUCTION
Ischemic heart disease is considered as one of the most common, serious and life threatening diseases. The prevalence of the disease is increasing all over the world and it is predicted to turn into the first cause of death by 2020.[1]
The treatment goals in this disease include explanation for and ensuring the patient, assessing and treating the risk factors, balancing the patient's activities, pharmacologic treatment, vascular repairing and finally enhanced external counterpulsation (EECP).[1]
Based on the viewpoints of several investigators, EECP is used as a treating method in patients suffering from stable angina, those having symptoms despite undergoing the most appropriate pharmacologic treatments, or those who are not able to endure vascular repairing treatment.[2] This method has healing and clinical effects, escalates the perfusion in coronary arteries, opens or forms collaterals (small branches of blood vessels) and increases the level of NO2 in blood. It therefore enables patients to start their active life again with decreased angina severity.[3] In Iran, Nasr et al. reported significantly longer exercise test time in patients with refractory angina pectoris after EECP.[4] Moreover, several studies all over the world showed that patients with angina experienced desirable effects of EECP on their quality of life for long periods after the treatment.[5–7]
On the other hand, in the last the two decades, the tendency to assess and improve quality of life in chronic patients have increased substantially. Quality of life studies can provide comprehensive and precise methods for increasing data related to diseases and treatment effects.[8] Moreover, the usage of quality of life surveys in clinical activities can help improve the clinical performance by suggesting treatment modifications, life prolonging factors and communicational requirements.[9]
Knowledge about quality of life and factors affecting it will help nurses, as main members of therapeutic staff, to lead the care process toward quality of life improvement. As a result, existing individual problems and needs would be recognized by assessing quality of life.
According to the previously mentioned facts, increased incidence of heart diseases and the important effects they have on all aspects of patients’ lives, studying EECP is vital. In addition, it is noteworthy that EECP, as a safe, low-cost, low-stress and noninvasive treatment method, has not yet got an appropriate attention in the treatment of patients with angina pectoris in Iran. Moreover, a review on the literatures demonstrates that there is not enough research investigating different aspects and benefits of this method in Iran. Therefore, we decided to carry out this research to determine the effects of EECP on patients’ quality of life. We also aimed to evaluate the effects of EECP on physical and mental components of quality of life in patients with angina.
MATERIALS AND METHODS
This quasi experimental (clinical trial) study was conducted in Shahid Chamran and Sina Hospitals which are the only hospitals having EECP device in Isfahan province. The target population was all patients with angina. Based on convenient sampling method, all patients who referred to the two hospitals to be treated with EECP and participated in all treatment sessions (35 sessions) were selected. According to clinical exams and paraclinical tests, Patients had been selected for EECP by a physician. After coming to the medical center, a medical document, including clinical and demographic data, was prepared. Due to insufficient number of ECCP instruments in the province and the large number of required treatment sessions, each patient needs to be treated for seven weeks. Therefore, considering the statistical formula, similar studies and advices from statistics professionals, the sample size was estimated as equal to 64 persons. Sampling was performed from November 2007 to May 2009.
EECP is a mechanical, outpatient and noninvasive procedure in which pneumatic cuffs, similar to those in blood pressure instrument, are tied on both legs of the patient. During the treatment procedure the patient should lie on a bed in the treatment room. Three electrodes are attached to the patient's chest skin and connected to the electrocardiogram device. This device shows the heart rhythm of a patient during the treatment period. Moreover, blood pressures of patients are controlled during this period. Cuffs are connected to an air resource to be inflated and deflated according to the electrocardiograph. Therefore, they are inflated at the beginning of each diastole and deflated as a systole starts. The inflation starts from the cuffs on the calves, and continues to thighs and finally buttocks. When the cuffs are inflated, blood is pumped from the ends toward the heart. The number of EECP treatment sessions is variable since no specific instruction exists. One widely used regimen in the United States is one session a day, five days a week, for seven weeks resulting in a total of 35 one-hour sessions.[10]
According to the physician's opinion, patients were selected for EECP and thus entered in this study if they could not undergo other methods, such as coronary artery bypass graft or percutaneous coronary intervention (PCI), or if such methods did not significantly affect their angina pain. In addition, patients with clinical signs of coronary artery disease (CAD), myocardial infarction or ischemia, or congestive heart failure were also included.
