Abstract
Recent success in cancer immunotherapy has reinvigorated the hypothesis that the immune system can control many if not most cancers, in some cases producing durable responses in a way not seen with many small molecule drugs. Agonistic CD40 monoclonal antibodies (mAb) offer a new therapeutic option which has the potential to generate anti-cancer immunity by various mechanisms. CD40 is a tumor necrosis factor receptor superfamily member expressed broadly on antigen-presenting cells (APC) such as dendritic cells, B cells, and monocytes as well as many non-immune cells and a range of tumors. Agonistic CD40 mAb have been shown to activate APC and promote anti-tumor T cell responses and to foster cytotoxic myeloid cells with the potential to control cancer in the absence of T-cell immunity. Thus, agonistic CD40 mAb are fundamentally different from mAb which block negative immune checkpoint such as anti-CTLA-4 or anti-PD-1. Initial clinical trials of agonistic CD40 mAb have shown highly promising results in the absence of disabling toxicity, both in single-agent studies and in combination with chemotherapy; however, numerous questions remain regarding dose, schedule, route of administration, and formulation. Recent findings regarding the role played by the IgG isotype and the Fc gamma receptor (FcγR) in mAb crosslinking, together with insights into mechanisms of action, particularly with regards to the role of myeloid cells, are predicted to help design next-generation CD40 agonistic reagents with greater efficacy. Here, we will review the preclinical and clinical data and discuss the major issues facing the field.
Introduction
The last decade has seen unprecedented progress in cancer immunotherapy, with recent approval of two cancer immunotherapy drugs: a cell-based vaccine for use in metastatic prostate cancer (sipuleucel-T) (1) and an anti-CTLA-4 monoclonal antibody (mAb) for use in metastatic melanoma (ipilimumab) (2). Newer success with PD-1/PD-L1 blocking mAb (3,4) underline the potential of immune control and indicate that many cancer types are immunogenic yet able to annul effective destruction. A major advantage of cancer immunotherapy is the prospect of a durable response, but the difficulty is that only an unidentified proportion of patients (<25%) respond. Immunostimulatory mAb offer an attractive way of boosting anti-cancer responses and might be used to potentiate existing responses or as adjuvants for cancer vaccines (5). Preclinical models show that both approaches are effective. In such models one of the most effective reagents is agonistic CD40 mAb, particularly against lymphoid tumors. Like all such immunostimulators, effectiveness is greatest when controlling the more immunogenic tumors. Most of these studies point to CD8 T-cell effectors without the need for CD4 help, suggesting that triggering CD40 with a crosslinking mAb on antigen presenting cells (APC) can substitute for stimulation normally provided by helper T-cells via CD40 ligand (CD40-L). Other potential mechanisms of action have emerged, further driving translational efforts to develop CD40 mAb as a cancer therapy. Clinical activity observed in initial trials with several CD40 agonistic mAb is highly promising. This review will focus on agonistic CD40 mAb, how they work, and what we have learned from clinical trials to date that can help pave the way forward.
Mechanisms of action of agonistic CD40 mAb
CD40 is a tumor necrosis factor receptor superfamily member expressed on APC such as dendritic cells (DC), B cells, and monocytes as well as many non-immune cells and a wide range of tumors (6–8). Interaction with its trimeric ligand on activated T helper cells results in APC activation, required for the induction of adaptive immunity.
Physiologically, signaling via CD40 on APC is thought to represent a major component of T cell help and mediates in large part the capacity of helper T cells to license APC. Ligation of CD40 on DC, for example, induces increased surface expression of costimulatory and MHC molecules, production of proinflammatory cytokines, and enhanced T cell triggering. CD40 ligation on resting B cells increases antigen-presenting function and proliferation. The consequences of CD40 signaling are multifaceted and depend on the type of cell expressing CD40 and the microenvironment in which the CD40 signal is provided (8). Like some other members of the TNF receptor family, CD40 signaling is mediated by adapter molecules rather than by inherent signal-transduction activity of the CD40 cytoplasmic tail. Downstream kinases are activated when the receptor-assembled, multicomponent signaling complex translocates from CD40 to the cytosol (9) and a number of well-characterized signal transduction pathways are activated (10,11).
In pre-clinical models, rat anti-mouse CD40 mAb show remarkable therapeutic activity in the treatment of CD40+ B-cell lymphomas (12,13) (with 80–100% of mice cured and immune to re-challenge in a CD8 T-cell dependent manner) and are also effective in various CD40-negative tumors (14,15). These mAb are able to clear bulk tumors from mice with near terminal disease (12). To date, four CD40 mAb have been investigated in clinical trials: CP-870,893 (Pfizer and VLST) (16), dacetuzumab (Seattle Genetics) (17), Chi Lob 7/4 (University of Southampton) (18), and lucatumumab (Novartis) (19) (Table 1). These reagents show diverse activities ranging from strong agonism (CP-870,893) to antagonism (lucatumumab) (20). Currently there is no satisfactory explanation for this heterogeneity, with little evidence for epitope specificity being the determining factor, and some suggestion that isotype and Fc:FcγR may be important, given that F(ab')2 fragments of CD40 are usually inactive. Indeed, preclinical experiments show that such activity requires that the CD40 mAb has an intact Fc and hence F(ab')2 could not substitute for IgG, even when given in large doses to compensate for its shorter half-life (21).
Table 1.
