Abstract
Background:
Chronic periodontitis is seen in majority of population and is responsible for the high tooth morbidity as well as mortality.
Materials and Methods:
One thousand and twenty-six subjects were selected by multistage stratified randomized sampling technique. They were examined in free dental camps organized in preselected rural areas by using community periodontal index of treatment need. The impact of known risk factors for periodontal disease, e.g., oral hygiene habits, age, gender, smoking, and pan + tobacco chewing, was also observed.
Results:
Deep pockets were observed in 52.7% of the subjects and 17.8% of the sextants. Shallow pockets were observed in 37.4% of the subjects and 36.4% of the sextants. Calculus had the highest score in 9.8% of the subjects and 43.8% of the sextants. None of the subjects and negligible number of the sextants was found to be having bleeding or healthy periodontium as the highest score.
Conclusion:
Periodontal disease severity was found to be increased with increasing age. Severity was also more in smokers and in the subjects using finger and powder to maintain their oral hygiene.
Keywords: Community periodontal index of treatment need survey, cross-sectional survey, index teeth, periodontitis, prevalence
INTRODUCTION
Chronic periodontitis is one of the common dental diseases with high tooth mortality as well as morbidity. Majority of the population is suffering from moderate grade of periodontitis that initiates at an early age, and clinical manifestations of the disease with noticeable morbidity start after 35 years of age, which if left untreated will ultimately result in loss of tooth. It needs planning to prevent periodontitis at a community level. Planing is based on baseline information about health-related states in terms of distribution as well as determinants. In the United States, several national oral health surveys have assessed periodontal health, e.g., the health examination survey (1960-1962) and National Health and Nutritional Examination Survey III (1988-1994).[1] No such national health survey has been done in India till date. Limited number of regional surveys have been done showing the prevalence of periodontal disease.[2–6]
Cross-sectional surveys are simple and economic. They need an appropriate study sample with clear-cut disease diagnostic criteria at a community level, e.g., chronic periodontitis can be diagnosed if on full/partial mouth examination, single site is affected from equal to or more than 2 mm of attachment loss.[1] Survey also provide useful information about the possible risk factors responsible for disease of interest and finally a hypothesis can be formulated regarding etiologic factors and prevention/intervention of disease. It also helps in deciding the requirement of infrastructure, manpower, and finances from health agencies.
Majority of the studies were cross-sectional surveys, which estimated the prevalence of periodontitis by using community periodontal index of treatment need (CPITN). This index was developed specially by joint committee of World Health Organization (WHO) and Federation Dentaire International (FDI) to evaluate the periodontal status and treatment need at a community level.[7] It was simple, inexpensive, and less time consuming because of examining a subset of index teeth. The index was also having certain limitation of not reflecting the true extent and severity of periodontal status in comparison to the indices measuring all the teeth. Present study was done with the following aims and objectives:
To estimate the prevalence of periodontal disease in subjects aged between 26 and 55 years and above in Meerut (Uttar Pradesh, India), using CPITN of periodontal disease assessment
To assess the periodontal treatment need of the population surveyed
To estimate the effects of age and gender, smoking, oral hygiene habits, and pan and tobacco chewing on the periodontal status of the study population.
MATERIALS AND METHODS
The study population was selected by multistage stratified randomized sampling technique. Sixteen villages were selected from Tehsil Meerut and 60-65 subjects of different age groups were examined among the participants after obtaining their written consent in one village. Information was collected using structured questionnaire. Demographic and socio-demographic variables were recorded including age, gender, address, religion, occupation, educational status, medical history, oral hygiene habits, and any other habit such as smoking, pan and tobacco chewing, etc.
