Abstract
Systematic evidence reviews support the efficacy of physical activity programs and multifactorial strategies for fall prevention. However, community settings where fall prevention programs occur often differ substantially from the research settings in which efficacy was first demonstrated. Because of these differences, alternative approaches are needed to judge the adequacy of fall prevention activities occurring as part of standard medical care or community efforts. This paper uses the World Health Organization Innovative Care for Chronic Conditions (ICCC) framework to rethink how fall prevention programs might be implemented routinely in both medical and community settings. We highlight examples of innovative programs and policies that provide fall prevention strategies consistent with the ICCC framework, and provide evidence where available on the effects of these strategies on processes and outcomes of care. We close by proposing a “no wrong door” approach to fall prevention and management, in which older adults who are found to be at risk for falls in either a medical or community setting are linked to a standard fall risk evaluation across three domains (physical activity, medical risks and home safety).
Keywords: accidental falls, fall prevention, chronic care model, implementation research, program evaluation
INTRODUCTION
Falls are defined as “an unexpected event in which participants come to rest on the ground, floor, or lower level.”1 About one-quarter of community-dwelling older adults fall every year,2 resulting in annual medical costs of at least $19 billion in the United States alone.3 While most falls do not result in injury, 5–10% of falls cause serious injuries such as major head trauma, lacerations, or fractures.4 Frequent falls predict nursing home placement5 and may cause older adults to restrict their daily activities.
Over the past 30 years, researchers have made remarkable progress in developing effective interventions to prevent and manage falls among older adults.6 Meta-analyses of randomized controlled trials show benefits of multifactorial fall prevention activities that include fall risk assessment, medical management, physical activity, and home modification.6, 7 Although very recent meta-analyses suggest that the magnitude of fall reduction generated by multifactorial programs may be smaller than previously thought,8–10 the benefits are still clinically important. Fall prevention and management (FP/M) activities are generally grouped into three categories based on the individual’s health and functional status. These include:
Health promotion strategies that encourage physical activity incorporating balance, flexibility, and strength training and home environment self-assessments for healthy older adults;
Multifactorial fall risk assessment and management, including medical review, adapted physical activity, and in-depth home assessment and modification, which are most appropriate for those at higher risk for falls due to underlying medical conditions or functional impairments; and
Minimizing the consequences of falls (e.g., use of hip protectors or medications to preserve bone mineral density), a strategy for those at the highest risk for falls and/or for those with a high underlying risk of injury if a fall occurs (e.g., patients with osteoporosis).
Implementing and sustaining these FP/M strategies is often difficult. In addition to fundamental issues in implementing research into practice,11 a major challenge specific to FP/M is that requisite activities can occur in multiple settings (e.g., outpatient medical care, senior center, home-based services), and be carried out by multiple provider types (e.g., physicians, nurses, social workers, rehabilitation therapists, physical activity instructors) over multiple intervals. Traditionally, each aspect of fall prevention has operated in relative isolation from other aspects. For example, community senior centers offer exercise classes, medical providers perform medical management, and home health agencies provide home safety evaluations with community agencies or private companies installing recommended equipment (e.g., grab bars). There is no guarantee that an older adult, coming into contact with any one of these services, will receive the others required to replicate activities shown to reduce falls in randomized, controlled trials.
It seems clear, then, that successful implementation of fall prevention activities in community settings requires a new approach involving a higher degree of coordination across settings and providers, as well as more effective collaboration with older adults and their caregivers. Given limited resources, it is unlikely that every possible combination of providers and sites for a new, linked set of fall prevention activities will be tested for efficacy in reducing falls in randomized, controlled trials. Therefore, we believe that a new set of concepts are needed to judge the adequacy of linked FP/M activities implemented in applied settings.
This article describes FP/M from a chronic care perspective to help researchers, practitioners, and policy makers better understand the strengths and weaknesses of existing programs and services in their geographic area. Falls are obviously acute events, but the underlying risk for falls is often a result of chronic problems. The collective result of these problems is a chronic state we call “fall risk.” Fall risk has important parallels with other chronic conditions, such as diabetes. In both cases, the risk of an acute event (a heart attack in the case of diabetes, or a fall in the case of fall risk), can be reduced through individuals and their providers taking action on the sources of risk, such as changing lifestyle or adopting risk-reducing interventions (e.g., medication for diabetes, or gait and balance training for fall risk).
