Abstract
Introduction:
Obstructive sleep apnea (OSA) is often associated with congenital craniofacial malformations such as Pierre-Robin Syndrome, Hemifacial Microsomia, Treacher Collins Syndrome resulting in decreased pharyngeal airway, which, in severe cases, leads to tracheostomy dependence. Some pediatric patients had tracheostomies done and others with severe respiratory distress were considered tracheostomy candidates.
Materials and Methods:
Twelve patients with severe respiratory distress without tracheostomy and ten patients with tracheostomy were treated by mandibular distraction osteogenesis using either external or internal devices. The expansion of mandibular framework was analyzed using bony cephalometric landmarks and computed tomography (CT).
Results:
The results demonstrated average mandibular elongation of 29 mm on each side using the external devices and 22 mm using the internal devices, and an increase in mandibular volume and pharyngeal airway. The group of patients with tracheostomies were decannulated and in the patients with respiratory distress there was improved airway with improvement of signs and symptoms of OSA with elimination of oxygen requirement.
Conclusions:
Mandibular distraction is a useful method in younger children with OSA expanding the mandible and concomitantly advancing the base of tongue and hyoid bone increasing the pharyngeal airway. The external devices permit greater distraction length, the removal is simple but the devices are uncomfortable for the patients. On the other hand, the internal devices are more comfortable for patients but permit shorter distraction length and require a second operation for removal.
Keywords: Mandibular distraction osteogenesis, obstructive sleep apnea, tracheostomy
INTRODUCTION
Children with microretrognathia may develop respiratory distress caused by glossoptosis resulting in obstructive sleep apnea (OSA). The anatomic obstruction along the entire airway can lead to cardio-pulmonary arrest and even death.[1–3] Tracheostomy is traditionally the safest and most effective treatment option though associated with frequent morbidity, and occasional mortality.[2–4]
A new advance in the treatment of micrognathia, is mandibular distraction osteogenesis, in which the tongue base is advanced anteriorly via its muscular attachments to the mandible, relieving pharyngeal airway obstruction. Distraction osteogenesis has been used successfully to treat OSA.[5–9]
The purpose of this study is to present the management of respiratory distress and tracheostomy dependent pediatric patients with OSA due to micrognathia and upper airway obstruction by mandibular distraction osteogenesis using internal and external devices.
MATERIALS AND METHODS
Twenty-two children with age ranging from six months to eight years with craniofacial anomalies associated with micrognathia and OSA underwent mandibular distraction in an attempt to relieve severe upper airway obstruction [Figure 1]. Twelve patients with severe complaints of OSA and ten patients had tracheostomy placed were treated. Some patients were treated by bilateral external distraction devices and some were treated by bilateral internal distraction devices. Each patient was evaluated before and after distraction of the mandible by lateral cephalograms, and head and neck CT in axial and sagittal planes [Figure 2].[10–14]
Figure 1.

Two year old boy with Pierre Robin Syndrome associated with severe mandibular hypoplasia and obstructive sleep apnea with permanent tracheostomy
Figure 2.
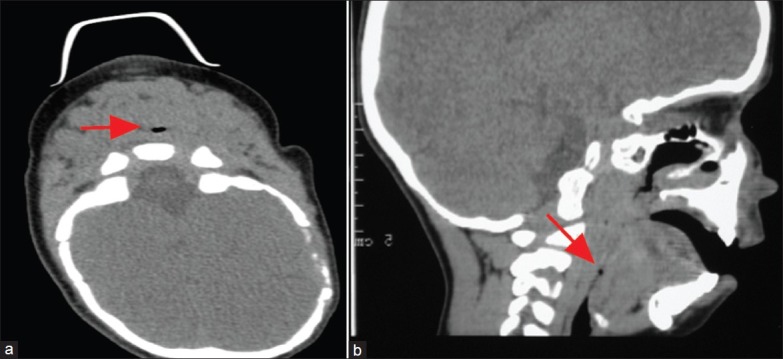
Axial CT (a) and sagittal CT (b) show the obstruction of the airway (arrows)
The lateral cephalometric X-rays and CT scans in lateral aspects reveal mandibular hypoplasia that causes retroposition of the base of the tongue and inadequate pharyngeal space. Polysomnographic sleep studies revealed respiratory disturbance index greater than 10 apneas per hour and oxygen saturation less than 85%.
