Abstract
Purpose:
The aim of this study is to present muscle patterns observed with the direction of instability in a series of patients presenting with recurrent shoulder instability.
Materials and Methods:
A retrospective review was carried out on shoulder instability cases referred for fine wire dynamic electromyography (DEMG) studies at a specialist upper limb centre between 1981 and 2003. An experienced consultant clinical neurophysiologist performed dual needle insertion into four muscles (pectoralis major (PM), latissimus dorsi (LD), anterior deltoid (AD) and infraspinatus (IS)) in shoulders that were suspected to have increased or suppressed activation of muscles that could be contributing to the instability. Raw EMG signals were obtained while subjects performed simple uniplanar movements of the shoulder. The presence or absence of muscle activation was noted and compared to clinical diagnosis and direction of instability.
Results:
A total of 140 (26.6%) shoulders were referred for fine wire EMG, and 131 studies were completed. Of the shoulders tested, 122 shoulders (93%) were identified as having abnormal patterns and nine had normal patterns. PM was found to be more active in 60% of shoulders presenting with anterior instability. LD was found to be more active in 81% of shoulders with anterior instability and 80% with posterior instability. AD was found to be more active in 22% of shoulders with anterior instability and 18% with posterior instability. IS was found to be inappropriately inactive in only 3% of shoulders with anterior instability but in 25% with posterior instability. Clinical assessment identified 93% of cases suspected to have muscle patterning, but the specificity of the clinical assessment was only correct in 11% of cases.
Conclusion:
The DEMG results suggest that increased activation of LD may play a role in both anterior and posterior shoulder instability; increased activation of PM may play a role in anterior instability.
Keywords: Dynamic electromyography, electromyography, multidirectional instability, muscle activation patterns, recurrent shoulder instability
INTRODUCTION
Glenohumeral instability (henceforward referred to as shoulder instability) is a symptomatic abnormal motion of the glenohumeral joint (GHJ), which presents as a spectrum of symptoms from cryptogenic pain to a sense of, or actual, displacement (subluxation/dislocation).[1] The prevalence of shoulder instability has been reported as 10% of all athletic injuries, the majority of which are traumatic in nature.[2]
Atraumatic shoulder instability may exist as a collagen deficiency disorder of the connective tissues of the shoulder (the spectrum which includes generalized joint laxity or the so-called benign hypermobility syndrome), and may be associated with aberrant muscle activation or inappropriate muscle suppression.
Furthermore, the shoulder may displace or be symptomatic in more than one direction – the so-called multidirectional instability (MDI). The recommendation for these two groups of patients has been to prescribe a physiotherapy program that targets the rotator cuff muscles.[3] However, some patients fail to respond. Previously patients who have failed to respond to a therapy-based rehabilitation programme have been offered a capsular procedure (inferior capsular shift).[4] However, some patients fail this procedure. The senior author considered early on that these cases might be explained by a failure of normal muscle activation patterns outside the rotator cuff, and demonstrated the value of DEMG in describing aberrant muscle patterns in selected muscles.[1,5]
The purpose of this paper is to present the DEMG data collected on a large cohort of patients with recurrent shoulder instability and to demonstrate that muscles other than the rotator cuff play a role in generating shoulder instability.
Inappropriate muscle activation has been observed to contribute to shoulder instability and studies have reported that muscles can have both a stabilizing and destabilizing role.[6–16] The methodology, the definition of subject groups and data analysis, varies considerably between studies. This makes the understanding of aberrant muscle control around the shoulder girdle and its relationship to shoulder instability a potentially fruitful area of further research.
The study of muscle function through EMG is an established method for quantifying muscle activity through electrical activity. EMG was first used in the clinical setting as a tool to help in the diagnostic assessment of muscle activity around the shoulder girdle in the early 1970s, but since then there have been few published studies in large numbers of patients and different directions of instability.[16] Its use at this specialist shoulder unit was established over 25 years ago and has been performed by an experienced neurophysiologist on a large number of patients. The study reports on patterns observed in four muscles: Pectoralis major (PM), latissimus dorsi (LD), anterior deltoid (AD), and infraspinatus (IS). These muscles were chosen as they had been observed in the clinic to be involved in some cases of recalcitrant shoulder instability. Importantly, they were accessible to fine wire EMG, and had an explicit, well-documented action on the GHJ.
