Abstract
A 44 year old female presented with an intraoral soft tissue swelling in the retromolar region, which was painless, mobile and fluctuant in nature. Computed tomography as well as preoperative ultrasound revealed thick walled cystic lesion. The lesion was clinically diagnosed as mucocele. Ultrasound guided fine needle aspiration was done, which revealed turbid, straw colour fluid. This cystic swelling was completely excised and histopathologically identified to be low grade Mucoepidermoid carcinoma. This unusual presentation of Mucoepidermoid carcinoma as an intraoral cyst is one of the rare and unique reported case.
Keywords: Cyst, mucoepidermoid carcinoma, mucocele, malignant minor salivary gland tumor
INTRODUCTION
Mucoepidermoid carcinoma (MEC) is the most common malignant neoplasm of major and minor salivary glands. MEC is reported to manifest variable biologic aggressiveness, basically showing correlation with its histological features and is graded by a 3-tiered system.[1]
In 1945, Stewart et al.,[2] recognized MEC of the salivary gland as a separate entity among salivary neoplasm. MEC is thought to arise from pluripotent reserve cells of the excretory ducts of salivary gland that have the potential to differentiate into squamous, columnar, mucous cells, clear cells, and epidermoid cells. Although no specific etiologic factors have been identified, exposure to ionizing radiation has been reported in some cases. MEC account for good number of all salivary gland tumors, commonly arising within the parotid gland and is the most common malignant tumor to arise in children and adolescents under 20 years of age.[3] The tumor presents as firm to hard mass and is usually asymptomatic. Pain is associated with high grade malignant tumors. Most of the time they do not cause facial nerve paralysis when they occur in parotid gland.
Majority of the MEC in children are well differentiated or grade I neoplasm. Low grade MEC has a better 5 year survival rate of 92–100% compared to high-grade MEC with 0–43% survival rate. An overall incidence of lymph node involvement ranges from 18–28%.[4] Postoperative local recurrence is more likely to occur in patients with positive margins regardless of the grade.[5]
The gross appearance varies with the grade of the tumor. Low-grade mucoepidermoid tumor presents as well-circumscribed though unencapsulated ovoid masses usually 2–4 cm in diameter. On gross examination, solid gray-white or gray-pink areas are mixed with mucous-filled macro cysts, while intermediate grade neoplasms are grossly similar but lack macrocysts. High-grade tumors may be similar in size and presentation but are not well circumscribed and infiltration is often evident. They do not contain macro cysts although hemorrhage and necrosis lead to areas of cystic degeneration.
Minor salivary glands are found in all the areas of oral mucosa with an exception of anterior portion of palate and gingiva. These minor salivary glands are often involved in tumor formation constituting a small portion of salivary gland tumors. The salivary gland tumors account for 5% of head and neck neoplasms. The minor salivary gland tumors almost account for 14–22% of all salivary gland carcinomas. Most of the tumors arising from these minor salivary glands are malignant.[6]
The most common presenting symptom is a slowly enlarging painless mass of several years duration clinically mimicking a pleomorphic adenoma or other benign neoplasm. Pain and tenderness along with rapid enlargement may be seen with high-grade lesions. The clinical presentation of MEC can be submucosal, subdermal, or central. Central MECs are rare with less than 100 cases having been reported.[7] The cystic presentation of MEC is very rare and attributed to cystic degeneration of the central cells or accentuation of macrocysts, which are characteristic feature of MEC. We report on an unusual unique case of MEC in an adult, presenting as a retromolar mucocele.