WHO’S INNOVATIVE CARE FOR CHRONIC CONDITIONS (ICCC) FRAMEWORK
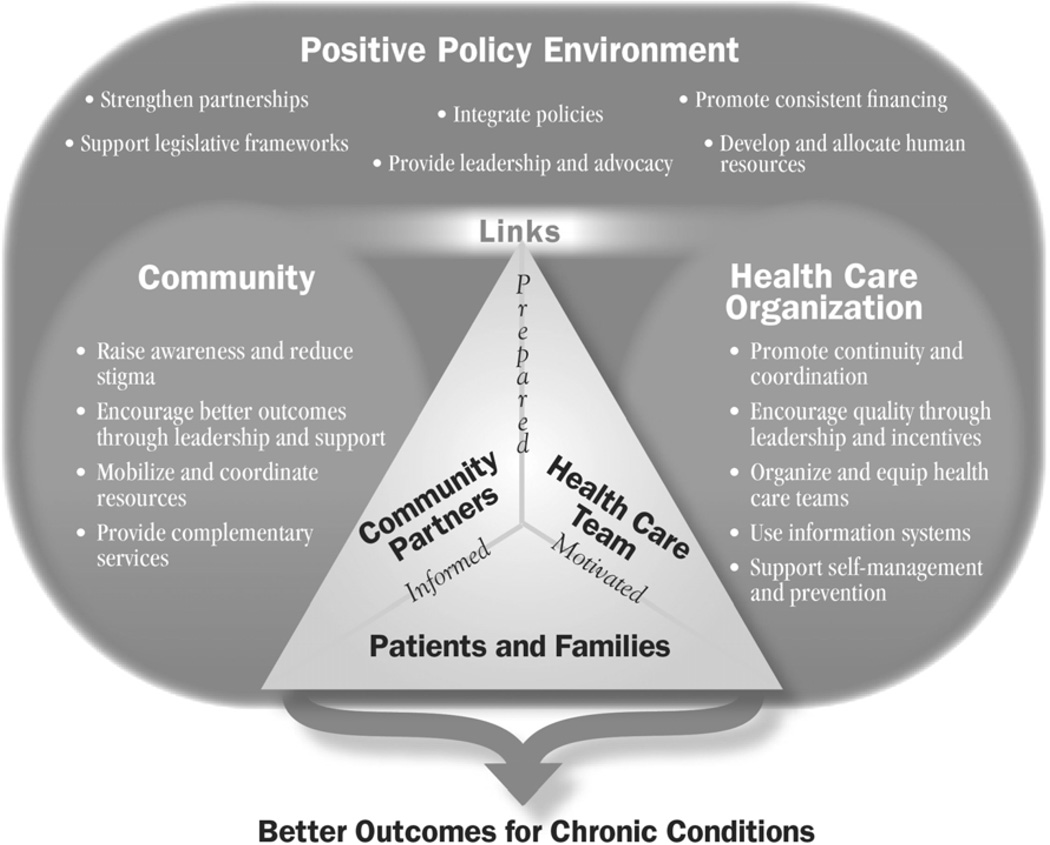
Given that the life-course of chronic health problems, such as fall risk, depends on an affected individual’s own actions and engagement with various providers, those involved in the solution must extend beyond the medical domain. The World Health Organization Innovative Care for Chronic Conditions (ICCC) model (Figure 1),12 based on the Chronic Care Model,13 provides a framework for rethinking chronic care service delivery by emphasizing changes in health care, encouraging consumer self-management activities, and improving linkages to community resources.14, 15 The value of describing collaborative FP/M through the ICCC approach lies in the model’s connections between ongoing activities at the consumer and provider levels to community-level participation as appropriate, operating in a supportive policy environment. Successful linkages can lead to older adults and caregivers who are informed, motivated, and prepared to manage and reduce fall risk. Below we describe examples of current FP/M efforts that are consistent with specific ICCC principles. Examples are taken from our collective experience and knowledge of the literature, supplemented by targeted literature searches using Medline, PubMed, Google, and Google Scholar. While we are most familiar with the status of fall prevention activities in the United States, we have included examples of relevant international activities as well.
Figure 1. The Innovative Care for Chronic Conditions Framework.
Image reprinted with permission of the World Health Organization.
Operating Principles in Health Care Organizations
Encourage quality through leadership and incentives
In the US, there are currently two major organized attempts to improve the quality of care for falls. First is the US Medicare system’s Physician Quality Reporting Initiative,16 in which physicians receive up to a 1.5% bonus if they report on certain quality measures, including screening patients for future fall risk at least once in 12 months.17 Additionally, the US Department of Veterans Affairs (VA), which provides health care for almost 5.5 million veterans nationally,18 recently added two new quality indicators related to falls within broader measures on the quality of geriatric care. These indicators, derived from the Assessing Care of Vulnerable Elders (ACOVE) project,19 include whether older veterans were asked about previous falls, and whether a basic evaluation for those with a fall history included the following items: circumstances of the fall; current medications; relevant chronic conditions; diagnostic plans/therapeutic recommendations; and documentation of action taken as appropriate. Although financial incentives are not currently tied to these indicators, results may serve to increase quality improvement activities geared toward veterans’ health on this key issue.