The clinical question to be addressed by EMG in patients was to simply establish whether the four key muscles being studied were active or not, when compared with the expected normal patterns of activity, established by previous researchers.[17–20] Normal activation patterns were based on established literature and the biomechanical actions of muscles.[17–20] Figure 1a-c illustrates normal activation patterns for the muscles when performing five different planes of movement. We were not attempting to establish whether there were thresholds for the amount of individual muscle activation for specific movements or in specific directions of instability and, therefore, normalization of the EMG signal was not undertaken. EMG formed part of a clinical picture, and further tests such as imaging and diagnostic arthroscopy were also undertaken as appropriate to help correctly classify cases. The aim of this study is to present the relationship between the muscle patterns observed with the direction of instability in a series of patients presenting with recurrent shoulder instability.
Figure 1.
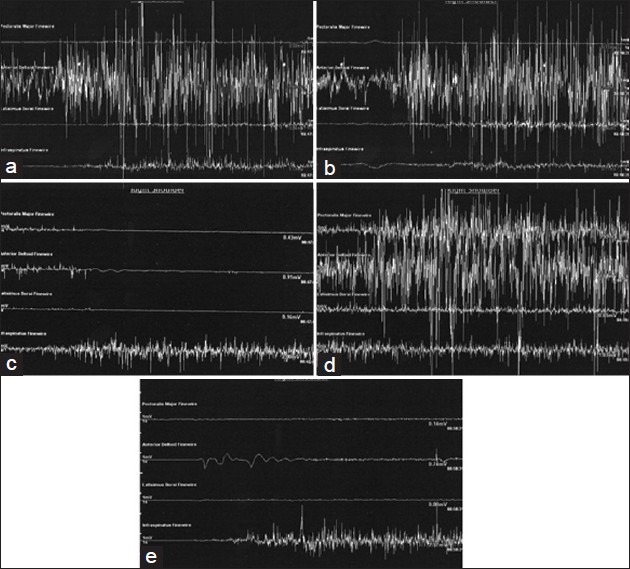
Patterns of normal electromyography (EMG) activity. In trace, the four EMGs shown in order from top to bottom are pectoralis major (PM), anterior deltoid (AD), latissimus dorsi (LD), and infraspinatus (IS). (a) EMG activity during flexion: PM and LD inactive and AD and IS active. (b) EMG activity during abduction: PM and LD inactive and AD and IS active. (c) EMG activity during external rotation: PM, LD, and AD inactive, activity only in IS. (d) EMG activity during flexion/ adduction: Activity in all the muscles. (e) EMG activity in extension with minimal or no activity in PM/AD/LD, but activity in IS
MATERIALS AND METHODS
Subjects
A records review was carried out for patients presenting with recurrent shoulder instability to a specialist shoulder service between 1983 and 2003. A total of 875 patient notes were reviewed and within this group 1057 shoulders were identified with recurrent shoulder instability. Clinically apparent abnormal muscle patterning shoulder instability was seen in 526 shoulders (49.7%). Fine wire EMG was requested in 140 shoulders (130 patients) with suspected, subclinical or clinically complex muscle patterning. There were a total of 67 females and 63 males with a median age of 22 years. A total of 83 right shoulders and 47 left shoulders were tested. There were 10 bilateral cases. A total of 131 shoulders were analysed as nine patients failed to complete the test. The majority of patients had an atraumatic history to their instability.
Clinical assessment of muscle patterning was made by the senior orthopedic consultant through observation of movement, displacements of the GHJ, scapular dyskinesia, and palpating abnormal muscle tone. The direction of instability was assessed using the standard apprehensive and draw tests for instability, or was clearly visible as the patient performed active movements. In addition, for some cases a diagnostic arthroscopy was performed which indicated characteristic features which further confirmed the direction of instability.
Electromyography equipment and procedure
A dual needle insertion technique was used where pairs of fine wires custom made of tungsten and coated with Teflon (diameter = 0.050 mm) were inserted intramuscularly, using one hypodermic needle for each wire with an interelectrode distance of about 1 cm.[21] The Teflon insulation (0.0125 mm thick) was removed from a length of approximately 2 mm at the intramuscular end, and about 20 mm at the other end. Connecting cables joined the wires with a differential preamplifier of a 4 channel EMG machine (Sapphire 2, Medilec, UK). Single, unrectified sweeps lasting 10 s were recorded from four muscles simultaneously. Signals were collected and were printed out for later analysis.
