Abstract
Tularemia is a zoonotic disease caused by the Category A bioterrorism agent Francisella tularensis. In Scandinavia, tularemia transmission by mosquitoes has been widely cited in the literature. We tested >2,500 mosquitoes captured in Alaska and found Francisella DNA in 30% of pooled samples. To examine the potential for transmission of Francisella by mosquitoes, we developed a mosquito model of Francisella infection. Larvae of Anopheles gambiae Giles and Aedes aegypti (L.) readily ingest F. tularensis but do not efficiently transfer infective doses of the bacterium to the pupal or adult stage. After a bloodmeal containing Francisella, adult female An. gambiae and Ae. aegypti retained detectable levels of Francisella DNA for 3 d, but when they took a second bloodmeal, the mammalian host was not infected. This study suggests that although Francisella DNA can be detected in a significant portion of wild-caught mosquitoes, transmission of Francisella is either very inefficient or is species dependent for the Francisella strain or the arthropod vector.
Keywords: Francisella, mosquito, detection, transmission
Tularemia, a zoonotic, febrile disease, is caused by the bacterium Francisella tularensis. The combination of high virulence (30–60% untreated fatality rate), low infectious dose (10–25 colony-forming units [CFU] cause disease) (Saslaw and Carlisle 1961), and ability to be aerosolized, led to the classification of F. tularensis as a Category A bioterrorism agent by the Centers for Disease Control and Prevention (Darling et al. 2002).
Currently, four subspecies of F. tularensis have been identified (Keim et al. 2007), and their genomes have been sequenced (Rohmer et al. 2007). F. tularensis subsp. tularensis, or Type A, has the highest human mortality rate, is found mainly in North America and is most commonly associated with lagomorphs, rodents, and ticks. F. tularensis subsp. holarctica, or Type B, produces milder disease symptoms in humans and is found throughout the Northern Hemisphere (Keim et al. 2007). Type B has been isolated from ponds and streams (Forsman et al. 1990) and is most frequently associated with water dwellers such as muskrats, beavers, and mosquitoes (Olin 1942, Keim et al. 2007). F. tularensis subsp. mediasiatica and F. tularensis subsp. novicida have been identified in the central Asian republics of the former USSR (Olsufjev and Meshcheryakova 1982) and in other parts of the Northern Hemisphere and Australia, respectively, but they are less virulent and rarely cause human disease (Petersen and Schriefer 2005). F. tularensis subsp. novicida, U112 strain (U112), is a convenient laboratory model because of its reduced virulence in humans, its genetic similarities to F. tularensis subsp. tularensis and available genetic tools. In addition, it is very virulent in mice and causes a disease in these animals, similar to tularemia in humans.
Mosquitoes are efficient vectors that transmit viruses and protozoan parasites, causing >50 diseases in humans (Eldridge and Edman 2003). Examples of mosquito-transmitted diseases include malaria, yellow fever, dengue fever, and the various encephalitides (Eastern equine encephalitis, Japanese encephalitis B, Western equine encephalitis, and West Nile encephalitis). Although no transmission of bacterial pathogens by mosquitoes has been firmly established, mosquito borne transmission of Francisella has been suggested by a retrospective study of a tularemia outbreak in Sweden (Eliasson et al. 2002). Our previous work demonstrated that F. novicida can replicate in a mosquito cell line derived from An. gambiae (Read et al. 2008). However, no recent laboratory studies directly address disease transmission of Francisella by mosquitoes.
Female mosquitoes can feed on multiple hosts during their life span and do not always feed on the same host species, making mosquitoes potential vectors for diseases between different animal species including humans. Some mosquitoes are attracted to the higher body temperature due to fever induced by an acute or relapsing infection which makes transmission of pathogens to subsequent hosts more likely (Lehane 2005). Disease transmission can be mechanical, on the proboscis through interrupted feedings, or the mosquito might serve as a biological vector with microbial replication between blood feeding events (Petrishcheva 1965).
F. tularensis can reproduce and survive inside ticks (Ixodidae) for an extended time (>70 d) and can be transmitted through a bite at any point during infection (Olsufev 1960). Live mosquitoes have been captured and tested positive for F. tularensis (Petrishcheva 1965). In a more recent study examining the presence of Francisella in arthropods collected in the Czech republic, viable Francisella was isolated from ticks, but attempts to detect the bacterium by culture in mosquitoes were unsuccessful (Hubalek and Halouzka 1997).
In Scandinavia, where Francisella Type B is endemic, tularemia transmission is attributed to mosquitoes (Eliasson et al. 2002). However, evidence for mosquito transmission is mainly circumstantial. Two mechanisms of acquisition of bacteria by female mosquitoes can be envisioned: first, infection during larval development in water, followed by transstadial transmission to adult mosquitoes, or second, acquisition of Francisella through a bloodmeal on an infected host. To test these hypotheses we used An. gambiae and Ae. aegypti as model species to study the interactions between Francisella and mosquitoes.
Materials and Methods
Mosquito Capture in the Field and Detection of DNA in Pooled Samples
From May to August 2006, mosquitoes were collected at five different locations in the area around Fairbanks, AK (Fig. 1). Mosquito Magnet traps or CO2 traps were used for the collection. The captured mosquitoes were frozen at −20°C. DNA was extracted from pools of 10 individual mosquitoes by using the DNeasy tissue kit (QIAGEN, Valencia, CA). DNA was eluted in a total of 60 μl of deionized water and stored at −80°C.