Organize and equip healthcare teams, support self-management and prevention, and promote continuity/coordination
The Assessing Care of Vulnerable Elders-2 (ACOVE-2) project exemplifies the ICCC principles of organizing healthcare teams and supporting patient self-management.20 ACOVE-2 was a clinical intervention to improve to the quality of care for community-dwelling adults aged 75 and older with falls, incontinence, and cognitive impairment.21 First, physicians received three hours of education on efficient approaches to addressing each condition. Patients were then screened for the target conditions prior to a scheduled visit. On the visit date, physicians received the results of the screen with a condition-specific structured visit form. This form guided physicians to 1) consider important elements of the history and physical examination, and 2) develop an intervention plan by suggesting diagnostic tests and treatments and enabling automatic orders for simple procedures (e.g., obtaining orthostatic blood pressures) to be completed by allied professionals. Consistent with ICCC principles, patient education materials including community resource information (e.g., physical activity programs) were available in examination rooms, supporting patient self-management. This practice redesign intervention demonstrated improved quality of care for falls compared to screening for falls without practice redesign.20 Building on this work, the ACOVEprime project is implementing additional quality improvement processes for falls and incontinence by collaborating more with allied professionals and (where available) using electronic health records for screening and documentation. Some practices in ACOVEprime are scheduling planned follow-up visits for patients with falls, consistent with the ICCC principle of improving continuity and coordination.
Use information systems
Previous research has suggested that emergency medical services22 and geographic information systems23 can be used to identify individuals with injurious falls and to monitor long term effects of prevention strategies. However, to our knowledge, data such as these have not been routinely used to date. More progress is being made in developing clinical information systems to support FP/M, both in the US and abroad.24
Operating principles in the community
Mobilize and coordinate resources
Interventions to prevent falls that mobilize and coordinate resources have been summarized in a recent Cochrane meta-analysis of five controlled before-after studies.25 An example is Australia’s Stay on your Feet program, which served 80,000 community elders and invoked multiple strategies for success, including community education, home hazard reduction, state and local policy development, social marketing approaches, and working with clinicians and other professionals.26 Using administrative data on fall-related hospitalizations, evaluators documented rates of self-reported falls among a sample of intervention and control participants, finding that relative reduction in fall rates was consistent with the significant reduction in fall-related hospitalizations.26 Program sustainability was assessed five years post-intervention showing evidence of changed practices among health professionals and older adults.27
Provide complementary services
Several programs have been developed that offer FP/M interventions complementing services traditionally offered by healthcare providers (e.g., medical management). Two key complementary services provided by community-based agencies include physical activity classes at various intensity levels and assessment and modification of the home environment to reduce hazards that may contribute to falls. Community physical activity programs focusing on muscle strengthening, flexibility, and balance retraining using trained health professionals offer the most promise for reducing falls.7 Program examples based on these elements and implemented in community-based settings include Tai Chi for older adults28 and FallProof.29 Evidence-based FP/M activities are also being implemented in senior centers through the Step by Step program.30,31 This program trained senior center staff to provide group education on fall risk reduction, physical activity, and monitoring interventions based on participants' fall risk assessments with evaluation results forthcoming.30
The home environment might be overlooked by health and social care providers when assessing for fall risk. However, up to three-quarters of falls by community elders occur in and around the home.32, 33 Home modification is defined as converting or adapting the environment to make performing tasks easier, reduce accidents, and support independent living within communities of choice.34 Such changes include removing hazards, adding special features or assistive devices, moving furnishings, changing where activities occur, and making renovations.35 Professional home assessment, consumer education, and installation of home modifications, as part of an integrated risk management intervention, has contributed to improved functioning, decreased fear of falls, and reduced incidence of falls in community elders.7, 36, 37 This is especially true for those with a history of falls.38 Implementing home modifications requires both behavioral and environmental changes by the older adult, including a willingness to alter the home and subsequently use devices and adaptations once present.
Raise awareness, reduce stigma, and encourage better outcomes through leadership and support
Raising awareness and reducing stigma associated with falls is critical because older adults may be unaware that preventive interventions can improve outcomes. Older adults may also not report their falls to others due to fear of being labeled as frail or disabled. Current research suggests that FP/M messages geared toward older adults should promote health and independence rather than focusing on reducing falls.39 The Archstone Foundation’s Senior Fall Prevention Programs Initiative is a recent effort to raise awareness, reduce stigma, and encourage better outcomes by funding two types of community projects. First, Archstone’s Program Expansion grants fund California-based community agencies that are expanding existing FP/M activities using evidence-based practices and collaborative partnerships. Second, their Coalition Development grants support multiple and diverse organizations to mobilize new and existing FP/M efforts and facilitate increased awareness of falls-related health promotion activities. Both of these projects are developing community-level leadership and support to improve health and functional outcomes, directly or indirectly, for community elders at risk for falls.
Operating principles in the policy environment
Many stakeholders who work to improve visibility and accessibility of FP/M programs and services are also engaged in policy activities at the local, state, and federal levels. The policy environment is distinct from community and health care organizations in the ICCC model as it can facilitate or impede activities carried out by organizations. Below are examples of entities generating a supportive policy environment for FP/M and the strategies they are employing.
