Abstract
Context
Medicare covers chiropractic care, but the health-care community knows little about the demographic characteristics of older adults who use chiropractic services under the Medicare program. Researchers do not know the demographic composition of chiropractic users under Medicare, how the demographics of chiropractic use and rates of use have changed over time, and how users' characteristics vary geographically across the United States. An understanding of the demographics of chiropractic users can help chiropractic organizations, policy makers, and other stakeholders plan for an equitable allocation of resources to meet the chiropractic health-care needs of all of Medicare's beneficiaries.
Objective
The study intended to evaluate Medicare administrative data to determine (1) longitudinal trends in the demographic composition of the population that used chiropractic services, (2) longitudinal trends in rates of chiropractic use by demographic group, and (3) geographic variations in chiropractic use among minorities.
Design
The research team used a serial cross-sectional design to analyze administrative data for beneficiaries of Medicare during the years 2002 to 2008, using a 20% random sample that provided those beneficiaries' racial and geographical characteristics. The team restricted the study's actual sample to adults aged 65 to 99 and defined chiropractic users as beneficiaries who had at least one paid claim for chiropractic care on a date of service in an analyzed calendar year.
Outcome Measure(s)
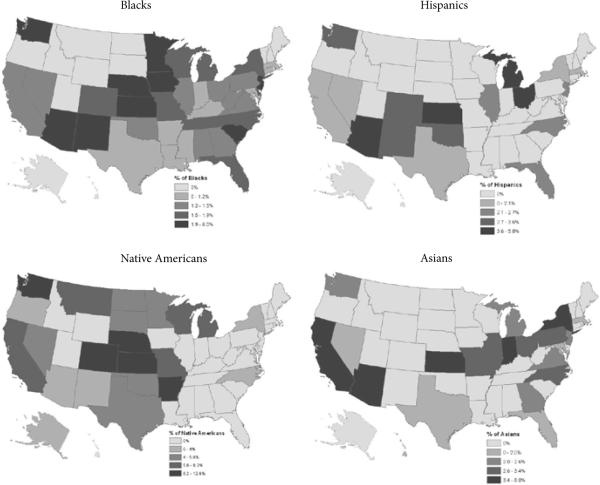
For each state in the United States and the District of Columbia for each of the 7 years studied, the team determined the number of chiropractic users in total and the number of users in selected demographic categories and calculated percentage estimates and averages for each category. The team analyzed 2008 data for rates of use within racial groups and for geographic variations in those rates and quantified variations in rates by state using the coeffcient of variation (CV). The team mapped race-specific rates for selected minorities, categorized by quintiles, to illustrate geographic variations by state.
Results
Analysis by beneficiary's race showed that the proportion of chiropractic users who were white hovered at 96% to 97% throughout the time period studied, while 1% to 2% were black. Each of the other racial categories comprised 1% or less of users, and the percentages showed little change over time. Rates among racial minorities showed greater geographic variation than did rates for whites. The greatest geographic variations in use by specific racial minorities occurred among Hispanics, Asians, and Native Americans.
Conclusion
The research team's results showed little longitudinal variation in the demographics of chiropractic use under Medicare but a striking difference in rates of use between whites and minorities, and substantial geographic variations in user rates among racial minorities. The research team's findings suggest the possibility that barriers may exist for minorities' access to chiropractic care. As minority populations in the US continue to grow, the health-care community can expect that any impact on population health that these barriers cause will grow as well.
