Abstract
Ten cleft lip and palate patients with complete unilateral (five patients) and bilateral (five patients) clefts were treated by a multidisciplinary team integrated by psychologists, surgeons, orthodontists, prosthodontists, pediatric dentists, and speech pathologists, to obtain ideal soft tissue and hard tissue continuity, facial symmetry, functional and esthetic dentitions, excellent nasal architecture, subtle, and hidden lip scars. No hypernasality and adequate social adaptation were found in the 30 years follow-up (20-30 years follow-up with an average of 25.5 years). The patients were treated in a pro-active fashion avoiding complications and related problems, executing the ideal surgical, dental, and speech therapy plan, based on a close follow-up over the entire period. Those patients treated at the right time required less surgeries and less salvaging maneuvers and presented complete dentitions with less dental prosthesis or dental implants and stable occlusions, than those who missed the ideal dental and surgical treatment opportunities. The focus of this article is the need of a close long-term follow-up to ensure an ideal patient's quality of life.
Keywords: Cleft lip, cleft palate, hypernasality, alveolar bone grafting, dental occlusion, velo-pharyngeal incompetence, pharyngeal flap, posterior palate reposition, long-term follow-up, team work
INTRODUCTION
Cleft lip and palate surgery has been a challenge through centuries, basically because what seems to be perfect in the beginning deforms during growth and development ruining the initial patient, family, and doctors expectations. Second, because the more aggressive the surgery is, the soft tissues′ retraction and deformation increases. Another issue is the timing for the different interventions, if it is performed too early, growth would be impaired, and if too late the teeth eruption and maxillary growth could be permanently endangered.[1]
Different cleft lip and palate centers around the world propose so many different treatment protocols; mostly based on personal egos and the need to coin names, cities, or universities, but basically, some with minimal variations, quite often misguiding the newer surgeons into misleading protocols.[2–6] Time is usually magic, is placing things in the right place through history, and tells what is right and what it is not; time and only time demonstrate if the interventions were positive and how growth and development accompanies the treatments. The journals had their pages printed over and over again with the same techniques that appear and later on, disappear, to be printed again years later with the same ideas, principles, and repetitions.[2,7] Easy examples have been: primary bone grafting in the newborn with iliac crest bone grafts or multiple z-plates crossing the lip philtrum columns against Millard advance and rotation ideal design[2,8–11] or primary periosteoplasty with major incisions and flap movements in the newborn with severe post-surgical retraction, limiting maxillary growth, and poor or no bone cleft alveolar development and still requiring alveolar bone grafting between ages of 5 and 9 years (according to the teeth eruption),[4] this is particularly true after the use of cone beam bone scan, where most patients have no bone for maxillary stability, continuity, and nasal alae support; or when to decide to move the teeth across with orthodontics or to decide for a dental implant; obviously some surgical techniques do not include bone grafts; as a consequence no dental implant can be placed, some with major periodontal soft tissue retractions and teeth loss.[4,12]
Perhaps, the most crucial issue is: surgeons trying new ideas in newborns, children, or adolescents, whatever the new technique, variation or personal touch, they could not be evaluated until the patients reach the end of growth. That is why is so important to force, oblige, or demand the non-expert surgeons not to try new ideas until he or she has become a master in the traditional techniques and create variations or plan innovations on a previous wide experience, and base the protocol changes in the Gillies[13] and Millard surgical principles[11,14,15] and sound biological concepts, also to plan accordingly to the newer oral and maxillofacial concepts to obtain ideal dentitions.