Prior to testing, the procedure was fully explained to patients and verbal consent was gained: Patients were able to withdraw from the test at any point if they so wished. Since the test was part of normal clinical practice, ethical approval for this study was not sought or required. Bony landmarks were used to help locate muscle sites for electrode insertion. The patients were asked to perform gentle resisted tests to ensure that each electrode was in the correct muscle. The patients were tested while seated, and individual recordings from the four muscles were obtained during each of five uniplanar movements with the arm unloaded [Table 1]. Recording was started about 2 s before the subject was asked to move, so that the premovement state (anticipatory presetting phase) could also be studied and to eliminate the “noise” associated with voluntary relaxation. The patients were asked to perform the movements slowly to a count of four and were encouraged not to hurt themselves, or to risk a displacement that would be painful or result in dislocation. Activation of a muscle was identified as any activity over resting baseline. Inappropriate activation or inappropriate inactivation of any muscle studied was noted.
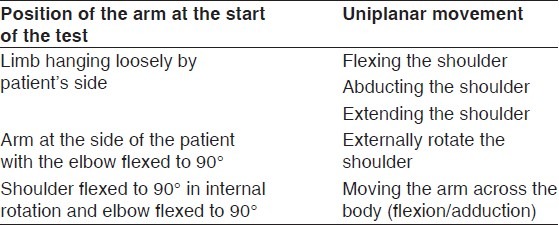
Table 1.
Testing positions for electromyography tests
The reference normal activation patterns for the four specific muscles in the planes tested were assumed as follows: Sternal fibers of PM only active in cross body adduction; LD active on extension and cross body adduction; AD active in flexion, abduction, and cross body adduction (does not play a role in external or internal rotation when the arm is at the side of the body); IS acts as a force couple with the rotator cuff and is active in all movements. Abnormal activation patterns for the four specific muscles in the planes tested were therefore assumed as follows: Activity in PM on flexion, abduction, external rotation, and extension; AD active on external rotation and extension; LD active in flexion, abduction, and external rotation; and IS inactive in any one of the movements.
DEMG recordings were then analysed by the same neurophysiologist for all patients studied, and the interpretation of the muscle patterns was documented in the case notes. The analysis of the patterns was made independently of the senior orthopedic consultant's clinical assessment and knowledge of other diagnostic tests.
RESULTS
A total of 140 (26.6%) out of 526 shoulders with a component of muscle patterning were referred for dynamic EMGs. The group comprised 67 females and 63 males with a median age of 22 years (range, 7-44). A total of 131 shoulders completed the EMG tests and nine (five females, four males) were excluded: Four due to technical difficulties, three due to patient-related factors (one unwell on the day, one apprehensive of the procedure, and one fainted), and two patients did not attend the appointment. A total of 78 right shoulders, and 43 left shoulders, and in 10 cases both shoulders, were tested.
Out of the 131 shoulders that completed the test, 122 (93%) had abnormal patterns and nine (7%) were reported as having normal activation patterns. Table 2 summarizes the muscle patterns observed according to the direction of instability (anterior, posterior, inferior, and MDI). Figure 2 highlights the overall contribution of PM and LD to anterior and posterior directions of shoulder instability. Each shoulder had a median of two muscles that were inappropriately active.
Table 2.
Dynamic electromyography results
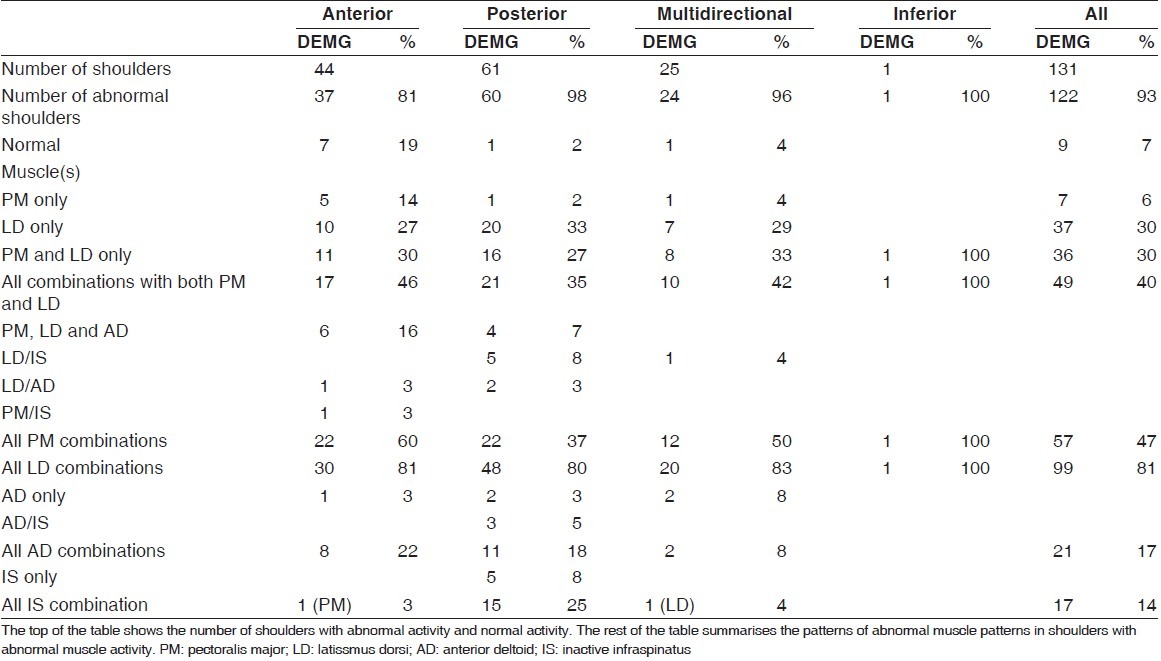
Figure 2.