The operation for external devices (Unidirectional Distraction Device, KLS Martin, Tuttlingen, Germany) was performed intraorally by an incision at the buccal vestibulum exposing the lateral surface of the mandibular body between the mental nerve anteriorly and gonial area posteriorly. In order to advance the mandible, the osteotomy was performed in the mandibular body just anterior to the gonial angle, taking care not to damage the adjacent teeth or tooth buds. While planning a forward distraction vector, two extraoral pins were placed bi-cortically through the cheek across the planned osteotomy line and two extraoral unidirectional mandibular devices were fixed on each side of the mandible [Figure 3]. It is important to place the device parallel to the mandibular body in order to advance the retruded mandible. When the internal device was used, a submandibular retroangular approach was used, exposing the lateral surface of the mandibular body between the mental nerve anteriorly and gonial area posteriorly. An osteotomy was performed anterior to the gonial angle and two internal unidirectional mandibular devices were fixed on each side of the mandible.
Figure 3.

At the end of the operation after bilateral mandibular distraction with unidirectional extraoral devices
The patients with severe OSA were maintained several days in intensive care unit for monitoring the postoperative airway and oxygen saturation until the swelling reduced and the distraction was initiated.
After four days of latency period, gradual lengthening of the mandible was done on both sides at a rate of 1 mm per day as necessary until slight overcorrection of the occlusion commenced, followed by 10 weeks retention period [Figures 4 and 5]. The amount of mandibular advancement was measured by the distraction device on each side and by cephalometric measurements.
Figure 4.

After bilateral mandibular distraction before commencement of lengthening. (a) Anterior view (b) Lateral view
Figure 5.

At the end of 30 mm of bilateral forward distraction of the mandible. (a) Anterior view (b) Lateral view
The preoperative and postoperative pharyngeal airway were measured from sagittal and axial images before surgery and compared to the CT done after distraction and decannulation. Endoscopic visualization of upper airway was completed before decannulation.
The patients were followed clinically and by polysomnography for the following 12-24 months. Polysomnography was performed for all children one month after removal of the distraction devices and compared to the polysomnography before distraction. After the 10 weeks of consolidation period, the external distraction devices were removed by simple unscrewing of the pins and the internal devices were removed in a second operation.
RESULTS
The average amount of mandibular advancement was 29 mm with the external devices and 22 mm with the internal devices [Figure 5]. The mandible developed marked advancement with slight overcorrection during distraction. The devices were removed after 10 weeks of latency period. All patients’ dental occlusion was slightly overcorrected.
The panoramic X-rays demonstrate the mandibular body osteotomy and the amount of bone lengthening. The cephalometric analysis demonstrated advancement of the hyoid bone along the axis of mandibular body after distraction in all patients of an average of 10 mm with the external devices and 8 mm with the internal devices. The axial and sagittal CT after mandibular distraction in all patients demonstrated marked increase in lateral and axial pharyngeal width [Figure 6].
Figure 6.
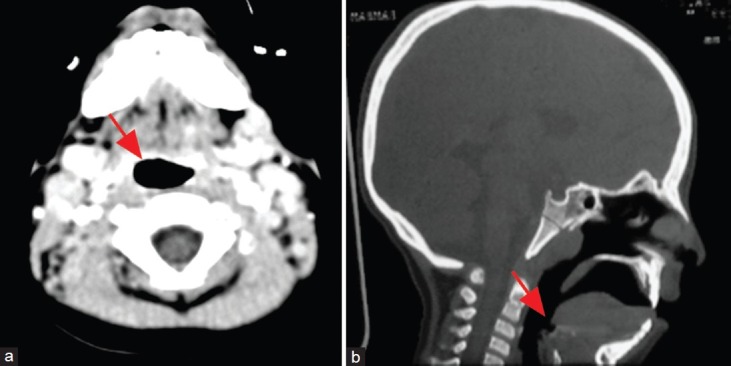
The post distraction (a) axial CT and (b) sagittal CT show the increased airway (arrows)
Following distraction, in all 12 patients in respiratory distress there was improvement in symptoms of OSA and all ten patients with tracheostomies were decannulated successfully at the end of the retention period and removal of the distraction device [Figure 7]. After decannulation, the oxygen saturation level rose to over 93% in all patients with marked clinical improvement in signs and symptoms of sleep apnea. The Respiratory Disturbance Index (RDI) was less than 3 episodes per hour in all the patients.