Agonistic CD40 monoclonal antibodies in clinical trials*
| mAb | |||
|---|---|---|---|
| CP-870,893 | Dacetuzmumab | Chi Lob 7/4 | |
| Company/Institution | Pfizer/VLST | Seattle Genetics | Univ. of Southampton |
| Formulation | Fully human | Humanized | Chimeric |
| Isotype | IgG2 | IgG1 | IgG1 |
| Maximum dose | 0.2 mg/kg | Up to 12 mg/kg | Up to 160 mg total |
| Route of administration | i.v | i.v. | i.v. |
| Dosing interval | Every 3–4 weeks | Weekly | Weekly × 4 |
| Toxicity | Mild to moderate cytokine release syndrome | Mild to moderate cytokine release syndrome Non-infectious inflammatory eye disorders |
Study to address is underway |
| Diseases targeted | Melanoma Pancreatic carcinoma Mesothelioma |
Hematological malignancies, especially Non-Hodgkin's lymphoma | Advanced solid tumors and lymphoma |
| Clinical efficacy | Objective tumor responses reported in melanoma and pancreatic carcinoma (about 20%) | Objective tumor responses (in refractory and relapsed NHL, 12% as single agent; 47% with rituximab and gemcitabine) | Study to address is underway |
| Combinations explored | Chemotherapy Melanoma vaccine Tremelimumab |
Chemotherapy Rituximab |
None yet |
| Current clinical trials | With tremelimumab in metastatic melanoma With gemcitabine for resectable pancreatic carcinoma |
None | First-in-human trial for patients with advanced solid tumors and lymphoma |
only reagents showing agonistic activity are included and thus lucatumumab (Novartis) has not been discussed
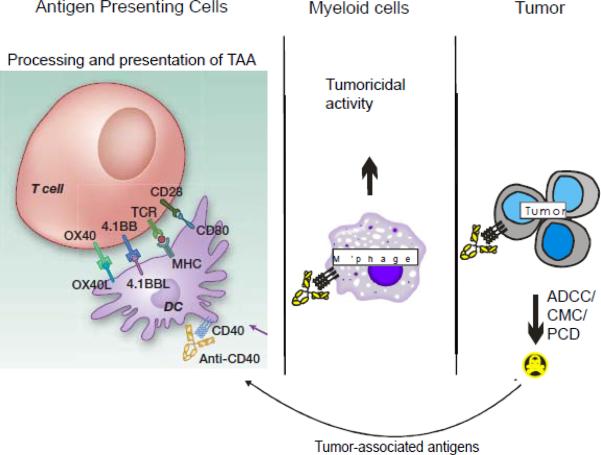
Although the primary mechanistic rationale invoked for agonistic CD40 mAb is to activate host APC, especially DC (termed “licensing” of DC), in order to induce clinically meaningful anti-tumor T-cell responses in patients, other immune mechanisms that are not necessarily mutually exclusive have been proposed (Figure 1). These include T cell-independent but macrophage-dependent triggering of tumor regression (22,23). CD40-activated macrophages can become tumoricidal, and least in pancreatic cancer, may also facilitate the depletion of tumor stroma which induces tumor collapse in vivo (23). Importantly, these mechanisms do not require expression of CD40 by the tumor, which has justified inclusion of patients with a broad range of tumors in many of the clinical trials. Insofar as these strategies aim to activate DC, macrophages, or both, the goal is not necessarily for the CD40 mAb to kill the cell it binds to, for example, via complement mediated cytotoxicity (CMC) or antibody dependent cellular cytoxicity (ADCC). Thus, by design, the strong agonistic mAb CP-870,893 is a fully human IgG2 molecule, which does not mediate CMC or ADCC (24). In contrast, other human CD40 mAb used to date have been of the IgG1 isotype and therefore more able to mediate CMC and ADCC against CD40+ tumors, such as nearly all B cell malignancies, a fraction of melanomas, and between 40%–75% of carcinomas (Figure 1). Dacetuzumab, for example, has been primarily tested in patients with B-cell malignancies that nearly uniformly express CD40 (17). Finally, there is some evidence that ligation of CD40 on tumor cells promotes apoptosis and that this can be accomplished without engaging any immune effector pathway. This has been shown for CD40+ B cell malignancies and certain solid tumors such as CD40+ carcinomas and melanomas (25–29). For low-grade B-cell malignancies (as for normal B cells), CD40 activation may actually be a strong activation and perhaps growth signal (30), and patients with such tumor types have often, but not always, been excluded from clinical trials of agonistic CD40 mAb. In fact, blocking the potential CD40-CD40L tumor growth signal has been a rationale for developing the CD40 antagonistic mAb lucatumumab in diseases such as chronic lymphocytic leukemia (CLL) (19). Immunologically, direct tumor cytotoxicity accomplished by CD40 agonists is hypothesized to provide a source of tumor antigen that can be processed and presented by host APC which are simultaneously activated by the same intervention. This “two-for-one” mechanism postulated for strong CD40 agonists has provided further justification for single-agent clinical trials, even though it seems likely that combining CD40 mAb with strong vaccines or cytokines may be clinically more potent for driving an adaptive anti-tumor immune response.
Figure 1. Potential mechanisms of action of agonistic CD40 mAb on various immune effectors.
The primary consequence of CD40 mAb is to activate DC (often termed licensing) (first panel) and potentially myeloid cells and B cells (not shown) and increase their ability to process and present Tumor-Associated Antigens (TAA) to local CTLs. Work from numerous model systems suggest that DC are the most potent in performing this function and show that only in tumors which are relatively immunogenic and hence have sufficient on-going immune recognition will control be established with this treatment. Recent data from genetic tumor models now underscore the ability of agonistic CD40 mAb to generate tumoricidal myeloid cells (middle panel) when CTL responses cannot be established. Finally, agonistic CD40 mAb can have a cytotoxic effect on tumor by initiating ADCC, CMC or program cell death (PCD) (third panel (tumor)). It is not clear to what extent anti-CD40 mAb can promote cell death in solid tumors, but hematological malignancies are susceptible to killing. Tumor associated antigens released from dead and dying tumor cells (panel 3 (tumor) have the potential to be cross-primed by APC and presented to CTL (panel 1) without the need for T-cell help.