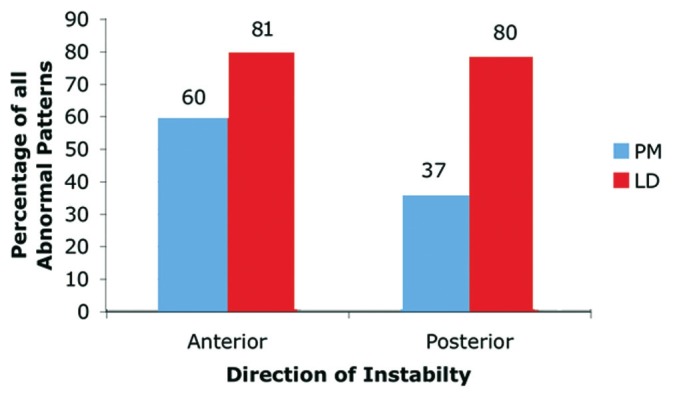
The percentage of shoulders that had abnormal muscle patterns involving pectoralis major (PM) or latissimus dorsi (LD) either acting alone or in combination with other muscles
We compared clinical accuracy in detecting abnormal muscle patterns with the DEMG output. Abnormal muscle patterns were identified de novo in 47 shoulders that had subclinical muscle patterning (i.e., suspected, but not clinically obvious aberrant patterning).
Seventy-five shoulders had abnormal muscle patterning identified clinically. Dynamic EMG confirmed that these shoulders had muscle patterning, but the identification of the specific muscle with abnormal activity was incorrect in 34 shoulders (45%). The clinically abnormal patterns were confirmed exactly in only eight shoulders (11%). In the other 33 shoulders (44%), the diagnosis was partially correct. In this latter group, at least one of the four muscles identified as abnormal by clinical examination was confirmed by dynamic EMG. However, dynamic EMG also picked up abnormal pattern in other muscles that had subclinical patterns [Figure 3]. Figure 4 illustrates examples of abnormal EMG patterns.
Figure 3.
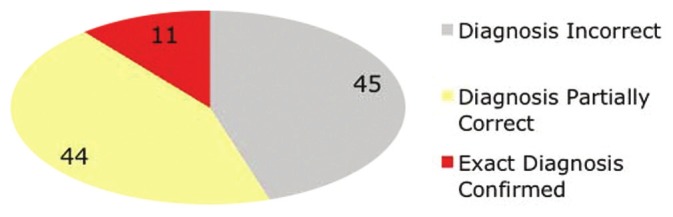
Clinical patterns of abnormal muscle patterning was exactly confirmed in only a small proportion of shoulders (Red; 11%)
Figure 4.
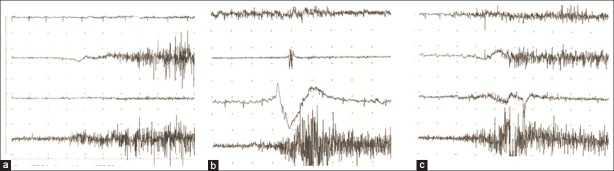
Patterns of abnormal electromyography activity. In trace, the four electromyographys shown in order from top to bottom are pectoralis major (PM), anterior deltoid (AD), latissimus dorsi (LD), and infraspinatus (IS). (a) Abnormal electromyography activity in AD during extension. (b) Abnormal electromyography activity in PM and LD during extension. (c) Abnormal electromyography activity in PM during external rotation
DISCUSSION
Functional stability of the GHJ is achieved by the principle of concavity compression generated by the rotator cuff, mediated through the capsulolabral complex, supported by relative osteoarticular congruency.[22,23] Rehabilitation protocols for the management of shoulder instability have essentially focused on recruitment and regaining strength with endurance of the rotator cuff.[3] Recently, the role other muscles (in particular PM and LD) that may play in GHJ instability has been discussed.[10,12,13] Adverse timing and aberrant recruitment of larger superficial torque muscles around the thorax and the shoulder girdle may also contribute to shoulder instability, either in conjunction with abnormal patterns of the rotator cuff or in isolation. This review of cases of recurrent shoulder instability at a specialist tertiary referral shoulder service has shown abnormal activation patterns in PM, LD, AD, and ISP and further contributes to that discussion.
