Abstract
Purpose:
Distal clavicle fracture associated with complete coracoclavicular ligament disruption represents an unstable injury, and osteosynthesis is recommended. This study was performed (1) to retrospectively analyse the clinico-radiological outcomes of two internal fixation techniques, and (2) to identify and analyse radiographic fracture patterns of fracture that are associated with this injury.
Materials and Methods:
A total of 15 patients underwent osteosynthesis with either (1) acromioclavicular joint-spanning implants (Group 1, Hook plate device, n = 10) or (2) joint-sparing implants (Group 2, distal radius plate, n = 5); these were reviewed at a mean period of 26.1 months (12 to 40 months). Clinical outcomes were measured using Constant Score (CS), Simple Shoulder Test (SST), and Walch ACJ score (WS). Radiographs and ultrasonography were used to assess the glenohumeral and acromioclavicular joints, and the subacromial space. Preoperative radiographs were analyzed for assessment of fracture lines to identify radiographic patterns. Statistical analysis of the data was performed to determine any significant differences between the two groups.
Results:
The overall clinical outcome was satisfactory (CS 80.8, SST 11.3, WS 17.6) and a high union rate (93.3%) was observed. Radiographic complications (acromioclavicular degeneration and subluxation, hook migration, abnormal ossification) did not negatively influence the final clinical outcomes. Four distinct radiographic fracture patterns were observed. A statistically significant difference ( P < 0.05) was observed in the reoperation rates between the two groups.
Conclusions:
Internal fixation of this fracture pattern is associated with a high union rate and favorable clinical outcomes with both techniques. A combination of distal radius plate and ligament reconstruction device resulted in stable fixation and significantly lower reoperation rates, and should be used when fracture geometry permits (Types 1 and 2).
Design:
Retrospective review of a consecutive clinical case series.
Setting:
Level 1 academic trauma service, Public Hospital.
Keywords: Acromioclavicular joint, comminution, distal clavicle fracture, fracture patterns, hook plate, locking radius plate, ultrasound
INTRODUCTION
Distal clavicle fractures associated with partial and complete coracoclavicular ligament disruption are potentially unstable, and non-operative treatment of these fractures is associated with a high non-union rate.[1–3] Partial ligament disruptions (conoid or trapezoid) retain some inherent stability, and should be distinguished from complete dual ligament disruptions that result in an uncommon and highly unstable subgroup. Internal fixation of these fractures necessitates the use of acromioclavicular joint spanning implants (Clavicle Hook plate, Synthes, USA) that overcome distraction forces by subacromial leverage; however, subacromial/acromioclavicular joint encroachment with these implants is associated with subacromial pathology, and this may negatively influence the final outcomes.[4,5] To overcome the shortcomings of the joint-spanning implants, acromioclavicular joint-sparing implants (2.4 mm LCP® Distal radius plates, Synthes, USA) have been suggested.[6] Additionally, a combination of this implant with some form of coracoclavicular fixation using sutures/anchors/endobutton devices (TightRope™, Arthrex, FL, USA) has been recently described for use in the highly unstable fracture subgroup.[7] However, comparative clinico-radiological outcomes of the two techniques are lacking in literature.
The purpose of this study was (1) to analyze the overall and comparative clinico-radiological outcomes (radiographic and ultrasonographic) of surgical treatment of distal clavicle fractures associated with complete coracoclavicular ligament disruption, and (2) to identify and analyze radiographic patterns of fracture and comminution that are associated with this injury.
MATERIALS AND METHODS
The hospital records of all patients who were surgically treated for lateral clavicle fractures between 2005 and 2008 at three hospitals were retrospectively evaluated to identify the study group. Appropriate approvals and consent were obtained. Inclusion criteria for this study was defined as: (i) Acute, isolated, non-comminuted and comminuted fractures of the lateral clavicle, (ii) complete disruption of both coracoclavicular ligaments, confirmed on radiographs and at surgery, (iii) absence of concomitant or pre-existing subacromial pathology (rotator cuff tears, acromial undersurface degeneration), (iv) surgical treatment with either a joint-spanning implant alone (Group 1), or combination of a joint-sparing implant and coracoclavicular fixation with either endobutton device , suture anchor, or coracoid cerclage (Group 2) [Figures 1a and b], and (v) follow-up period of at least 6 months for radiographic evidence of union. Exclusion criteria was defined as: (i) partial disruption of the coracoclavicular ligaments at surgery, (ii) subacromial pathology (iii) concomitant injuries to the ipsilateral shoulder girdle, (iv) surgical treatment with any technique other than those described in the inclusion criteria, and (v) follow-up period inadequate for complete union.