Role of FcR crosslinking with CD40 mAb
Recent studies have highlighted the importance of FcγR for crosslinking agonistic CD40 mAb, offering the opportunity of Fc region engineering for `fine tuning' the relative level of agonistic activity. This work is important because it helps explain why F(ab')2 of CD40 mAb, unlike the parental IgG, were not agonistic and how a bivalent mAb when hyper-crosslinked by FcγR can mimic the molecular changes and transmembrane signaling that follows CD40:CD40L interaction in the immunological synapse of an APC and a T helper cell. Fcγ receptors are coded by a multigene complex with a number of members (FcγR-I, -II and –III in human and FcγR-I, -II, -III and –IV in mice), each containing a range of allelic variants with differing, functions, cell distribution and affinities for IgG isotypes. Most of the FcγR are able to trigger cellular activation as a result of signaling via an immunoreceptor tyrosine-based activation motif (ITAM). In addition, there is one family member, FcγRIIb (the homologous receptor in mice is sometimes called FcγRII), which is widely distributed on hematological and non-hematological tissues that contains an immunoreceptor tyrosine-based inhibition motif (ITIM) in its cytoplasmic domain and is inhibitory to cellular responses. Activatory and inhibitory FcγR often work in concert such that the balance of their engagement on effector cells, i.e. the activatory:inhibitory ratio (A:I), regulates cellular responses and immunological outcome.
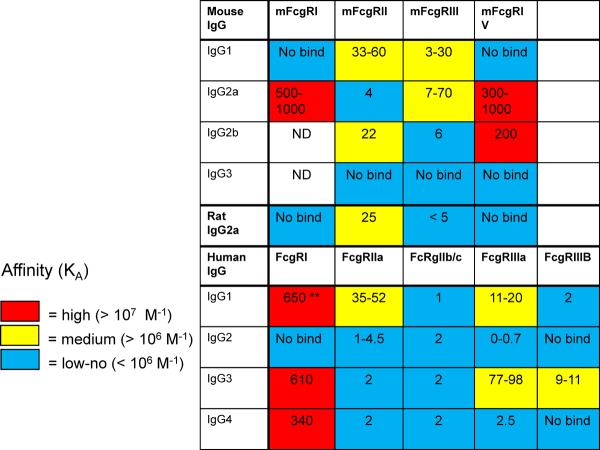
Most clinical mAb used to date have been of the human IgG1 isotype, selected because they bind with a high A:I ratio to a wide range of FcγR and are active in ADCC (Figure 2). IgG2 by contrast is relatively inactive in recruitment of FcγR-expressing effectors as it only binds to one FcγR with appreciable efficiency, the H131 allelic variant of FcγRIIa. Three of the clinical CD40 mAb used to date are IgG1 (dacetuzumab, Chi Lob 7/4, and lucatumumab) – and hence should mediate CMC and ADCC, while the fourth (CP-870,893) is IgG2; however, it is now apparent that the IgG2 Pfizer reagent is far more agonistic (see below).
Figure 2. Binding affinities of mouse, rat and human IgG to mouse and human Fcγ receptors.
The values for the mouse IgG binding to mouse FcgR are taken from Nimmerjahn et al (58) and White et al (31). The values for rat IgG2a binding to mouse FcgR are provided by Dr Ian Mockridge (University of Southampton). The values for the human IgG and FcγR are taken from Bruhns et al (33). Mouse IgG1 and rat IgG2a, which are highly agonistic as anti-CD40 reagents, bind to the inhibitory FcγRII with modest affinity (yellow box) but not to the activatory FcγR, FcγRI or IV. A similar isotype does not exist in humans making it difficult to select an isotype with similar agonistic properties. It is important to note that the affinity measurements for FcγR:IgG binding can show considerable variation, depending on the methods used. Thus while the relative affinities are correct the exact values are subject to experimental differences.
** Affinity values: a KA value of 650 in the table equates to 6.5 × 107 M−1. Where a range of affinities is shown this indicates measurements from different publications or binding to different alleles of certain human FcγR, such as FcγRIIa and FcγRIIIa. ND: not determined. No bind: indicates that an affinity measurement could not be made due to low binding.
Considerable insight regarding the impact of isotype in the function of CD40 mAb comes from the studies of White and colleagues (31) and Li and Ravetch (32). Both groups found that the inhibitory receptor FcγRIIb was critical in controlling the agonistic activity of CD40 mAb. Despite all having the same V-region sequences, rat IgG2a and mouse IgG1 CD40 mAb which bind relatively strongly to FcγRIIb were far more agonistic than equivalent mouse IgG2a reagents. These results are surprising because just as most human therapeutic mAb have used IgG1 (because of its stronger binding to the activatory FcγR, high A:I ratio and potent cytotoxic activity), in mice IgG2a shows similar functionality and would be a first choice when making a therapeutic (33) However, human IgG1 and mouse IgG2a mAb are only most appropriate when cytotoxic activity is required, yet are clearly not the most potent CD40 mAb agonists. White and colleagues (31) have gone on to show that the FcγRIIb is only required for crosslinking, since the ITIM containing cytoplasmic tail of the molecule can be deleted, at least in vitro, and it still provides crosslinking function to agonistic CD40 mAb. Furthermore, when individual FcγR, activatory and inhibitory, were over expressed on feeder cells, then they were all able to provide the necessary crosslinking of CD40 mAb (mouse IgG1 or IgG2a) to promote B-cell activation and proliferation. Thus, it appears the importance of FcγRIIb reflects availability of FcγRIIb in vivo rather than a special function, such as signaling or affinity.
An alternative suggestion for the relatively lower of potency of mouse IgG2a (mIgG2a) CD40 mAb is the cytotoxic activity toward CD40+ APC via CMC or ADCC when the activatory FcγR is engaged. While this would be a logical explanation, there is no evidence to support this. We have found that in mice, in vivo administration of mIgG2a CD40 mAb does not significantly delete CD40-expressing B cells or DCs (23,31), and a mixture of mIgG1 and mIgG2a CD40 mAb did not reduce the agonistic activity of the mIgG1 (32). Furthermore, deleting NK cells or using mice deficient in FcγRIV, both manoeuvres known to reduce the cytotoxic activity of mIgG2a, did not increase the agonistic activity of mIgG2a CD40 mAb. These observations reinforce the view that there is nothing inherently amiss or cytotoxic with mIgG2a mAb; rather, activatory FcγR are not available and/or not at the right location to provide crosslinking to the IgG2a CD40 mAb on DC, macrophages or B cells.