Ten index teeth (17, 16, 11, 26, 27, 37, 36, 31, 46, and 47) were examined according to WHO guidelines using sterilized CPITN probe and a mouth mirror under good light source. A tooth was probed to determine pocket depth, detect calculus, and find bleeding response. The sites examined per tooth were mesial, midfacial, distofacial, mesiolingual/palatal, midlingual/palatal, and distolingual/palatal. Before each clinical session, the use of the WHO probe was calibrated by applying the probe to a thumb nailed with enough pressure to cause blanching. This was recognized as a pressure of approximately 20-25 g. After drying the tooth, the probe was gently inserted between tooth and gingiva to the full depth of the sulcus or pocket and the probing depth was read by observation of the position of the black band. Index teeth planned for extraction for any cause were excluded from CPITN scoring. When one or more index teeth were found to be missing or excluded during examination, substitute teeth were selected as per the laid-down norms.[7]
The dentition was divided into six sextants. Scoring was done on all index teeth. The scoring was done as follows: code 0, healthy; 1, bleeding on probing; 2, supra or subgingival calculus; 3, shallow pocket of 4-6 mm; 4, deep pocket of 6 mm or more; and X, a sextant with less than two teeth (excluded sextant). Population groups or individuals were allocated to the appropriate treatment needs category on the following basis: 0 = no treatment (code 0), I = improvement in personal oral hygiene (code 1), II = I + scaling (code 2 and 3), III = I + II + complex treatment (code 4).[7]
RESULTS
The sample of 10260 subjects (10260 sextants) consisting of 683 males and 343 females was divided into four groups: group I, 26-35 years; group II, 36-45 years; group III, 46-55 years; and group IV: 56 years and above. Data were collected both on the basis of percentage of individuals and percentage of sextants having different CPITN scoring and treatment needs. After calculating the mean values and standard deviation, Chi-square test and “Z” test were done to evaluate inter-group statistical significance of the observations.
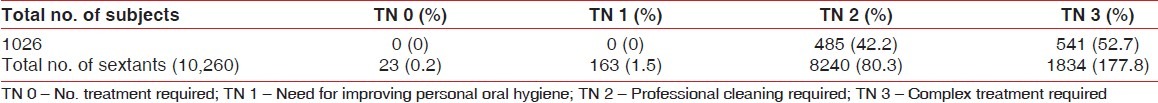
Deep periodontal pockets were recorded in 52.7% of the subjects and 17.8% of the sextants. Shallow pockets were observed in 37.4% of the subjects and 36.4% of the sextants. Calculus was found to be present in 9.8% of the subjects and 43.8% of the sextants. None of the subjects and negligible number of sextants was found to be having either bleeding or healthy periodontium (code 0) as the highest score [Tables 1 and 2]. Treatment need III was present in 52.7% of the subjects and 17.8% of the sextants. Treatment need II was observed in 47.7% of the subjects and 80.3% of the sextants. On the basis of sextants, scaling was the treatment needed in largest group of population [Table 3].
Table 1.
Age-wise and overall distribution of subjects with different periodontal status
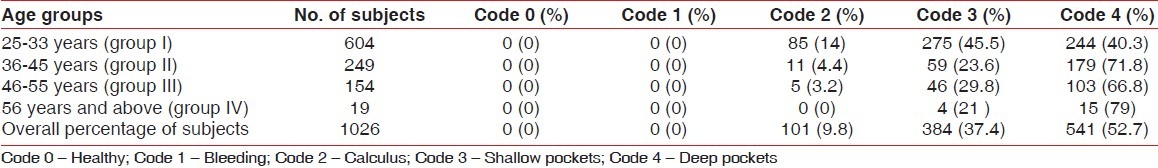
Table 2.
Age-wise and overall distribution of sextants with different periodontal status
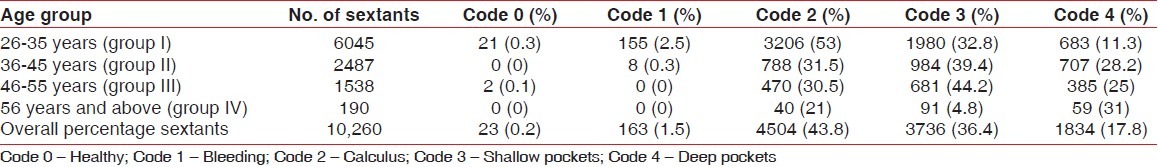
Table 3.
Overall estimation of treatment needs on the basis of percentage of subjects and percentage of sextants
Agewise changes have been observed in CPITN coding both on the basis of sextant as well as subjects. Deep pockets were observed to be maximum (31%) in group IV (56 years and above). It decreased with age as follows: 25% in group III (46-55 years), 28.2% in group II (36-45 years), and 11.3% in group I (25-35 years).