Moreover, patients with any severe valvular heart disease, atrial fibrillation, overt congestive heart failure, uncontrolled hypertension (blood pressure > 180/100 while on medications), phlebitis, deep vein thrombosis, bleeding and coagulation problems were not good candidates for EECP and therefore were excluded from the present study. Likewise, pregnant or potentially pregnant women were not included. In addition, patients who did not complete the EECP treatment course or died during the treatment were eliminated from the investigation list.
A two-part questionnaire was used to collect data. In the first part, patients’ demographic and clinical data including age, sex, weight, height, employment status, the years of enduring coronary artery disease, occupied treatments, used drugs, blood pressure status, blood lipid profile, history of diabetes mellitus, familial history of coronary artery disease, smoking, history of myocardial infarction and left ventricular ejection fraction were recorded. In the second part, the standard 36-item Short Form (SF-36) quality of life questionnaire was utilized to assess quality of life. After obtaining permissions from the patients, the questionnaires were completed before and immediately after the treatment by interviews. Moreover, three months after completion of the treatment, the questionnaires were completed once more by 20-30 minute phone calls. Finally, the data from the last phase were compared with the results before and immediately after the treatment.
SF-36 is a general standard questionnaire with high validity and reliability. Although it was first used in Sweden, the translated versions are now being utilized in several countries.[11,12] The validity of the Farsi version has been determined by Motamed et al.[13] on employees of Shiraz University, Montazeri et al.[14] on healthy population aging more than 15 years in Tehran, and Mohammadpour et al.[15] on the healthy population aging more than 40 in Mazandaran province. In these studies, the investigators reported the Cronbach's alpha to range from 0.79 to 0.90.
The questionnaire consists of the 36 questions measuring eight health-related concepts. Six questions are related to general health, ten to physical functioning, four to role limitations due to physical problems, two to bodily pain, four to vitality, five to mental health, three to role limitations due to mental problems and two to social functioning. All subscales are summarized in physical and mental scales. For scoring the questionnaire, raw scores of quality of life in each scale (physical or mental) are calculated separately (range from 0 to 100) by adding the scores of the questions in that scale and dividing the result to the number the questions. High scores demonstrate better quality of life.[16]
After data were collected and both scales of quality of life were scored, data analysis was carried out using descriptive and analytic statistics in SPSS11.5. In descriptive statistics, parameters such as frequency, mean, and standard deviation were used. In analytic statistics, paired t-test and repeated measure tests were utilized.
FINDINGS
The findings of this study declared that the majority of subjects (48.4%) aged 56-71 years (mean: 65 ± 10.54) and were men (59.4%). Most subjects (73.4%) have had coronary artery disease for 0-10 years. In addition, the majority of patients had a history of hypertension (57.8%) and hyperlipidemia (56.3%). The history of myocardial infarction and familial history of coronary artery disease were found among 70.3% and 73.4% of the participants, respectively. Moreover, 85.9% of the patients were not smoking at the time of treatment.
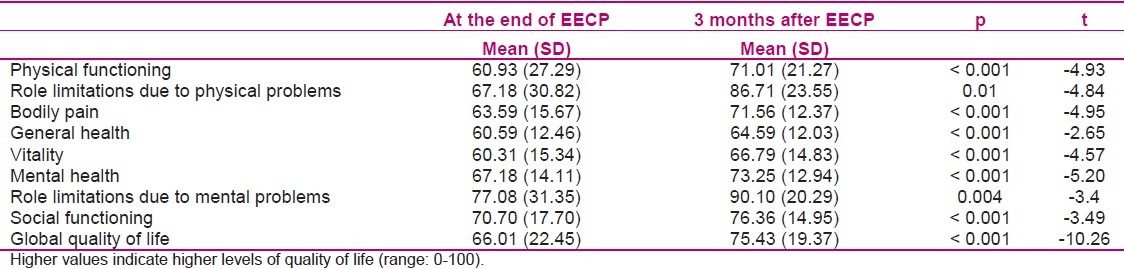
Tables 1,2 and 3 summarize the findings related to the comparison of quality of life in the three above-mentioned stages. Based on Table 1, comparison between mean scores of the subscales before and immediately after EECP by paired t-test revealed significant differences (P < 0.05). The scores 3 months after EECP significantly increased compared to before the treatment (Table 2). In addition, paired t-test showed significant differences in all subscales except functional limitations due to physical and mental problems and general health (P < 0.05). Likewise, the comparison between the scores immediately and three months after EECP indicated significant differences (Table 3).
Table 1.