CASE REPORT
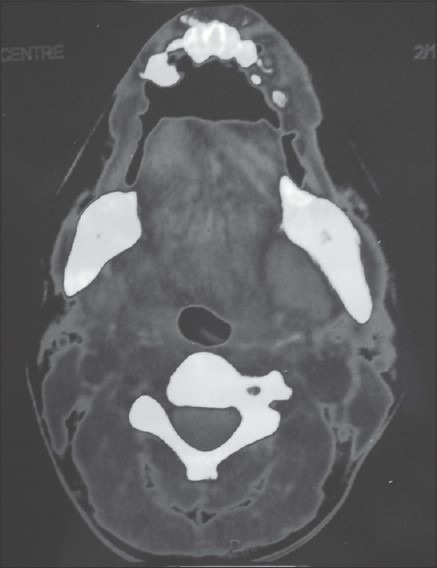
A 44-year-old female presented with painless intraoral swelling in left retromolar area since 2 years. This swelling was gradually increasing in size with time. Clinical examination revealed a 2 cm smooth, spherical swelling at left retromolar region, which was normothermic, non-tender, soft in consistency, fluctuant, fluid-filled, bluish in color with stretched mucous membrane [Figure 1]. Regional lymph nodes were not palpable.
Figure 1.

Clinical photograph showing intraoral soft tissue swelling in the left retromolar region bluish in colour with diffuse margins and stretched mucous membrane.
Ultrasound examination showed a thick walled cystic space occupying lesion in the floor of mouth in left submandibular region. Blood examination revealed hemoglobin 12.2 gm/dl, chest X-ray was normal. Ultrasound-guided fine needle aspiration was done using 18 G needle, which revealed hazy, straw color fluid. Aspirate was sent for fluid analysis, which revealed amorphous nature of fluid without presence of cells. After aspiration size of swelling reduced significantly. Blood picture was non contributory to any systemic pathology. Preoperative clinical diagnosis of retention cyst of salivary gland was made. Surgical excision was planned but unfortunately patient did not turn up for next appointment as swelling was reduced after aspiration.
After 2 years patient again visited with the same complaint of intraoral swelling since 3 months. Size of swelling was increased significantly to 4 cm extending from left retromolar region to left maxillary tuberosity. CT scan revealed hypodense non-enhancing lesion medial to left mandibular angle. The imaging gave a conclusion remark of possibilities such as mucocele, lymphangioma, or necrotic lymph node [Figures 2 and 3].
Figure 2.
Computed Tomography (CT) scan showing a cystic lesion present medial to the angle of the mandible.
Figure 3.
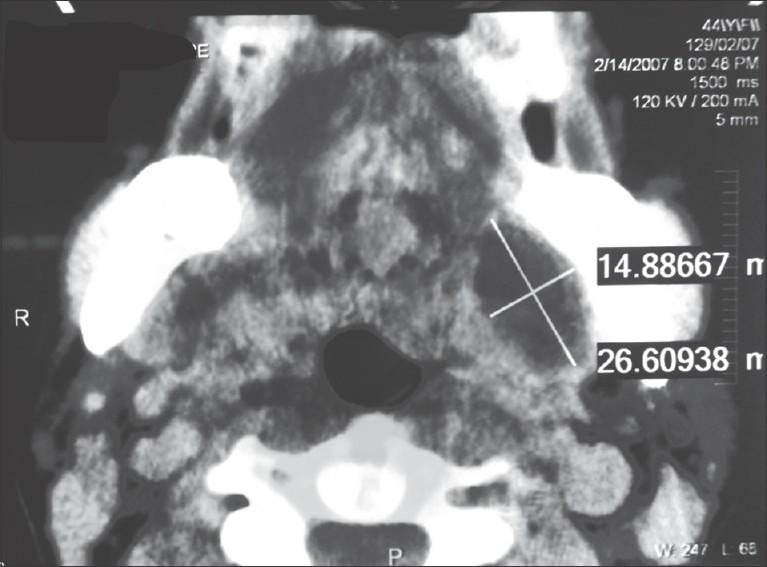
Contrast CT scan showing cystic lesion medial to the angle of the mandible measuring 1.5 cm × 2.6 cm.
Clinical diagnosis of mucocele was made and surgical excision was planned via submandibular approach. Under general anesthesia left submandibular incision was given. Blunt dissection was done to expose left submandibular gland. Care was taken to preserve marginal mandibular nerve. Cystic sac was identified on medial aspect of angle of mandible. Blunt dissection was performed to gently free sac from adjacent soft tissue attachments. Cystic sac was excised [Figure 4], with care taken to prevent any damage to cyst wall. Intraoral examination was done to check for complete enucleation. Hemostasis was achieved and closure was done in layers. Specimen was marked and sent for histopathological examination.