On inter-group comparison, most of the differences were statistically significant with “Z” values more than 1.96. The pattern of observation was nearly the same for different treatment need categories. Shallow pockets were observed to be maximum (48%) in group IV (56 years or older) and minimum (32.8%) in group I (26-35 years). Calculus was maximum (53%) in group I (26-35 years) and minimum (21%) in Group IV (56 years and above). The severity of the disease has been observed to increase with increasing age [Tables 1 and 2].
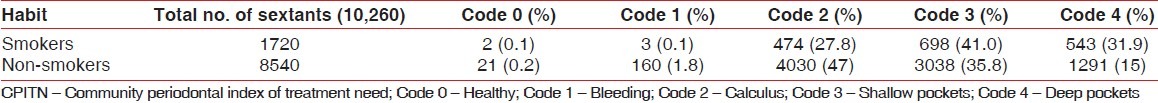
CPITN periodontal status was found to be nearly the same for male and female gender. The difference was not significant statistically. In smokers, the percentage of deep pockets was observed to be double in comparison to non-smokers. The difference was significant statistically with χ2 calculated (360.2) > χ2 tabulated (9.488) at “P” value 0.05. Shallow pockets were also found to be more in smokers than non-smokers. Calculus was less (27.8%) in smokers than non-smokers (47.1%) [Table 4].
Table 4.
Percentage of sextants with different CPITN codings on the basis of smoking
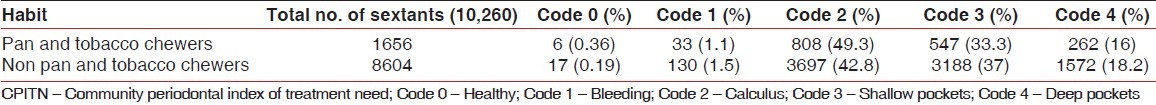
Deep pockets were more (27.1%) in individuals using finger and powder to maintain their oral hygiene in comparison to datun users (19.3%) and toothbrush and paste users (15.2%). The same pattern was observed for shallow pockets. The difference was statistically significant with “Z” values calculated more than tabulated for both disease severity and treatment needs [Table 5]. The difference in periodontal status of pan and tobacco users and non-chewers was small but significant statistically. Percentage of sextants with severe disease was little more (18.2%) in non-chewers than chewers (16%) [Table 6].
Table 5.
Percentage of sextants with different CPITN codings on the basis of oral hygiene habits
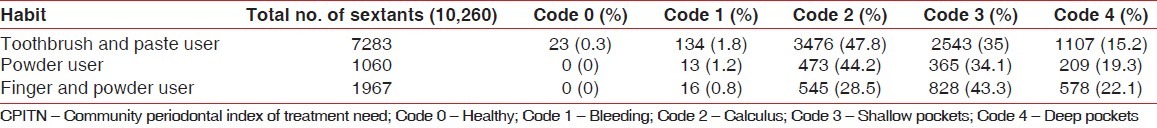
Table 6.
Percentage of sextants with different CPITN codings on the basis of pan and tobacco chewing
DISCUSSION
Overall estimation of CPITN code 4 and 3 on the basis of percentage of subjects was 52.7% and 37.4%, respectively. 90% of the subjects were found to be having chronic periodontitis. The same prevalence of periodontitis was reported from Bangladesh, Burkina Faso, Kenya, Libya, and Nepal.[8] The prevalence of periodontitis (90%) in the present study was different from the prevalence (27%) reported by Joseph and Cherry[3] in Trivandrum. The main reasons were the age of the population and oral hygiene habits. More than 50% of the population was below 30 years of age and 70% of the population studied was using toothbrush once daily and the rest 30% was using brush twice daily.
Jagedeesan et al.[4] demonstrated 45% overall prevalence in Pondicherry, which was also less in comparison to the present study. Pondicherry is a small union territory having small population with good infrastructure and health services, as reported by the authors. The large percentage of people affected from periodontitis in the present study may be because of improper oral hygiene maintenance with inferior health services and infrastructure at rural areas in district Meerut. Prevalence of periodontitis was different when data presentation was done on the basis of percentage of subjects and sextants affected from periodontal disease; 52.7% of the subjects and 17.8% of the sextants were observed to be having code 4 disease severity.