Global quality of life scores before and at the end of EECP as measured by SF-36
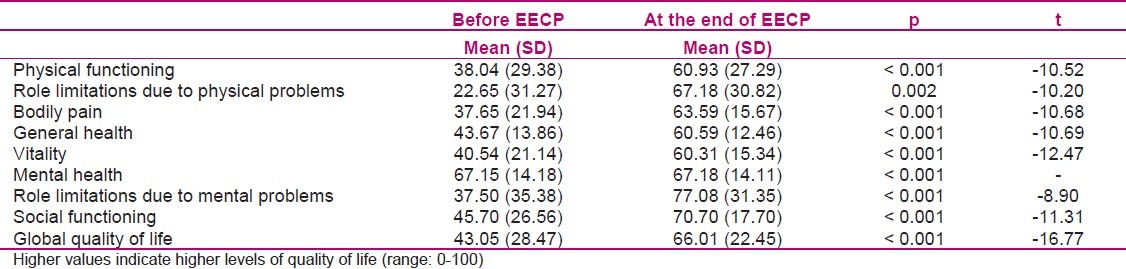
Table 2.
Global quality of life scores before and at 3 months after EECP as measured by SF-36
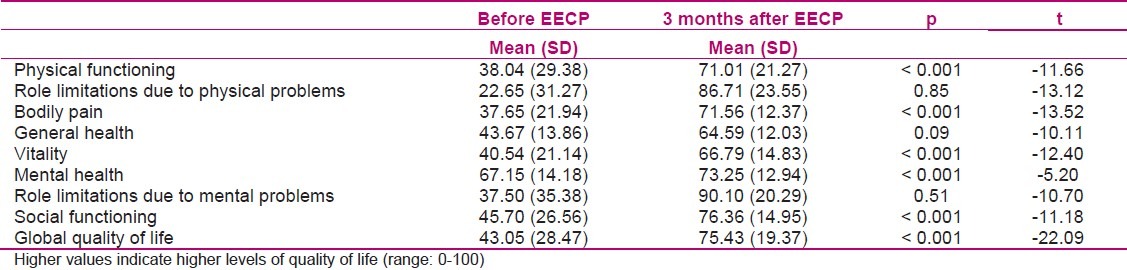
Table 3.
Global quality of life scores immediately and 3 months after EECP as measured by SF-36
DISCUSSION
The findings of this study showed significant improvements in quality of life among patients in all eight subscales, including physical function, role limitations due to physical problems, bodily pain, general health, vitality, mental health, role limitations due to mental problems and social function, following treatment with EECP. The improvements remained up to three months after the treatment.
Investigating subscales related to the physical component consisting physical functioning, role limitations due to physical problems, bodily pain, and general health indicates positive effects of EECP on patients’ physical status. As previous studies demonstrated,[5–7] the improvements caused by EECP will result in physical health promotion, bodily pain reduction, and eventually physical functioning development. Therefore, patients would be able to do their daily activities. Similarly, Shea et al. showed EECP to reduce angina pains, increase exercise time, improve coronary perfusion, and finally enhance physical functioning. They suggested EECP as a useful and safe method in patients with chronic and stable angina.[5] Likewise, Smith et al. reported EECP to increase exercise duration and improve patients’ functioning and quality of life without affecting the peak oxygen consumption.[6] Manchanda et al. also indicated that EECP enhanced activity endurance and left ventricular function which in turn led to improved quality of life.[7] Arora et al. used SF-36 and cardiac version of the Quality of Life Index immediately and twelve months after EECP and reported a significant improvement in doing ordinary activities, work ability, bodily pain and general health. They also suggested hemodynamic effects of EECP may stimulate intra-myocardial vessel growth and/or modify coronary perfusion similar to what is seen during vigorous exercise. These effects could lead to an improvement in physical health and quality of life.[17] Moreover, Nichols et al. showed EECP to improve quality of life in patients with angina and enable them to do their previous activities.[18] Michaels et al. surveyed the two-year outcomes of EECP in patients with stable angina pectoris. They evaluated quality of life in patients immediately and two years after treatment by five-point scales. They observed a significant improvement in general health and quality of life which remained stable in the two-year follow-up period among the majority of patients.[19] Similarly, Soran et al. evaluated two-year outcomes of EECP in patients with angina pectoris using five-point scales of quality of life six months, one year and two years after treatment. Like Michaels et al., they reported improvements in general health status and quality of life after EECP. They observed that EECP reduced the number of angina episodes and improved myocardial perfusion. They therefore suggested such effects to possibly improve physical functioning and quality of life which can last for two years.[20]
Assessment of mental subscales such as vitality, mental health, role limitations due to mental problems and social functioning in this study revealed higher levels of vitality, enjoyment and social functioning after EECP which could have been caused by physical health promotion. However, more accurate investigations would need further evaluations of mental health status by more specific questionnaires and comparing their results with those gathered by general SF-36 quality of life questionnaire.