Chiropractic users make up a large proportion of complementary and alternative medicine (CAM) users. As the US population ages and baby boomers become eligible for Medicare, many likely will continue to use CAM, including chiropractic care, for certain health-care needs, such as spinal pain. In 2005, Ness and colleagues reported the results of their survey, which indicated that 88% of adults over 65 years of age reported using CAM, and 46% of CAM users used chiropractic services.1 Among respondents to a survey of older adults residing in the community who reported using CAM, chiropractic services were among the most frequently used CAM therapies, at 16.3%.2 A survey of older adults enrolled in an insurance plan supplemental to Medicare found that among the 41% of respondents who used CAM, 20% used chiropractic services.3
Chiropractic Use Among Minorities
Several investigations have used data from the National Health Interview Survey (NHIS) to evaluate the use of CAM in general, and chiropractic in particular by racial category.4–7 Arcury et al focused on use among older adults and reported that the percentage of chiropractic users was 1.5% among blacks, 3.1% among Hispanics, and 0.6% among Asians in 2002.4 Graham et al reported that 8% of adult users of chiropractic services in 2002 were Hispanics and 2.7% were non-Hispanic blacks.6 Graham et al also found that minority adults who used CAM tended to be more highly educated and have higher incomes, but even after controlling for these sociodemographic factors, blacks were 29% and Hispanics 22% less likely to use CAM than whites. Barnes et al found that Native Americans and whites in 2007 used CAM at higher rates than did Asians and blacks.5 Su and Li reported that 3.05% of African Americans, 3.81% of Hispanics, and 4.39% of Asians used chiropractic care in 2007.7 In contrast, a cohort study that Carey and Garrett conducted in 2003 found that blacks with acute low back pain were only slightly less likely to see a chiropractor than a medical doctor,8 and Carey et al's survey in 2009 found that the proportions of blacks and whites with chronic back and neck pain who sought care from chiropractors were not significantly different.9
With regard to the use of chiropractic by older US adults in particular, multiple studies have found that older users are more likely to be white and female,10–13 and a survey in 2007 of chiropractic users under Medicare found that users were less likely to be African American or Hispanic.14 In their study in 2007 of a cohort of Mexican Americans aged 65 and older, Loera et al found the rate of use for Hispanics to be 2.4%.15 In a survey of participants in the Demonstration of Expanded Coverage of Chiropractic Services Under Medicare, which was conducted from 2005 to 2007, Hispanics comprised 4% of chiropractic users, blacks and Native Americans each comprised 2%, and Asians comprised less than 1%.12 The demonstration project's producers did not design it, however, to be nationally representative with regard to racial composition. The sample for the demonstration study included participants from only five states: Illinois, Iowa, Maine, New Mexico, and Virginia. The choice of New Mexico, with its large Hispanic population, may account for the relatively high proportion of older Hispanics reported to be chiropractic users. Similarly, relatively large populations of blacks in Virginia and Illinois may account for a higher percentage of chiropractic users among older black adults than the literature had reported previously.
Racial Disparities in Chiropractic Care
Back and neck pain are the most common conditions for which patients use chiropractic services,16 and the phenomenon of racial disparity in the care of patients with pain complaints is well established. The health-care needs of minorities with pain complaints are chronically under-served.17–20 A systematic review found that racial disparities in pain management were similar to disparities in other medical services.21 Most reported disparities in pain management, however, were differences in medical evaluations and treatments; less is known about racial disparities in choice of provider type. Researchers have reported lower rates of prevalence of back and/or neck pain for blacks and Hispanics as compared with whites,9,22,23 but relatively small differences in need do not justify gross disparities.
Treatment preferences, however, may account for racial disparities in the use of chiropractic. Patients who choose chiropractic tend to have a holistic philosophical orientation toward health.24,25 Phillips found that social networks influenced a patient's choice of a provider for care of low back pain; patients with close ties to family and friends were less likely to select a nontraditional provider.26 Researchers have observed racial differences in patients' reasons for choosing CAM,27 and racial differences in patients' preferences and beliefs may at least partially explain disparities. Availability of chiropractic services may also contribute to disparities in use. A study of the practices of minority chiropractors in Erie County, New York found smaller proportions of chiropractors and chiropractic patients in areas with relatively high minority populations.28 A possible contributing factor may be the fact that chiropractors are not eligible for inclusion in the National Health Service Corps, which contracts with providers to forgive student-loan debt in exchange for practice in medically underserved communities.