Figure 4.
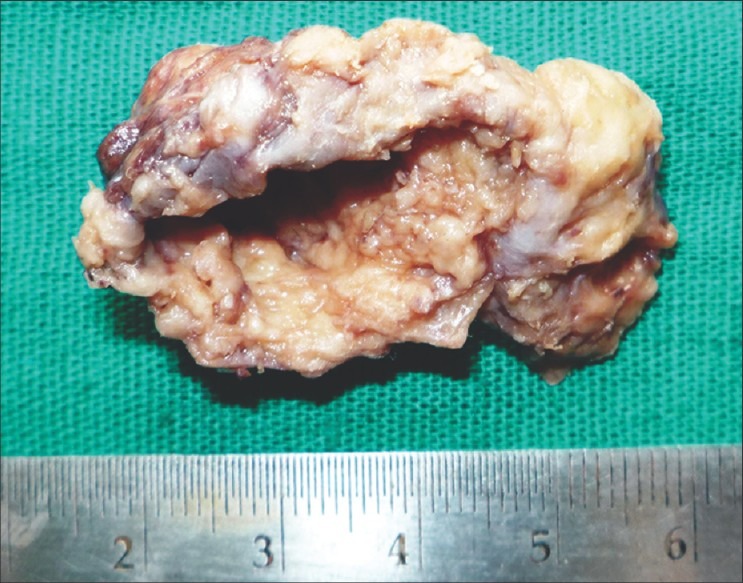
Gross examination showing a cystic lesion, roughly oval in shape, creamish brown in color, and nodular surface.
Patient was discharged after 3 days of observation. Follow-up revealed uneventful healing without any major complications or recurrence. A follow-up of 15 months was uneventful.
Histopathology
The histopathology picture showed a large macrocystic area lined by the dysplastic epithelial cells. The connective tissue capsule was thick with a variety of patterns presented by the dysplastic epithelial cells. Large sheets with syncytial arrangement of cells, small nests and islands, single strands of cells forming India file and reticular pattern. The connective tissue showed a dense lymphocytic response with formation of germinal centers. Very few microcysts were seen. The unique feature histopathologically is that the tumor showed all types of cell differentiation: epidermoid, squamous, intermediate, mucus, clear, and columnar cells forming variety of epithelial patterns [Figures 5 and 6].
Figure 5.
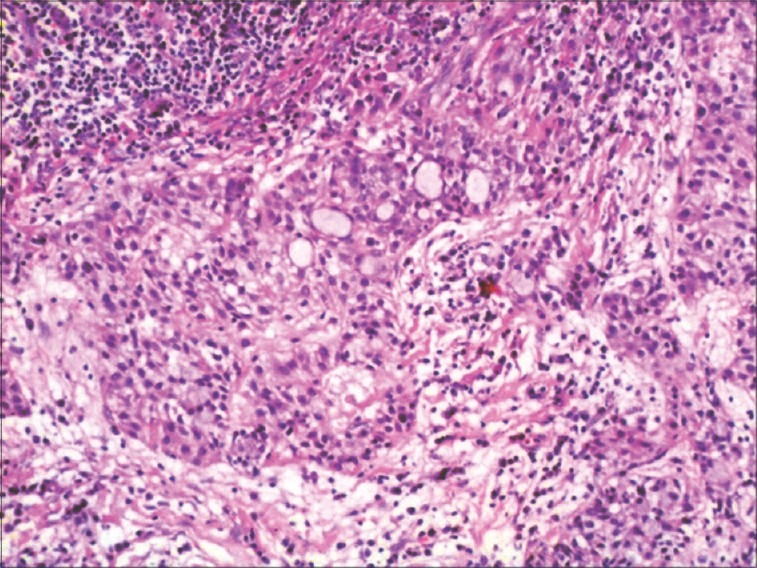
Photomicrograph showing malignant epidermoid cells, intermediate cells and mucous cells forming microcystic areas. Chronic inflammatory cell infiltrate is seen (H and E, 10×).
Figure 6.
