Abstract
Hereditary gingival fibromatosis is a rare benign oral condition characterised by slow and progressive enlargement of both maxillary and mandibular attached gingiva. It may develop as an isolated disorder but can feature along with a syndrome. A case of 12 year old female child who presented with generalised severe gingival overgrowth, involving both the arches and covering almost the entire dentition, and had all the teeth remaining invisible within the confinement of gingival tissues. The excess gingival tissue, in this non-syndromic case was removed by conventional gingivectomy using local as well as general anaesthesia. The post-operative result was uneventful and the patient appearance improved considerably. Good aesthetic result was achieved to allow patient to practice oral hygiene measures. After treatment regular recall visits are necessary in order to evaluate oral hygiene and stability of periodontal treatment.
Keywords: Gingival fibromatosis, gingivectomy, hereditary gingival fibromatosis
INTRODUCTION
Gingival diseases of genetic origin are uncommon conditions and their most common clinically evident form is known as hereditary gingival fibromatosis (HGF). It may occur singly or in association with other inherited syndromes.[1] This condition is also known as, elephantiasis gingivae, diffuse fibroma, familial elephantiasis, idiopathic fibromatosis; hereditary gingival fibromatosis, congenital familial fibromatosis.[2] It is inherited as autosomal dominant trait and has an incidence of 1:350000.[2,3] The condition does not manifest itself until after eruption of permanent teeth and is most commonly seen associated with the permanent teeth. This gingival overgrowth is due to excessive production of collagen in the gingival corium.[4] HGF is characterised by diffuse enlargement of gingiva that is slowly progressive, sometimes covering the major parts of, or the total, tooth surfaces.[2] This enlargement may project into the vestibule and floor of the mouth, interfere with normal mastication and even lip closure that make the speech difficult. The enlarged gingival tissue appears firm and pink with exaggerated stippling.[2,5] The gingival hyperplasia may be generalised (symmetric) or localised (nodular) can involve the buccal and lingual tissues of both maxillary and mandibular arches.[6] Local involvement mainly affects the maxillary tuberosities and lingual surfaces of lower molars[2,6] and is typically characterised by the presence of multiple large masses. The symmetric form, which is the most common type of disorder, results in uniform enlargement of the gingiva that is firm, dense, resilient, insensitive fibrous tissue that covers the alveolar ridges and extends over the teeth resulting in extensive pseudo pockets.[7] The degree of enlargement may vary from mild to severe and may be the same between the individuals of the same family.[6] HGF is seldom present at birth but may be noted at an early age. It usually begins at the time of eruption of permanent dentition but can develop with the eruption of primary dentition. If the enlargement is present before tooth eruption the dense fibrous tissue may interfere with or prevent the eruption.[8] The most common effects related to gingival overgrowth are diastema, mal-positioning of teeth, and prolonged retention of primary teeth.[7]
Depending on the extension of gingival enlargement, patients complain of functional and aesthetic problems. However, the gingival overgrowth does not usually affect the alveolar bone.[6] Although, this hereditary condition exhibit autosomal dominant mode of transmission, an autosomal recessive inheritance has also been reported.[9] A very rare and unusual case of unilateral HGF has also been reported along with localised aggressive periodontitis involving first molars.[10]
Gingival fibromatosis may be familial or idiopathic.[2] The familial variation may occur with a number of other inherited syndromes when it could be associated with some of the following; for e.g., Zimmerman Laband syndrome,[11,12] Murray Puretic drescher (juvenile hyaline fibromatosis),[13] Rutherfurd, Cross, Cowden syndrome, multiple hamartomas, tuberous sclerosis.[6,14]
HGF may be associated with other clinical manifestations such as hypertrichosis,[15] growth retardation,[16] hypopigmentation, mental deficiency,[17] epilepsy,[18] splenomegaly,[11] optic and auditory defects, cartilage and nail defects and dentigerous cysts.[4] The most common syndrome of HGF includes hypertrichosis, epilepsy and mental retardation, the two latter features, however are not present in all cases.[19]
Autosomal dominant forms of gingival fibromatosis, which are usually non-syndromic, have been genetically linked to the chromosome 2p21-p22 and 5q13-q22.[6,20] In modern times, a mutation in the Son of Sevenless 1(SOS-1) gene has been suggested as a possible cause of isolated (non-syndromic) gingival fibromatosis. However, no definite linkage has been established.[6] Recently, a locus for autosomal dominant HGF has been mapped to a region on chromosome,[2,20] although at least two genetically distinct loci seem to be responsible for this type of HGF.[21]
The histological features of HGF include moderate hyperplasia of a slightly hyperkeratotic epithelium with extended rete pegs. The underlying avascular stroma is almost entirely made up of dense collagen bundles with only few fibroblasts.[2,8]
It appears that the human gingival fibroblasts from hereditary fibromatosis tissue have characteristics of permanently activated fibroblasts. They grow faster and produce more collagen and fibronectin than fibroblasts from normal human gingiva (NGF),[22] partly under the autocrine control of TGF-beta reducing the proteolytic activities of HGF fibroblasts; which again favour the accumulation of extracellular matrix.[23] Elevated and prolonged expression of the proto-oncogene c-myc is implicated in deregulated cell growth and Tipton et al. have investigated the role of this oncogene in human gingival fibroblasts cell line and increase proliferation was related to elevated c-myc expression.[24]
This report presents the clinical features and the management of 12 year old female child with a severe variety of HGF.