This work clearly has considerable implications when designing human reagents. First, it is important to note that unfortunately the mouse IgG1/IgG2a differences which allow the activatory and inhibitory FcγR to be differentially engaged do not exist in humans (Figure 2). In particular there is no human equivalent to the mouse IgG1 (and rat IgG2a) with its preferential binding to FcγRIIb. An alternative is to engineer human IgG1 to increase its tendency to bind to FcγRIIb. Early results show this can by highly successful with S267E and S267E/L328F Fc region substitutions increasing affinity by 30- and 430-fold, respectively, with a corresponding improvement in their ability to activate B cells via CD40 in vitro (AL White, personal communication) and to increase the in vivo immunostimulatory and therapeutic activity in human FcγRIIB transgenic mice (32,34).
Clinical development of agonist CD40 mAb
The effort over the last 10 years to develop CD40 agonists as a new class of drug for cancer treatment has been extensive (20). These approaches primarily include agonistic CD40 mAb but also include recombinant CD40L and CD40L gene therapy – all of which have been tested in patients, each with promising initial results (20). Many other formulations to accomplish CD40-mediated immune activation are in preclinical testing (35,36). In the first clinical trial of CD40 agonists, recombinant human CD40L showed clinical activity and led to long-term complete remission in a patient with advanced squamous cell cancer of the head and neck (37). Similarly, CP-870,893 has shown clinical efficacy in a number of settings of patients with advanced cancer. The initial trial, testing a single intravenous infusion of CP-870,893, resulted in four partial responses out of 29 patients with advanced cancer, with all responses at the maximum tolerated dose (MTD) of 0.2 mg/kg (16). One of these patients received 9 subsequent doses of CP-870,893 over the next year and a half (roughly one infusion every 8 weeks) and remains in complete remission more than 5 years later. Peripheral B cell depletion and activation is a prominent pharmacodynamic effect of CP-870,893 (16). However, a trial of weekly CP-870,893 was performed in 27 advanced cancer patients, and no objective clinical responses were observed, with some evidence suggesting that the dosing interval of one week was too short although further study is needed(38).
Because of a potential synergy between chemotherapy (to release tumor antigen) and CD40 agonists (to activate APC), CP-870,893 has been tested in combination with carboplatin and paclitaxel (every 3 weeks in a trial of advanced cancer patients (39)) and gemcitabine (every 4 weeks in a trial of patients with metastatic pancreatic carcinoma (23)). Objective tumor regressions were observed in about 20% of patients in each study. In pancreatic cancer, these findings were seen as significant because the response rate of standard-of-care gemcitabine alone is 5% or less. A trial of gemcitabine with CP-870,893 for patients with resectable pancreatic cancer recently opened at the University of Pennsylvania, as has a trial of CP-870,893 in combination with anti-CTLA-4 blocking mAb tremelimumab for patients with metastatic melanoma. A trial of CP-870,893 with cisplatin and pemetrexed for patients with advanced mesothelioma was recently completed at the University of Western Australia based on a previously published murine model (40). Importantly, whether or not CP-870,893 mAb infusion is associated with the induction of cellular tumor-specific immunity in patients, as predicated by preclinical models, remains to be fully explored, although it is noteworthy that two patients with melanoma receiving CP-870,893 with chemotherapy developed widespread vitiligo (39), a T cell-dependent autoimmune phenomenon.
Dacetuzumab, a weaker CD40 agonist than CP-870,893, has shown single-agent activity when given intravenously every week, especially in patients with diffuse large B cell lymphoma (DLBCL) (41). Stable disease but not tumor regression was observed with dacetuzumab in multiple myeloma (42) and CLL (43). Preclinical data suggest synergy of dacetuzumab and other agents such as CD20 mAb rituximab, leading to combination clinical trials (44). In a phase 1b study of dacetuzumab in combination with rituximab and gemcitabine in patients with relapsed or refractory DLBCL, complete response rate was 20% and partial response rate was 27% (45). However, a randomized, double-blind phase IIb clinical trial of dacetuzumab vs. placebo in combination with rituximab plus ifosfamide, carboplatin and etoposide chemotherapy for patients with relapsed or refractory DLBCL was terminated early because it was decided that the study was unlikely to meet its primary endpoint of superior complete response rate in the dacetuzumab arm. In further analysis, however, dacetuzumab investigators recently presented data demonstrating a trend towards increased survival in the dacetuzumab arm. Presence at baseline of a 15-gene signature of the tumor from DLBCL patients treated with dacetuzumab predicts clinical response with an 80% overall accuracy, suggesting the prospect of patient selection to aid in the development of dacetuzumab (46). This signature includes genes directly regulated by CD40 stimulation, part of the CD40 pathway network, or a component of the germinal center B cell–like or activated B cell–like classifier (46). Currently, there are no registered trials of dacetuzumab.
The third agonistic CD40 mAb, Chi Lob 7/4, again less agonistic than CP-870,893, is undergoing initial clinical testing. Infusion of this chimeric IgG1 mAb has been well tolerated up to 160 mg per intravenous weekly dose times four in patients with advanced histologically proven CD40-expressing solid tumors or DLBCL (18). Eleven of the first 21 patients have had stable disease as best response (no complete or partial responses). Enrollment and dose escalation are continuing.
Interestingly, the MTD of a single infusion of CP-870,893 is estimated at 0.2 mg/kg, but single doses of at least 12 mg/kg dacetuzumab and Chi Lob 7/4 of at least 160 mg total have been tolerated in patients, highlighting the differences in each of these three mAb.