Fig. 1.
Partial map of Alaska showing the interior region as used by the Department of Health and Human Services Epidemiology section and Fairbanks the collection site for mosquitoes.
To test the samples for Francisella DNA, we used a TaqMan real-time polymerase chain reaction (PCR) assay (Emanuel et al. 2003, Versage et al. 2003). The target is an 86-bp fragment of the fopA gene, which encodes a 43-kDa outer membrane protein. Amplification was carried out on an ABI 7900 real-time PCR instrument (Applied Biosystems, Foster City, CA). Primer and probe concentration were optimized according to the instructions (see ABI PRISM 7900HT Sequence Detection System user’s manual). Each reaction contained 600 nM forward (fopA-F) (AACAATGGCACCTAGTAATATTTCTGG) and reverse (fopA-R) (CCACCAAAGAACCATGTTAAACC) primer, 250 nM probe (5-carboxyfluorescein [FAM]-TGGCAGAGCGGGTACTAACATGATTGGT-5-carboxytetramethylrhodamine) and TaqMan Universal PCR Master Mix (Applied Biosystems) at a final 1× concentration. The extracted mosquito DNA was diluted (10×) and 2 μl was added to a final reaction volume of 25 μl. Thermal cycling conditions were as follows: 50°C for 2 min, 95°C for 10 min, 45 cycles at 95°C for 15 s and 60°C for 60 s, and then 45°C for 5 min.
Mosquito Identification
For positive pools the first half of the CO1 gene was amplified, and the products were sequenced using standard DNA barcoding methods. These sequences were used to query the Barcode of Life database (www.barcodinglife.org) to obtain identifications. Locally collected mosquitoes that were identified using the key published by Darsie and Ward (2005) were used to validate the results. Based on our sequencing data, known distributions, and our collection effort in the Fairbanks area, the pools were assigned a predominant species.
Mosquito Rearing
All captive mosquito related procedures were conducted in an approved Biohazard Safety Level-2 laboratory modified to Arthropod Containment Level-2 insectary. Mosquitoes were kept at 28°C, 50% RH, and a photoperiod of 12:12 (L:D) h.
Artifical Feeding
Artificial bloodmeals were used in colony maintenance and exposure of adult female mosquitoes, by using the Mishra feeder method (Mishra et al. 2005). The bottom of a glass jar was wrapped with parafilm leaving a small pocket in the center for blood. Warm water (40°C) was poured into the jar, and 2 ml of defibrinated sheep’s blood was injected between the parafilm and the glass jar, and the jar was placed directly on the mosquito cage.
Ae. aegypti Laboratory Colony
Ae. aegypti eggs were obtained from the Division of Vector Borne Infectious Diseases, Centers for Disease Control and Prevention (DVBID, CDC) in Fort Collins, CO. To hatch the eggs, a 4-cm piece of the egg strip was placed in 500 ml of 2-d-old tap water with 0.1 g of rabbit food. Larvae were fed 0.1 g of rabbit food daily the first 3 d and 0.3 g daily for days 4–7. When larvae molted into pupae, these were picked with a transfer pipette and placed into a petri dish inside a 30- by 30- by 30-cm insect cage. Adults were fed a nectar substitute, 10% sucrose solution, inside a 100-ml jar with a gauze pad lid, turned upside down on top of the cage.
Adult female mosquitoes were given a bloodmeal once a week. For feeding, the Mishra feeder was placed on top of the cage for 1 h. Twenty-four hours after feeding, an oviposition site was inserted into the cage. The oviposition site consisted of a 0.24-L cup with 100 ml of water, lined with a brown paper towel (egg paper); it was removed 48 h later. We separated the egg paper and kept it moist for 24 h. The egg paper was either placed in water for hatching, or stored for later use. For storage, egg paper was allowed to dry at 28°C and 50% humidity for 5 d and then placed in an envelope, at room temperature, for up to 6 mo (Gerberg et al. 1994).
An. gambiae Laboratory Colony
An. gambiae eggs were obtained from the DVBID, CDC in Fort Collins, CO. To hatch, the egg paper was rinsed into a larva tray containing 500 ml of deionized water and trace amounts of ground fish food. On day 1 (D1) after hatching, 250 ml of deionized water and larvae from the larva tray was placed in a second larva tray and deionized water was added to each tray to bring the volume to 500 ml. This process was repeated for each larva tray on D2 and D3. Trace amounts of ground fish food were sprinkled on each tray on D1–D10. Pupae were picked with a transfer pipette and placed in a petri dish with a funnel lid, inside a 30- by 30- by 30-cm insect cage. A nectar substitute, 10% sucrose solution, inside 100-ml jar with a gauze pad lid was placed upside down on top of the cage.
Adult females were fed a bloodmeal twice a week. Twenty-four hours after feeding an oviposition site was placed inside the cage. The oviposition site consists of a petri dish containing cotton wool covered with filter paper and saturated with 35 ml of deionized water. After 48 h the oviposition site was removed, and eggs hatched within 24 h.