Figure 1a.
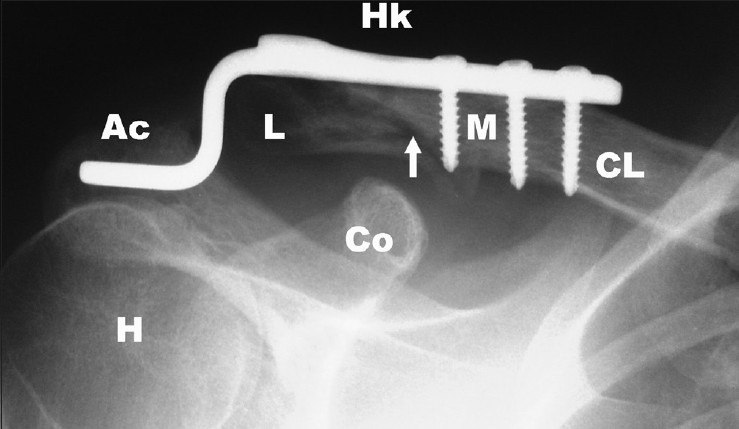
Surgical treatment of an unstable distal clavicle fracture with a joint-spanning implant (Group 1). (Hk: Hook plate, CL: Clavicle, M: Medial fragment, L: Lateral fragment, arrow: Fracture line, Ac: Acromion, H: Humeral head, Co: Coracoid process)
Figure 1b.
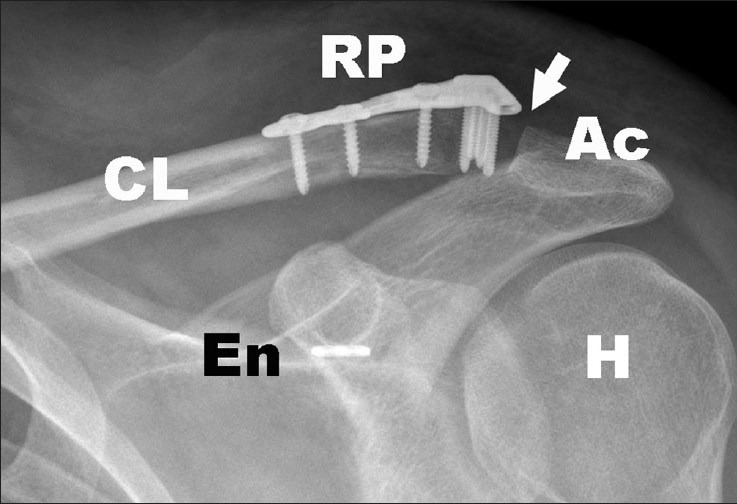
Surgical treatment of an unstable distal clavicle fracture with a joint-sparing implant and coracoclavicular ligament reconstruction using endobutton device (Group 2). (RP: Locking distal radius plate, arrow: Acromioclavicular joint, Ac: Acromion, CL: Clavicle, En: Endobutton, H: Humeral head)
The clinical records and operative notes were analyzed to identify patients that satisfied the criteria described above, and all other lateral clavicle fracture patients were excluded. Pre-operative radiographs of the study group were obtained and analyzed with a graphic analysis software; fracture lines were traced to identify involvement of the acromioclavicular joint, lateral fragment integrity, and presence/absence of comminution.
The follow-up clinical protocol included a subjective evaluation of pain and functional status by interview, evaluation of active and passive range of motion by clinical examination, and evaluation of muscle strength in elevation and external rotation using a portable dynamometer. Clinical acromioclavicular joint tests (tenderness and Paxinos sign) and rotator cuff tests (lag signs, bear-hug test, impingement signs) were used to evaluate these structures.[8–11] Clinical outcome measures included (i) Simple shoulder test, (ii) Constant and Murley shoulder score, and (iii) Walch acromioclavicular joint score.[12,13]
The follow-up radiographic protocol consisted of standardized radiographs that included a true glenohumeral anteroposterior view (neutral rotation, elbow by the side), and a weight bearing comparative cephalic-tilt view; these were analyzed for implant migration, acromioclavicular joint pathology (degeneration, instability), subacromial changes (degeneration, osteolysis), acromiohumeral interval measurement (normal interval = 7 mm or more), peri-coracoid changes (abnormal bone formation), and glenohumeral changes.[14] In addition, in those cases where implant had been previously removed, past radiographs were obtained from the records and individually analyzed as described above.