Provide leadership and advocacy, strengthen partnerships, and integrate policies
Several entities provide leadership and advocacy to create and strengthen working partnerships within and between non-profit and governmental agencies at local and state levels – aging, health care, public health, social services, mental health, housing, transportation, emergency services, urban planning – and private business sectors, such as fitness clubs and new housing developers. The goal of these policy efforts is to integrate disparate FP/M policies and collectively achieve public health goals related to reducing fall incidence. Examples include local and state level leadership and advocacy through the California Fall Prevention Center of Excellence’s40 StopFalls Network and recent Fall Prevention Summit, and the US National Council on Aging’s FallsFree Coalition that involves interested organizations nationally.41 Their activities have focused primarily on harnessing organizational interest for FP/M, creating viable policy solutions that involve multiple stakeholders including older adult consumers, and outlining feasible implementation strategies – critical activities given that current efforts operate in a relatively decentralized environment. One small, but powerful policy activity resulting from leadership and advocacy efforts is the creation of local and state government proclamations for a Fall Prevention Awareness day or week, usually coinciding with the first week in autumn.42
US federal entities also have provided significant leadership, resulting in strengthened partnerships and policy changes. The US Administration on Aging (AoA) spearheaded the Evidence-Based Disease Prevention Grants Program in 2003, which funded an effectiveness study of A Matter of Balance program using a volunteer lay leader model43 and the Step by Step program described earlier. In 2006, AoA funded the state of Connecticut to expand the reach of Step by Step to eight additional US states to implement the Matter of Balance-Volunteer Lay Leader model program.
From the US legislative realm, two key policies that have been successfully integrated at federal, state, and local levels are the Fair Housing Amendments Act (1989) and the Americans with Disabilities Act (1990). Both acts champion the overall goal of minimizing barriers within the built environment. Mandates from these acts have been highly institutionalized, contributing to fall prevention through increased access to assistive devices (e.g., grab bars in bathrooms), promoting walkway accessibility (e.g., accessible routes within housing complexes and widened doorways), and removing physical and or structural barriers (e.g., adding curb cuts). In addition, some states have opted to increase accessibility and community walkability through other structural features, such as in-pavement lighting and audible crosswalks with countdowns, street medians, and clear signage. A key limitation of these policies is that they are restricted to public and or multi-use dwellings, leaving out the 75% of community elders who live in single-family homes, duplexes, and triplexes.44 Outside the US, New Zealand has developed an ambitious policy to prevent injuries from falls.45 Key interventions in their National Strategy include leadership building in fall prevention; education and dissemination; developing programs based on best practices; environmental modification; and resource reallocation.
Support legislative frameworks, develop and allocate human resources, and promote consistent financing
Policy-focused leadership and advocacy efforts, if successful, result in targeted legislation that creates consistent financing mechanisms and human resource development. In the US, state and national level legislation has been proposed to strengthen FP/M infrastructure, with the recent passage of bills in the state of Maine46 and the US Senate’s Safety of Seniors Act of 2007.47 These bills promote fall prevention education for various professionals, support research, program development and program evaluation related to falls, and (in the federal bill) a national public education campaign. Both bills were signed into law without appropriations, suggesting that the ICCC goal of promoting consistent financing for fall-related efforts has yet to be achieved in the US. Nonetheless, these legislative efforts suggest that the problem of falls is visible within the policy realm and continued advocacy efforts are critical.
CHALLENGES AND SOLUTIONS TO IMPROVING IMPLEMENTATION OF EVIDENCE-BASED FP/M STRATEGIES
The first challenge facing those who want to implement successful FP/M strategies is diffusing knowledge of the FP/M evidence base. Evidence supporting FP/M provides a basic understanding of the kinds of activities that decrease fall risk,6 but this knowledge may not have fully diffused into community settings. Perhaps for this reason, there is a remarkable diversity of ways in which fall prevention activities are delivered, with overlapping services in some areas and lack of availability of services in others.
The second challenge facing champions of FP/M is that providing FP/M involves multiple health and social services. FP/M’s complexity consists of different terminology, operations, administration, financing, and reimbursements across settings,48 justifying the comment that US health and social care delivery systems are a “nightmare to navigate.”49 Therefore, even successful linkages between FP/M activities, especially those linking medical care and social care, are inherently fragile. Recent studies of health care systems implementing ICCC principles on complex health problems (e.g., diabetes) suggest that the connection to community resources was generally the weakest link.50–52 Even if a case manager is assigned to an older adult with the sole responsibility to provide to care coordination (assessment, treatment planning, implementation, monitoring, and evaluation involving older adults, caregivers, and professional providers),53 a breakdown at any point of the care coordination process can leave older adults and their caregivers without needed FP/M supports.