Chiropractic care is different from many other types of health care in that the spinal manipulation frequently employed in treatment usually involves frequent, close physical contact between doctor and patient. Such close contact requires development of a level of trust that racial tensions may impede. Older southern blacks, for example, who experienced the cruelty of segregation and continue to feel the effects of racial discrimination, may lack the level of trust required to allow themselves to be physically manipulated by a white chiropractor. From 1991 through 2009, blacks comprised less than 1% of chiropractors.29 In 2009 the racial composition of US chiropractors was 85% Caucasian (white), 2.6% Asian/Pacific Islander, 1% Hispanic, 0.9% black or African American, 0.4% Native American, and 10.2% other or mixed race.29 Many chiropractic colleges have instituted programs to attract minority students, but a lack of role models has hampered the effectiveness of efforts to recruit minorities.30
A patient should base his or her decision to use a health-care service on need and/or preference. For most of the pain conditions that chiropractors treat, such as nonspecific low back pain for which no gold standard of care exists, chiropractic care is not the only appropriate choice. Thus, use of chiropractic care is likely preference sensitive, and researchers have shown that patients' preferences for different treatment choices under Medicare vary geographically.31 Racial disparities in chiropractic services may thus be attributable to differences in local health-care cultures and practices.32 Favorable biases of communities may be particularly strong in communities where chiropractic colleges are located and maintain student-intern clinics in low-income and minority neighborhoods.
To prevent and correct racial health-care disparities, the Institute of Medicine has recommended that health-professional training programs include cross-cultural education.33 The American Osteopathic Society has recommended a nine-point approach for organizations to use for correction of health-care disparities, including (1) offering technical assistance to providers who are unable to eliminate disparity in the treatment of pain in their practices and (2) monitoring access to and coordination of quality pain care.20 The National Center for Complementary and Alternative Medicine (NCCAM) has affirmed its commitment to helping facilitate the development of an integrated health system in the United States, in which “no health disparities exist between the majority population and racial/ethnic minority populations.” NCCAM recommends the development of targeted, public-health educational programs focused on particular disease areas to reach minority and ethnic populations.34
Intent of Current Study
Medicare covers chiropractic care, but the health-care community knows little about the demographic characteristics of older adults who use chiropractic services under the Medicare program. Researchers do not know the demographic composition of chiropractic users under Medicare, how the demographics of chiropractic use and rates of use have changed over time, and how users' characteristics vary geographically across the United States.
An understanding of the demographics of chiropractic users can help chiropractic organizations, policy makers, and other stakeholders plan for an equitable allocation of resources to meet the chiropractic health-care needs of all of Medicare's beneficiaries. In the current study, the research team analyzed a large, nationally representative sample of claims data for Medicare over a 7-year period. The team examined (1) longitudinal trends in the demographic composition of the population who used chiropractic services, (2) longitudinal trends in rates of chiropractic use by demographic group, and (3) geographic variations in chiropractic use among minorities. (2) longitudinal trends in rates of chiropractic use by demographic group, and (3) geographic variations in chiropractic use among minorities.
METHODS
Design and Data Handling
The research team used a serial, cross-sectional design to analyze administrative data for selected demographic characteristics—age, sex, and race—of beneficiaries of Medicare who used chiropractic services. The team obtained the data used in this study under a data user agreement with the Centers for Medicare and Medicaid Services. The research team's institutional review board reviewed and approved the research plan. The team used Excel 2007 (Microsoft Corp, Redmond, Washington) to tabulate the data and analyzed it using Excel and Stata 11 (Statacorp, College Station, Texas). The team performed data mapping with ArcMap 10.0 (ESRI, Redlands, California).
Sampling
The research team merged claims data from Medicare's Carrier Files with beneficiaries' demographic data from Medicare's denominator files. Denominator files contain demographic and enrollment information, including self-reported race, for each beneficiary enrolled in Medicare during a calendar year. The carrier files provided 20% representative samples of all claims for Medicare Part B. Medicare randomly generates the 20% sample based upon the last digit of the beneficiary's social security number.
The research team restricted the study's sample to adults aged 65 to 99 (living as of January 1st of each year), for the years 2002 to 2008. The team restricted the analysis to claims records for services provided by chiropractic physicians practicing within the 50 US states and the District of Columbia. For the sake of simplicity, the research team categorized the District of Columbia as a state in the current study.