Unidirectional instability
Anterior instability
Anterior instability represented 37 of cases in this cohort compared to 60 cases of posterior instability, implying that anterior instability is less common in myocardial perfusion imaging (MPI). Both PM and LD were found to be inappropriately active in anterior instability, 60% and 81%, respectively. PM appeared to be more inappropriately active in anterior instability than in posterior instability.
Anatomically, the PM muscle has three origins. Its upper fibers (clavicular portion) originate from the anterior surface of the sternal half of the clavicle, its lower fibers (sternal portion) from the anterior surface of the sternum, and the costal portion from the cartilages of first six or seven ribs and aponeurosis of the external oblique; all portions insert on to the crest of the greater tubercle of the humerus. The action of the whole muscle with the origin fixed is to adduct and medially rotate the humerus. The sternal portion also depresses the shoulder girdle by virtue of its attachment on the humerus. If the lower fibers of PM are short, there is forward depression of the shoulder girdle often accompanied by the pull of pectoralis minor on the scapula.[19]
If PM is active in abduction and/or external rotation particularly in end range positions, it may medially rotate the humerus; when combined with downward depression of the shoulder girdle, excessive anterior translation of the humerus on the glenoids can occur. If this is not balanced by the combined rotator cuff, anterior translation of the humeral head may result. This has been demonstrated in a cadaveric study.[12] These authors also noted that simulated decreased muscle activity in IS resulted in decreased compressive forces at the glenoid. If either anteriorly directed forces increased or compressive forces decreased, then stability of the GHJ decreased. Only one case of anterior instability in this series showed inappropriate inactivity of IS. As EMGs were not normalized, the data cannot indicate the ratio of PM to IS activity, and it can be assumed that although IS was active the resultant anterior instability may have been due to the relative increased activation of PM. The action of PM alone may create an anterior translation of the GHJ. A case of persistent anterior dislocation has demonstrated that the administration of botulinum toxin to PM enabled relocation of the GHJ. The GHJ remained stable strongly suggesting that in this case, the persistence of anterior dislocation was a direct result of increased activation of PM.[24]
The LD originates from the spinous processes of the last six thoracic vertebrae, last three or four ribs, through the thoracolumbar fascia from the lumbar and sacral vertebrae and posterior one-third of the external lip of the iliac crest as well as a slip from the inferior angle of the scapula. It inserts into the intertubercular groove of the humerus. Its action with the origin fixed is to medially rotate, adduct, and extend the shoulder joint. By continued action, it depresses the shoulder girdle and assists in lateral flexion of the trunk.[19]
With the arm in an end range position of abduction and external rotation, the action of LD (medial rotation and depression of the shoulder girdle) is similar to PM and could result in anteriorly directed forces on the GHJ. Cadaveric models have demonstrated that thoracohumeral muscle activity creates a more anteriorly directed joint reaction force that resulted in anterior translation.[10] The ratio between anteriorly directed translational forces and compressive forces increased during abduction due to this muscle activity, suggesting that thoracohumeral muscle activity may decrease glenohumeral stability based on the joint position and applied loads. Such inappropriate activity in the thoracohumeral muscles may be of relevance in the early and late phases of rehabilitation and following surgical stabilization, when the compressive forces of the rotator cuff may still be compromised and could result in anteriorly directed forces jeopardizing the success of repair.[25,26]
In this study, AD was inappropriate in 22% of anterior instability but acted mainly with other muscles when displacement occurred. Commenting on deltoid is difficult without additional information on the middle and posterior portions of deltoid, and it is difficult to determine whether its over activation noted on DEMG in this study was having a destabilising effect. The stabilising role of deltoid has been studied: Deltoid is an important anterior stabilizer and its function becomes more important when the shoulder becomes more unstable.[9,14] This may explain its inappropriate over activation in the 22% cases of anterior instability found in this review when additional muscles such as PM and LD were having a destabilising effect. Another study proposed that forces from AD may aggravate posterior instability.[7] It appears reasonable, by virtue of its anatomy, to assume that if there is an abnormal force couple between the different parts of deltoid, the stabilizing effect may be affected resulting in either anterior or posterior translation of the shoulder dependent on the direction of movement of the humerus.