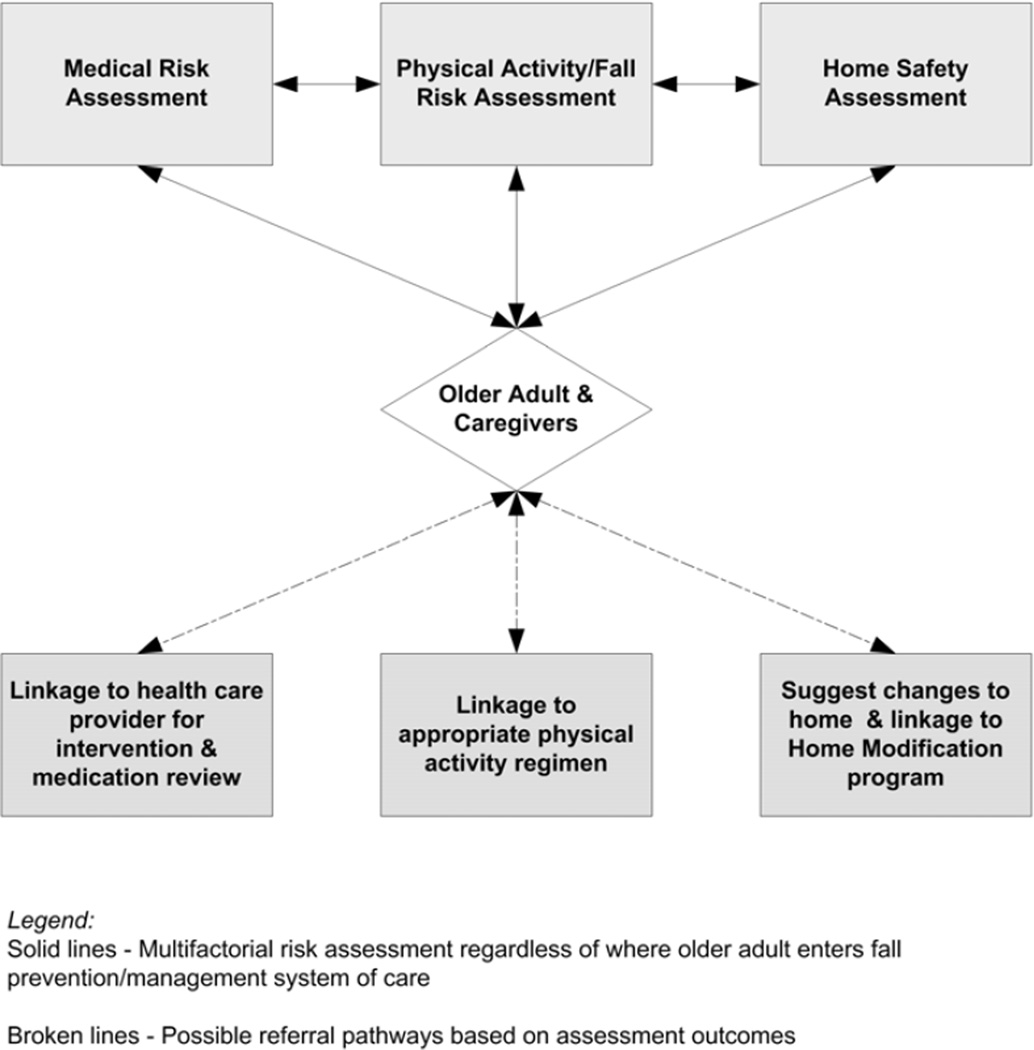
In this article, we have attempted to respond to the challenge of diffusing knowledge by synthesizing and describing the FP/M evidence base for a broad readership. To address mechanisms that can better coordinate FP/M activities, we now describe an application of the ICCC model through a “no wrong door” approach to FP/M (Figure 2). In this approach, older adults assessed as at risk for falls in one of the three areas (e.g., medical management) should receive at least a minimal evaluation in the other two areas (physical activity and home safety) regardless of where older adults enter a system of care involved in FP/M. In many cases, there are various professionals who can perform these activities, regardless of formal role. Ideally, engagement with a particular provider who becomes concerned about fall risk (e.g., a senior center physical activity instructor) would trigger linkages to an initial assessment in one particular area (e.g., physical activity/fall risk assessment), followed by referrals to the appropriate complementary providers (e.g., physician, occupational therapist) to complete the other necessary activities (e.g., medical risk assessment, home safety assessment). Trained providers completing various risk assessments would then connect older adults and caregivers directly to programs and services to address the identified risk in the most appropriate manner.
Figure 2. “No Wrong Door” approach to fall prevention and management.
Adapted from: Alkema, G. E. Technical Assistance Brief #2: Integrating Fall Prevention Components in Existing Organizational Structures. Los Angeles, CA: Fall Prevention Center of Excellence; 2006.