Words of caution and toxicity
The development of agonistic CD40 mAb as a novel cancer therapy has not been universally endorsed. Concerns cited include the prospect of triggering cytokine release syndromes (47), autoimmune reactions (47), thromboembolic syndromes (because CD40 is expressed by platelets and endothelial cells), hyper immune stimulation leading to activation-induced cell death or tolerance (48,49), and tumor angiogenesis possibly on the basis of CD40-dependent activation of tumor endothelial cells (50). It is hypothesized that these effects may cause untoward toxicity or the promotion of tumor growth (51), but most of these concerns have not been realized in a clinically significant way. For the strongest agonist tested, CP-870,893, the most common side effect is cytokine release syndrome, manifesting as chills, fever, rigors, and other symptoms soon after infusion, but this has largely been grade 2 or less, transient, and easily managed in the outpatient setting (16,38,39). Several cases of thromboembolic events have been observed with CP-870,893, but this has been confounded by the advanced state of the cancer patients treated in these trials for whom thromboembolism is a well-recognized comorbidity related to the cancer burden. Autoimmune reactions have not been observed, including no cases of colitis, dermatitis, hypophysitis, or thyroiditis (in distinction, for example, to the FDA approved mAb ipilimumab). Noninfectious inflammatory eye disorders have been observed with dacetuzumab but not CP-870,893 (41). Agonist CD40 mAb have also triggered mild elevations in liver enzymes and decreases in circulating platelet numbers, but importantly, liver necrosis, hemolysis and disseminated intravascular coagulation has not been reported in patients. With regard to hyper immune stimulation, weekly infusion of CP-870,893 led to evidence for chronic B cell activation associated with a marked diminution in circulating T cell numbers (38) – potentially consistent with activation induced cell death – but these effects have not been observed when CP-870,893 is dosed every three or more weeks. Overall, toxicity has not been a major issue with CD40 agonists in the clinic. It remains to be proven, of course, that immune activation can be optimally and reliably achieved in vivo in patients treated at the current doses, schedules, and routes of administration. Local administration of CD40 mAb, rather than systemic, is one alternative approach that merits further testing (52).
Future challenges
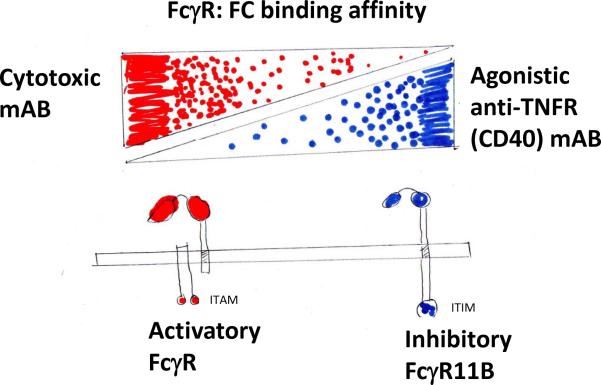
To improve the clinical effectiveness of agonistic CD40 mAb, several major challenges remain to be addressed including: testing of appropriate therapeutic combinations; determining optimal dose, schedule, and route of administration; and identifying appropriate patient populations. It is also critical that we improve our understanding of the mechanism of action of different CD40 mAb and understand which of the many mechanisms is the most appropriate for a given situation or disease (Figure 1). Such understanding will allow the design of more appropriate and more potent CD40 agonists for different diseases. For example, Chi Lob 7/4, being a modest agonist of the IgG1 isotype, is able to delete B cells and this is likely to be important in B-cell malignancies such as DLBCL; however, in these same patients DC are not being depleted and are available for cross-priming tumor antigens to generate useful CD8 responses (PWM Johnson and T Williams, personal communication). Nevertheless, these same IgG1 reagents may not be sufficiently agonistic to promote DC activation and allow cross-priming of antigen for the generation of robust T cell responses. In this situation, CD40 mAb efficacy may be improved by Fc region engineering to increase binding to FcγRIIb to promote agonistic activity, assuming that FcγRIIb in humans behaves in a similar manner to that in mice. The likely cost of such manipulations is a reduced FcγR binding A:I ratio and hence reduced cytotoxic activity which would reduce the direct killing of the tumors at the cost of improved T-cell immunity. The schematic in Figure 3 demonstrates this change in function as mouse mAb move from binding mainly to the activatory FcγRs (cytotoxic) to the inhibitory FcγRIIb (agonistic).
Figure 3.
Schematic demonstrating that, at least in mice, strong binding of mAb to the activatory FcγR (IgG2a) will favor cytotoxic activity via recruitment of cellular effectors, such as NK and macrophages. In contrast, mAb which bind more strongly to the inhibitory FcγR, FcγRIIb (IgG1) will be stronger agonist ideal for crosslinking TNFR molecules and promoting Ab and T-cell responses. On-going work is underway to demonstrate if similar properties can be exploited with human mAb.
At the other extreme and for reasons which are still not understood, CP-870,893 is highly agonistic and might be an ideal candidate to generate T-cell responses against a co-administered vaccine (20). This level of agonism might not be ideal for systemic use since MTD is reached at 0.2 mg/kg, possibly before saturation of CD40 receptors on tissue resident DC or macrophages is achieved. Local administration might overcome this. Perhaps an alternative reagent for systemic use would display an agonistic activity somewhere between that of dacetuzumab/Chi Lob 7/4 and CP-870,893, and which could be used at appreciable doses with an improved likelihood of fully engaging macrophages and DC in the tissues. Whether the Fc region of a human IgG can be `tweaked' by protein engineering to achieve such characteristics is not yet clear. Such a reagent likely needs a reduced A:I ratio to allow Fc:FcγRIIb crosslinking without target killing. Hence, it would display reduced B-cell killing, but could be used at increased doses to promote both myeloid and T cell effectors within solid tumors and their draining lymph nodes.
Conclusions
In our view, agonistic CD40 mAb represent a promising strategy for novel cancer therapeutics. Preclinical investigations with CD40 agonists have been robust and highlight multiple mechanisms of action including activation of APC that drives anti-tumor T cells, activation of macrophages that are tumoricidal, and induction of apoptosis in CD40+ tumor cells such as lymphoma or certain solid tumors. Initial clinical trials of agonistic CD40 mAb have shown clinical activity in the absence of disabling toxicity. Some clinical responses have been dramatic and very durable, but response rates remain 20% or less. It seems likely that at least for solid tumors, agonistic CD40 mAb will be most effectively used in combination with other modalities such as chemotherapy, radiation, or vaccines; however, single agent therapy for B cell lymphoma remains an important possibility. Phase II clinical trials with the strongest agonistic CD40 mAb (CP-870,893 and Chi Lob 7/4) with or without chemotherapy have not been performed but are needed.