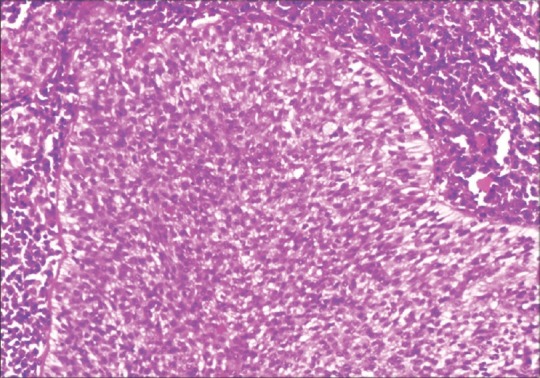
Photomicrograph showing syncytial arrangement of intermediate cells, and presence of columnar, mucous, and epidermoid cells (H and E, 10×).
DISCUSSION
Salivary gland tumours account for 5% of head and neck neoplasm with mucoepidermoid carcinoma as the most common malignant tumor.[3,6] Mucoepidermoid carcinoma is the most common malignant salivary gland neoplasm in children and adolescence and is rarely found in children under the age of 10 years.[6] Up to 35% of all salivary neoplasms in children are malignant, and 60% of these are MEC.
Tumors of the minor salivary glands account for 10–15% of all salivary gland neoplasms.[8] The most common complaint is a painless swelling in the mouth (60%), with symptoms having been present for more than 12 months. The most common sites for tumors of minor salivary gland origin are the palate, buccal mucosa, and upper lip, which accounts for more than 75% of cases. The palate is the most common site for all tumors of minor salivary gland origin (55%) and more than 60% of these are malignant.
MEC was first described by Volkman in 1895, which was further elaborated upon by Stewart in 1945 as mucoepidermoid tumor. The credit of naming the tumor as MEC goes to Foot and Frazell (1953). The MEC can be associated with major salivary glands, minor salivary glands, and can also occur as an intraosseous tumor frequently called as central MEC.[9]
The common age group for the occurrence of MEC in males and females is around 43 years. The overall female predilection has been seen many number of times. The gender difference is extremely pronounced in patients with lesions of the tongue and retromolar area. The females outnumber the males by 76–80%. The 46% of MEC's occurring intraorally in the minor salivary glands arise in a variety of location including ectopic salivary gland tissue. Most of the cases are frequently seen to be associated with palate, cheek, mandible, lip, and tongue. Lesser number of MECs are associated with retromolar area, oropharynx, and ectopic salivary gland.
The MEC in minor salivary glands are generally slowly developing lesions which are asymptomatic with a history lasting from 1½ to 10 years.
The clinical presentation of MEC of minor salivary gland is protean and defies concise description. Many lesions present as small solid masses, or as a soft tissue lesion with granular or papillary surfaces and ulcerated lesions. Some of the MEC present as bluish or red-purple, fluctuant, smooth surfaced mass, which appear very similar to mucocele.
The present case was unusual, presenting as a large mucocele but in a typical gender and age group. The middle aged woman showed a prolonged, slow progression of tumor formation, misleading the patient and the clinician.
In histopathology, MECs are characterised by a variety of growth patterns and cell types. These two basically form the basis for diagnosis and grading of the MEC. The tumor presents mucous, epidermoid, intermediate, columnar, and clear cells, which are arranged in a combination of cystic and solid patterns.[10] The cell population of a specific type is important in grading of the MEC. Previously, a two grade system of low and high was used; later a third intermediate grade was introduced. The 3-tier system of grading MEC is universally accepted.
Histopathologically, macro and microcystic patterns with mucous and intermediate cells helped in diagnosis and grading. The case differs from others as it shows all the six cell differentiation, which is uncommon. The epithelial patterns were also many and unique to low grade MEC.
The differential diagnosis for MEC is generally to distinguish it from other salivary gland tumors like adenosquamous carcinoma, polymorphous low grade carcinoma, and squamous cell carcinoma. In MEC, the recurrence rate is approximately 25% and 10% in low grade lesions. Metastasis and survival rate are related to the histological grade and stage. The treatment for MEC in minor salivary glands is primarily surgical. A wide excision with removal of underlying bone if involved is recommended.