The success of a “no wrong door” approach depends heavily on changes at the consumer and provider levels. First, older adults need to be willing to participate in risk assessments and make suggested changes. Second, providers need to 1) be aware of FP/M assessment and intervention processes available within and outside their organization, 2) connect older adults to these programs in the health care and community service sectors by giving program information to older adults and/or caregivers and making referrals through intra-and inter-organizational channels, and 3) follow up to ensure that older adults in need are actually linked with the intended services. Follow up, in particular, is very important because fall risk assessments that are not tightly linked to appropriate interventions will not prevent falls, as suggested by a recent meta-analysis.9 Effective follow-up also depends on information systems that support each provider with the necessary information from other providers about an older adult’s fall risk just when key information is needed.54 Building an information system architecture that supports providers requires far more than technology – it requires thoughtful design of the information system in terms of content, integration with providers’ work routines, security, and delineation of responsibilities among providers.
Several organization and policy-level factors are also necessary to increase access and utilization of FP/M services including developing and enhancing program capacity built upon evidence-based models; training staff in appropriate risk assessments and interventions for a particular setting; educating older adults, caregivers, and various health and social care providers on FP/M activities; exploring reimbursement streams to ensure sustainability and cost-effectiveness of FP/M programs; and harnessing the power of collaborative partnerships to achieve these goals. Similar to implementing other evidence-based practices,55 contextual issues such as staffing ratios, face-to-face time with older adults, organizational resources and culture, leadership styles, and internal evaluation processes can greatly promote or hinder linkage and care coordination processes. Specific policy-level solutions to increase the use of FP/M activities in the US include instituting Medicare coverage for FP/M assessments,16 expanding the role of Medicare managed care plans in offering exercise classes as part of their benefit packages,56 and providing tax credits for adults of all ages who make home modifications to support safe aging in place.
CONCLUSIONS
For chronic health conditions that particularly affect older adults, evidence to support FP/M efforts is among the strongest. Adopting this evidence routinely, however, requires appropriate implementation and sustainability strategies that involve multiple providers collaborating with older adults and caregivers. Practitioners, policy-makers, and researchers could improve awareness and diffusion of FP/M activities by inventorying the local landscape of fall prevention champions, services and policies, and then evaluating to what extent ICCC and “no wrong door” principles are used in standard practice. Once practitioners identify quality gaps in current fall prevention activities, they can determine the causes of these gaps, implement an improvement program targeting a particular quality gap, and then evaluate the improvement program to see if it has improved the quality of care and generated better outcomes for older adults.57 It takes a village of stakeholders working together to prevent falls and reduce fall risk, tasks that no one stakeholder can accomplish alone. In that spirit, we hope that readers will write responses to this article with information about additional innovative programs and policies to support fall prevention activities throughout the world.
Acknowledgments
The authors appreciate the comments of the anonymous peer reviewers on a previous version of this manuscript.
Funding
David Ganz is supported by the UCLA Claude Pepper Older Americans Independence Center funded by the National Institute on Aging (5P30AG028748). Gretchen Alkema is supported by the VA Greater Los Angeles HSR&D Center of Excellence for the Study of Healthcare Provider Behavior (Postdoctoral Fellowship #TPP 65-007) and Fall Prevention Center of Excellence funded by the Archstone Foundation. Shinyi Wu is supported by the Roybal Center for Health Policy Simulation funded by the National Institute on Aging (5P30 AG024968-02).
Footnotes
A previous version of this manuscript was prepared for the National Institutes of Health/National Academy of Sciences workshop on the social determinants of adult health and mortality, Washington, DC, USA, May 22, 2007. The opinions expressed in this article are the authors and do not necessarily reflect the views of the National Institutes of Health or the National Academy of Sciences.
Competing interests
The authors have no competing financial interests with respect to this manuscript.
Copyright permission
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in IP and any other BMJPGL products to exploit all subsidiary rights, as set out in our license.
REFERENCES
- 1.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53:1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 2.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297:77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 3.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141–158. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 5.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 6.Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. Br Med J. 2004;328:680. doi: 10.1136/bmj.328.7441.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003 doi: 10.1002/14651858.CD000340. CD000340. [DOI] [PubMed] [Google Scholar]
- 8.Campbell AJ, Robertson MC. Rethinking individual and community fall prevention strategies: a meta-regression comparing single and multifactorial interventions. Age Ageing. 2007 Nov;36(6):656–662. doi: 10.1093/ageing/afm122. [DOI] [PubMed] [Google Scholar]
- 9.Gates S, Fisher JD, Cooke MW, Carter YH, Lamb SE. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. Bmj. 2008 Jan 19;336(7636):130–133. doi: 10.1136/bmj.39412.525243.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beswick AD, Rees K, Dieppe P, et al. Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet. 2008 Mar 1;371(9614):725–735. doi: 10.1016/S0140-6736(08)60342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grol RP. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39:II-46–II-54. doi: 10.1097/00005650-200108002-00003. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Preparing a Health Care Workforce for the 21st Century: The Challenge of Chronic Conditions. Geneva, Switzerland: 2005. [Google Scholar]
- 13.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 14.Boyd CM, Boult C, Shadmi E, et al. Guided Care for multimorbid older adults. Gerontologist. 2007;47:697–704. doi: 10.1093/geront/47.5.697. [DOI] [PubMed] [Google Scholar]
- 15.Pearson ML, Wu S, Schaefer J, et al. Assessing the implementation of the Chronic Care Model in quality improvement collaboratives. Health Serv Res. 2005;40:978–996. doi: 10.1111/j.1475-6773.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tinetti ME, Gordon C, Sogolow E, Lapin P, Bradley EH. Fall-risk evaluation and management: challenges in adopting geriatric care practices. Gerontologist. 2006;46:717–725. doi: 10.1093/geront/46.6.717. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare and Medicaid Services. [Accessed December 24, 2007];Physician Quality Reporting Initiative. http://www.cms.hhs.gov/PQRI/
- 18.United States Department of Veterans Affairs. [Accessed December 27, 2007];Fact Sheet: Facts About the Department of Veterans Affairs. http://www1.va.gov/opa/fact/vafacts.asp.
