Abstract
Background:
Sleep is an essential need in every individual's life. A disorder in the natural sleep can cause physical and mental problems. The elderly are usually faced with more sleep problems. Therefore, the present study aimed to define sleep behavior among the elderly hospitalized in Zahedan.
Materials and Methods:
This is a descriptive analytical study conducted on 300 elderly people aged 60 years and over who were hospitalized in Zahedan. In this research convenience sampling method was used and the research tool was a questionnaire. The data were collected through interviews. Descriptive (frequency distribution) and inferential (X2) statistical tests were employed to analyze the data.
Findings:
The results showed that 62% of the hospitalized elderly people (total of 300) had sleep disorder. About 44.7%took sleep medication in order to sleep, and only 16.7% did not take sleeping medications. About 44.7% had no special schedule for the time of their sleeping and waking up, and 4.3% were involved in drug abuse and smoking, and had a big dinner before sleeping. There was a significant association between sleep disorder, gender, education, living in urban or rural areas, the cause of hospitalization, and suffering from a chronic disease
Conclusions:
Sleep disorder and inappropriate sleep related behaviors had a high prevalence among the elderly. With regard to the important role of sleep in the quality of life of the elderly, detection of the reasons of sleep disorder, motivating them to practice an appropriate sleep behavior, and preventing them from having inappropriate sleep related behaviors are crucial issues.
Keywords: Sleep behavior, elderly, hospitalized elderly
INTRODUCTION
Sleep is essential for everybody and any disturbance in the natural sleep patterns can cause mental problems, and diminish the function of the brain. Although sleep disorder may be seen at any age, the elderly usually experience more problems.[1,2,3] As a matter of fact, the prevalence of sleep disorder is estimated to be about 10-20% in the general population.[4] Epidemiological studies report that 12-54% of the elderly suffer from sleep disorder.[5] Sleep disorders significantly influence the individuals’ quality of life resulting in a noticeable decrease in the physical, emotional and social aspects of their daily functions.[2]
The effect of sleep disorders and the illnesses they cause are seen more amongst the elderly compared to young people.[6]
The elderly often complain of problems such as difficulty in going to sleep, disintegration of sleep, short duration of sleep, low quality of sleep and drowsiness during daytime.[7] The most common sleep disorder in the elderly is insomnia from which 50% of the elderly suffer. Sleep disorder in the elderly results in short memory, concentration disorder, chronic fatigue,[8] visual auditory and behavioral disorders, higher risk of falling down, disability in daily life activities, napping during daytime, depression, and high intake of sleep medications.[6,2] Hospitalization can also worsen the clients’ sleep disorder.[9] Diseases, medications, environmental factors, depression and anxiety are among the most common causes for hospitalized clients’ sleep disorders. Studies have shown that insomnia can result in fatigue, irritability, aggression, and low tolerance to pain.[10] Since the elderly have the highest rate of incidence of hospitalization (38%), and the longest duration of stay in hospitals (45%), they experience the highest level of sleep disorder.[11]
Sleep related changes are among the main concerns of the elderly and should not be underestimated.[12] Although the prevalence of sleep disorders grows by age, these problems are not inevitable.[13] Investigation of individuals’ sleep health necessitates close detection of sleep habits and behaviors as well as environmental factors affecting sleep.[4] A comprehensive study of sleep behavior and appropriate interventions can help the elderly obtain their needed sleep and rest in order to have their highest function.[12] Therefore, the researcher decided to conduct a study on sleep related behaviors of hospitalized elderly people.
MATERIALS AND METHODS
This is a descriptive analytical study. The population studied comprised 300 elderly subjects, selected through convenient sampling, who were 60 years old and over, and were hospitalized in different hospitals in Zahedan. The researcher frequently visited all wards of hospitals in Zahedan, after obtaining the necessary official permissions, and selected the subjects based on the inclusion criteria until reaching the needed sample size. The data were collected with a questionnaire structured by the researcher. The validity (content and face) and reliability (test-retest) of the questionnaire were confirmed. The questionnaire, completed through interviews, included two sections of demographic characteristics, and sleep related behavior. The collected data were analyzed through SPSSver18.
Descriptive statistical tests such as concrete and relative frequency, mean, SD and inferential tests (x2) were employed to detect the association between the qualitative variables.