Figure 7.

Two years of follow up following tracheostomy decannulation: Adequate subsequent mandibular growth and no need for tracheostomy
DISCUSSION
Children with craniofacial anomalies and mandibular hypoplasia are at high risk for upper airway obstruction in the neonatal period. Symptoms range in severity from increased fragmentation of sleep and OSA to continuous upper airway obstruction. The children have a retruded mandible and glossoptosis that often compromise upper airway, a condition with potential for morbidity and mortality.[2,15,16] In severe cases, the children are treated by permanent tracheostomy. Long-standing tracheostomies are associated with high morbidity such as tracheomalacia, chronic bronchitis, laryngeal stenosis and risk of death due to mucus plug or dislodgement of tracheostomy tube. Moreover, patients who undergo tracheostomy require complex nursing care.[2,17,18]
Some reviews have supported the use of distraction for OSA in patients with mandibular deficiency.[5,6,7,8,9] In a retrospective study, four tracheostomy dependent children were successfully decannulated after mandibular distraction osteogenesis.[5] Dealing with children with congenital malformation associated with mandibular deficiency we propose that overcorrection of lengthening of the mandible is preferable in the treatment of OSA. During the growth of the children, the orthodontist is able to adapt the occlusion and if necessary to restrict the mandibular growth.
Post distraction polysomnograms showed an improvement in the apnea indexes for all children and reduced symptoms of OSA. Using the external distraction devices the operation was performed intraorally using an extraoral device. External devices permit greater distraction length, the removal is simple by unscrewing the pins, but they are uncomfortable for the patients.
In severe obstructive sleep apnea, mainly in children without tracheostomy, extraoral devices are preferred over the intraoral devices. The extraoral devices are better anchored in the two bone stumps of both sides of the osteotomy by bi-cortical pins and can be better controlled during distraction osteogenesis. The extraoral devices may distract for longer distance than intraoral devices and can change the vector of lengthening by using bidirectional or multiplanar distraction devices. Another advantage of the extraoral devices is that they can be changed to another device if necessary and there is no need for a second operation under general anesthesia to remove the device as with the intraoral devices. However, the internal devices are more comfortable for the patients but permit shorter distraction length, have less control on the vector of lengthening and need second operation for removal.
The vector of lengthening should be forward in order to advance the mandible and hyoid bone forward, therefore the device should be parallel to the mandibular body.
Application of mandibular distraction osteogenesis is an important component in treatment of OSA and permits mandibular advancement in younger children. The role of distraction osteogenesis in treatment of OSA is better defined with the experience gained in distraction osteogenesis and vector control.
In sagittal CT, the hyoid bone was demonstrated to be advanced between 8 and 10 mm enabling opening of the pharyngeal airway.