The follow-up ultrasonographic protocol included evaluation of the acromioclavicular joint, subacromial space, glenohumeral joint, bicipital groove and biceps long tendon, and suprascapular and spinoglenoid notches; ultrasound assessment was performed by a senior radiologist experienced in shoulder ultrasound.
Statistical analysis was performed using a statistical software (SPSS Inc, Chicago, USA) to determine mean values and range of measured parameters of the overall and implant specific groups. Significant differences between clinical and radiological parameters were determined using the non-parametric Mann-Whitney/Wilcoxon rank-sum test for numerical data, and the Fisher's Exact test for categorical data.
RESULTS
Fifteen patients (13 males, 2 females) were included in the study. The average age of the patients in the study group was 34.5 years (range, 20 to 57 years). The mechanism of injury was a direct impact to the ipsilateral shoulder sustained during a fall; in 8 patients, the fracture was sustained during a cycling-related sporting activity (competitive or recreational). Ten patients were operated using a joint-spanning implant (Group 1) and 5 were operated using a joint-sparing implant technique (Group 2).
The mean follow-up period was 26.1 months (range, 12 to 40 months). The overall and group-specific clinico-radiological outcomes and the types and distribution of fracture patterns are summarized in Table 1.
Table 1.
Overall and group.specific clinico.radiological outcomes and fracture patterns
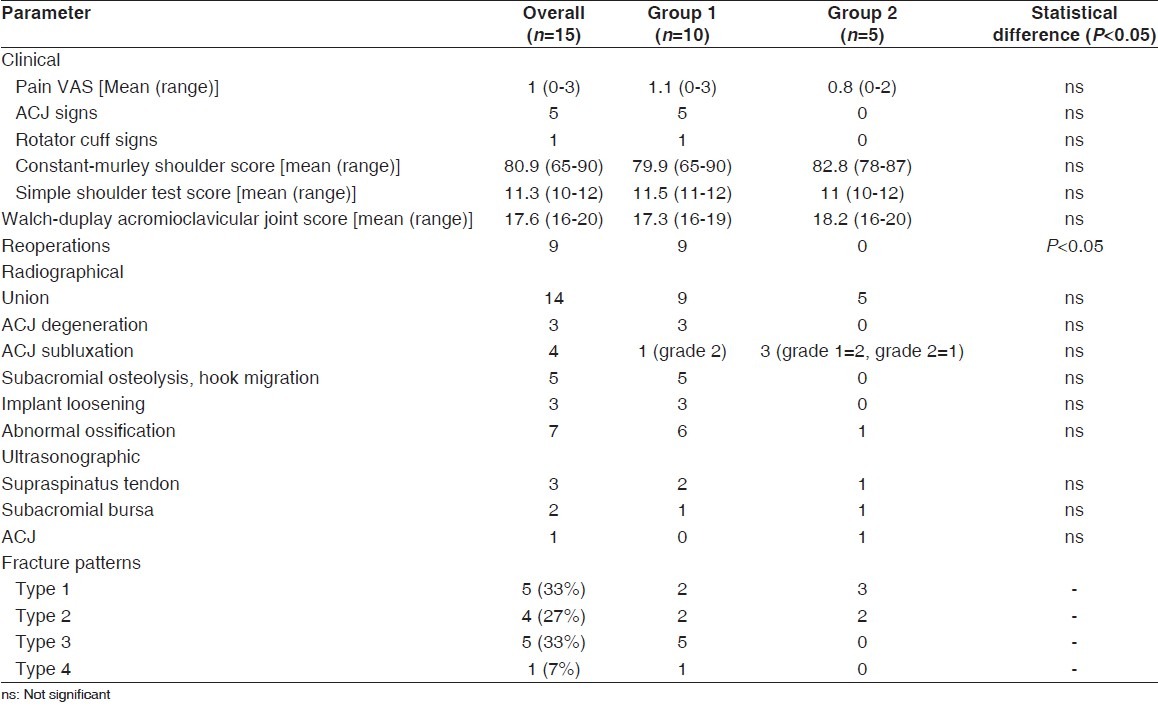
Clinical outcomes: The mean CS was marginally higher in Group 2, while the mean SST score was marginally higher in Group 1; none of these differences were statistically significant. Acromioclavicular joint signs were positive in half of the Group 1 patients, and in none in Group 2; however, the Walch scores for the acromioclavicular joint were not significantly different for the two groups. Return to pre-operative level of recreational and competitive sports was seen in approximately two-thirds of the patients of Group 1, and all patients of Group 2; this difference was not found to be statistically significant. Reoperation rates related to implant removal were significantly higher ( P < 0.05) in Group 1 patients (90 %) as compared to Group 2 (0%).