CASE REPORT
A 12 years old female child reported to the Department of Periodontics, Government Dental College and Hospital, Nagpur complaining of gingival swelling, which caused severe compromise in her speech, mastication and aesthetics and led to considerable disfigurement of her facial profile, owing to the severity of gingival enlargement. The patient reported that the gingival enlargement started with the eruption of permanent dentition but progressed slowly to cover the entire permanent dentition. No single tooth was visible due to enlargement in anterior region whereas only occlusal portions of teeth were visible in posterior region. It was difficult to predict whether the positions of teeth were hampered due to massive gingival mass. However, the panoramic radiograph revealed normal bone height and tooth positioning.
The extra oral examination revealed an exaggerated convex profile with highly incompetent lips as the tissue bulge was protruding out of the mouth. The intra oral examination revealed generalised gingival overgrowth including both maxillary and mandibular arches extending into the vestibular areas [Figure 1]. The pink, leathery consistency tissue was hard on palpation and covered complete crowns of the entire dentition. The intra-oral examination confirmed that the patient used to masticate with assistance from the gums, however, no ulcerations were found on the occlusal surfaces of the enlarged tissue. A scanty amount of plaque and food debris was entrapped into the posterior teeth which were partially visible amongst the entire dentition with no significant inflammation present around them.
Figure 1.

Pre-operative view showing exuberance of gingival overgrowth
Routine blood investigations were done and values were found within normal range although haemoglobin values was slightly below normal range (8.5 gms%). The blood group examination was also done owing to the need for blood transfusion which was deemed necessary for maxillary arch gingivectomy after complete clinical evaluation. Based on the provisional diagnosis, an incisional biopsy was done and sent for histopathological examination to confirm the diagnosis.
The patient's medical history did not reveal any drug induced gingival enlargement or hormonal changes and exhibited no signs of hypertrichosis or mental retardation that could be associated with gingival hyperplasia.
Her family history was significant because her elder sister (15 years old) also revealed the presence of gingival enlargement but, was not willing for treatment as it was not causing any aesthetic and functional compromise. Her parents did not reveal any evidence of gingival overgrowth.
The enlarged tissue was removed by the external bevel gingivectomy under local anaesthesia quadrant wise only in the mandibular arch. Periodontal dressing was applied and chlorhexidine, haematinics and fortified B-Complex vitamins were prescribed for two weeks. For maxillary arch gingivectomy was performed under general anaesthesia. The patient was admitted to the hospital a day before the surgery where she was pre-medicated with requisite antibiotics and anti-inflammatory agents (Amoxicillin and Cloxacillin 500 mg, in divided doses 12 hourly and Piroxicam 20 mg, 8 hourly). There was significant blood loss during the surgery which was compensated by putting the patient on blood transfusion (2 pints of 350 ml each over 2 days). The post-operative instructions were reinforced and a custom made acrylic stent was placed against the surgical area containing periodontal dressing. The patient was discharged on the third day and was asked to continue with the medications till 7 days.
The histological evaluation of the section revealed moderately dense to highly dense collagenous connective tissue with collagen bundles arranged in haphazard manner. The connective tissue was relatively avascular with scanty inflammatory cells infiltrate. The overlying epithelium was hyper-plastic with enlarged rete ridges. The histopathological picture was suggestive of gingival fibromatosis [Figure 2].