The multidisciplinary protocol needs to have certain flexibility to accommodate patients with very low income, limited intelligence, those living in communities away from the medical and dental coverage, and those victims suffering from mala praxis and experimental surgery. We will include some ideas for these groups of patients. The education of cleft lip and palate surgery needs to be tutorial with extensive exposure to patients and to expert surgeons with years of experience demonstrating the best surgical techniques. Surgical safaris or short trips to poor communities to "help" the cleft patients with inadequate surgeries, and worst of all, no long-term follow-up would not allow the novel surgeon to understand the growth and development of the jaws, the speech, and psychological personality, this is not acceptable nowadays. Actually, there are several centers in Latin America with surgical groups that permanently return to the underdeveloped cities to control the surgical outcomes and continuing with the chain of surgeries required, this situation could benefit the patients and the training surgical centers, with positive outcomes for the sick patient and the learning surgeons; again, the compromise between the traveling surgical teams must be to integrally treat the cleft lip and palate individual, including the regular secondary problems, as speech therapy, otological problems treatment, also the paramount importance of the dental specialties to complete treatments to reach the ideal dentition. The most common problems encountered in the adult cleft patients are as follows: oro-nasal fistulas, dental malocclusions, incomplete anterior teeth, speech substitutions, omissions, and distortions; also breathing limitations, snoring, hypoacusia, nasal septal deviation and lip and nose abnormalities secondary to poor surgical design, execution, inadequate technical management, excessive scarring, infection secondary to the surgical environment, postoperative care and management, and poor patient selection, this is especially true in the underdeveloped countries with children in hunger and presenting vitamin deficiencies.[4,16]
Our cleft lip and palate surgeries were performed as late as possible but still as early as needed. The initial lip surgery was postponed up to 3-6 months, understanding that the tissues grow so fast, and a millimeter surgical defect when the child is born will become into a one-centimeter by the end of growth.[17] The first palate surgery was delayed until the orthodontists had created an ideal maxillary arch, with progressive soft tissue improvement utilizing the orthopedics plates, indirectly, a minimal soft tissue surgery would be then required, since the wide cleft transformed into a minimal line in the mid-palate; the more aggressive the surgery is, the more healing retraction will happen, creating small maxillas with crossbites and possible fistulas and inadequate alveolar tissues to create a proper anterior seal.[18–21] The patient needs to have an ideal speech by the time he goes to school, between the ages of 4 and half and 5 years, delaying this could permanently limit the speech development. The primary dentition should be maintained free of caries and periodontal disease, orthopedics plates should stimulate maxillary growth and align the anterior maxilla waiting the teeth eruption up to the age of 5-8 when the lateral incisor, central, or canine could be in the development stage to indicate the alveolar bone grafting and solve the eruption problem, avoiding impacted teeth, fistulas, lack of maxillary continuity, and maxillary peri-nasal deficiency, mixed dentition orthodontics is indicated to bring all the teeth into the maxillary arch, align, and level them.[22] Definitive orthodontics would be necessary once the dentition is completed and the patient has reached the age of 14 or 15 years, when maxillo-mandibular osteotomies combined with orthodontics; and prosthodontics could be indicated and completed to replace missing teeth in the cleft area.[23–25]
Psychology evaluation is fundamental for the family to understand the problem and for the child to adapt socially, living with the malformation and sequential treatment, there is so much a specialist in the field can help to prevent personality disorders.