- 19.Wenger NS, Shekelle PG. Assessing care of vulnerable elders: ACOVE project overview. Ann Intern Med. 2001;135(8 Pt 2):642–646. doi: 10.7326/0003-4819-135-8_part_2-200110161-00002. [DOI] [PubMed] [Google Scholar]
- 20.Wenger NS, Roth CP, Shekelle PG, et al. A controlled trial of a practice-based intervention to improve primary care for falls, incontinence, and dementia. J Gen Intern Med. 2005;20(S1):52. [Google Scholar]
- 21.Reuben DB, Roth C, Kamberg C, Wenger NS. Restructuring primary care practices to manage geriatric syndromes: the ACOVE-2 intervention. J Am Geriatr Soc. 2003;51:1787–1793. doi: 10.1046/j.1532-5415.2003.51565.x. [DOI] [PubMed] [Google Scholar]
- 22.Wofford JL, Heuser MD, Moran WP, Schwartz E, Mittelmark MB. Community surveillance of falls among the elderly using computerized EMS transport data. Am J Emerg Med. 1994;12:433–437. doi: 10.1016/0735-6757(94)90055-8. [DOI] [PubMed] [Google Scholar]
- 23.Yiannakoulias N, Rowe BH, Svenson LW, Schopflocher DP, Kelly K, Voaklander DC. Zones of prevention: the geography of fall injuries in the elderly. Soc Sci Med. 2003;57:2065–2073. doi: 10.1016/s0277-9536(03)00081-9. [DOI] [PubMed] [Google Scholar]
- 24.Liaw ST, Sulaiman N, Pearce C, et al. Falls prevention within the Australian general practice data model: methodology, information model, and terminology issues. J Am Med Inform Assoc. 2003;10:425–432. doi: 10.1197/jamia.M1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McClure R, Turner C, Peel N, Spinks A, Eakin E, Hughes K. Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database Syst Rev. 2005 doi: 10.1002/14651858.CD004441.pub2. CD004441. [DOI] [PubMed] [Google Scholar]
- 26.Kempton A, van Beurden E, Sladden T, Garner E, Beard J. Older people can stay on their feet: final results of a community-based falls prevention programme. Health Promot. Int. 2000;15:27–33. [Google Scholar]
- 27.Barnett LM, Van Beurden E, Eakin EG, Beard J, Dietrich U, Newman B. Program sustainability of a community-based intervention to prevent falls among older Australians. Health Promot Int. 2004;19:281–288. doi: 10.1093/heapro/dah302. [DOI] [PubMed] [Google Scholar]
- 28.Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in oder adults: A randomized controlled trial. J Gerontol Med Sci. 2005;60:187–194. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 29.Rose DJ. Promoting functional independence in older adults at risk for falls: The need for a multidimensional programming approach. J Aging Phys Act. 2002;10:1–19. [Google Scholar]
- 30.Baker DI, Gottschalk M, Bianco LM. Step by Step: integrating evidence-based fall-risk management into senior centers. Gerontologist. 2007;47:548–554. doi: 10.1093/geront/47.4.548. [DOI] [PubMed] [Google Scholar]
- 31.Murphy TE, Tinetti ME, Allore HG. Hierarchical models to evaluate translational research: Connecticut collaboration for fall prevention. Contemp Clin Trials. 2008 May;29(3):343–350. doi: 10.1016/j.cct.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Norton R, Campbell AJ, Lee-Joe T, Robinson E, Butler M. Circumstances of falls resulting in hip fractures among older people. J Am Geriatr Soc. 1997;45:1108–1112. doi: 10.1111/j.1532-5415.1997.tb05975.x. [DOI] [PubMed] [Google Scholar]
- 33.Kochera AS. Falls among Older Persons and the Role of the Home: An Analysis of Cost Incidence and Potential Savings from Home Modifications. Washington, DC: AARP; 2002. [PubMed] [Google Scholar]
- 34.Pynoos J, Tabbarah M, Angelelli J, Demiere M. Improving the delivery of home modifications. Technol Disabil. 1998;8:3–14. [Google Scholar]
- 35.Pynoos J, Nishita CM, Perelman L. Advancements in the home modification field: A tribute to M. Powell Lawton. J Housing Elderly. 2003;17:105–116. [Google Scholar]
- 36.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. Br Med J. 2002;325:128–133. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–816. doi: 10.1111/j.1532-5415.2006.00703.x. [DOI] [PubMed] [Google Scholar]
- 38.Lord SR, Menz HB, Sherrington C. Home environment risk factors for falls in older people and the efficacy of home modifications. Age Ageing. 2006;35(S2):ii55–ii59. doi: 10.1093/ageing/afl088. [DOI] [PubMed] [Google Scholar]