Medicare's records identify chiropractic claims by provider specialty code 35. The research team excluded from the analysis any disallowed claims and duplicate claims for the same patient, provider, procedure, and date of service. To reduce the likelihood of identification of individuals, the research team excluded beneficiaries who were older than 99 and suppressed any data fields with fewer than 11 observations. The research team aggregated the data to the state level for each year. For 2008, the number of beneficiaries in the 20% sample was slightly more than 5 million. The research team defined chiropractic users as beneficiaries who had at least one paid claim for chiropractic care on a date of service in an analyzed calendar year. The number of chiropractic users in the 20% sample ranged from a low of 326 000 in 2002 to a high of 364 000 in 2005.
Analyses
The research team examined the data both geographically and longitudinally for (1) the demographic composition of the chiropractic user population by state and year, and (2) rates of chiropractic use within demographic groups by state and year. The team determined the composition of the chiropractic user population by age, sex and race by dividing the number of chiropractic users per demographic category by the total number of chiropractic users. The team obtained rates of chiropractic use by dividing the number of chiropractic users by the total number of beneficiaries. Mean rates of use were calculated at both the state level and the individual level. The team estimated national total statistics by multiplying results from the 20% sample by a factor of five.
Because rates remained essentially stable over the time period studied, the research team analyzed only data for 2008 (the most recent year with available data) to evaluate for geographic variations in rates of use among demographic groups. The research team quantified variations in average rates of use by state using the coeffcient of variation (CV). The team mapped race-specific rates of use for selected minorities, categorized by quintiles, to illustrate geographic variations by state.
RESULTS
Demographic Composition of Chiropractic User Population
The estimated total number of chiropractic users increased over the study's time period from 1.6 million to 1.7 million (Table 1). Nationally, the basic demographic composition of the chiropractic user population showed little change from 2002 to 2008. The average age of chiropractic users remained just under 74 years; 41% to 42% of users were male. Analysis by race showed that the proportion of chiropractic users that were white hovered at 96% to 97% throughout the time period studied, while 1% to 2% were black. Each of the other racial categories comprised 1% or less of users and the percentage showed little change over time.
Table 1.
Trends in the Demographic Composition of the Chiropractic User Population Under Medicare
| Year | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|---|---|
| Total usersa | 1 630 950 | 1 689 035 | 1 767 655 | 1 821 430 | 1 803 055 | 1 759 615 | 1 721 160 |
| Mean age, yearsb | 73.8 | 73.8 | 73.8 | 73.8 | 73.9 | 73.9 | 73.9 |
| Composition of chiropractic usersb: | |||||||
| Male | 41.1 | 41.3 | 41.4 | 41.5 | 41.5 | 41.8 | 41.8 |
| White | 96.7 | 96.7 | 96.6 | 96.4 | 96.4 | 96.4 | 96.4 |
| Black | 1.6 | 1.6 | 1.7 | 1.7 | 1.7 | 1.7 | 1.7 |
| Asian | 1.0 | 0.9 | 0.9 | 0.9 | 1.0 | 1.0 | 1.0 |
| Hispanic | 0.9 | 0.9 | 0.9 | 0.9 | 0.8 | 0.8 | 0.7 |
| Native American | 0.4 | 0.4 | 0.4 | 0.4 | 0.5 | 0.5 | 0.5 |
| Other races | 0.5 | 0.5 | 0.5 | 0.5 | 0.6 | 0.6 | 0.7 |
National estimate, extrapolated from 20% representative sample.
Averages weighted by number of chiropractic users per state.
Rates of Chiropractic Use by Demographic Characteristics
Evaluation of chiropractic use by demographic characteristics revealed little variation over time (Table 2). By state, rates of use over the period varied little between men and women (men 7.5%, women 7.7%; individual level averages, 6.8% and 6.9%). User rates for both men and women ranged from less than 1% in the District of Columbia to over 20% in North Dakota. The highest rates of use for both men and women occurred in the northwestern United States, particularly the northern plains and prairie region. The lowest rates were in the southeastern United States and Hawaii. The range in rates of use and the pattern of geographic variations for white users were nearly identical to those observed for men and women generally. By state, use of chiropractic care averaged 8% among whites (individual level average, 7.4%). Rates of chiropractic use among racial minorities were substantially lower.