Posterior instability
The key muscles which seemed to be involved in posterior instability in this study were LD and IS. LD was inappropriately active in 80% of cases (33% alone), and IS was inappropriately inactive in 25% (8% alone) of posterior instability indicating that posterior translation of the GHJ may be more a result of over activation of LD and/or inactivity of IS.
In posterior instability, when the arm is more commonly in a forward elevation position, it is reasonable to surmise that the insertion of LD into the intertubercular groove of the humerus could result in excess medial rotation and downward depression of the shoulder resulting in posterior translation of the GHJ. If the muscle is inappropriately active, its resultant effect at the shoulder girdle creating a downward depression of the scapula and excessive internal rotation of the GHJ could result in posterior displacement. There is a lack of information with regard to muscle activation patterns in posterior instability, but clinical observations of this less common direction of instability suggest inappropriate activation of LD; in addition, rehabilitation programmes that have targeted the postural trunk muscles as well as the rotator cuff have been found to be beneficial in managing cases of posterior instability.[25] Whether this directly reduces the inappropriate action of LD has yet to be addressed. In this study, 33% of posterior instabilities were due to LD alone compared to only 2% of PM, 3% of AD, and 8% of IS indicating that this muscle may play a big role in posterior instability.
The IS originates from the medial two-thirds of the infraspinous fossa and inserts onto the middle facet of the greater tubercle of the humerus and shoulder joint capsule. It laterally rotates the shoulder joint and stabilizes the humeral head in the glenoid cavity during movements of this joint.[19]
It has been suggested that the rotator cuff acts as a single unit to stabilize the GHJ. However, recent research has indicated that the parts of the rotator cuff do not co-contract at similar intensity and that different portions of the rotator cuff are active in different planes of movement.[27] IS was inactive in 25% of posterior instability cases in this series and was the only muscle involved in 8% of posterior instability. As mentioned earlier, this study was unable to look at relative activity of muscles against each other so it can be assumed that the IS may have been activating but was suppressed compared to the more superficial torque muscles resulting in displacement. It can also not be assumed that activation patterns in IS are representative of what is occurring in the rest of the rotator cuff and so further studies including EMG analysis of supraspinatus and subscapularis are required to gain a more accurate understanding of rotator cuff activation in GHJ instability. This study suggests that IS may play more of a role in posterior instability. The patients whose GHJ posteriorly sublux when the limb is elevating in the sagittal plane possibly due to over activation of LD have been stabilized when the movement is repeated with resisted external rotation and abduction. This suggests that activating the posterior rotator cuff and deltoid can prevent posterior instability.[25]
In posterior GHJ instability, PM was found to be inappropriately active in 37% of cases but acting alone in only one case (2%). AD was only found to be inappropriately active in 18% of posterior instability. The early experience with cases of so-called voluntary (an historic term no longer used in this institution) posterior instability appeared to indicate that posterior humeral head displacement was a result of activation of PM and/or AD with suppression of the rotator cuff,[22] these results do not wholly support this.
Multidirectional instability
The term multidirectional instability (MDI) as described in this paper is defined as a shoulder that is symptomatically unstable in all three directions. This does not equate to a shoulder that is multidirectionally lax but only symptomatic in one direction. Such cases have an element of inferior instability and then dependent on the plane of movement can experience symptoms both in an anteroinferior direction as well as a posteroinferior direction.
LD appeared to be the most dominant muscle involved in MDI. Considering the results indicate that LD can contribute both to anterior and posterior instability, it would be feasible to explain that MDI with abnormal muscle patterning may be due to over activation of LD. It is also reasonable to expect LD to create an inferior translation of the GHJ, depending on which plane the arm is placed it will influence GHJ translation in either an anteroinferior or a posteroinferior direction. There was only one case of pure inferior instability in this study that showed inappropriate activation of both the PM and LD as discussed earlier and both these muscles can create downward depression at the shoulder girdle and if there is associated suppression within the RC and/or deltoid, this will cause inferior instability.
A recent study showed altered recruitment patterns of deltoid in subjects with MDI compared to normal subjects when performing rotation at neutral and 90° of abduction.[14] More interestingly, abnormalities were observed in the deltoid rather than the rotator cuff in subjects with MDI. The study, however, did not clearly define MDI. As not all the deltoid and RC were needled in this study, results are not comparable.