Radiographic outcomes [Figure 2a-d]: Radiographic union was observed in 93.3% of fractures (9 in Group 1, 5 in Group 2) with only one non-union with subsequent fragment resorption (Group 1). Radiographic acromioclavicular joint degeneration was present in 3 patients (Group 1); all 3 patients had a clinically symptomatic AC joint. Radiographic acromioclavicular joint superior subluxation was present in 4 patients (Group 1 = 1 patient, 10%; Group 2 = 3 patients, 60%); none of these were clinically symptomatic. Subacromial osteolysis and hook migration were seen in 5 patients (Group 1); implant removal was necessary in 4 of these 5 patients, and at final follow-up, resolution of the radiographic subacromial osteolytic lesions was observed. Signs of progressive implant loosening (screws and/or plate disengagement) were seen in 3 patients (Group 1).
Figure 2.
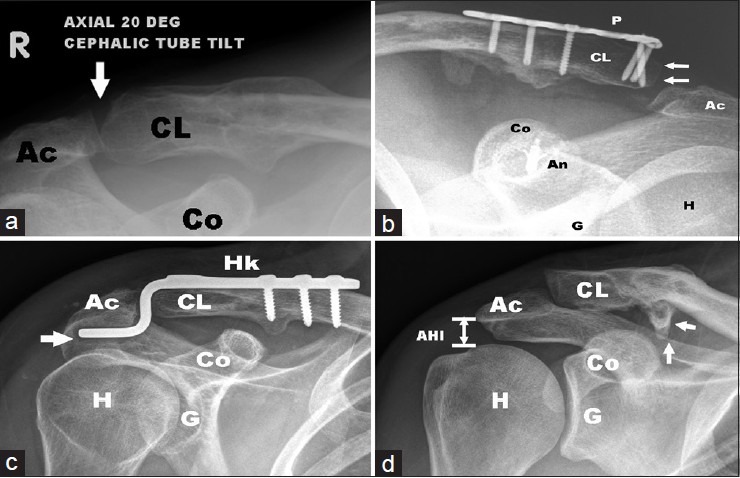
Radiographic outcomes of surgical treatment at follow-up are shown. (a) Acromioclavicular joint degeneration (arrow). (b) Acromioclavicular joint subluxation (arrows), (c) Hook migration and osteolysis of acromial undersurface (arrow), (d) Peri-coracoid ossification (arrows). (Ac: acromion, CL: clavicle, Co: coracoid, P: plate, An: suture anchor, G: glenoid, H: humeral head, Hk: hook plate, AHI: acromiohumeral interval)
The acromio-humeral interval was within the normal range in all 15 patients. Abnormal bone formation was present in 7 patients (Group 1 = 6, Group 2 = 1).
Ultrasonographic outcomes [Figure 3a and b]: Supraspinatus lesions were seen in 3 patients; these included partial articular-side tears (Group 1 = 1 patient, 10%; Group 2 = 1 patient, 20%), and supraspinatus bursal-side degenerative changes (Group 1 = 1 patient, 10%). None of these co-related with clinical signs. Acromioclavicular joint screw penetration was observed in 1 patient (Group 2); this penetration was not apparent on plain radiographs and the patient was asymptomatic at the final follow-up. No abnormalities were detected in the subacromial bursa on static ultrasound evaluation; dynamic testing revealed abnormal subacromial bursal "bunching" with arm abduction in 2 patients (Group 1 = 1, Group 2 = 1).
Figure 3.