In conclusion, bilateral mandibular distraction is a useful method in younger children in order to improve airway for patients suffering from respiratory distress and in order to decannulate permanent tracheostomy by expanding the mandible and concomitantly advancing the base of tongue and hyoid bone, increasing the pharyngeal airway.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tomaski SM, Zalzal GH, Saal HM. Airway obstruction in the Pierre Robin sequence. Laryngoscope. 1995;105:111–4. doi: 10.1288/00005537-199502000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Guilleminault C. Obstructive sleep apnea syndrome and its treatment in children: Areas of agreement and controversy. Pediatr Pulmonol. 1987;3:429–36. doi: 10.1002/ppul.1950030610. [DOI] [PubMed] [Google Scholar]
- 3.Cohen SR, Simms C, Burstein FD, Thomsen J. Alternatives to tracheostomy in infants and children with obstructive sleep apnea. J Pediatr Surg. 1999;34:182–6. doi: 10.1016/s0022-3468(99)90253-1. discussion 187. [DOI] [PubMed] [Google Scholar]
- 4.Sidman JD, Sampson D, Templeton B. Distraction osteogenesis of the mandible for airway obstruction in children. Laryngoscope. 2001;111:1137–46. doi: 10.1097/00005537-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Williams JK, Maull D, Grayson BH, Longaker MT, McCarthy JG. Early decannulation with bilateral mandibular distraction for tracheostomy-dependent patients. Plast Reconstr Surg. 1999;103:48. doi: 10.1097/00006534-199901000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Mandell DL, Yellon RF, Bradley JP, Izadi K, Gordon CB. Mandibular distraction for micrognathia and severe upper airway obstruction. Arch Otolaryngol Head Neck Surg. 2004;130:344–8. doi: 10.1001/archotol.130.3.344. [DOI] [PubMed] [Google Scholar]
- 7.Monasterio FO, Drucker M, Molina F, Ysunza A. Distraction osteogenesis in Pierre Robin sequence and related respiratory problems in children. J Craniofac Surg. 2002;13:79–83. doi: 10.1097/00001665-200201000-00018. discussion 84. [DOI] [PubMed] [Google Scholar]
- 8.Denny AD, Talisman R, Hanson PR, Recinos RF. Mandibular distraction osteogenesis in very young patients to correct airway obstruction. Plast Reconstr Surg. 2001;108:302–11. doi: 10.1097/00006534-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Morovic CG, Monasterio L. Distraction osteogenesis for obstructive apneas in patients with congenital craniofacial malformations. Plast Reconstr Surg. 2000;105:2324–30. doi: 10.1097/00006534-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Ono I, Ohura T, Narumi E, Kawashima K, Matsuno I, Nakamura S, et al. Three-dimensional analysis of craniofacial bones using three-dimensional computer tomography. J Craniomaxillofac Surg. 1992;20:49–60. doi: 10.1016/s1010-5182(05)80468-8. [DOI] [PubMed] [Google Scholar]
- 11.Girod S, Keeve E, Girod B. Advances in interactive craniofacial surgery planning by 3D simulation and visualization. Int J Oral Maxillofac Surg. 1995;24:120–5. doi: 10.1016/s0901-5027(05)80872-0. [DOI] [PubMed] [Google Scholar]
- 12.McCance AM, Moss JP, Fright WR, James DR, Linney AD. A three dimensional analysis of soft and hard tissue changes following bimaxillary orthognathic surgery in skeletal III patients. Br J Oral Maxillofac Surg. 1992;30:305–12. doi: 10.1016/0266-4356(92)90180-q. [DOI] [PubMed] [Google Scholar]
- 13.Kawamata A, Fujishita M, Nagahara K, Kanematu N, Niwa K, Langlais RP. Three-dimensional computed tomography evaluation of postsurgical condylar displacement after mandibular osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:371–6. doi: 10.1016/s1079-2104(98)90059-2. [DOI] [PubMed] [Google Scholar]
- 14.Rachmiel A, Aizenbud D, Pillar G, Srouji S, Peled M. Bilateral mandibular distraction for patients with compromised airway analyzed by three-dimensional CT. Int J Oral Maxillofac Surg. 2005;34:9–18. doi: 10.1016/j.ijom.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Cosman B, Crikelair GF. Mandibular hypoplasia and the late development of glossopharyngeal airway obstruction. Plast Reconstr Surg. 1972;50:573–9. doi: 10.1097/00006534-197212000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Dattilo DJ. The mandibular trapezoid osteotomy for the treatment of obstructive sleep apnea: Report of a case. J Oral Maxillofac Surg. 1998;56:1442–6. doi: 10.1016/s0278-2391(98)90413-x. [DOI] [PubMed] [Google Scholar]
- 17.Argamaso RV. Glossopexy for upper airway obstruction in Robin sequence. Cleft Palate Craniofac J. 1992;29:232–8. doi: 10.1597/1545-1569_1992_029_0232_gfuaoi_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 18.Cohen SR, Simms C, Burstein FD. Mandibular distraction osteogenesis in the treatment of upper airway obstruction in children with craniofacial deformities. Plast Reconstr Surg. 1998;101:312–8. doi: 10.1097/00006534-199802000-00008. [DOI] [PubMed] [Google Scholar]