It is important to emphasize that agonistic CD40 mAb as immunostimulatory agents strikingly differ in their proposed mechanism of action compared to mAb that accomplish immune activation by blocking negative checkpoint molecules such as CTLA-4 or PD-1. Indeed, the prospect of combining agonistic CD40 mAb with anti-CTLA-4 or anti-PD-1 mAb is enticing and represents a real immunological opportunity to “step on the gas” while “cutting the brakes”. As noted in this issue of Clinical Cancer Research, combinations of novel immunotherapy – especially immunodmodulatory mAb – is an important goal (53–57).
In summary, with such a wealth of potential mechanisms of action and the ability to fine tune mAb structure and function to suit particular requirements, the next decade is likely to see rapid advances with agonistic CD40 mAb.
Acknowledgements
Supported by National Institutes of Health grants R01 CA158186 and R01 CA169123 (to R.H. Vonderheide) and by grants from the Cancer Research UK and National Centre for the 3Rs (to M.J. Glennie). We also thank Dr Ruth French for her help in reviewing this manuscript.
Footnotes
Disclosure
Dr. Vonderheide reports receiving research funding from Pfizer Corporation.
References
- 1.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 2.Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–54. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455–65. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Melero I, Hervas-Stubbs S, Glennie M, Pardoll DM, Chen L. Immunostimulatory monoclonal antibodies for cancer therapy. Nat Rev Cancer. 2007;7:95–106. doi: 10.1038/nrc2051. [DOI] [PubMed] [Google Scholar]
- 6.Eliopoulos AG, Young LS. The role of the CD40 pathway in the pathogenesis and treatment of cancer. Curr Opin Pharmacol. 2004;4:360–7. doi: 10.1016/j.coph.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Grewal IS, Flavell RA. CD40 and CD154 in cell-mediated immunity. Annu Rev Immunol. 1998;16:111–35. doi: 10.1146/annurev.immunol.16.1.111. [DOI] [PubMed] [Google Scholar]
- 8.van Kooten C, Banchereau J. CD40-CD40 ligand. J Leukoc Biol. 2000;67:2–17. doi: 10.1002/jlb.67.1.2. [DOI] [PubMed] [Google Scholar]
- 9.Matsuzawa A, Tseng PH, Vallabhapurapu S, Luo JL, Zhang W, Wang H, et al. Essential cytoplasmic translocation of a cytokine receptor-assembled signaling complex. Science. 2008;321:663–8. doi: 10.1126/science.1157340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dadgostar H, Zarnegar B, Hoffmann A, Qin XF, Truong U, Rao G, et al. Cooperation of multiple signaling pathways in CD40-regulated gene expression in B lymphocytes. Proc Natl Acad Sci U S A. 2002;99:1497–502. doi: 10.1073/pnas.032665099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gallagher E, Enzler T, Matsuzawa A, Anzelon-Mills A, Otero D, Holzer R, et al. Kinase MEKK1 is required for CD40-dependent activation of the kinases Jnk and p38, germinal center formation, B cell proliferation and antibody production. Nat Immunol. 2007;8:57–63. doi: 10.1038/ni1421. [DOI] [PubMed] [Google Scholar]
- 12.Tutt AL, O'Brien L, Hussain A, Crowther GR, French RR, Glennie MJ. T cell immunity to lymphoma following treatment with anti-CD40 monoclonal antibody. J Immunol. 2002;168:2720–8. doi: 10.4049/jimmunol.168.6.2720. [DOI] [PubMed] [Google Scholar]
- 13.French RR, Chan HT, Tutt AL, Glennie MJ. CD40 antibody evokes a cytotoxic T-cell response that eradicates lymphoma and bypasses T-cell help. Nat Med. 1999;5:548–53. doi: 10.1038/8426. [DOI] [PubMed] [Google Scholar]
- 14.Todryk SM, Tutt AL, Green MH, Smallwood JA, Halanek N, Dalgleish AG, et al. CD40 ligation for immunotherapy of solid tumours. J Immunol Methods. 2001;248:139–47. doi: 10.1016/s0022-1759(00)00349-5. [DOI] [PubMed] [Google Scholar]
- 15.van Mierlo GJ, den Boer AT, Medema JP, van der Voort EI, Fransen MF, Offringa R, et al. CD40 stimulation leads to effective therapy of CD40(−) tumors through induction of strong systemic cytotoxic T lymphocyte immunity. Proc Natl Acad Sci U S A. 2002;99:5561–6. doi: 10.1073/pnas.082107699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vonderheide RH, Flaherty KT, Khalil M, Stumacher MS, Bajor DL, Hutnick NA, et al. Clinical activity and immune modulation in cancer patients treated with CP-870,893, a novel CD40 agonist monoclonal antibody. J Clin Oncol. 2007;25:876–83. doi: 10.1200/JCO.2006.08.3311. [DOI] [PubMed] [Google Scholar]
- 17.Khubchandani S, Czuczman MS, Hernandez-Ilizaliturri FJ. Dacetuzumab, a humanized mAb against CD40 for the treatment of hematological malignancies. Curr Opin Investig Drugs. 2009;10:579–87. [PubMed] [Google Scholar]
- 18.Johnson PW, Steven NM, Chowdhury F, Dobbyn J, Hall E, Ashton-Key M, et al. A Cancer Research UK phase I study evaluating safety, tolerability, and biological effects of chimeric anti-CD40 monoclonal antibody (MAb), Chi Lob 7/4. J Clin Oncol. 2010;28:2507. abstract. [Google Scholar]
- 19.Bensinger W, Maziarz RT, Jagannath S, Spencer A, Durrant S, Becker PS, et al. A phase 1 study of lucatumumab, a fully human anti-CD40 antagonist monoclonal antibody administered intravenously to patients with relapsed or refractory multiple myeloma. Br J Haematol. 2012;159:58–66. doi: 10.1111/j.1365-2141.2012.09251.x. [DOI] [PubMed] [Google Scholar]