Figure 2.
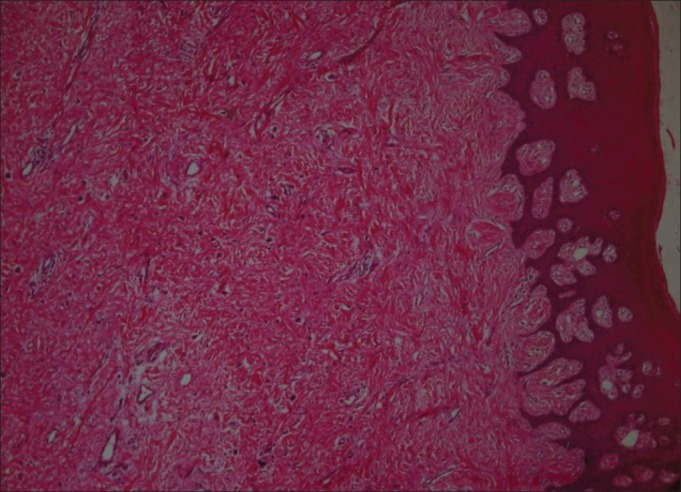
Stained section shows relatively thick parakeratinized epithelium with underlying connective tissue composed of interlacing thick bundles of collagen fibres, fibroblasts, few blood vessels and areas of chronic inflammatory cell infiltrate (H and E, 4×)
Post-surgical healing was uneventful. The stent contained periodontal dressing was removed after one week. The surgical area was profusely irrigated with Betadine and normal saline. Post-operative instructions were reinforced and the patient was recalled after two weeks, one month and three month intervals for post-surgical evaluation. Post surgically her facial profile improved dramatically and the patient was satisfied with the result [Figure 3].
Figure 3.

Post-operative view (6 weeks)
DISCUSSION
This article reports a symmetric case of hereditary gingival fibromatosis of severe variety. Although the genetic mechanism is not fully understood, majority of research workers have attributed this condition related with hereditary factors.[6,20,21] However, this case presented here can be considered a severe variant of HGF by virtue of exception not exhibiting any signs or symptoms relating to any syndrome.
The diagnosis was made on the basis of clinical presentation, family history and histopathological features.
HGF can be inherited as an autosomal dominant or autosomal recessive condition.[2,7] Bozzo and colleagues[25] in a four generation pedigree with 50 of 105 at risk family members developing gingival fibromatosis. In the present case, the gingival enlargement was a hereditary condition, probably autosomal dominant, due to its existence in siblings (sister), although her mother and father were phenotypically normal. Moreover it was unrelated to endocrine problems or use of medications.
Literature has shown contradictory evidence regarding the cellular and molecular mechanisms that led to gingival fibromatosis. Some authors report have reported an increase in the proliferation of gingival fibroblasts; whereas others have reported slower than normal growth.[14]
The gingival overgrowth usually begins at the time of eruption of permanent dentition[6,7] or less frequently with the eruption of primary dentition.[6] In present case, the patient reported that the gingival enlargement started at the time of eruption of permanent dentition, and hence there was delayed eruption of permanent dentition. The enlargement has influenced the alignment of her teeth resulting in diastema, malposition and delayed eruption [Figure 3]. The extent and severity of fibromatosis in this case has covered almost all teeth thereby causing difficulty in mastication and speech. The patient narrated that she often used to chew food with her gums and never used to practice oral hygiene measures. Although there was presence of pseudo pockets with concomitant material alba and scanty plaque, marginal inflammation was evident around the teeth.