The cleft palate surgery needs to be divided into three areas: (1) The soft palate must be closed with adequate muscle reconstruction[26] and posterior repositioning before the 18th month of life, because the ear function and the primary sphincter closure are fundamental to prevent ear infections and develop the language. Using vomerian flaps could help creating a nasal layer and avoid future oro-nasal fistulas.[27–30] The hard palate could have been reduced and alveolar segments aligned utilizing orthopedics appliances; reducing the severity of flap elevation and surgical wound tension; consequently, less healing retraction and better maxillary growth after surgery. (2) The hard palate surgery could be performed between the ages of 3 and 5 years old, so far the children are using acrylic plates to conform the maxilla and obturate the anterior palate, and carefully following speech therapy. A fourth palatal intervention could be needed to treat velo-pharyngeal incompetence, superiorly based pharyngeal flap, pharyngoplasty, or posterior palate repositioning by push-back techniques or bone transport via distraction osteogenesis.[31–34]
Alveolar cleft reconstruction and grafting is fundamental to allow, maxillary stability, adequate teeth eruption, orthodontics finishing, nasal ala support, and esthetic smile.[35,36] Primary periosteoplasty usually fails to conform an integral alveolar shape to comply with the basic biological requirements, teeth cannot erupt though the fibrous scar tissue, incomplete bone leads to periodontal disease and inadequate site for implant placement for those missing the central, lateral, or canine teeth. This was recently demonstrated in detail by cone-beam radiology or CT scan, where there could be integrity in the soft tissue, but not adequate bone to move teeth orthodontically or insert dental implants, also secondary maneuvers to bone graft or improve the soft tissue quantity and quality are sterile, since the periodontal ligament serves to communicate saliva and bacteria into the grafting material, producing infection and severe gingival retraction.[21]
Soft tissue surgery for the lip and nose must take into consideration the growth and development, retraction, poor scarring, visible marks, and removing tissue should be avoided, understanding that in the new born, all tissues are misplaced and as general rule, tissue removal is contraindicated. Meticulous and detailed careful surgery must be carried out in order not to produce major retractions, asymmetries, or deficient areas.
MATERIALS AND METHODS
All cleft patients and families (five unilateral and five bilateral) were instructed to follow a protocol including A primary team evaluation with systematic explanation of the problem, how to be treated, different specialties involved, timing of different treatment interventions, complete family inclusion in all phases of treatment, and psychological support is advisable. We initiate the treatment utilizing orthopedic maxillary plates with nasal extensions to lengthen the columella and improve the lateral cartilage shape, continuing with Millard's rotation and advancement technique for the unilateral and Victor Veau straight line for the bilateral cleft lips, a secondary orbicularis muscle reconstruction will be needed, between 3 and 6 months of age. Before the year has elapsed, a posterior palate soft tissue closure is performed, by a muscle reconstruction and nasal and oral mucosa layered flaps, vomerian flaps are tailored, elevated and closed, at the same surgical stage. Orthopedics appliances are utilized to act as obturator as well as to promote maxillary growth and segments alignment. This treatment allows anterior cleft palate reduction, tongue good positioning, and speech development. The required anterior palatal surgery is minimized and easy palatal flaps elevations and medial closure would be done without much retraction or postoperative fistulas. The patients were instructed to follow an aggressive speech therapy protocol, since 9-12 months of age, to develop a proper language and different exercises were given to follow with the family, until perfect and adequate velo-pharyngeal closure was obtained and language was free of omissions, distortions, and substitutions. The patients should have had an excellent speech development or secondary interventions have to be performed by 5 years of age. Detailed 3D CT scan to analyze the velopharyngeal mechanism helps in deciding to choose from Superior repositioning pharyngeal flaps, posterior palate distraction osteogenesis, or secondary pushback palatoplasty.
Orthodontics is one of the fundamental pillars to create an ideal facial growth and development and excellent dentition, the minimally aggressive surgery, and the correct timing for maxillary guidance and stimulation. The orthodontics is divided into four phases:
Predentition orthopedics
Primary dentition orthopedics
Mixed dentition orthodontics
ermanent dentition orthodontics
These four phases were instituted separately, acrylic splints and fixed appliances needed to be in placed for exact periods of time, and never meant to stayed all through the growing years. The orthodontics mechanics were applied as long as needed and as short as possible; understanding the damage and consequences in terms of carious teeth, periodontal disease, teeth loss, patient discomfort, and economics, when the braces were maintained over the time required [Figure 1].
Figure 1.