Bacterial Strains and Culture
F. novicida strain U112 was used for all experiments. For fluorescent microscopy experiments the Francisella shuttle vector pNLFTP6-GroE-GFP (Maier et al. 2004) was transformed into U112 by using chemical transformation (Anthony et al. 1991). Bacteria were grown in tryptic soy broth (TSB) containing cysteine and dextrose overnight before exposure experiments.
Exposure of Larvae to Francisella
Less than 16 h after hatching, 20–30 larvae were transferred per petri dish containing 50 ml of deionized water and food (see above). We added 500–1,000 μl of U112 or U112 expressing green fluorescent protein(GFP)culture (2× 104–6 × 1011 CFU) to experimental dishes and 500– 1,000 μl of TSB to control dishes. The larvae were exposed to the GFP-expressing bacteria until they were collected for microscopic analysis.
Larvae at all stages of development and pupae were picked from the petri dishes using screen dippers and placed into clean dishes containing 50 ml of deionized water. They were allowed to swim for 5 min to rinse bacteria from the surface cuticle. We repeated this washing step three times. Larvae (n = 100/mosquito species) and pupae (n = 100/mosquito species) were separated for DNA extraction by placing them individually into 1.5-ml microcentrifuge tubes. We washed these samples twice with 500μl of phosphate-buffered saline (PBS) and aspirated the PBS. Pupae (n=100/mosquito species) also were placed in 15 ml of deionized water, inside an insect cage for DNA extraction from adult mosquitoes. When all adults had emerged the cage was placed in a freezer (−20°C) to kill the mosquitoes, and individual adult mosquitoes were placed into 1.5-ml microcentrifuge tubes and DNA was extracted as described below. Ae. aegypti exposure was performed in 12 individual experiments. An. gambiae exposure was performed in eight experiments, and the total sample size is shown in Table 1.
Table 1.
Detection of F. novicida DNA in Ae. aegypti and An. gambiae larvae, pupae, and adults tested for F. novicida DNA presence using qPCRa
|
F. tularensis exposed larvae
|
Unexposed larvae
|
|||||
|---|---|---|---|---|---|---|
| Larvae | Pupae | Adults | Larvae | Pupae | Adults | |
| Ae. aegypti | 50/106 | 0/137 | 0/101 | 1/101 | 4/150 | 0/100 |
| An. gambiae | 83/101 | 8/101 | 0/109 | 5/101 | 2/100 | 0/100 |
Results are listed as positive samples/total samples.
For analysis by fluorescent microscopy, larvae exposed 24 h after hatching until analysis and were washed as described above and mounted on a microscope slide before examination with a TE81 microscope (Olympus, Tokyo, Japan) with confocal capabilities.
Exposure of Adult Female Mosquitoes to Francisella
Female mosquitoes were separated into small cardboard containers and allowed to feed on an artificial bloodmeal containing F. novicida (108 CFU/ml) as described under colony maintenance. Mosquitoes that had fed were separated and collected immediately (0 h) and after 24, 48, and 72 h for DNA extraction and quantitative (q)PCR analysis.
DNA Extraction
All mosquito life stages were stored at −20°C until DNA extraction. For DNA extraction, we used the Wizard Genomic DNA Purification Kit, animal tissue protocol (Promega, Madison, WI). DNA samples were stored at −80°C.
Real-Time PCR
We used the ABI Prism 7900HT Sequence Detection System (Applied Biosystems) to test all DNA samples. FAM and SYBR Green were used as fluorescence reporters. For TaqMan analysis, the same protocol as described for testing wild-caught mosquitoes was used (see above).
qPCR reactions, using SYBR Green as the reporter, contained fopA-F and FopA-R primer (600 nM each), template, and 1× Platinum SYBR Green qPCR Super-Mix-UGD with ROX (Invitrogen, Carlsbad, CA) in 25 μl of water. After activation of UGD at 50°C for 2 min followed by ROX activation at 95°C for 10 min, the cycling conditions were as described above for the TaqMan assay followed by determination of a melting curve.
Mouse Feeding and Transmission
Mice were cared for in accordance with protocols approved by the UAF Institutional Animal Care and Use Committee (UAF-IACUC protocol 7-41). All mice were obtained from UAF animal quarters from a local breeding colony. Mice were anesthetized by intraperitoneal injection of ketamine (70 mg/kg) and xylazine (10 mg/kg), and their eyes were covered with an antibiotic salve. The anesthetized mice were placed on the mesh of the mosquito cage to allow feeding by female mosquitoes that fed on a bloodmeal containing F. novicida (108 CFU/ml) 72 h prior. After 1 h, each mouse was returned to its cage. Mice were observed for up to 7 d and then placed in a 0.95-L opaque plastic container with a gauze pad soaked in Isoflurane (0.25 ml) for euthanasia.
Calculations and Statistical Analysis
The amount of DNA in picograms was converted to genome equivalents of U112 by using the following calculation: amount of DNA (bp) = (0.978 × 109) × DNA (pg) (Dolezel et al. 2003). U112 has a 1,910,031-bp genome; therefore, 1 pg of U112 DNA is equivalent to 512 U112 genomes. Student’s t-test was used to determine statistical significance (P≤0.05) between sample groups.