The microscopic features of the present case were classic of gingival fibromatosis. The tissue showed excess amount of collagen in an avascular corium with overlying parakeratinized epithelium.[26]
The treatment need varies according to the degree of severity, when the enlargement is minimum, good scaling of the teeth and home care may be essential to maintain good oral health. The relative increase in the gingival mass contemplates the need for surgical intervention owing to the functional and aesthetic compromise. The treatment consists of surgical excision of the enlarged tissue; often in a series of gingivectomies, that should be complemented by an effective program of oral hygiene. Few studies have documented the use of carbon dioxide laser,[27] however, the most widely used method of removing large quantities of tissue is the conventional external bevel gingivectomy with gingivoplasty particularly when there are pseudo pockets and no attachment loss.[7,26] A periodontal flap procedure may be preferred if fibromatosis is accompanied with attachment loss and osseous defects.[6] Whenever possible the treatment should be performed after the complete eruption of permanent dentition. Recurrence is a common feature over varying periods. One report indicated that there is less chance of recurrence if the gingivectomy is delayed until permanent dentition is in place.[14] However slight recurrence was seen after 20 months.[26] In several reported cases, there was no recurrence in a period of 2 years,[6] 3 years,[28] or even 14 years follow up.[29] For the present case; gingivectomy under local anaesthesia was favoured treatment only in mandibular arch. However, general anaesthesia was preferred for maxillary arch gingivectomy because of the patient compliance and severity of gingival enlargement, There was no recurrence after one year of follow up.
CONCLUSION
HGF is a rare disorder characterised by varying degrees of attached gingival overgrowth. Aesthetic and functional compromises often demand surgical intervention; although recurrence cannot be predicted. Good aesthetic result was achieved without the recurrence of gingival overgrowth. After treatment regular recalls are necessary in order to evaluate oral hygiene and stability of periodontal treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza's Clinical Periodontology. 11th ed. St. Louis Missouri: Saunders; 2010. p. 40. [Google Scholar]
- 2.Varma BR, Nayak RP. Clinical Periodontology. 2nd ed. New Delhi: Arya (Medi) Publishing House; 2009. p. 177. [Google Scholar]
- 3.Eley BM, Soory M, Manson JD. Periodontics. 6th ed. China: Churchill Livingstone: Elsevier; 2010. pp. 113–4. [Google Scholar]
- 4.Doufexi A, Mina M, Ioannidou E. Gingival overgrowth in children: Epidemiology, pathogenesis and complications. A literature review. J Periodontol. 2005;76:3–10. doi: 10.1902/jop.2005.76.1.3. [DOI] [PubMed] [Google Scholar]
- 5.Lobao DS, Silva LC, Soares RV, Cruz RA. Idiopathic gingival fibromatosis: A case report. Quintessence Int. 2007;38:699–704. [PubMed] [Google Scholar]
- 6.Bansal A, Narang S, Sowmya K, Sehgal N. Treatment and two year follow up of a patient with hereditary gingival fibromatosis. J Indian Soc Periodontol. 2011;15:406–9. doi: 10.4103/0972-124X.92581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shafer WG, Hine MK, Levy BM. A Textbook of Oral Pathology. 4th ed. Philadelphia: W.B. Saunders; 1983. pp. 785–6. [Google Scholar]
- 8.Lindhe J, Karring T, Lang NP. Clinical Periodontology and Implant dentistry. 4th ed. Blackwell-Munksgaard, Singapore: Jaypee brothers; 2003. pp. 275–6. [Google Scholar]
- 9.Emerson TG. Hereditary gingival fibromatosis: A family pedigree of four generations. Oral Surg Oral Med Oral Pathol. 1965;19:1–9. doi: 10.1016/0030-4220(65)90207-0. [DOI] [PubMed] [Google Scholar]