Clinical versus electromyography examination
Shoulders suspected clinically to have abnormal muscle patterning were confirmed with EMG, but, in nearly half the cases, the suspected specific muscles were incorrectly identified suggesting that diagnostic EMG can be useful in the diagnosis of occult muscle patterning in the etiology of shoulder instability. A more specific assessment of muscle activation patterns may further assist in developing specific rehabilitation protocols so increasing the success of physiotherapy treatment.
Limitations
This study is based on retrospective data which weaken the strength of the conclusions. However, the cohort size is large and there are no other epidemiological studies to date on aberrant muscle activity in such a large number of symptomatic shoulders. The method of EMG analysis was based on the previous literature and the accepted biomechanical action of the muscles and has not been compared to asymptomatic subjects, currently the subjects of further study in this institution. The reported data also failed to highlight the specific movement in which the muscles were acting inappropriately that could have further helped to validate the conclusions made in this study. It has been acknowledged that additional muscles (e.g. subscapularis, supraspinatus, trapezius, and serratus anterior) that are involved both in GHJ stability as well as scapulo-thoracic control should be tested to further understand the role other muscles play in shoulder instability. The increased inappropriate activation of PM, LD, and AD has been hypothesized to be a cause for GHJ instability, but it is not clear if these muscles are acting solely and create abnormal translation of the GHJ or are increasing their activation as a secondary effect to compensate for the instability.
CONCLUSION
LD and PM were the two muscles predominantly involved in instability in this study; further work is required to better understand their role. LD appeared to be inappropriately active in both cases of anterior and posterior instability, PM appeared to be more involved in anterior instability and IS appeared to play a role in posterior instability. Clinical assessment for inappropriate muscle activation is often inaccurate and incomplete: DEMG helps to avoid incomplete diagnoses in patients with cryptogenic shoulder instability, particularly those in whom previous interventions including rehabilitation programmes have failed to achieve stability of the shoulder. MDI can be characterized with greater confidence and accuracy. The mechanism of instability is not necessarily the same for all directions of instability. DEMG helps to characterize the specific pathology for each/all directions where muscle-patterning contributes to the instability, and can help to explain some of the failures of surgical interventions on these cases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lewis A, Kitamura T, Bayley JIL. Mini symposium: Shoulder instability (ii) The classification of shoulder instability: New light through old windows! . Curr Orthop. 2004;18:97–108. [Google Scholar]
- 2.Walton J, Paxinos A, Tzannes A, Callanan M, Hayes K, Murrell GA. The unstable shoulder in the adolescent athlete. Am J Sports Med. 2002;30:758–67. doi: 10.1177/03635465020300052401. [DOI] [PubMed] [Google Scholar]
- 3.Burkhead WZ, Jr, Rockwood CA., Jr Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74:890–6. [PubMed] [Google Scholar]
- 4.Neer CS, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder: A preliminary report. J Bone Joint Surg. 1980;62A:897–908. [PubMed] [Google Scholar]
- 5.McAuliffe TB, Pangayatselvan T, Bayley JI. Failed surgery for recurrent anterior dislocation of the shoulder. J Bone Joint Surg. 1988;70B:798–801. doi: 10.1302/0301-620X.70B5.3192583. [DOI] [PubMed] [Google Scholar]
- 6.Barden JM, Balyk R, Raso VJ, Moreau M, Bagnall K. Atypical shoulder muscle activation in multidirectional instability. Clin Neurophysiol. 2005;116:1846–57. doi: 10.1016/j.clinph.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 7.Blasier RB, Soslowsky LJ, Malicky DM, Palmer ML. Posterior glenohumeral subluxation: Active and passive stabilization in a biomechanical model. J Bone Joint Surg. 1997;79A:433–40. [PubMed] [Google Scholar]