Results
Is F. tularensis Present in Wild Caught Mosquitoes?
To assess the possibility of Francisella transmission by mosquitoes in the interior region of Alaska, we surveyed local mosquito populations for the presence of Francisella DNA. We captured 2,610 mosquitoes during summer 2006 in the subarctic environment around Fairbanks, AK (Fig. 1) and pooled these into samples of 10 mosquitoes. The predominant species in the Fairbanks area during the sampling period are Ochlerotatus communis (DeGeer), Ochlerotatus punctor (Kirby), Ochlerotatus diantaeus (Howard, Dyar & Knab), and Ochlerotatus excrucians (Walker), as well as Culiseta alaskaensis (Ludlow) and Culiseta impatiens (Walker). Other less frequently encountered mosquitoes include Aedes vexans (Meigen), Ochlerotatus canadiensis (Theobald), and Ochlerotatus intrudens (Dyar) (L.L.-C., D.S.S., and K.H., unpublished data).
Extracted DNA was then tested for the presence of the Francisella fopA gene by real-time qPCR (Emanuel et al. 2003). This assay detects all four subspecies of F. tularensis but does not detect F. philomiragia, a closely related species. Thirty percent of the pooled samples were positive for Francisella fopA DNA, with values ranging from 8 to 77 fg of bacterial DNA. This corresponds to 1,000–10,000 genome equivalents in the total sample of 10 pooled mosquitoes.
Forty pools that yielded positive results for Francisella had sufficient mosquito DNA for DNA Barcoding. Of these, eight species were identified, five with high confidence: Culiseta alaskaensis (n=4), Culiseta impatiens (n = 5), Ochlerotatus communis (n = 8), Ochlerotatus fitchii (Felt & Young) (n = 1), Aedes vexans (n = 1), and three without high confidence (see Discussion): Culiseta incidens (Thomson) (n = 9), Ochlerotatus pionips (Dyar) (n = 2), and Ochlerotatus excrucians (n = 6).
Do Mosquito Larvae Ingest Francisella?
Because Francisella DNA is present in a significant portion of wild-caught mosquitoes, we wanted to assess the possibility of Francisella transmission in a laboratory mosquito model. We had shown previously that F. tularensis subsp. novicida can replicate in a cell line derived from An. gambiae and that this replication depended on known virulence factors encoded in the Francisella pathogenicity island (Read et al. 2008). We therefore decided to use An. gambiae and Francisella novicida in our model. In addition to An. gambiae, we choose the medically important model mosquito Ae. aegypti as an alternative mosquito species to assess the interactions between mosquitoes and Francisella. For both mosquito species, laboratory protocols and colony maintenance is well established. In addition tropical mosquitoes cannot survive and establish in the subarctic environment of Alaska and the choice of these species added another layer of biosafety to our experiments.
Infection of mosquitoes during larval development have been mentioned in the literature as a potential mechanism for acquiring the pathogen (Vonkavaara et al. 2008). After 3 d of exposure, the larvae were washed, mounted on a microscope slide, and visualized using fluorescent microscopy. Examination of exposed larvae showed fluorescent signal in both the Ae. aegypti and An. gambiae (Fig. 2A and B), whereas no signal was detected in negative control larvae (Fig. 2C). These findings suggest that F. novicida is ingested by these mosquito species as they strain particulate matter from their watery surrounds. We did not detect an influence on larval survival due to the presence of F. novicida in the rearing water, indicating that exposure to this Francisella subspecies is not lethal to the larvae (Fig. 3).
Fig. 2.

Fluorescent microscopy of ingested bacteria. Larvae were raised in water containing F. novicida expressing GFP for 3 d, washed, fixed, and mounted on a microscope slide. (A) Digestive tract of an Ae. aegypti larva that has been exposed to a strain of U112 expressing GFP. (B) Digestive tract of an An. gambiae larva that has been exposed to a strain of U112 expressing GFP. The green fluorescent dots (arrows) indicate individual bacterium in the larval gut. (C) Digestive tract of an An. gambiae larva that has not been exposed to a strain of U112 expressing GFP. There are no individual green fluorescent dots indicating no bacteria presence.
Fig. 3.
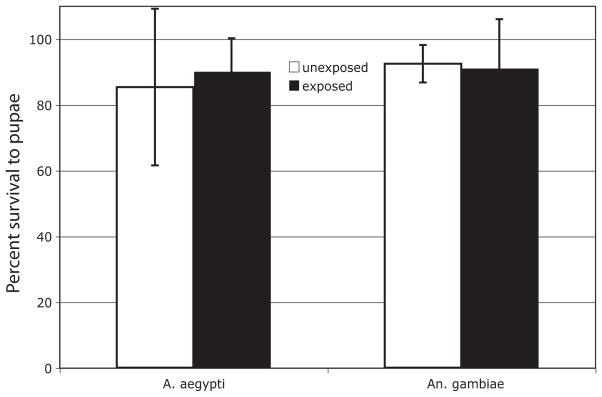
Survival of larvae after exposure to Francisella. Values represent percentage of survival of larvae to pupal stage after exposure to Francisella and standard deviation of 14 (Ae. aegypti) and 10 (An. gambiae) independent experiments.