- 10.Sandhu SP, Kakar V, Gogia G, Narula SC. Unilateral gingival fibromatosis with localised aggressive periodontitis (involving first molars): An unusual case report. J Indian Soc Periodontol. 2009;13:109–13. doi: 10.4103/0972-124X.55834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laband P, Habib G, Humphrey G. Hereditary gingival fibromatosis: Report of an affected family with associated splenomegaly and skeletal and soft tissue abnormalities. Oral Surg Oral Med Oral Pathol. 1964;17:339–51. doi: 10.1016/0030-4220(64)90506-7. [DOI] [PubMed] [Google Scholar]
- 12.Oikawa K, Cavaglia AM, Lu D. Laband syndrome: Report of case. J Oral Surg. 1979;37:120–2. [PubMed] [Google Scholar]
- 13.Sciubba JJ, Niebloom T. Juvenile hyaline fibromatosis (Murray-Puretic Drescher Syndrome): Oral and systemic findings in siblings. Oral Surg Oral Med Oral Pathol. 1986;62:397–409. doi: 10.1016/0030-4220(86)90289-6. [DOI] [PubMed] [Google Scholar]
- 14.James PL, Prasad SV. Gingival fibromatosis: Report of case. J Oral Surg. 1971;29:55–9. [PubMed] [Google Scholar]
- 15.Horning G, Fischer J, Barker B, Killoy WJ, Lowe JW. Gingival fibromatosis with hypertrichosis. A case report. J Periodontol. 1985;56:344–7. doi: 10.1902/jop.1985.56.6.344. [DOI] [PubMed] [Google Scholar]
- 16.Bhowmick SK, Gidvani VK, Retting KR. Hereditary gingival fibromatosis and growth retardation. Endocr Pract. 2001;7:383–7. doi: 10.4158/EP.7.5.383. [DOI] [PubMed] [Google Scholar]
- 17.Araiche M, Brode H. A case of fibromatosis gingivae. Oral Surg Oral Med Oral Pathol. 1959;12:1307–10. doi: 10.1016/0030-4220(59)90218-x. [DOI] [PubMed] [Google Scholar]
- 18.Ramon Y, Berman W, Bubis JS. Gingival fibromatosis combined with cherubism. Oral Surg Oral Med Oral Pathol. 1967;24:435–48. doi: 10.1016/0030-4220(67)90416-1. [DOI] [PubMed] [Google Scholar]
- 19.Gorlin RJ, Cohen MM, Levis LS. Syndromes of head and neck. 3rd ed. New York: Oxford University Press; 1990. pp. 847–55. [Google Scholar]
- 20.Hart TC, Pallos D, Bowden DW, Bolyard J, Pettanati MJ, Cortelli JR. Genetic linkage of hereditary gingival fibromatosis to chromosome 2p21. Am J Hum Genet. 1998;62:876–83. doi: 10.1086/301797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hart TC, Pallos D, Bozzo L, Almeida OP, Marazita ML, O’Connell JR, et al. Evidence of genetic heterogeneity for hereditary gingival fibromatosis. J Dent Res. 2000;79:1758–64. doi: 10.1177/00220345000790100501. [DOI] [PubMed] [Google Scholar]
- 22.Tipton DA, Howell KJ, Dobbous MK. Increase proliferation, collagen and fibronectin production by hereditary gingival fibromatosis fibroblast. J Periodontol. 1997;68:524–30. doi: 10.1902/jop.1997.68.6.524. [DOI] [PubMed] [Google Scholar]
- 23.Coletta RD, Almeida OP, Reynolds MA, Sauk JJ. Alteration in expression of MMP-1 and MMP2 but not TIMP-1and TIMP-2 in hereditary gingival fibromatosis is mediated by TGF-beta 1 autocrine stimulation. J Periodontal Res. 1999;34:457–63. doi: 10.1111/j.1600-0765.1999.tb02281.x. [DOI] [PubMed] [Google Scholar]
- 24.Tipton DA, Woodard ES, 3rd, Baber MA, Dabbous MK. Role of c-myc proto-oncogene in the proliferation of hereditary gingival fibromatosis fibroblast. J Periodontol. 2004;75:360–9. doi: 10.1902/jop.2004.75.3.360. [DOI] [PubMed] [Google Scholar]
- 25.Bozzo L, de Almedia OP, Scully C, Aldred MJ. Hereditarygingival fibromatosis. Report of an extensive four-generation pedigree. Oral Surg Oral Med Oral Pathol. 1994;78:452–4. doi: 10.1016/0030-4220(94)90037-x. [DOI] [PubMed] [Google Scholar]
- 26.Baptista IP. Hereditary gingival fibromatosis: A case report. J Clin Periodontol. 2002;29:871–4. doi: 10.1034/j.1600-051x.2002.290913.x. [DOI] [PubMed] [Google Scholar]
- 27.Miller M, Truhe T. Lasers in dentistry: An overview. J Am Dent Assoc. 1994;124:32–5. doi: 10.14219/jada.archive.1993.0034. [DOI] [PubMed] [Google Scholar]
- 28.Bittencourt LP, Campos V, Moliterno LF, Ribeiro DP, Sampaio RK. Hereditary gingival fibromatosis: Review of literature and a case report. Quintessence Int. 2000;31:415–8. [PubMed] [Google Scholar]
- 29.Gunhan O, Gardener DG, Bostanci H, Gunhan M. Familial gingival fibromatosis withunusual histologic findings. J Periodontol. 1995;66:1008–11. doi: 10.1902/jop.1995.66.11.1008. [DOI] [PubMed] [Google Scholar]