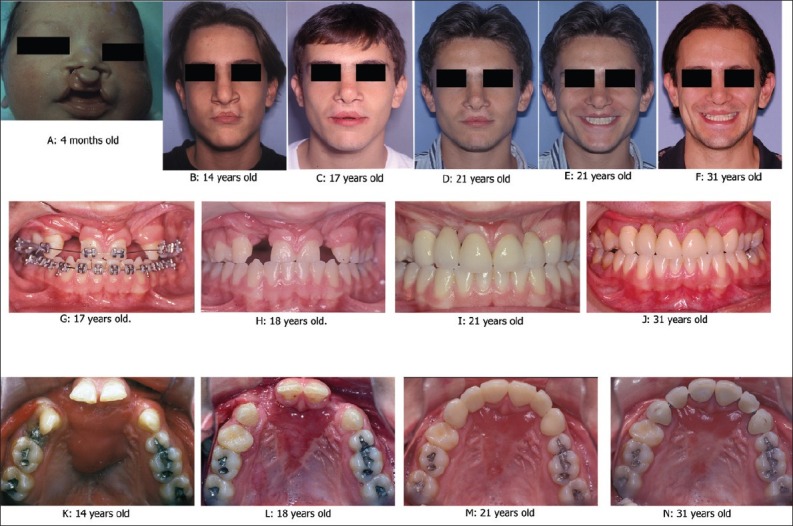
Age changes with treatment in case 1. Refer text for treatment plan
If treatment protocol was not followed, extra surgical interventions, teeth loss, and increased morbidity were observed. A unilateral and another bilateral patients will illustrate the salvaging maneuvers to overcome the short coming expected secondary to poor maxillary growth and hypernasality.
RESULTS
All patients in the study were followed between 20 and 30 years, completing every treatment protocol phase, until the cleft patient showed ideal facial esthetics, excellent dental occlusions, no hypernasality, and adequate social adaptation [Figure 2]. The unilateral cleft patients underwent Millard's rotation and advancement rhino-cheiloplasties and Boyne's alveolar bone grafting. The cleft palate was treated by Schwekendieck palatoplasty adding vomerian flaps. To obtain final ideal occlusions: 3 out of 10 required no dental implants, their occlusion were managed by orthodontics; 2 out of 10 missed lateral incisors and replaced by osseointegration fixtures, and 1 out of 10 required a fixed prosthesis. The bilateral cleft patients underwent Veau straightline rhino-cheiloplasty, the cleft palate were treated by Schwekendieck palatoplasty, and all bilateral clefts required a secondary surgery lip surgery for orbicularis oris reconstruction and central lip tubercle reconstruction. Uni- and bilateral clefts needed complete orthodontics treatment, as well as alveolar bone three-layer bone grafting; the parietal was the bone donor site. Four-phases orthodontics was indicated in all patients and the occlusion were finalized by prosthodontics and teeth whitening.
Figure 2.
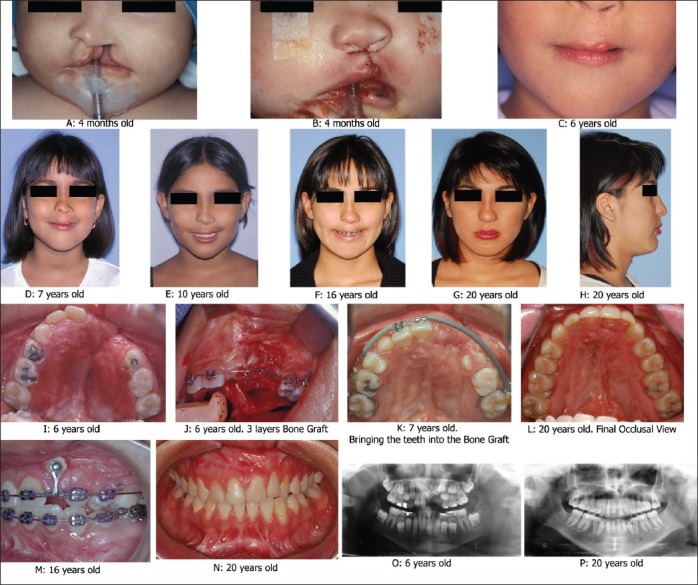
Age changes with treatment in case 2. Refer text for treatment plan
All patients finished college level and 80% continue to a University degree, all patients developed adult couple relationships, and 80% were married or were married at one point in time. Two females, the younger in the group, even though they have different couple relationships, still are not married.