Are Bacteria Carried Through the Molts to Pupal and Adult Stages?
We next asked whether the infected larvae retain the bacteria to the pupal and adult life stages. When we allowed infected larvae of Ae. aegypti and An. gambiae to metamorphose, there was no significant amount of F. novicida DNA in the resulting pupae or adults (Table 1). Disappearance of F. novicida DNA during the molt argues against active infection and replication of the bacteria in the pupae. Although some An. gambiae pupae tested positive for Francisella (Table 1), they contained nearly 500-fold lower amounts of Francisella DNA compared with the larvae (Fig. 4) (one-tailed t-test, df = 82, P = 0.0028).
Fig. 4.
Quantity of Francisella DNA in mosquitoes after larval exposure. Amount of DNA measured by qPCR in positive samples of life stages from two mosquito species exposed during larval development. Shown are amounts of DNA as well as the median of all for all positive Ae. aegypti larvae, An. gambiae larvae, and An. gambiae pupae. Ae. aegypti pupae and adult mosquitoes for both species were all negative and are therefore not included in this graph. Asterisk (*) indicates statistical significance (Student’s t-test; P < 0.05) between results.
Can Adult Mosquitoes Acquire Francisella With a Bloodmeal?
To assess whether feeding of female adult mosquitoes on bloodmeals containing Francisella can lead to the infection of mosquitoes and subsequent transmission to an uninfected host, Ae. aegypti and An. gambiae were fed an artificial bloodmeal containing F. novicida. Mosquitoes fed on bloodmeals containing Francisella were positive at all time points for F. novicida DNA over the first 72 h (Table 2); however, the quantity of bacterial DNA decreased over time for both mosquito species (Fig. 5A and B). The bacterial DNA in positive adults dropped by ≈4 orders of magnitude, which was observed between 48 and 72 h and approached our detection limits. This reduction in bacterial DNA level and the survival of the adult mosquitoes argue against efficient infection and replication of bacteria after a bloodmeal by female mosquitoes.
Table 2.
Detection of F. novicida DNA in Ae. aegypti and An. gambiae females allowed to feed on infected blood and tested at 24, 48, and 72 h after feeding for the presence of F. novicida DNAa
| 0 h | 24 h | 48 h | 72 h | |
|---|---|---|---|---|
| Ae. aegypti | 4/4 | 14/15 | 16/16 | 36/42 |
| An. gambiae | 7/7 | 17/18 | 16/16 | 44/49 |
Results are listed as positive samples/total samples.
Fig. 5.
Quantity of Francisella DNA in female mosquitoes after bloodmeal containing Francisella. Female Ae. aegypti mosquitoes (A) and An. gambiae (B) were allowed to feed on bloodmeals containing F. novicida. The amount of Francisella DNA was determined 0, 24, 48, and 72 h after feeding by using qPCR. Plots show quantities of DNA for all positive fed females as well as the median of all samples. Asterisk (*) indicates statistical significance (P < 0.05) between samples.
Do Mosquitoes Transmit Francisella to Mice?
After confirming bacterial DNA presence at 72 h after infection of mosquitoes, we proceeded with mousefeeding experiments; we were unable to obtain efficient feeding of female mosquitoes on mice before 3 d after the initial Francisella-containing bloodmeal and the amount of bacterial DNA in female mosquitoes dropped close to or below detection limits after 3 d (Table 2; Fig. 4). We therefore let female mosquitoes feed on mice 3 d after having a bloodmeal containing Francisella. For the Ae. aegypti feedings, one mosquito fed on the first mouse, four mosquitoes fed on the second mouse, and nine mosquitoes fed on the third mouse. For the An. gambiae feedings, seven mosquitoes fed on the first mouse, seven mosquitoes fed on the second mouse, and 19 mosquitoes fed on the third mouse. No signs of disease or changes in behavior were observed in any of the mice. Blood and spleen were harvested from each mouse and tested by qPCR for F. novicida DNA, and all samples were negative.
Discussion
Although mosquitoes have been suggested a major vector for Francisella mainly in Scandinavian countries, a laboratory model to study Francisella–mosquito interactions is missing. Here, we evaluated the presence of Francisella in mosquitoes in Alaska and assessed a laboratory model with available genomic information (An. gambiae and Ae. aegypti) to study interaction of mosquitoes and this important zoonotic agent.
Mosquitoes ingest amoebae, bacteria, and decaying organic matter during larval development (Clements 1992). Therefore, presence of U112 DNA in A. aegypti and An. gambiae mosquito larvae living in water with high U112 titers was not unexpected. We investigated whether larvae maintain bacteria to the pupal stage of development. During the molting process from larvae to pupa, the lining of the foregut and hindgut are shed (Clements 1992). The peritrophic membrane of the midgut does not get shed during molting. If the bacteria were to persist in the pupae, it would suggest hemocoelic or intracellular bacterial presence within the mosquito larva or survival in the midgut during the molting process.