Table 2.
Average State-level Rates of Chiropractic Use by Demographic Characteristics, 2008
| Mean | States | SD | Minimum | Maximum | CV | |
|---|---|---|---|---|---|---|
| Men | 7.5% | 51 | 4.0% | 0.8% | 20.2% | 0.54 |
| Women | 7.7% | 51 | 4.3% | 0.8% | 21.2% | 0.56 |
| Whites | 8.0% | 51 | 4.1% | 1.7% | 21.2% | 0.51 |
| Blacks | 1.4% | 51 | 1.3% | 0.0% | 6.0% | 0.91 |
| Asians | 1.2% | 51 | 1.8% | 0.0% | 8.0% | 1.51 |
| Hispanics | 1.0% | 50 | 1.6% | 0.0% | 5.8% | 1.55 |
| Native Americans | 3.0% | 45 | 3.7% | 0.0% | 12.6% | 1.25 |
| Other races | 3.7% | 51 | 3.8% | 0.0% | 16.7% | 1.02 |
Abbreviations: SD = standard deviation; CV = coefficient of variation.
Mean user rate by state.
States with fewer than 11 beneficiaries not included.
Geographic Variation in Use of Chiropractic Among Racial Minorities
Geographic variations in chiropractic use in 2008 were typical of the entire time period studied (Figure 1). Rates of chiropractic use among racial minorities showed greater geographic variation than did rates for whites. The greatest geographic variation in use by specific racial minorities occurred among Hispanics (CV 1.55), Asians (CV 1.51) and Native Americans (CV 1.25).
Figure 1.
Geographic Variations in Rates of Chiropractic Use by Minorities
Blacks
By state, use of chiropractic care averaged 1.4% among blacks (individual level average, 1.6%). The research team had insufficient data to calculate user rates among blacks in 13 states. The state with the highest user rate for blacks was Iowa at 6%. Other states with higher rates of use among blacks were scattered across the country (Figure 1).
Asians
By state, use of chiropractic care averaged 1.2% among Asians (individual level average, 2.0%). The research team had insufficient data to calculate user rates for Asians in 30 states. User rates for Asians ranged up to a high of 8% in Kansas. For states other than Kansas, the research team observed the highest rates of use for Asians in Arizona, Indiana, New York, and California (Figure 1).
Hispanics
By state, use of chiropractic care averaged 1% among Hispanics (individual level average, 1.5%). The research team found no Hispanic beneficiaries in the sample in one state and insufficient data to calculate user rates for Hispanics in 34 states. User rates for Hispanics ranged up to a high of 6% in Kansas. For states other than Kansas, the research team observed the highest rates of use for Hispanics in Michigan, Ohio, and Arizona. Most states with sufficient Hispanic chiropractic users to calculate rates were in the Southwestern United States (Figure 1).
Native Americans
By state, use of chiropractic care averaged 3% among Native Americans (individual level average, 2.8%). The research team found no Native American beneficiaries in the sample in six states and insufficient data to calculate user rates for Native Americans in 29 states. User rates for Native Americans ranged up to a high of 12.6% in Kansas. After Kansas, the highest rates of use were in Arkansas, Nebraska, Colorado and Washington; the lowest rates were in states east of the Mississippi River (Figure 1).
Other Races
By state, use of chiropractic care by other races averaged 3.7% (individual level average, 3.7%). Insufficient data existed to calculate user rates for other races in 16 states. User rates for other races ranged up to high of 16.7% in South Dakota. The research team observed the highest rates of use for other races in the north-central plains and prairie states; the lowest rates were in the South and scattered across the country.