DISCUSSION
Those patients who lived in a cosmopolitan city with first-level medical care and who their parents were in the health field or there was enough motivation from the surgical team had a much better treatment outcome; every phase of the treatment was completed and their final result required less surgery, with minimally aggressive interventions and complete dentitions with less dental implants, or compromised occlusions. It is a very long treatment with multiple specialists interventions,[22] important economic investment, and continuous visit through so many years; there is a tendency to get tired, stop treatment phases, interrupt the dental or speech therapies, and to ignore the need for further surgeries to improve details that show through the facial growth and development. Obviously, the economy factor plays a major role in continuing and completing every phase of the protocol.[5] A word of caution is given to the different world team, in relation to include the parents from the beginning and be clear and explain in detail the whole treatment plan, emphasizing the importance of timing, multiple specialists, and show the family the final outcomes, since the patient is in the womb, up to 18 years of treatment; if the family do not see every step in the major protocol objectives, they will not follow the treatment phases and will go from one surgical team to another, with a poor predictability and usually falling into the adventurous surgeons, who will try “new procedures” and will never have the true tender and loving care that the cleft patient needs and only the historic cleft teams would have. The new specialists have to start working in a well-established team and learn by observation and through years of experience dedicate entirely to this group of patients, those surgeons, orthodontists, and speech pathologists who do not execute their expertise constantly will never devote to the Excellency, the details, and sophisticated ways to obtain the perfection, the ideal, to reach the next level of completion.
The cleft team must start with the final objectives in written; the child must be seen at age 16-18 years old, with ideal lip and nose morphology (in rest and functional positions), perfect dental occlusion, complete dentition, no fistulas, language with no hypernasality, distortions, omissions or substitutions, normal breathing, and no sleep apnea. These objectives need to be clear in every specialist or technician involved with the patient, and when in doubt, bring the patient to the team evaluation.[22]
The main reason why most of the cleft patients have a limited or mediocre result is related to different facts: (1) a single specialist direct the treatment protocol, (2) economy is an issue, not to complete every aspect of the treatment, (3) poorly informed patient that quits the treatment protocol, (4) lack of multispecialists evaluation, where the surgeon evaluates areas outbound of his competency, this is very common in relation to surgeons speech outcomes analysis, an outside Speech Pathologist report would uncover severe shortcomings, and (5) patients living in faraway communities and non-intelligent families, who do not take the patient to the health centers or do not comprehend the importance of complying with the protocol.
CONCLUSIONS
The cleft lip and palate patient needs to be evaluated, treated, and critically analyzed by a competent Cleft Team; the minimal follow-up is 18 years, to understand the outcomes of the established protocol dictated by the particular team. It takes that time to be able to truthfully see the mistakes and the successes that a protocol may have to offer. New procedures, technical variations, to apply new materials or ideas require 18 years follow-up to see the true results, those results need to be revised by outsiders to warranty the benefits enunciated by the pioneer. It is fundamental to respect the cleft patient and family, keeping clear in the cleft team that no innovation should be tried in novel hands; they have to be carried out by expert surgeons after team approval and with responsibility followed until a certain benefit is extrapolated to other cleft teams. Our group of patients (five complete unilateral and five bilateral cleft lip and palate) were followed between 20 and 30 years, with an average of 24.6 years; and the major emphasis other than applying historic surgical techniques with excellent background, the speech therapy and the dental treatments were ideally finalized. Orthodontics was divided into four phases timing, and prosthodontics was utilized to obtain ideal dental occlusions. Those patients living near the health care centers and intelligent parents had a better evolution and better outcome, than those living faraway or parents reluctant to comply with all phases of the treatment protocol. The long-term follow-up demonstrated the treatment protocol efficiency to all team members.