After metamorphosis of the Francisella-positive larvae, the resulting pupae and adult female Ae. aegypti tested negative for U112 DNA. Thus, it is unlikely that adult Ae. aegypti are able to transmit tularemia when exposed to U112 as larvae. Similar results were obtained for these life stages of An. gambiae. Only a small percentage of pupae tested positive of Francisella DNA, and no adult mosquitoes contained detectable levels of Francisella DNA. The amounts of detectable DNA in positive pupae were significantly lower than levels in larvae. We therefore conclude that no significant amounts of bacterial DNA persist through metamorphosis.
When exposed to Francisella via a bloodmeal containing the bacteria, both Ae. aegypti and An. gambiae maintained detectable levels of Francisella DNA for at least 3 d, making transmission during a subsequent bloodmeal theoretically feasible. The decreasing amount of detected genomes, however, indicate the bacterium is not actively replicating and infecting these mosquitoes despite reported replication in an An. gambiae-derived hemocyte-like cell line (Read et al. 2008). In this previous study, we showed that F. novicida can grow exponentially in An. gambiae hemocytes; this finding was in line with early results from Francis (1927), who found Francisella in hemocytes of infected ticks. These findings as well as macrophages and other immune cells serving as the Francisella replicative niche during the infection of vertebrate hosts led us to hypothesize that hemocytes could serve as a potential replicative niche in infected mosquitoes. The findings in the study presented here indicate that the innate defense mechanism or physical barriers of the mosquito protect hemocytes from becoming a replicative niche for the bacterium after a bloodmeal containing Francisella.
Previous research tested whether adult mosquitoes could transmit tularemia (Philip 1932). In these studies, adult females (Aedes) fed on infected animals and then fed on uninfected animals. They did not transmit tularemia if allowed to finish their bloodmeal; however, when feeding on an infected host was interrupted and the mosquito completed the meal on an uninfected animal the transmission rate was ≈2% (Philip 1932). Transmission rates were greater (10%) if the adult was interrupted during the infected feeding and crushed by slapping during the completion of its bloodmeal on the uninfected host (Philip 1932). This suggests mechanical transmission in these experiments. In addition the subspecies of Francisella used in these studies is not known.
Clinical evidence (Hanke et al. 2009) and epidemiological studies (Philip 1932, Olin 1942, Eliasson et al. 2002) suggested adult mosquitoes transmit tularemia. Outbreaks in Scandinavian countries coincide with the time of year that mosquitoes are most prevalent. Within the documented cases (582 from 1931 to 1938), >80% were women with lesions on their legs. This was in a geographic region where women commonly wore short skirts baring their legs during summer. The remaining cases were men, with the majority of lesions on their hands, face, and neck; they wore long pants and sleeves. None of the patients interviewed remember being bitten by anything other than mosquitoes (Olin 1942). Amore recent study outlined an outbreak of tularemia in Sweden in 2000; matched case-control studies revealed a strong correlation of illness and mosquito bites. Most cases occurred during peak mosquito season and declined after the first frost (Eliasson et al. 2002), which is known to greatly reduce the mosquito population.
Recently, several arthropod laboratory models of Francisella infection were developed. Infection of larvae of the greater wax moth, Galleria mellonella (L.) by injecting bacteria into the developing insect led to rapid death and this model can be used to easily screen chemical compounds for their activity against Francisella (Aperis et al. 2007). In addition, a model using adult Drosophila injected with the F. holarctica derived live vaccine strain (LVS) promises to yield insight into the innate immune response to Francisella in a genetically very accessible insect model species (Vonkavaara et al. 2008). Although these models greatly increased the methods available to study arthropod–pathogen interactions, they do not address the potential for Francisella transmission by mosquitoes or other potential insect vectors.
Despite evidence suggesting transmission of tularemia by mosquitoes, the exact route of transmission remains unknown. Ae. aegypti and An. gambiae larvae ingest U112 and maintain the bacteria until they pupate. Once exposed larvae have entered the pupal stage, U112DNA is no longer present throughout their remaining life cycle. After a bloodmeal containing the bacterium, Francisella DNA can be detected for at least 3 d in some mosquitoes, but levels declined and Francisella was detected in a lower percentage of mosquitoes. However, efficient transmission to uninfected hosts was not observed. We conclude that adult Ae. aegypti or An. gambiae cannot efficiently transmit tularemia during bloodmeals after being exposed to U112 only as larvae or after a bloodmeal on a bacteremic animal. Due to the extremely large host range of Francisella (F. tularensis has been isolated from >200 species spanning several phyla; Keim et al. 2007), we believe adaptations to specific mosquito species are unlikely; however, this assumption has to be tested in future experimental studies using different mosquito species. In addition, the relatively low human case rate in areas with large mosquito populations where tularemia is endemic in wildlife populations indicates a rather inefficient transmission by this vector. Supporting this interpretation are our results of significant percentages of mosquitoes in the interior of Alaska being positive by qPCR for Francisella DNA and very low rates of reported tularemia cases. In 2007, one case was reported, and no case was reported in 2008 for the interior region of Alaska (Jenkerson 2009) with a human population of ≈104,000. In many cases, these human infections can be linked to children playing with wild hares. The first Alaska isolation of F. tularensis was from rabbit ticks. Together, these results suggest that the local mosquitoes do not efficiently transmit Francisella to humans. However, to firmly establish the efficiency of local mosquito species in transmission of tularemia this ability has to be tested in the laboratory using locally caught mosquito species. Further knowledge about differences in the presence of Francisella DNA in different mosquito species can guide such efforts to identify potentially potent vectors for Francisella.