FINDING
About 54% of the elderly were male and 46% female with the mean age of 68.8(5.7) years. The lowest age of the samples was 60 and the highest 95 years. Most of the subjects (77.7%) were 60-74 years of age. About 69.6% lived in urban areas and 30.4% in rural areas. With regard to marital status, 69.7% were married and 29.3% were widowed. About 70% of the subjects were illiterate, 4.3% had reading and writing literacy, 12% primary school, 5.7% a high-school education, and 3% an associate and Bachelor's degree. About 76.3% of the subjects suffered from more than one chronic disease, 17% from one, and 6.7% suffered from no chronic diseases. The hospitalization was due to a chronic disease for 72.4% and acute diseases for 27.6%.
DISCUSSION
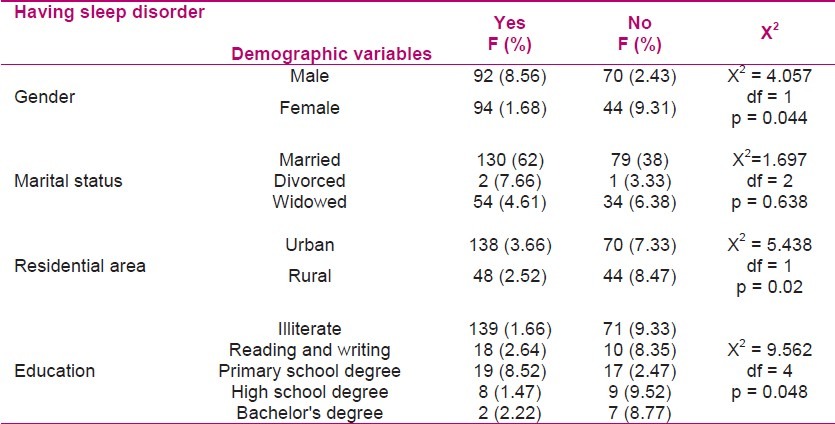
In The findings of this study showed that 62% of the subjects suffered from sleep disorder with a higher prevalence among female elderly subjects (68.1%) compared to male subjects (56.8%) (Table 1). Some other studies reported the prevalence of sleep disorder in the Iranian elderly to be 67% which is consistent with the result of the present study.[2] Epidemiologic data show that 12-54% of the elderly suffer from sleep disorder which is more prevalent among women compared to men. In a study by Mehra et al. on about 2400 elderly subjects, prevalence of insomnia was reported to be 54% in women and 36% in men.[5] In this study just as the current study the percentage of women suffering from insomnia is higher than the men.
Table 1.
Association of sleep disorder with demographic variables of the hospitalized subjects in Zahedan
The study by Foly et al. on over 9000 elderly people at ages of 65 and over found that, more than 42% of the subjects complained of a delay in going to sleep and sleep disintegration.[13]
Izadi Onji et al. (2006) showed that 390 hospitalized elderly in Kashan had low sleep quality, with women having lower sleep quality than men.[10]
Ahmadvand et al. (2008) studied 115 subjects over the age of 18 and reported that 59% had insomnia. About 67.9% of those aged 41-65 had insomnia with the highest frequency being in women (74.4%). They reported 60.9% sleep disorder in people over 65 years of age.[14]
In a study conducted by Ohayon and lemoine, the prevalence of insomnia was estimated to be 20-40% in west Europe with the highest level being in women and the elderly.[15]
In another study in Japan, the level of sleep disorder amongst the hospitalized elderly in Japan was reported to be 18.7% in men and 20.3% in women.[16] The results of the above researches show a higher prevalence of sleep disorders among the Iranian elderly possibly due to life style, socioeconomic and cultural factors, and low awareness of the importance of sleep and its role in elderly health.
In a survey conducted by Gallup on 1000 Americans at the age of 50 and over (43% were 65 or over) showed that 80% of the subjects believed sleep is important for elderly people's health. About 45% believed they needed more sleep compared to the youth, and 25% had sleep problems.[4]
Various studies as well as the present study showed higher rates of sleep disorder among women compared to men. Based on former studies, women experience sleep disorder twice as much as men due to various factors such as stress, diseases, sleeping place and being over weight.[14] Sleep disorder in women can also be due to post hormonal changes especially estrogen.[17] As women have more familial and social responsibilities, compared to men, the stress caused as a result of this can be another reason for higher prevalence of sleep disorder among women. Impaired sleep patterns caused during pregnancy and breast feeding may cause disordered sleep patterns even at the age of menopause.