- 8.Glousman R, Jobe F, Tibone J, Moynes D, Antonelli D, Perry J. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg. 1988;70:220–6. [PubMed] [Google Scholar]
- 9.Kido T, Itoi E, Lee SB, Neale PG, An KN. Dynamic stabilizing function of the deltoid muscle in shoulders with anterior instability. Am J Sports Med. 2003;31:399–403. doi: 10.1177/03635465030310031201. [DOI] [PubMed] [Google Scholar]
- 10.Konrad GG, Jolly JT, Labriola JE, McMahon PJ, Debski RE. Thoracohumeral muscle activity alters glenohumeral joint biomechanics during active abduction. J Orthop Res. 2006;24:748–56. doi: 10.1002/jor.20062. [DOI] [PubMed] [Google Scholar]
- 11.Kronberg M, Nemeth G, Brostrom L. Muscle activity and coordination in the normal shoulder, an electromyographic study. Clin Orthop Relat Res. 1990;257:76–85. [PubMed] [Google Scholar]
- 12.Labriola JE, Lee TQ, Debski RE, McMahon PJ. Stability and instability of the glenohumeral joint: The role of shoulder muscles. J Shoulder Elbow Surg. 2005;14:32–8. doi: 10.1016/j.jse.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 13.McMahon PJ, Lee TQ. Muscles may contribute to shoulder dislocation and stability. Clin Orthop Relat Res. 2002;403:18–25. doi: 10.1097/00003086-200210001-00003. [DOI] [PubMed] [Google Scholar]
- 14.Morris AD, Kemp GJ, Frostick SP. Shoulder electromyography in multidirectional instability. J Shoulder Elbow Surg. 2004;13:24–9. doi: 10.1016/j.jse.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 15.Pande P, Hawkins R, Peat M. Electromyography in voluntary posterior instability of the shoulder. Am J Sports Med. 1989;17:644–8. doi: 10.1177/036354658901700509. [DOI] [PubMed] [Google Scholar]
- 16.Rowe C, Pierce DS, Cark JG. Voluntary dislocation of the shoulder. J Bone Joint Surg. 1973;55A:445–60. [PubMed] [Google Scholar]
- 17.Inman VT, Saunders M, Abbott LC. Observations on the function of the shoulder joint. J Bone Joint Surg. 1944;62A:1–30. [Google Scholar]
- 18.Basmajian JV, De Luca, CJ . 5th ed. Baltimore, MD: Williams and Wilkins; 1985. Muscles Alive: Their Functions Revealed by Electromyography. [Google Scholar]
- 19.Kendall FP, McCreary EK, Provance PG. Chap. 8. Upper Extremity and Shoulder Girdle Strength Tests. In: Butler JP, editor. Muscles: Testing and Function, with Posture and Pain. 4th ed. Baltimore,MD: Williams and Wilkins; 1993. [Google Scholar]
- 20.Speer KP, Garrett WE. Muscular control of motion and stability about the pectoral girdle. In: Matsen FA, Fu FH, Hawkins RJ, editors. The Shoulder: A Balance of Mobility and Stability. Rosemant, Illinois, USA: American Academy of Orthopaedic Surgeons; 1993. [Google Scholar]
- 21.Kelly BT, Cooper LW, Kirkendall DT, Speer KP. Technical considerations for electromyographic research on the shoulder. Clin Orthop Relat Res. 1997;335:140–51. [PubMed] [Google Scholar]
- 22.Abboud JA, Soslowsky LJ. Interplay of the static and dynamic restraints in glenohumeral instability. Clin Orthop Relat Res. 2002;1:48–57. doi: 10.1097/00003086-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Lippitt SB, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT, 2nd, Matsen FA., 3rd Glenohumeral stability from concavity compression: A quantitative analysis. J Shoulder Elbow Surg. 1993;2:27–35. doi: 10.1016/S1058-2746(09)80134-1. [DOI] [PubMed] [Google Scholar]
- 24.Sinha A, Higginson DW, Vickers A. Use of botulinum A toxin in irreducible shoulder dislocation caused by spasm of pectoralis major. J Shoulder Elbow Surg. 1999;8:75–6. doi: 10.1016/s1058-2746(99)90059-9. [DOI] [PubMed] [Google Scholar]
- 25.Jaggi A, Lambert S. Rehabilitation for shoulder instability. Br J Sports Med. 2010;44:333–40. doi: 10.1136/bjsm.2009.059311. [DOI] [PubMed] [Google Scholar]
- 26.Malone AA, Jaggi A, Calvert PT, Lambert SM, Bayley JI. Muscle patterning instability — classification and prevalence in a reference shoulder service. In: Norris TR, Zuckerman JD, Warner JJ, Lee QT, editors. Surgery of the Shoulder and Elbow:An International Perspective. USA: American Academy of Orthopaedic Surgeons; 2006a. section 7. [Google Scholar]
- 27.Boettcher CE, Cathers I, Ginn KA. The role of shoulder muscles is task specific. J Sci Med Sport. 2010;13:651–6. doi: 10.1016/j.jsams.2010.03.008. [DOI] [PubMed] [Google Scholar]