- 39.Hughes K, van Beurden E, Eakin EG, et al. Older persons' perception of risk of falling: implications for fall-prevention campaigns. Am J Public Health. 2008 Feb;98(2):351–357. doi: 10.2105/AJPH.2007.115055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rose DJ, Alkema GE, Choi IH, Nishita CM, Pynoos J. Building an infrastructure to prevent falls in older Californians: The Fall Prevention Center of Excellence. Ann N Y Acad Sci. 2007;1114(1):170–179. doi: 10.1196/annals.1396.035. [DOI] [PubMed] [Google Scholar]
- 41.NCOA Center for Healthy Aging. Falls Free: Promoting a National Falls Prevention Action Plan: National Action Plan. Washington, DC: National Council on Aging; 2005. [Google Scholar]
- 42.British Columbia Ministry of Health. [Accessed April 23, 2008];Province Proclaims Falls Prevention Week for Seniors. http://www2.news.gov.bc.ca/news_releases_2005-2009/2007HEALTH0133-001417.htm#.
- 43.MaineHealth Partnership for Healthy Aging. [Accessed December 24, 2007];A Matter of Balance Volunteer Lay Leader Model. http://www.mmc.org/workfiles/mh_PFHA/MOBRepReport.pdf.
- 44.Pynoos J, Nishita CM, Cicero C, Caraveillo R. Aging in place, housing, and the law. The Elder Law Journal. 2008;16:101–129. [Google Scholar]
- 45.Dyson HR. [Accessed April 24, 2007];Preventing injury from falls: implementation plan 2006–2010. http://fallsimplementation.acc.co.nz/files/ACC2565.pdf.
- 46.LD 1707. [Accessed April 28, 2008];Resolve, Directing the Commissioner of Health and Human Services To Develop Strategies To Keep Senior Citizens Safe from Falls. http://janus.state.me.us/legis/LawMakerWeb/summary.asp?ID=280019739.
- 47.S.845. [Accessed April 28, 2008];A bill to direct the Secretary of Health and Human Services to expand and intensify programs with respect to research and related activities concerning elder falls. http://thomas.loc.gov/cgi-bin/bdquery/z?d110:SN00845:@@@L&summ2=m&.
- 48.Stone RI. Long-Term Care for the Elderly with Disabilities: Curent Policy, Emerging Trends, and Implications for the Twenty-First Century. Milbank Memorial Fund; 2000. Aug, [Google Scholar]
- 49.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, D.C: National Academy Press; 2001. [PubMed] [Google Scholar]
- 50.Hroscikoski MC, Solberg LI, Sperl-Hillen JM, Harper PG, McGrail MP, Crabtree BF. Challenges of change: A qualitative study of Chronic Care Model implementation. Annals of Family Medicine. 2006 Jul 1;4(4):317–326. doi: 10.1370/afm.570. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. American Journal of Managed Care. 2005;11:478–488. [PMC free article] [PubMed] [Google Scholar]
- 52.Pearson ML, Wu S, Schaefer J, et al. Assessing the implementation of the Chronic Care Model in quality improvement collaboratives. Health Services Research. 2005;40(4):978–996. doi: 10.1111/j.1475-6773.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moxley DP. The practice of case management. Thousand Oaks, CA: Sage Publications; 1989. [Google Scholar]
- 54.Elson RB, Faughnan JG, Connelly DP. An industrial process view of information delivery to support clinical decision making: implications for systems design and process measures. J Am Med Inform Assoc. 1997 Jul-Aug;4(4):266–278. doi: 10.1136/jamia.1997.0040266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rycroft-Malone J, Harvey G, Seers K, Kitson A, McCormack B, Titchen A. An exploration of the factors that influence the implementation of evidence into practice. Journal of Clinical Nursing. 2004;13(8):913–924. doi: 10.1111/j.1365-2702.2004.01007.x. [DOI] [PubMed] [Google Scholar]
- 56.Group Health Cooperative. [Accessed March 29, 2007];Senior Fitness Programs. http://www.ghc.org/classesAndEvents/seniorFitness.jhtml.
- 57.McQueen L, Mittman BS, Demakis JG. Overview of the Veterans Health Administration (VHA) Quality Enhancement Research Initiative (QUERI) J Am Med Inform Assoc. 2004 Sep-Oct;11(5):339–343. doi: 10.1197/jamia.M1499. [DOI] [PMC free article] [PubMed] [Google Scholar]