Springer et al. used specific questionnaires such as Spielberger State and Trait Anxiety Inventory (STAI), Beck Depression Inventory, the Symptom Check-List 90-Revised (SCL-90-R), and General Health Quality Index (GHQ) to survey psychosocial effects of EECP in angina patients. They reported improvements in mental subscales of quality of life such as overall well-being, ability to work and energy level in 85% of patients. They also found EECP to have a significant impact on decreasing levels of depression as a result of myocardial perfusion improvement due to EECP.[21] Furthermore, Arora et al. observed that EECP raised the energy level and the ability to engage in social activities with family and friends.[17] Linnemeier et al. studied the one-year outcomes of EECP in the treatment of angina in diabetic patients. They investigated quality of life by a five-point Likert scale six and twelve months after EECP. They observed improvements in patients’ satisfaction of life.[22]
In this study, quality of life in patients was investigated in two stages, i.e. immediately and three months after EECP sessions. The results were then compared with values calculated before EECP. Most previous studies evaluated long-term effects of EECP (for instance in two-year follow up periods) and confirmed its efficiency. However, considering the limited number of EECP instruments in Isfahan and the large number of treatment sessions for each patient leading to longer treatment courses in this study, there was no possibility to investigate more subjects for longer periods of time after treatment.
CONCLUSION
According to the findings of this study, EECP can improve quality of life in patients with angina pectoris. Therefore, this treatment method is suggested as a noninvasive method in reducing problems due to angina pectoris. However, it is essential to compare the effects of this method and other invasive and noninvasive treatment methods by general and specific quality of life questionnaires in order to determine whether such method has any kind of priority. Moreover, based on our results, nurses can familiarize patients with positive effects of the method on physical and mental components of quality of life at the time of reception and motivate them to complete treatment sessions to attain the positive effects
ACKNOWLEDGMENT
The authors would like to express their gratitude to Islamic Azad University, Khorasgan (Isfahan) Branch for supporting this project. We also would like to thank all staff and patients in EECP ward in Shahid Chamran and Sina Hospitals who made this study possible.
Footnotes
Source of Support: Khorasgan (Isfahan) Branch, Islamic Azad University
Conflict of Interest: None declared
REFERENCES
- 1.Antman EM, Selwyn AP, Braunwald E, Loscalzo J. In: Harrison,s principles of internal medicine, cardiovascular diseases. 1st ed. Saadat N, Rasooli MR, editors. Tehran: Andishe-rafie publication company; 2008. [Google Scholar]
- 2.Bonetti PO, Barsness GW, Keelan PC, Schnell TI, Pumper GM, Kuvin JT, et al. Enhanced external counterpulsation improves endothelial function in patients with symptomatic coronary artery disease. J Am Coll Cardiol. 2003;41(10):1761–8. doi: 10.1016/s0735-1097(03)00329-2. [DOI] [PubMed] [Google Scholar]
- 3.Mielniczuk L, da Silva LB, Haddad H. Enhanced external counterpulsation in ischemic heart disease and congestive heart failure. CMAJ. 2004;170(8):1223–4. doi: 10.1503/cmaj.1031171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nasr A, Hoseinabadi MH. Effect of EECP on exercise test time in patients with refractory angina pectoris in chamran hospital. Journal of Isfahan Medical School. 2005;23(76):30–5. [Google Scholar]
- 5.Shea ML, Conti CR, Arora RR. An update on enhanced external counterpulsation. Clin Cardiol. 2005;28(3):115–8. doi: 10.1002/clc.4960280304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbottsmith CW, Chung ES, Varricchione T, De Lame PA, Silver MA, Francis GS, et al. Enhanced external counterpulsation improves exercise duration and peak oxygen consumption in older patients with heart failure: a subgroup analysis of the PEECH trial. Congest Heart Fail. 2006;12(6):307–11. doi: 10.1111/j.1527-5299.2006.05904.x. [DOI] [PubMed] [Google Scholar]