DISCUSSION
As every chiropractor knows, an African American man named Harvey Lillard became the very first chiropractic patient in 1895, under the care of DD Palmer in Davenport, Iowa. At the start of the 21st century however, older chiropractic users in Iowa and throughout the United States were overwhelmingly white, and race-specific rates of chiropractic users among minorities were substantially lower than those for whites.
Chiropractic users' average age remained static over the 7 years of the current study. Nearly equal proportions of men and women used chiropractic services, and the percentage of chiropractic users who were male rose only slightly during the years of the study. By far, whites had the highest rate of chiropractic use, followed in order of decreasing usage by other races, Native Americans, blacks, Asians, and Hispanics. Whites comprised 96% to 97% of chiropractic users, blacks 1% to 2%, and all other racial minorities 1% or less. In general, the study's results confirm the findings of previous studies that relatively low proportions of minority populations use chiropractic services under Medicare.
Because the racial mix of the general population varies significantly by geographic region, corresponding variations in the racial composition of chiropractic users are to be expected. However, the research team's evaluation of race-specific user rates illuminates racial disparities that are independent of the racial mix of populations in specific geographic locations. Throughout the United States, the team found that rates of chiropractic use by minorities were substantially lower than those for whites. Geographic variations in race-specific user rates were relatively lower for whites and blacks and relatively higher for Hispanics, Asians, and Native Americans. Some of the very highest rates of chiropractic use occurred among minority populations in Kansas.
The reason or reasons for racial disparities in use of chiropractic care are unknown, and the solutions are uncertain. The reported disparities do not necessarily reflect intentional obstructions to access. The disparities may be the result of patient-related factors such as (1) level of education, (2) socioeconomic status, (3) language barriers, (4) cultural beliefs, (5) preferences about health care, (6) proclivity for seeking care, or (7) racial differences in underlying rates of specific conditions such as low back pain. They also may be due to provider-related factors, such as (1) failure of chiropractic outreach efforts to target or connect with minorities, (2) lack of racial diversity among chiropractors themselves, (3) racial discrimination by chiropractors, or (4) lack of racial and ethnic sensitivity in chiropractors' communications with minority patients. Geographic variations in proportions of minorities' use of chiropractic services may also reflect local or regional modifications of the effect of racial differences on patients' preferences. Higher rates of chiropractic use by minorities in certain states may be due to the influence of a community's favorable attitudes toward chiropractic care that modifies racially aligned beliefs and preferences. Researchers should perform additional studies to determine the actual underlying reasons for the disparities in use of chiropractic care by minorities, and chiropractic physicians and professional organizations should explore ways of reaching out to minorities.
Limitations
The reported results are for Medicare's beneficiaries aged 65 to 99 years in the United States. Inaccurate entry of information on claim forms for Medicare may have limited the validity of the results of this claims-based research. Because the research team had aggregated the data in the analytic file to the state level, it performed no statistical modeling to predict chiropractic use by demographic characteristics of individual beneficiaries. For minorities in certain states and years, no chiropractic claims occurred, and the research team suppressed data in fields with fewer than eleven observations. Consequently, the team had insufficient data to allow calculation of rates for certain races and states, and therefore, the generalizability of findings to the national level is limited accordingly. This study did not include data on expanded chiropractic services provided under a Medicare demonstration project that was conducted from 2005 to 2007.12
CONCLUSIONS
The study results showed little longitudinal variation in the demographics of chiropractic use under Medicare but a striking difference in rates of use between whites and minorities, and substantial geographic variations in user rates among racial minorities. The findings suggest the possibility that barriers exist for minorities' access to chiropractic care. As minority populations in the United States continue to grow, the health-care community can expect that any negative impact on population health that these disparities cause will continue to grow as well.
Despite the research team's awareness of numerous possible causes, the reasons for these striking racial disparities in chiropractic use remain uncertain. Chiropractic use in older US adults is likely sensitive to racial differences in patients' preferences and beliefs. Future investigations should focus on geographic areas with large and diverse populations, investigate patients' preferences and their reasons for seeking care, and employ predictive modeling for chiropractic use based upon individual demographic characteristics. Chiropractic physicians, educational institutions, and professional organizations also should consider ways of making chiropractic care more accessible to minorities.