- 20.Vonderheide RH. Prospect of targeting the CD40 pathway for cancer therapy. Clin Cancer Res. 2007;13:1083–8. doi: 10.1158/1078-0432.CCR-06-1893. [DOI] [PubMed] [Google Scholar]
- 21.Glennie MJ, Honeychurch J, French RR, Tutt AL. The application of monoclonal antibodies in the treatment of lymphoma. Methods in molecular medicine. 2000;40:85–97. doi: 10.1385/1-59259-076-4:85. [DOI] [PubMed] [Google Scholar]
- 22.Lum HD, Buhtoiarov IN, Schmidt BE, Berke G, Paulnock DM, Sondel PM, et al. In vivo CD40 ligation can induce T-cell-independent antitumor effects that involve macrophages. J Leukoc Biol. 2006;79:1181–92. doi: 10.1189/jlb.0405191. [DOI] [PubMed] [Google Scholar]
- 23.Beatty GL, Chiorean EG, Fishman MP, Saboury B, Teitelbaum UR, Sun W, et al. CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science. 2011;331:1612–6. doi: 10.1126/science.1198443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gladue RP, Paradis T, Cole SH, Donovan C, Nelson R, Alpert R, et al. The CD40 agonist antibody CP-870,893 enhances dendritic cell and B-cell activity and promotes anti-tumor efficacy in SCID-hu mice. Cancer Immunol Immunother. 2011;60:1009–17. doi: 10.1007/s00262-011-1014-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eliopoulos AG, Davies C, Knox PG, Gallagher NJ, Afford SC, Adams DH, et al. CD40 induces apoptosis in carcinoma cells through activation of cytotoxic ligands of the tumor necrosis factor superfamily. Molecular and cellular biology. 2000;20:5503–15. doi: 10.1128/mcb.20.15.5503-5515.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghamande S, Hylander BL, Oflazoglu E, Lele S, Fanslow W, Repasky EA. Recombinant CD40 ligand therapy has significant antitumor effects on CD40-positive ovarian tumor xenografts grown in SCID mice and demonstrates an augmented effect with cisplatin. Cancer Res. 2001;61:7556–62. [PubMed] [Google Scholar]
- 27.Funakoshi S, Longo DL, Beckwith M, Conley DK, Tsarfaty G, Tsarfaty I, et al. Inhibition of human B-cell lymphoma growth by CD40 stimulation. Blood. 1994;83:2787–94. [PubMed] [Google Scholar]
- 28.Kalbasi A, Fonsatti E, Natali PG, Altomonte M, Bertocci E, Cutaia O, et al. CD40 expression by human melanocytic lesions and melanoma cell lines and direct CD40 targeting with the therapeutic anti-CD40 antibody CP-870,893. J Immunother. 2010;33:810–6. doi: 10.1097/CJI.0b013e3181ee73a7. [DOI] [PubMed] [Google Scholar]
- 29.von Leoprechting A, van der Bruggen P, Pahl HL, Aruffo A, Simon JC. Stimulation of CD40 on immunogenic human malignant melanomas augments their cytotoxic T lymphocyte-mediated lysis and induces apoptosis. Cancer Res. 1999;59:1287–94. [PubMed] [Google Scholar]
- 30.Schultze JL, Michalak S, Seamon MJ, Dranoff G, Jung K, Daley J, et al. CD40 activated human B cells: an alternative source of highly efficient antigen presenting cells to generate autologous antigen-specific T cells for adoptive immunotherapy. J Clin Invest. 1997;100:2757–65. doi: 10.1172/JCI119822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White AL, Chan HT, Roghanian A, French RR, Mockridge CI, Tutt AL, et al. Interaction with FcgammaRIIB is critical for the agonistic activity of anti-CD40 monoclonal antibody. J Immunol. 2011;187:1754–63. doi: 10.4049/jimmunol.1101135. [DOI] [PubMed] [Google Scholar]
- 32.Li F, Ravetch JV. Inhibitory Fcgamma receptor engagement drives adjuvant and antitumor activities of agonistic CD40 antibodies. Science. 2011;333:1030–4. doi: 10.1126/science.1206954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bruhns P, Iannascoli B, England P, Mancardi DA, Fernandez N, Jorieux S, et al. Specificity and affinity of human Fcgamma receptors and their polymorphic variants for human IgG subclasses. Blood. 2009;113:3716–25. doi: 10.1182/blood-2008-09-179754. [DOI] [PubMed] [Google Scholar]
- 34.Smith P, DiLillo DJ, Bournazos S, Li F, Ravetch JV. Mouse model recapitulating human Fcgamma receptor structural and functional diversity. Proc Natl Acad Sci U S A. 2012;109:6181–6. doi: 10.1073/pnas.1203954109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanks BA, Jiang J, Singh RA, Song W, Barry M, Huls MH, et al. Re-engineered CD40 receptor enables potent pharmacological activation of dendritic-cell cancer vaccines in vivo. Nat Med. 2005;11:130–7. doi: 10.1038/nm1183. [DOI] [PubMed] [Google Scholar]
- 36.Mason NJ, Coughlin CM, Overley B, Cohen JN, Mitchell EL, Colligon TA, et al. RNA-loaded CD40-activated B cells stimulate antigen-specific T-cell responses in dogs with spontaneous lymphoma. Gene therapy. 2008;15:955–65. doi: 10.1038/gt.2008.22. [DOI] [PubMed] [Google Scholar]
- 37.Vonderheide RH, Dutcher JP, Anderson JE, Eckhardt SG, Stephans KF, Razvillas B, et al. Phase I study of recombinant human CD40 ligand in cancer patients. J Clin Oncol. 2001;19:3280–7. doi: 10.1200/JCO.2001.19.13.3280. [DOI] [PubMed] [Google Scholar]