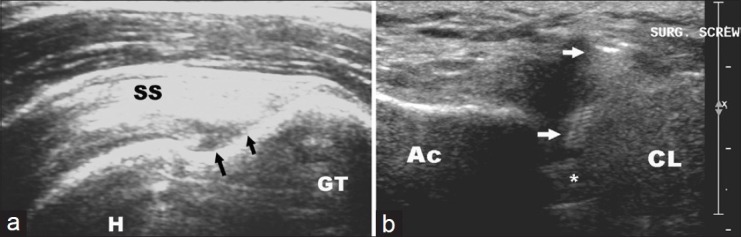
Ultrasonographic outcomes of surgical treatment at follow-up are shown. (a) Partial articular-surface supraspinatus tendon avulsion (Black arrows) (b) Screw penetration into the acromioclavicular joint (arrows). (GT: Greater tuberosity, H: Humeral head, SS: Supraspinatus, Ac: Acromion, CL: Clavicle, asterix: Acromioclavicular joint)
Radiographic evaluation of fracture comminution revealed 5 non-comminuted fractures (Group 1 = 2, Group 2 = 3), and 10 comminuted fractures (Group 1 = 8, Group 2 = 2). Analysis of the fracture lines and fragment cortices revealed repetitive patterns in the fracture geometry, and four types could be identified: (i) Type 1 pattern ( n = 5, 33%) involved a clean vertical or a short oblique type bicortical fracture line without any comminution [Figure 4a], (ii) Type 2 pattern ( n = 4, 27%) involved a zone of segmental comminution, between intact bicortical lateral and medial fragments [Figure 4b], (iii) Type 3 pattern ( n = 5, 33%) involved propogation of at least one fracture line into the juxta-articular cortex of the AC joint [Figure 4c] and (iv) Type 4 pattern ( n = 1, 7%) consisted of fracture line propogation into the acromioclavicular joint [Figure 4d].
Figure 4.
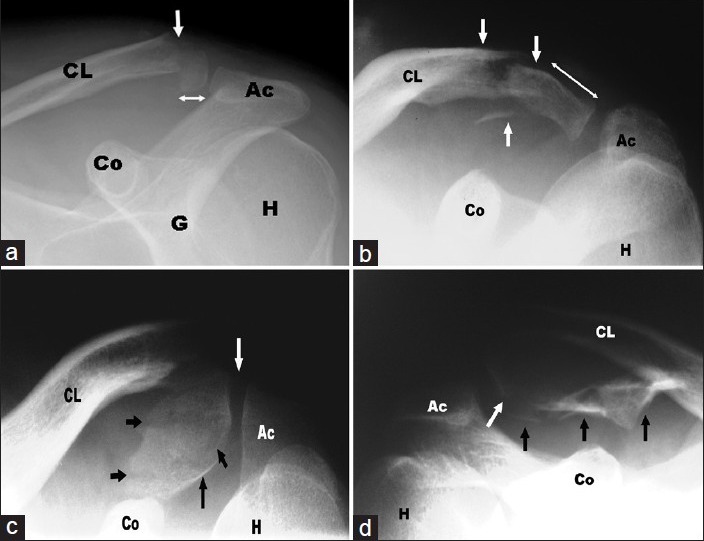
Radiographic fracture patterns: (a) Type 1, (b) Type 2, (c) Type 3, and (d) Type 4. (Ac: Acromion, CL: Clavicle, Co: Coracoid, G: Glenoid, H: Humeral head, arrows: Fracture lines)
DISCUSSION
The present study is the first study that describes overall and comparative outcomes (clinical, radiographic, and ultrasonographic) of surgical treatment of an uncommon lateral clavicular bony-ligamentous injury with joint-spanning and joint-sparing implants. In addition, four radiographic patterns of bone injury were identified to develop guidelines for choice of implants in these injuries.
Clinical outcomes and union rates after operative treatment of this injury are satisfactory, and this has been shown in other studies in literature.[3] In the present study, both types of implants resulted in satisfactory and comparable clinical outcome scores, irrespective of the radiographic outcomes. However, a significant difference in the reoperation rate for implant removal ( P < 0.05) in patients treated with a joint-spanning implant probably implies that a joint-sparing implant could be preferentially used whenever fracture geometry permits. Radiological outcomes, especially those associated with joint sparing techniques, have not been well documented in other studies. Subluxation of the acromioclavicular joint, (present in 60% of Group 2 patients) may be related to either concomitant injury to the acromioclavicular ligaments, or to a partial failure of the coracoclavicular ligament reconstruction; transfer of distraction forces to AC ligaments after fracture union may then induce gradual subluxation of this joint. This complication was rare in the other group, probably due to the joint spanning implant design; however, other radiological abnormalities like hook migration, subacromial osteolysis, implant loosening, and new bone formation were frequent.
The acromioclavicular joint spanning hook plate is a commonly used implant, and most studies have utilized this as the sole implant of choice.[15,16] Although clinical outcomes in these studies have been satisfactory, the effect of the subacromial hook on bursal tissues has been debated and use of the distal clavicle plate suggested.[6,7] By using ultrasonographic evaluation, this study demonstrated the safety of the joint-spanning hook plate in relation to rotator cuff and subacromial bursa. Persistent pain in the post-operative period probably resulted from acromial undersurface irritation; early plate removal after fracture union is recommended, and long-term clinical outcomes seem to be satisfactory after implant removal.