The results of this study showed that there is a significant association between education and sleep disorders (p = 0.048) (Table 1). This means that less sleep disorders are seen among the elderly with a higher education compared to those with lower education.
Izadi Onji et al. showed that the quality of sleep is poorer among the elderly with less literacy compared to those of other age groups.[10] Dogan et al. also concluded that there is a higher rate of sleep disorder among those with lower education.[18]
Higher rate of sleep disorders among illiterate or low educated elderly people may be due to the effect of education on the level of awareness and efficient problem solving methods. Low educated elderly people also face more socioeconomic problems and stress with a negative effect on their natural sleep habits, compared to those with higher education.
Based on the present study, there was no significant association between marital status and sleep disorder. This finding is not in accordance with the results of Izadi Onji et al. which reported sleep quality to be better among the married compared to those divorced and widowed.[10] This difference can possibly be due to having more family support that the widowed elderly receive after losing their spouses.
The results of the present study showed that there is a significant association between residential area and sleep disorder (p = 0.014) so that those who live in urban areas (66.3%) complained more of sleep disorders compared to those who live in rural areas. This is possibly due to the difference between the urban life style of the elderly and its related stress versus rustic elderly life and its simple and low expectations (Table 1).
Although sleep disorders increase by age, they are not necessarily a part of the aging process but are a result of secondary physical and mental diseases as well as their related medications.[19]
With regard to the high prevalence of sleep disorders and their complications and health related outcomes in the elderly, the main concern is the bilateral association between sleep disorder and physical diseases among them.
Hypertension, depression, cardiovascular diseases and CVA put people at a higher risk of sleep disorders and vice versa[20]; therefore, one of the major reasons for sleep disorders of the studied elderly in this study can be chronic diseases.
The results of the present study showed a significant association between hospitalization due to chronic and acute diseases and sleep disorders (p = 0.01) so that the elderly hospitalized due to a chronic disease were reported to have more sleep disorders compared to those due to acute diseases. Another finding of the present study is less complaint of sleep disorder among those with one chronic disease (51.1%) compared to those with two or more (66.5%) (Table 2).
Table 2.
Association of sleep disorder with occupation, type of disease, number of chronic diseases in the elderly in hospitals of Zahedan
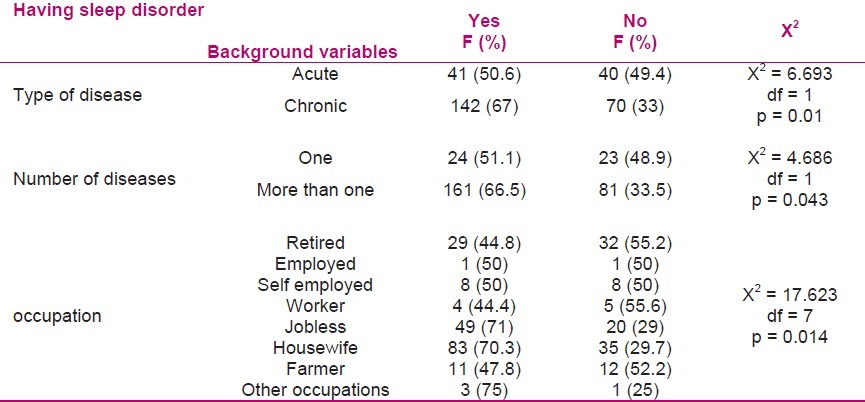
Most of the elderly regularly take several medications for their chronic diseases which worsen their sleep disorder. These medications are: beta blocker, bronchial vasodilators, corticosteroids, anti congestive, diuretics and other cardiovascular medications, especially anti depressants.[4] On the other hand, sleep disorder itself requires the elderly to take even more medication (Table 3).[9]
Table 3.
Frequency distribution of the subjects’ sleep and rest behaviors
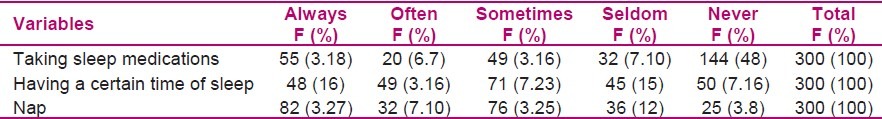
The results of the present study showed that 16% of the studied elderly always, 28.7% often, and only 16.7% never used to take sleep medications to go to sleep, reflecting the high intake of sleep medications among them. Mean while, high consumption of sleeping medications is a growing concern. It increased by 60% in US within 2000-2006, and American and European studies report 50% of sleep medications to be taken by those of 60 years of age and over. These medications are taken for a longer period of time compared to other medications.