Our positive results from pooled samples yielded identifications of eight species of mosquitoes. However, it remains possible that the positive mosquitoes were not conspecific with the identified sequences. Of the Culiseta species found, C. incidens, is an unusual find. This species is known from almost no records for interior Alaska. Darsie and Ward (2005) report it from the extreme southeast of Alaska and as far north as 65° latitude in Yukon, Canada. Its presence in interior Alaska is plausible but previously unreported in such numbers. Alternatively, these results may be DNA Barcoding misidentifications of C. alaskaensis, which shares nearly identical COI sequences. The three Culiseta species, which together represent 50% of the positive samples, differ in their biology from the remaining species in that the adults overwinter. These mosquitoes are the first adults biting in spring (April and May), larvae develop during the summer and new adults overwinter before taking a bloodmeal the following spring (Gjullin et al. 1961).
The BOLD database provided no matches for three good sequences. This is a normal result until the BOLD database has more thorough coverage and includes all extant species with 10 or more reference sequences each, representing the majority of infraspecific genetic diversity. The O. excrucians identifications were all somewhat ambiguous (99%) with close alternatives being O. stimulans (98%, not reported from Alaska but known from Yukon) or O. eudes (97%). Finally, the two O. pionips identifications were also uncertain (99%), with close alternatives being O. punctor (99%) or O. hexodontus (99%).
Although our studies failed to establish a laboratory model to study the interactions of Francisella with mosquitoes, the results suggest possibilities for surveillance of pathogenic bacteria in natural environments. Mosquitoes can be sentinels for detecting bacteria in an ecosystem independent of their vector competence. Collecting mosquitoes and testing for bacterial pathogens independent of possible transmission is a feasible approach if bacterial DNA can be detected for up to 3 d in mosquitoes that fed on a bloodmeal containing Francisella. Testing mosquitoes instead of vertebrate hosts has the advantage of easy capture by sing CO2 traps, less animal welfare issues and easier permitting. We do not know whether this approach is feasible for other bacterial pathogens. Currently, mosquitoes are mainly tested for pathogens that are known to be transmitted by this arthropod vector.
Acknowledgments
We thank Lisa McGilvary and Sarah Reiling for excellent technical support and Barry Miler for providing mosquito eggs to establish colonies at University of Alaska Fairbanks. We also thank Richard Darsie for confirmation of mosquito identifications. This publication was made possible by National Institutes of Health National Center for Research Resources grant RR016466.
Footnotes
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of the National Institutes of Health or National Center for Research Resources.
References Cited
- Anthony LS, Gu MZ, Cowley SC, Leung WW, Nano FE. Transformation and allelic replacement in Francisella spp. J Gen Microbiol. 1991;137:2697–2703. doi: 10.1099/00221287-137-12-2697. [DOI] [PubMed] [Google Scholar]
- Aperis G, Burgwyn Fuchs B, Anderson CA, Warner JE, Calderwood SB, Mylonakis E. Galleria mellonella as a model host to study infection by the Francisella tularensis live vaccine strain. Microbes Infect. 2007;9:729–734. doi: 10.1016/j.micinf.2007.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements AN. The biology of mosquitoes. Chapman & Hall; London, United Kingdom: 1992. [Google Scholar]
- Darsie RF, Jr, Ward RA. Identification and geographical distribution of the mosquitoes of North America, North of Mexico. University Press of Florida; Gainesville, FL: 2005. [Google Scholar]
- Darling RG, Catlett CL, Huebner KD, Jarrett DG. Threats in bioterrorism. I: CDC category A agents Emerg Med Clin North Am. 2002;20:273–309. doi: 10.1016/s0733-8627(02)00005-6. [DOI] [PubMed] [Google Scholar]
- Dolezel J, Bartos J, Voglmayr H, Greilhuber J. Nuclear DNA content and genome size of trout and human. Cytometry A. 2003;51:127–128. doi: 10.1002/cyto.a.10013. [DOI] [PubMed] [Google Scholar]
- Eldridge BF, Edman JD. Medical entomology: a textbook on public health and veterinary problems caused by arthropods. Kluwer Academic; Dordrecht, The Netherlands: 2003. [Google Scholar]