ACKNOWLEDGEMENT
I acknowledge the guidance, knowledge and expertise shared by Late Dr. Jose Barros-St-Pasteur, a double degree Maxillofacial Surgeon and my uncle.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pruzansky S. Description, classification, and analysis of unoperated clefts of the lip and palate. Am J Orthod. 1953;39:590. [Google Scholar]
- 2.Veau V. Traitement du bec-de-lievre simple: Procédé de M. Jalaquier. Presse Méd. 1910;18:825–7. [Google Scholar]
- 3.Millard DR., Jr Preservation of natural landmarks in unilateral cleft lip. J Am Med Assoc. 1959;169(2):133–4. doi: 10.1001/jama.1959.73000190001009. [DOI] [PubMed] [Google Scholar]
- 4.Tessier P, Delbet JP, Pastoriza J, Aiaich R. Labial and nasal sequelae of the complete harelip in adolescents.Relations with malformations and deformities of the maxilla. Ann Chir Plast. 1969;14:312–27. [PubMed] [Google Scholar]
- 5.Turvey TA, Vig K, Moriarty J, Hoke J. Delayed bone grafting in the cleft maxilla and palate: A multidisciplinary analysis. Am J Orthod. 1984;86:244–56. doi: 10.1016/0002-9416(84)90376-2. [DOI] [PubMed] [Google Scholar]
- 6.Schweckendiek W. Primary closure of cleft lip and cleft palate. Zahnarztl Prax. 1983;34:317–20. [PubMed] [Google Scholar]
- 7.Veau V, Borel S. Division Palatine.Anatomie Chirurqie, Phonetique. Paris: Masson. 1931 [Google Scholar]
- 8.Veau V. Operative treatment of complete double harelip. Ann Surg. 1922;76:143–56. doi: 10.1097/00000658-192208000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Millard DR., Jr A radical rotation in single harelip. Am J Surg. 1958;95(2):318–22. doi: 10.1016/0002-9610(58)90525-7. [DOI] [PubMed] [Google Scholar]
- 10.Millard DR Jr. The triad of Columella deformities. Plast Reconstr Surg. 1963;31(4):370–84. doi: 10.1097/00006534-196304000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Millard DR., Jr Rotation-advancement principle in cleft lip closure. Cleft Palate J. 1964;12:246–52. [PubMed] [Google Scholar]
- 12.Schweckendiek H. The problem of early and late surgery in congenital fissure of the of the lips and palate. Z Laryngol Rhinol Otol. 1951;30:51–6. [PubMed] [Google Scholar]
- 13.Gillies HD. London, England: Frowde; 1920. Plastic Surgery of the Face. [Google Scholar]
- 14.Millard DR., Jr Refinements in rotation-advancement cleft lip technique. Plast Reconstr Surg. 1964;33:26–38. doi: 10.1097/00006534-196401000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Millard DR., Jr The unilateral cleft lip nose. Plast Reconstr Surg. 1964;34:169–75. doi: 10.1097/00006534-196408000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Salyer KE. Early and late treatment of unilateral cleft nasal deformity. Cleft Palate Craniofac J. 1992;29:556–69. doi: 10.1597/1545-1569_1992_029_0556_ealtou_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 17.Salyer KE. Primary correction of the unilateral cleft lip nose: A 15-year experience. Plast Reconstr Surg. 1986;77:558–68. doi: 10.1097/00006534-198604000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Guerrero CA, Bell WH. Intraoral distraction. In: McCarthy JG, editor. Distraction of the craniofacial skeleton. New York: Springer-Verlag; 1999. pp. 219–48. [Google Scholar]