An important finding of this study is the grouping of the radiographic fracture patterns into four surgically relevant types. Types 1 and 2 are ideal indications for use of a joint-sparing implant; adequate bone stock in the distal fragment in these types will theoretically permit secure fixation across the fracture site. In types 3 and 4, inadequate distal fragment size may not permit secure bicortical fixation, thereby necessitating use of joint-spanning implants.
This study has limitations. The retrospective nature and small sample size does not permit identification of all possible fracture configurations, and statistical analysis may differ with larger numbers. However, the clinical results are similar to other literature studies that have analyzed joint-spanning implants.[15,16] Also, the current radiographic patterns described provide guidelines for implant choice, and are not intended to be used as a prognostic classification. We attribute the small size of the study group to the stringent inclusion and exclusion criteria that eliminated several other patients with lateral clavicle fractures, and this was necessary to obtain meaningful conclusions. Lateral clavicle fractures with complete disruption of the coracoclavicular ligaments should be regarded as a distinct entity that is perhaps biomechanically and prognostically different from similar fractures with partial ligament disruption.
CONCLUSIONS
Internal fixation of this unstable fracture pattern was associated with a high union rate. Overall clinical outcomes were favourable with both fixation techniques described. A combination of a locking distal radius plate with coracoclavicular ligament reconstruction resulted in stable fixation and significantly lower reoperation rates, and should be used preferentially in lesser comminuted fractures (Types 1 and 2).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: A case for fixation. Injury. 1992;23:44–6. doi: 10.1016/0020-1383(92)90125-c. [DOI] [PubMed] [Google Scholar]
- 2.Neer CS., 2nd Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963;3:99–110. doi: 10.1097/00005373-196303000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002-2003;61:32–9. [PubMed] [Google Scholar]
- 4.Chandrasen J, Badhe S, Cresswell T, De Beer J. The clavicular hook plate: Consequences in three cases. Eur J Trauma Emerg Surg. 2007;33:557–9. doi: 10.1007/s00068-006-6028-y. [DOI] [PubMed] [Google Scholar]
- 5.Charity RM, Haidar SG, Ghosh S, Tillu AB. Fixation failure of the clavicular hook plate: A report of three cases. J Orthop Surg (Hong Kong) 2006;14:333–5. doi: 10.1177/230949900601400320. [DOI] [PubMed] [Google Scholar]
- 6.Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: Early observations using a new technique. J Shoulder Elbow Surg. 2008;17:60–2. doi: 10.1016/j.jse.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Page RS, Bhatia DN. Non-comminuted lateral clavicle fractures associated with coracoclavicular ligament disruption: A new anatomical technique for superior fixation and stability. J Bone Joint Surg Br. 2010;92-B(SUPP I):214. [Google Scholar]
- 8.Barth J, Burkhart SS, De Beer JF. The bear-hug test: A new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006;10:1076–84. doi: 10.1016/j.arthro.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain. 1997;72:95–7. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 10.Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination.Part I: The rotator cuff tests. Am J Sports Med. 2003;31:154–60. doi: 10.1177/03635465030310011101. [DOI] [PubMed] [Google Scholar]
- 11.Walton J, Mahajan S, Paxinos A, Marshall J, Bryant C, Shnier R, et al. Diagnostic values of tests for acromioclavicular joint pain. J Bone Joint Surg Am. 2004;86:807–12. doi: 10.2106/00004623-200404000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–4. [PubMed] [Google Scholar]
- 13.Lippitt SB, Harryman DT, Matsen FA. A practical tool for evaluation of function: the Simple Shoulder Test. In: Matsen FA 3rd, Fu FH, Hawkins RJ, editors. The shoulder: A balance of mobility and stability. American Academy of Orthopedic Surgery: Rosemont (IL); 1993. pp. 501–18. [Google Scholar]
- 14.Weiner D, Macnab I. Superior migration of the humeral head. J Bone Joint Surg Br. 1970;52:524–7. [PubMed] [Google Scholar]
- 15.Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–64. doi: 10.1097/01.blo.0000203469.66055.6a. [DOI] [PubMed] [Google Scholar]
- 16.Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127:191–4. doi: 10.1007/s00402-006-0284-5. [DOI] [PubMed] [Google Scholar]