Numerous studies have shown a vast number of side effects of sleep medications that can even increase mortality.[21] Therefore, physicians should avoid excessive prescription of sleep medications and the elderly should be given necessary education about their side effects, and the prevention of self medications. Nurses can also play a major role in educating their patients on these topics. Sleep health includes sleeping habits and behaviors as well as environmental factors that can affect sleep.[4] Having a regular schedule for sleeping and waking up is among the healthy behaviors affecting sleep.
The findings of the present study showed that 16% of the studied elderly always, 28.7% often and 23.7% sometimes have a certain schedule for their sleeping and waking up while 15% seldom and 16.7% never had such a schedule. going to bed and getting up at a certain time is recommended (Table 3).[22] This seems to set ones sleep and waking up to a certain time and to decrease the delay in going to sleep.
The findings of the present study show that from the 300 elderly people studied, 27.3% always, 27% often, 25.3% sometimes, 12% seldom, and 8.3% never took a nap during the day (Table 3). Napping is a behavior that brings about sleep disorders.[4] Anxiety and napping especially in the evening can impair night sleep.[22] Foley states that an increase in age is not a direct cause of napping but it gives the elderly more chance and time to nap.[13] A study showed that a nap during the day can complete night sleep with the only negative effect of causing a delay in going to sleep at night.[10] Izadi Onji et al. reported no association between napping during the day and sleep quality, which needs further investigation. Finally, the elderly are recommended against frequent and long naps during the day, and are advised to go to bed just for sleeping and having sex.[10]
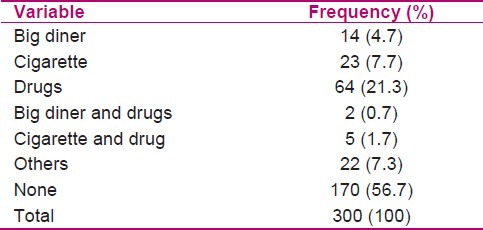
The present study showed that 56.7% of the subjects were not involved in drug abuse, did not have a big diner, drink alcohol, or smoking cigarettes before sleep. However 21.3% used drugs, 7.7% smoked cigarettes and 4.7% had a big diner before sleeping (Table 4). Eating heavy food or smoking is not recommended before sleep.[23] The use of cigarettes, coffee and nicotine can disrupt natural sleep.[4] Ahmadvand et al. showed heavy smokers to have more insomnia.[14] However, giving up this habit is very hard for the elderly, and needs education and a great deal of time.
Table 4.
Frequency distribution of taken materials before sleep among the subjects
CONCLUSION
Sleep disorders and inappropriate sleep behaviors had a high prevalence among the elderly. With regard to the important role of sleep in the quality of life of the elderly, it is crucial that we detect the causes of sleep disorders amongst them, and educate and motivate them to obtain appropriate behavior, and prevent them from inappropriate sleep behaviors. Therefore, strategies should be taken so that the elderly regularly assess their sleep habits and behaviors as a part of their health and try to promote the quality of their sleep.