- 19.Guerrero CA, Bell WH, Gonzalez M, Meza L. Intraoral distraction osteogenesis. In: Fonseca R, editor. Oral and Maxillofacial Surgery. Philadelphia: WB Saunders; 2000. pp. 343–402. [Google Scholar]
- 20.Guerrero CA. Intraoral bone transport in clefting. Oral Maxillofac Surg Clin North Am. 2002;14:509–23. doi: 10.1016/s1042-3699(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 21.Guerrero CA, Gonzalez M, Lopez PE, Bell WH, Dominguez E, Figueroa F. Oral and Maxillofacial Surgery. In: Fonseca RJ, Turvey TA, Marciani RD, editors. Intraoral Distraction Osteogenesis. 2nd ed. Elsevier Health Sciences; 2008. pp. 338–63. [Google Scholar]
- 22.American Cleft Palate-Craniofacial Association. Parameters for the evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies. Cleft Palate Craniofac J. 1993;30(Suppl 1):4. [PubMed] [Google Scholar]
- 23.Epker BN, Wolford LM. Middle-third facial osteotomies: Their use in the correction of congenital dentofacial and craniofacial deformities. J Oral Surg. 1976;34:324–42. [PubMed] [Google Scholar]
- 24.Fonseca RJ, Turvey TA, Wolford LM. Oral and maxillofacial surgery. In: Fonseca RJ, Baker SJ, Wolford LM, editors. Orthognathic surgery in the cleft patient. PA: W.B. Saunders; 2000. pp. 87–146. [Google Scholar]
- 25.Millard DR., Jr Wide and/or short cleft palate. Plast Reconstr Surg Transplant Bull. 1962;29:40–57. doi: 10.1097/00006534-196201000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Furlow LT., Jr Cleft palate repair by double opposing Z-plasty. Plast Reconstr Surg. 1986;78:724–38. doi: 10.1097/00006534-198678060-00002. [DOI] [PubMed] [Google Scholar]
- 27.Schweckendiek H. Zur zwiphasigen gaumenspalten operation bei primarem velumverschluss. Fortschr Kiefer Gesichtschir. 1955;1:73–6. [Google Scholar]
- 28.Schweckendiek W, Doz P. Primary veloplasty: Long term results without maxillary deformity. A twenty-five years report. Cleft Palate J. 1978;15:268–74. [PubMed] [Google Scholar]
- 29.Schweckendiek W. The technique of early veloplasty and its results. Acta Chir Plast. 1966;8:188–94. [PubMed] [Google Scholar]
- 30.Furlow LT., Jr Flaps for cleft lip and palate surgery. Clin Plast Surg. 1990;17:633–44. [PubMed] [Google Scholar]
- 31.Schendel SA, Oeschlaeger M, Wolford LM, Epker BN. Velopharyngeal anatomy and maxillary advancement. J Oral Maxillofac Surg. 1979;7:116–24. doi: 10.1016/s0301-0503(79)80023-5. [DOI] [PubMed] [Google Scholar]
- 32.Lopez P, Guerrero C. Posterior palate repositioning by distraction osteogenesis in clefts. Oral surg oral med oral patho. 2009;108:523. [Google Scholar]
- 33.Schweckendiek W. Long Term Treatment in Cleft Lip and Palate. In: Kehrer B, Slongo T, Graf B, Bettex M, editors. Speech development after two-stage closure of cleft palate. Bern: Hons Huber; 1981. pp. 307–14. [Google Scholar]
- 34.Schweckendiek W. Results of formation of a maxilla and speech after primaryveloplasty. Arch Ohren Nasen Kehlkopfheilkd. 1962;180:541–6. [PubMed] [Google Scholar]
- 35.Harsha BC, Turvey TA, Powers SK. Use of autogenous cranial bone grafts in maxilofacial surgery: A preliminary report. J Oral Maxillofac Surg. 1986;44:11–5. doi: 10.1016/0278-2391(86)90008-x. [DOI] [PubMed] [Google Scholar]
- 36.Millard DR Jr. Complete unilateral clefts of the lip. Plast Reconstr Surg Transplant Bull. 1960;25:595–605. [PubMed] [Google Scholar]