Acknowledgments
Dr. Whedon is supported by a research career development grant from the National Center for Complementary and Alternative Medicine, grant Number: 5K01AT005092-04. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Complementary & Alternative Medicine or the National Institutes of Health.
Footnotes
Author Disclosure Statement: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Ness J, Cirillo DJ, Weir DR, Nisly NL, Wallace RB. Use of complementary medicine in older Americans: results from the Health and Retirement Study. Gerontologist. 2005;45(4):516–524. doi: 10.1093/geront/45.4.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Najm W, Reinsch S, Hoehler F, Tobis J. Use of complementary and alternative medicine among the ethnic elderly. Altern Ther Health Med. 2003;9(3):50–57. [PubMed] [Google Scholar]
- 3.Astin JA, Pelletier KR, Marie A, Haskell WL. Complementary and alternative medicine use among elderly persons: one-year analysis of a Blue Shield Medicare supplement. J Gerontol A Biol Sci Med Sci. 2000;55(1):M4–M9. doi: 10.1093/gerona/55.1.m4. [DOI] [PubMed] [Google Scholar]
- 4.Arcury TA, Suerken CK, Grzywacz JG, Bell RA, Lang W, Quandt SA. Complementary and alternative medicine use among older adults: ethnic variation. Ethn Dis. 2006;16(3):723–731. [PubMed] [Google Scholar]
- 5.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008 Dec;(12):1–23. [PubMed] [Google Scholar]
- 6.Graham RE, Ahn AC, Davis RB, O'Connor BB, Eisenberg DM, Phillips RS. Use of complementary and alternative medical therapies among racial and ethnic minority adults: results from the 2002 National Health Interview Survey. J Natl Med Assoc. 2005;97(4):535–545. [PMC free article] [PubMed] [Google Scholar]
- 7.Su D, Li L. Trends in the use of complementary and alternative medicine in the United States: 2002–2007. J Health Care Poor Underserved. 2011;22(1):296–310. doi: 10.1353/hpu.2011.0002. [DOI] [PubMed] [Google Scholar]
- 8.Carey TS, Garrett JM. The relation of race to outcomes and the use of health care services for acute low back pain. Spine (Phila Pa 1976) 2003;28(4):390–394. doi: 10.1097/01.BRS.0000048499.25275.51. [DOI] [PubMed] [Google Scholar]
- 9.Carey TS, Freburger JK, Holmes GM, et al. Race, care seeking, and utilization for chronic back and neck pain: population perspectives. J Pain. 2009;11(4):343–350. doi: 10.1016/j.jpain.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davis MA, Sirovich BE, Weeks WB. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Serv Res. 2010;45(3):748–761. doi: 10.1111/j.1475-6773.2009.01067.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans MW, Jr, Ndetan H, Hawk C. Use of chiropractic or osteopathic manipulation by adults aged 50 and older: an analysis of data from the 2007 National Health Interview Survey. Top Integr Health Care. 2010;1(2):ID1.2005. http://www.tihcij.com/Articles/Use-of-Chiropractic-or-Osteopathic-Manipulation-by-Adults-Aged-50-and-Older-An-Analysis-of-Data-from-the-2007-National-Health-Interview-Survey.aspx?id=0000232. Published December 30, 2010. [Google Scholar]
- 12.Stason WB, Ritter G, Shepard DS, et al. Final Report: Evaluation of the Demonstration of Expanded Coverage of Chiropractic Services Under Medicare. Brandeis University; Waltham, MA: May 12, 2010. [Google Scholar]