- 38.Ruter J, Antonia SJ, Burris HA, 3rd, Huhn RD, Vonderheide RH. Immune modulation with weekly dosing of an agonist CD40 antibody in a phase I study of patients with advanced solid tumors. Cancer Biol Ther. 2010;10:983–93. doi: 10.4161/cbt.10.10.13251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vonderheide RH, Burg JM, Mick R, Trosko JA, Li D, Shaik MN, et al. Phase I study of CD40 antibody CP-870,893 in combination with carboplatin and paclitaxel in patients with advanced solid tumors. OncoImmunology. doi: 10.4161/onci.23033. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hasani A, Feeney K, Nowak A, Millward M. Audit of patients with mesothelioma treated with pemetrexed in a single institution in Western Australia. Asia Pac J Clin Oncol. 2010;6:350–6. doi: 10.1111/j.1743-7563.2010.01316.x. [DOI] [PubMed] [Google Scholar]
- 41.Advani R, Forero-Torres A, Furman RR, Rosenblatt JD, Younes A, Ren H, et al. Phase I study of the humanized anti-CD40 monoclonal antibody dacetuzumab in refractory or recurrent non-Hodgkin's lymphoma. J Clin Oncol. 2009;27:4371–7. doi: 10.1200/JCO.2008.21.3017. [DOI] [PubMed] [Google Scholar]
- 42.Hussein M, Berenson JR, Niesvizky R, Munshi N, Matous J, Sobecks R, et al. A phase I multidose study of dacetuzumab (SGN-40; humanized anti-CD40 monoclonal antibody) in patients with multiple myeloma. Haematologica. 2010;95:845–8. doi: 10.3324/haematol.2009.008003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Furman RR, Forero-Torres A, Shustov A, Drachman JG. A phase I study of dacetuzumab (SGN-40, a humanized anti-CD40 monoclonal antibody) in patients with chronic lymphocytic leukemia. Leuk Lymphoma. 2010;51:228–35. doi: 10.3109/10428190903440946. [DOI] [PubMed] [Google Scholar]
- 44.Lewis TS, McCormick RS, Emmerton K, Lau JT, Yu SF, McEarchern JA, et al. Distinct apoptotic signaling characteristics of the anti-CD40 monoclonal antibody dacetuzumab and rituximab produce enhanced antitumor activity in non-Hodgkin lymphoma. Clin Cancer Res. 2011;17:4672–81. doi: 10.1158/1078-0432.CCR-11-0479. [DOI] [PubMed] [Google Scholar]
- 45.Forero-Torres A, Bartlett N, Beaven A, Myint H, Nasta S, Northfelt DW, et al. Pilot study of dacetuzumab in combination with rituximab and gemcitabine for relapsed or refractory diffuse large B-cell lymphoma. Leuk Lymphoma. 2012 doi: 10.3109/10428194.2012.710328. [DOI] [PubMed] [Google Scholar]
- 46.Burington B, Yue P, Shi X, Advani R, Lau JT, Tan J, et al. CD40 pathway activation status predicts response to CD40 therapy in diffuse large B cell lymphoma. Sci Transl Med. 2011;3:74ra22. doi: 10.1126/scitranslmed.3001620. [DOI] [PubMed] [Google Scholar]
- 47.Tong AW, Stone MJ. Prospects for CD40-directed experimental therapy of human cancer. Cancer gene therapy. 2003;10:1–13. doi: 10.1038/sj.cgt.7700527. [DOI] [PubMed] [Google Scholar]
- 48.Kedl RM, Jordan M, Potter T, Kappler J, Marrack P, Dow S. CD40 stimulation accelerates deletion of tumor-specific CD8(+) T cells in the absence of tumor-antigen vaccination. Proc Natl Acad Sci U S A. 2001;98:10811–6. doi: 10.1073/pnas.191371898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berner V, Liu H, Zhou Q, Alderson KL, Sun K, Weiss JM, et al. IFN-gamma mediates CD4+ T-cell loss and impairs secondary antitumor responses after successful initial immunotherapy. Nat Med. 2007;13:354–60. doi: 10.1038/nm1554. [DOI] [PubMed] [Google Scholar]
- 50.Chiodoni C, Iezzi M, Guiducci C, Sangaletti S, Alessandrini I, Ratti C, et al. Triggering CD40 on endothelial cells contributes to tumor growth. J Exp Med. 2006;203:2441–50. doi: 10.1084/jem.20060844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bergmann S, Pandolfi PP. Giving blood: a new role for CD40 in tumorigenesis. J Exp Med. 2006;203:2409–12. doi: 10.1084/jem.20061754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fransen MF, Sluijter M, Morreau H, Arens R, Melief CJ. Local activation of CD8 T cells and systemic tumor eradication without toxicity via slow release and local delivery of agonistic CD40 antibody. Clin Cancer Res. 2011;17:2270–80. doi: 10.1158/1078-0432.CCR-10-2888. [DOI] [PubMed] [Google Scholar]
- 53.Gilboa E, McNamara JO, Pastor F. Use of oligonucleotide aptamer ligands to modulate the function of immune receptors. Clin Cancer Res. 2013;19:xx–xx. doi: 10.1158/1078-0432.CCR-12-2067. [DOI] [PubMed] [Google Scholar]
- 54.Melero I, Hirschhorn-Cymerman D, Morales-Kastresana A, Sanmamed MF, Wolchok JD. Agonist antibodies to TNFR molecules that costimulate T and NK cells. Clin Cancer Res. 2013;19:xx–xx. doi: 10.1158/1078-0432.CCR-12-2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sznol M, Chen L. Antagonist antibodies to PD-1 and B7-H1 (PD-L1) in the treatment of advanced human cancer. Clin Cancer Res. 2013;19:xx–xx. doi: 10.1158/1078-0432.CCR-12-2063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Melero I, Grimaldi AM, Perez-Gracia JL, Ascierto PA. Clinical development of immunostimulatory monoclonal antibodies and opportunities for combination. Clin Cancer Res. 2013;19:xx–xx. doi: 10.1158/1078-0432.CCR-12-2214. [DOI] [PubMed] [Google Scholar]
- 57.Ascierto PA, Kalos M, Schaer DA, Callahan MK, Wolchok JD. Biomarkers for immunostimulatory monoclonal antibodies in combination strategies for melanoma and other tumor types. Clin Cancer Res. 2013;19:xx–xx. doi: 10.1158/1078-0432.CCR-12-2982. [DOI] [PubMed] [Google Scholar]
- 58.Nimmerjahn F, Bruhns P, Horiuchi K, Ravetch JV. Immunity. 2005;23:41–51. doi: 10.1016/j.immuni.2005.05.010. [DOI] [PubMed] [Google Scholar]