Prevalence of periodontal diseases is based on disease definition or diagnostic criteria, e.g., in CPITN the advanced disease (code 4) is identified if one of the sites examined (60 sites in 10 index teeth) has pocket depth 6 mm or more. The sextant as well as the subject will be graded with code 4. The difference indicates that out of six sextants, in each individual only one or two were having sites with pocket depth 6 mm or more.[9,10]
Presence of calculus (code 2) in 9.8% of the subjects and 43.8% of the sextants does not reflect a true picture. It can be attributed to the method of examination of CPITN, as it first assess the highest score, e.g., deep pocket depth, and if the response is positive, presence of calculus and bleeding are not examined.[9,10]
Age has been shown to be a risk factor for periodontal disease. Age itself does not affect the periodontal status but it is the cumulative effect of untreated disease reflecting the effect of the age on disease severity.[2,3,5] Nonsignificant difference of periodontal status was observed on the basis of gender for different codes.[3]
Deep pockets were double in smokers in comparison to non-smokers. Smoking now is an established factor responsible for increase in severity of periodontal disease. Smoking affects microbial colonization, host immune responses, collagen metabolism, etc.[3,5]
Disease severity was more in persons using finger and powder for oral hygiene maintenance. Finger and powder is not as effective as toothbrush and paste in maintenance of oral hygiene on a daily routine.[2,3]
More percentage of deep pockets in non pan and tobacco chewers than chewers can be explained on the basis of recession. Recession is expected to be more in tobacco and pan chewers. The parameter measured in CPITN is pocket depth which will be reduced because of recession. True severity of disease (clinical attachment loss) may be more.
CONCLUSION
Periodontal disease was found to be highly prevalent in the study population (90%) and the periodontal treatment needs increased with advancing age. Oral habits like smoking, and pan and tobacco chewing had a significant adverse effect on the periodontal health and treatment needs. Individuals who used toothbrush and paste for cleaning their teeth required significantly less treatment compared to those who used other methods.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Brown LJ, Loe H. Prevalence, extent, severity and progression of periodontal disease. Periodontol 2000. 1993;2:57–71. doi: 10.1111/j.1600-0757.1993.tb00220.x. [DOI] [PubMed] [Google Scholar]
- 2.Kaimenyi JT, Gururaja TR. Periodontal health status of adult population of Kenya and India. Indian Soc Periodontol. 1982;2:17–20. [PubMed] [Google Scholar]
- 3.Joseph PA, Cherry RT. Assessment of periodontal treatment needs in patients attending dental college hospital, Trivandrum. Indian Soc Periodontol. 1996;20:67–71. [Google Scholar]
- 4.Jagedeeran M, Rotti SB, Danabolan M. Oral health status and risk factors for dental and periodontal diseases among rural women in Pondicherry. Indian J Community Med. 2000;25:1. 31. [Google Scholar]
- 5.Joshi NV, Marawar PP. Periodontal health status of rural population of Ahmedabad district, Maharashtra using CPITN indicing system. J Indian Soc Periodontol. 2004;7:115–7. [Google Scholar]
- 6.Singh S, Gupta ND, Sharma AK, Bay A. Periodontal health status of rural and urban population of Aligarh district of Uttar Pradesh state. Indian Soc Periodontol. 2005;9:86–90. [Google Scholar]
- 7.Ainamo J, Brames D, Beagrie G, Cutress J, Martin J. Development of World Health Organization (WHO) Community Periodontal Index of Treatment Needs (CPITN) Int Dent J. 1982;32:281–91. [PubMed] [Google Scholar]
- 8.Pilot T, Barnes DE, Leclercq MH, McCombie BJ, Sardo Infirri J. Periodontal conditions in adults, 35-44 years of age: An overview of CPITN data in the WHO Global Oral Data Bank. Community Dent Oral Epidemiol. 1986;14:310–2. doi: 10.1111/j.1600-0528.1986.tb01079.x. [DOI] [PubMed] [Google Scholar]
- 9.Lewis JM, Murgan MV, Wright FA. The validity of CPITN scoring and presentation method for measuring periodontal conditions. J Clin Periodontol. 1994;21:1–6. doi: 10.1111/j.1600-051x.1994.tb00268.x. [DOI] [PubMed] [Google Scholar]
- 10.Benigeri M, Brodeur J-M, Payette M, Charbonneau A, Ismail AI. Community periodontal index of treatment needs and prevalence of periodontal conditions. J Clin Periodontol. 2000;27:308–12. doi: 10.1034/j.1600-051x.2000.027005308.x. [DOI] [PubMed] [Google Scholar]