- 7.Manchanda A, Soran O. Enhanced external counterpulsation and future directions: step beyond medical management for patients with angina and heart failure. J Am Coll Cardiol. 2007;50(16):1523–31. doi: 10.1016/j.jacc.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 8.Collins E, Langbein WE, Dilan-Koetje J, Bammert C, Hanson K, Reda D, et al. Effects of exercise training on aerobic capacity and quality of life in individuals with heart failure. Heart Lung. 2004;33(3):154–61. doi: 10.1016/j.hrtlng.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 9.Narimani K. Comparative study of quality of life before and 1 month after coronary artery bypass grafting. Proceedings of the 1st Iranian congress on nursing care in Ischemic heart diseases; 2005 Jan 6-8; Tehran, Iran; 2005. 2009;29 [Google Scholar]
- 10.Wikipedia. Enhanced external counter pulsation [Online] 2008. Available from: URL: http://en.wikipedia.org/wiki/Enhanced_external_counterpulsation/
- 11.Benito-Leon J, Morales JM, Rivera-Navarro J. Health-related quality of life and its relationship to cognitive and emotional functioning in multiple sclerosis patients. Eur J Neurol. 2002;9(5):497–502. doi: 10.1046/j.1468-1331.2002.00450.x. [DOI] [PubMed] [Google Scholar]
- 12.Nicholl CR, Lincoln NB, Francis VM, Stephan TF. Assessing quality of life in people with multiple sclerosis. Disabil Rehabil. 2001;23(14):597–603. doi: 10.1080/09638280110043933. [DOI] [PubMed] [Google Scholar]
- 13.Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The short Form Health Survey (SF-36): Translation and Validation Study of the Iranian Version. Quality of life Research. 2005;14(3):875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 14.Motamed N, Ayatollahi AR, Zare N, Sadeghi-Hassanabadi A. Validity and reliability of the Persian translation of the SF-36 version 2 questionnaire. East Mediterr Health J. 2005;11(3):349–57. [PubMed] [Google Scholar]
- 15.Mohammad Pour RA, Akbari KH, Mohammad Pour F. Is Persian version of Health-related quality of life questionnaire valid and reliable? Proceedings of the 4th Iranian congress on epidemiology 2007 May 26-28; Urmia, Iran. 2007:41–2. [Google Scholar]
- 16.Ware JE, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P, et al. The factor structure of the SF-36 Health Survey in 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1159–65. doi: 10.1016/s0895-4356(98)00107-3. [DOI] [PubMed] [Google Scholar]
- 17.Arora RR, Chou TM, Jain D, Fleishman B, Crawford L, McKiernan T, et al. Effects of enhanced external counterpulsation on Health-Related Quality of Life continue 12 months after treatment: a substudy of the Multicenter Study of Enhanced External Counterpulsation. J Investig Med. 2002;50(1):25–32. doi: 10.2310/6650.2002.33514. [DOI] [PubMed] [Google Scholar]
- 18.Nichols WW, Estrada JC, Braith RW, Owens K, Conti CR. Enhanced external counterpulsation treatment improves arterial wall properties and wave reflection characteristics in patients with refractory angina. J Am Coll Cardiol. 2006;48(6):1208–14. doi: 10.1016/j.jacc.2006.04.094. [DOI] [PubMed] [Google Scholar]
- 19.Michaels AD, Linnemeier G, Soran O, Kelsey SF, Kennard ED. Two-year outcomes after enhanced external counterpulsation for stable angina pectoris (from the International EECP Patient Registry [IEPR]) Am J Cardiol. 2004;93(4):461–4. doi: 10.1016/j.amjcard.2003.10.044. [DOI] [PubMed] [Google Scholar]
- 20.Soran O, Kennard ED, Kfoury AG, Kelsey SF. Two-year clinical outcomes after enhanced external counterpulsation (EECP) therapy in patients with refractory angina pectoris and left ventricular dysfunction (report from The International EECP Patient Registry) Am J Cardiol. 2006;97(1):17–20. doi: 10.1016/j.amjcard.2005.07.122. [DOI] [PubMed] [Google Scholar]
- 21.Springer S, Fife A, Lawson W, Hui JC, Jandorf L, Cohn PF, et al. Psychosocial effects of enhanced external counterpulsation in the angina patient: a second study. Psychosomatics. 2001;42(2):124–32. doi: 10.1176/appi.psy.42.2.124. [DOI] [PubMed] [Google Scholar]
- 22.Linnemeier G, Rutter MK, Barsness G, Kennard ED, Nesto RW. Enhanced External Counterpulsation for the relief of angina in patients with diabetes: safety, efficacy and 1-year clinical outcomes. Am Heart j. 2003;146(3):453–8. doi: 10.1016/S0002-8703(03)00251-5. [DOI] [PubMed] [Google Scholar]