- 13.Weigel P, Hockenberry JM, Bentler SE, et al. A longitudinal study of chiropractic use among older adults in the United States. Chiropr Osteopat. 2010 Dec;18:34. doi: 10.1186/1746-1340-18-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wolinsky FD, Liu L, Miller TR, et al. The use of chiropractors by older adults in the United States. Chiropr Osteopat. 2007 Sep;15:12. doi: 10.1186/1746-1340-15-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loera JA, Reyes-Ortiz C, Kuo YF. Predictors of complementary and alternative medicine use among older Mexican Americans. Complement Ther Clin Pract. 2007;13(4):224–231. doi: 10.1016/j.ctcp.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lawrence DJ, Meeker W. Chiropractic and CAM utilization: a descriptive review. Chiropr Osteopat. 2007 Jan;15:2. doi: 10.1186/1746-1340-15-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10(12):1187–1204. doi: 10.1016/j.jpain.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Mossey JM. Defining racial and ethnic disparities in pain management. Clin Orthop Relat Res. 2011;469(7):1859–1870. doi: 10.1007/s11999-011-1770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paulson M, III, Dekker AH. Healthcare disparities in pain management. J Am Osteopath Assoc. 2005;105(6)(suppl 3):S14–S17. [PubMed] [Google Scholar]
- 20.Paulson MR, Dekker AH, Aguilar-Gaxiola S. Eliminating disparities in pain management. J Am Osteopath Assoc. 2007;107(9)(suppl 5):ES17–ES20. [PubMed] [Google Scholar]
- 21.Cintron A, Morrison RS. Pain and ethnicity in the United States: a systematic review. J Palliat Med. 2006;9(6):1454–1473. doi: 10.1089/jpm.2006.9.1454. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976) 1987;12(3):264–268. doi: 10.1097/00007632-198704000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Plesh O, Adams SH, Gansky SA. Racial/Ethnic and gender prevalences in reported common pains in a national sample. J Orofac Pain. 2011;25(1):25–31. [PMC free article] [PubMed] [Google Scholar]
- 24.Coulehan JL. Chiropractic and the clinical art. Soc Sci Med. 1985;21(4):383–390. doi: 10.1016/0277-9536(85)90218-7. [DOI] [PubMed] [Google Scholar]
- 25.Coulter ID, Hurwitz EL, Adams AH, Genovese BJ, Hays R, Shekelle PG. Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine (Phila Pa 1976) 2002;27(3):291–296. doi: 10.1097/00007632-200202010-00018. discussion 297–298. [DOI] [PubMed] [Google Scholar]
- 26.Phillips RB. Physician Selection in Low Back Pain Patients [dissertation] University of Utah; Salt Lake City: 1987. [Google Scholar]
- 27.Chao MT, Wade C, Kronenberg F, Kalmuss D, Cushman LF. Women's reasons for complementary and alternative medicine use: racial/ethnic differences. J Altern Complement Med. 2006;12(8):719–720. doi: 10.1089/acm.2006.12.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bluestein P. Minorities and the chiropractic profession in Erie County, New York. J Am Chiropr Assoc. 1998;35(3):37–45. [Google Scholar]
- 29.Christensen MG, Kollasch MW, Hyland JK, et al., editors. Practice Analysis of Chiropractic 2010: a project report, survey analysis, and summary of chiropractic practices in the United States. National Board of Chiropractic Examiners; Greeley, CO: 2010. [Google Scholar]
- 30.Callender A. Recruiting underrepresented minorities to chiropractic colleges. J Chiropr Educ. 2006;20(2):123–127. doi: 10.7899/1042-5055-20.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wennberg JE, O'Connor AM, Collins ED, Weinstein JN. Extending the P4P agenda, I: how Medicare can improve patient decision making and reduce unnecessary care. Health Aff (Millwood) 2007;26(6):1564–1574. doi: 10.1377/hlthaff.26.6.1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bynum JP, Fisher ES, Song Y, Skinner J, Chandra A. Measuring racial disparities in the quality of ambulatory diabetes care. Med Care. 2010;48(12):1057–1063. doi: 10.1097/MLR.0b013e3181f37fcf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666–668. [PMC free article] [PubMed] [Google Scholar]
- 34.The National Center for Complementary and Alternative Medicine Special populations program: strategic plan to address racial and ethnic health disparities. [Accessed May 18, 2011];National Institutes of Health Web site. http://nccam.nih.gov/about/plans/health-disparities/. Published May 2002.