Since, nurses spend more time with the patients in hospitals compared to other health team members, they are in a better position to detect sleep disorders and educate the patients about healthy sleep behaviors. Inappropriate sleep behavior seems to be due to lack of awareness which can be decreased or amended through the necessary education
ACKNOWLEDGMENT
We would like to greatly acknowledge the Health Promotion Association of Zahedan, Research Deputy of University of Medical Sciences, and the manager of Social Security hospital, as well as all the elderly attending this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Monahan F, Sands JK, Neighbors M, Marek JF. Phipps’ Medical-Surgical Nursing: Health and Illness Perspectives. Philadelphia: Elsevier Mosby; 2007. pp. 10–29. [Google Scholar]
- 2.Hosian Abdi R, Noroozi Tabrizi K, Poresmaeeli R, Karimloo M, Madah SB. Survey of massage effect on pressure points in elderly quality of sleep. Rehabilitation. 2008;9(2):8–14. [Google Scholar]
- 3.Smeltzer SC, Bare BG, Hinkle JL, Cheever KH. Brunner & Suddarth's Textbook of Medical Surgical NursingAuthors. 11th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 4.Bloom HG, Ahmed I, Alessi CA, Ancoli-Israel S, Buysse DJ, Kryger MH, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc. 2009;57(5):761–89. doi: 10.1111/j.1532-5415.2009.02220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehra R, Stone KL, Ancoli-Israel S, Litwack-Harrison S, Ensrud KE, Redline S. Interpreting wrist actigraphic indices of sleep in epidemiologic studies of the elderly: the Study of Osteoporotic Fractures. Sleep. 2008;31(11):1569–76. doi: 10.1093/sleep/31.11.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaz Fragoso CA, Gill TM. Sleep complaints in community-living older persons: a multifactorial geriatric syndrome. J Am Geriatr Soc. 2007;55(11):1853–66. doi: 10.1111/j.1532-5415.2007.01399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldman SE, Stone KL, Ancoli-Israel S, Blackwell T, Ewing SK, Boudreau R, et al. Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep. 2007;30(10):1317–24. doi: 10.1093/sleep/30.10.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamel NS, Gammack JK. Insomnia in the elderly: cause, approach, and treatment. Am J Med. 2006;119(6):463–9. doi: 10.1016/j.amjmed.2005.10.051. [DOI] [PubMed] [Google Scholar]
- 9.Zeraati F, Saifrabiee M, Araghchian M, Saburi T. Quality of sleep and sleep medication use in adults admitted to hospital in the inner parts Ekbatan. Scientific Journal of Hamadan University of Medical Science. 2009;16(4):31–6. [Google Scholar]
- 10.Izadi Onji FS, Adib Hajbagheri M, Afazel MR. Quality of sleep and associated factors in hospitalized elderly patients in Kashan 2006. Fiaze. 2008;12(4):52–9. [Google Scholar]
- 11.Smeltzer S, Bare B, Hinkle J. Community&Public Health Nursing? 6th ed. Phildelphia: Mosby; 2004. pp. 700–15. [Google Scholar]
- 12.Hofmanwold G. In: Nursing in elderly. Abedi HA, Shahriari M, Alimohammadi N, Yazdannik A, Yosefi H, editors. Isfahan: Orroj Publication; 2003. p. 359. [Google Scholar]
- 13.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 14.Ahmadvand A, Sepehrmanesh Z, Ghoreyshi F, Mosavi S. Survey of incidence insomnia in eighteen age person and upper in Kashan 2008. Feize. 2009;13(4):313–21. [Google Scholar]
- 15.Ohayon MM, Lemoine P. Sleep and insomnia markers in the general population. Encephale. 2004;30(2):135–40. doi: 10.1016/s0013-7006(04)95423-1. [DOI] [PubMed] [Google Scholar]
- 16.Shirakawa S, Takahashi K. Epidemiology of sleep disorders. Nihon Rinsho. 1998;56(2):475–81. [PubMed] [Google Scholar]
- 17.Kalleinen N, Polo O, Himanen SL, Joutsen A, Urrila AS, Polo-Kantola P. Sleep deprivation and hormone therapy in postmenopausal women. Sleep Med. 2006;7(5):436–47. doi: 10.1016/j.sleep.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Dogan O, Ertekin S, Dogan S. Sleep quality in hospitalized patients. J Clin Nurs. 2005;14(1):107–13. doi: 10.1111/j.1365-2702.2004.01011.x. [DOI] [PubMed] [Google Scholar]
- 19.Ancoli-Israel S, Ayalon L. Diagnosis and treatment of sleep disorders in older adults. Am J Geriatr Psychiatry. 2006;14(2):95–103. doi: 10.1097/01.JGP.0000196627.12010.d1. [DOI] [PubMed] [Google Scholar]
- 20.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30(2):213–8. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 21.Sivertsen B, Omvik S, Pallesen S, Nordhus IH, Bjorvatn B. Sleep and sleep disorders in chronic users of zopiclone and drug-free insomniacs. J Clin Sleep Med. 2009;5(4):349–54. [PMC free article] [PubMed] [Google Scholar]
- 22.Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: Sleep disorders commonly found in older people. CMAJ. 2007;176(9):1299–304. doi: 10.1503/cmaj.060792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: 2. Management of sleep disorders in older people. CMAJ. 2007;176(10):1449–54. doi: 10.1503/cmaj.070335. [DOI] [PMC free article] [PubMed] [Google Scholar]