- Eliasson H, Lindback J, Nuorti JP, Arneborn M, Giesecke J, Tegnell A. The 2000 tularemia outbreak: a case-control study of risk factors in disease-endemic and emergent areas, Sweden. Emerg Infect Dis. 2002;8:956–960. doi: 10.3201/eid0809.020051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emanuel PA, Bell R, Dang JL, McClanahan R, David JC, Burgess RJ, Thompson J, Collins L, Hadfield T. Detection of Francisella tularensis within infected mouse tissues by using a hand-held PCR thermocycler. J Clin Microbiol. 2003;41:689–693. doi: 10.1128/JCM.41.2.689-693.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsman M, Sandstrom G, Jaurin B. Identification of Francisella species and discrimination of type A and type B strains of F. tularensis by 16S rRNA analysis. Appl Environ Microbiol. 1990;56:949–955. doi: 10.1128/aem.56.4.949-955.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis E. Microscopic changes of tularaemia in the tick Dermacentor andersoni and the bed bug Cimex larius. Public Health Rep. 1927;42:2763–2772. [Google Scholar]
- Gerberg EJ, Barnard DR, Ward RA. Manual for mosquito rearing and experimental techniques. Am Mosq Control Assoc. 1994:98. [Google Scholar]
- Gjullin CM, Sailer RI, Stone A, Travis BV. Agriculture Handbook No 182. USDA, Agricultural Research Service; Washington, DC: 1961. The mosquitoes of Alaska. [Google Scholar]
- Hanke CA, Otten JE, Berner R, Serr A, Splettstoesser W, von Schnakenburg C. Ulcer-oglandular tularemia in a toddler in Germany after a mosquito bite. Eur J Pediatr. 2009;168:937–940. doi: 10.1007/s00431-008-0862-3. [DOI] [PubMed] [Google Scholar]
- Hubalek Z, Halouzka J. Mosquitoes (Diptera: Culicidae), in contrast to ticks (Acari: Ixodidae), do not carry Francisella tularensis in a natural focus of tularemia in the Czech Republic. J Med Entomol. 1997;34:660–663. doi: 10.1093/jmedent/34.6.660. [DOI] [PubMed] [Google Scholar]
- Jenkerson SA. Bulletin, Section of Epidemiology. Division of Public Health, Department of Health and Social Services; State of Alaska: 2009. 2008 Annual (January–December) Infectious Disease Report; p. 14. [Google Scholar]
- Keim P, Johansson A, Wagner DM. Molecular epidemiology, evolution, and ecology of Francisella. Ann NY Acad Sci. 2007;1105:30–66. doi: 10.1196/annals.1409.011. [DOI] [PubMed] [Google Scholar]
- Lehane MJ. The biology of blood-sucking in insects. Cambridge University Press; Cambridge, NY: 2005. [Google Scholar]
- Maier TM, Havig A, Casey M, Nano FE, Frank DW, Zahrt TC. Construction and characterization of a highly efficient Francisella shuttle plasmid. Appl Environ Microbiol. 2004;70:7511–7519. doi: 10.1128/AEM.70.12.7511-7519.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra K, Kumar Raj D, KHazra R, Dash AP. A simple, artificial-membrane feeding method for the radio-isotope labelling of Aedes aegypti polypeptides in vivo. Ann Trop Med Parasitol. 2005;99:803–806. doi: 10.1179/136485905X65189. [DOI] [PubMed] [Google Scholar]
- Olin G. The occurance and mode of transmission of tularemia in Sweden. Acta Pathol Microbiol Scand. 1942;19:220–247. [Google Scholar]
- Olsufev NG. Human diseases with natural foci. Foreign Languages Publishing House; Mosow, Russia: 1966. Tularemia. [Google Scholar]
- Olsufjev NG, I, Meshcheryakova S. Infraspecific taxonomy of tularemia agent Francisella tularensis McCoy et Chapin. J Hyg Epidemiol Microbiol Immunol. 1982;26:291–299. [PubMed] [Google Scholar]
- Petersen JM, Schriefer ME. Tularemia: emergence/ re-emergence. Vet Res. 2005;36:455–467. doi: 10.1051/vetres:2005006. [DOI] [PubMed] [Google Scholar]
- Petrishcheva PA. Vectors of diseases of natural foci. Vol. 54. Israel Program for Scientific Translation; Israel: 1965. [Google Scholar]
- Philip CB. Experimental transmission of tularemia by mosquitoes. Public Health Rep. 1932;47:12. [Google Scholar]
- Read A, Vogl SJ, Hueffer K, Gallagher LA, Happ GM. Francisella genes required for replication in mosquito cells. J Med Entomol. 2008;45:1108–1116. doi: 10.1603/0022-2585(2008)45[1108:fgrfri]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Rohmer L, Fong C, Abmayr S, Wasnick M, Larson Freeman TJ, Radey M, Guina T, Svensson K, Hayden HS, Jacobs M, et al. Comparison of Francisella tularensis genomes reveals evolutionary events associated with the emergence of human pathogenic strains. Genome Biol. 2007;8:R102. doi: 10.1186/gb-2007-8-6-r102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saslaw S, Carlisle HN. Studies with tularemia vaccines in volunteers. IV Brucella agglutinins in vaccinated and nonvaccinated volunteers challenged with Pasteurella tularensis. Am J Med Sci. 1961;242:166–172. doi: 10.1097/00000441-196108000-00004. [DOI] [PubMed] [Google Scholar]
- Versage JL, Severin DD, Chu MC, Petersen JM. Development of a multitarget real-time TaqMan PCRassay for enhanced detection of Francisella tularensis in complex specimens. J Clin Microbiol. 2003;41:5492–5499. doi: 10.1128/JCM.41.12.5492-5499.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vonkavaara M, Telepnev MV, Ryden P, Sjostedt A, Stoven S. Drosophila melanogaster as a model for elucidating the pathogenicity of Francisella tularensis. Cell Microbiol. 2008;10:1327–1338. doi: 10.1111/j.1462-5822.2008.01129.x. [DOI] [PubMed] [Google Scholar]