In present case, unusual clinical presentation of MEC as intraoral benign cyst lead us to design the surgical procedure conservatively. The excised mass resembles a thick walled, tense sac completely filled with fluid. The specimen was grossly giving impression of cyst. Histopathological diagnosis of MEC necessitated radical approach with either neck dissection or radiotherapy or both. Patient was referred to radiologist for postsurgical radiotherapy. The patient followed up for 15 months without any recurrence noted.
This case is unique in its own because it not only proves histopathology as the surgeons’ third eye but also it enlightens remoulding the treatment plan according to pathology report.
CONCLUSION
The clinical course of minor salivary gland carcinomas is variable and often characterised by late relapse. The early diagnosis and treatment of minor salivary gland carcinomas leads to a better outcome and prognosis. The MEC often masquerades as a benign or inflammatory condition, hence clinicians must be aware of the differential diagnosis to be considered. Many of the cases of minor salivary gland carcinomas are referred from multidisciplinary clinics. Awareness of this entity in a mucocele like presentation is important for dental practitioners.
Although typical clinical picture of MEC is reported by various authors; the tumour can show diversity in clinical and histopathological presentation. The benign clinical appearance not only leads to less radical treatment but also risks further complications. Thus, we report this cystic presentation of MEC, which may in future guide surgeons for perfect differentiation. In this case the diversity of clinical picture and microscopic reality lead us to combat the tumor from all fronts successfully.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bernardes VF, Ramos-Jorge ML, Carmo MA, Cardoso SV, Mesquita RA, Aguiar MC. Intraoral mucoepidermoid carcinoma of salivary glands: Lack of association among clinicopathological features and immunoexpression of c-erbB-2 in 29 cases. Int J Morphol. 2008;26:1005–11. [Google Scholar]
- 2.Baker SR, Malone B. Salivary Gland malignancy in children. Cancer. 1985;55:1730–6. doi: 10.1002/1097-0142(19850415)55:8<1730::aid-cncr2820550819>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 3.Margaret SB, Katya I, Derrick IW. Muco epidermoid carcinoma. A clinicopathologic study. Am J Surg Pathol. 2001;25:835–45. doi: 10.1097/00000478-200107000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Guzzo M, Andreola S, Sirizzotti G, Cantu G. Mucoepidermoid carcinoma of the salivary glands: Clinicopathologic review of 108 patients treated at the National Cancer Institute of Milan. Ann Surg Onocol. 2002;9:688–95. doi: 10.1007/BF02574486. [DOI] [PubMed] [Google Scholar]
- 5.Pires FR, de Almeida OP, de Araújo VC, Kowalski LP. Prognostic factors in head and neck mucoepidermoid carcinoma. Arch Otolaryngol Head Neck Surg. 2004;130:174–80. doi: 10.1001/archotol.130.2.174. [DOI] [PubMed] [Google Scholar]
- 6.Spiro RH. Management of malignant tumours of the salivary glands. Oncology. 1998;12:671–80. [PubMed] [Google Scholar]
- 7.García CJ, Flores PA, Arce JD, Chuaqui B, Schwartz DS. Ultrasonography in the study of salivary gland lesions in children. Pediatr Radiol. 1998;28:418–25. doi: 10.1007/s002470050375. [DOI] [PubMed] [Google Scholar]
- 8.Vander Poorten VL, Balm AJ, Hilgers FJ, Tan IB, Keus RB, Hart AA. Stage as major long-term outcome predictor in minor salivary gland carcinoma. Cancer. 2000;89:1195–204. doi: 10.1002/1097-0142(20000915)89:6<1195::aid-cncr2>3.3.co;2-a. [DOI] [PubMed] [Google Scholar]
- 9.Jansisyanamont P, Blanchaert RH, Ord RA. Intraoral minor salivary gland neoplasms: A single institution experience of 80 cases. Int J Oral Maxillofac Surg. 2002;31:257–61. doi: 10.1054/ijom.2002.0223. [DOI] [PubMed] [Google Scholar]
- 10.Dardick I. Colour Atlas. Text of Salivary gland tumour pathology. 2001:163–77. [Google Scholar]


