Abstract
Background
The Cub and Sushi Multiple Domains 1 (CSMD1) gene, located on the short arm of chromosome 8, codes for a type I transmembrane protein whose function is currently unknown. CSMD1 expression is frequently lost in many epithelial cancers. Our goal was to characterize the relationships between CSMD1 somatic mutations, allele imbalance, DNA methylation, and the clinical characteristics in colorectal cancer patients.
Methods
We sequenced the CSMD1 coding regions in 54 colorectal tumors using the 454FLX pyrosequencing platform to interrogate 72 amplicons covering the entire coding sequence. We used heterozygous SNP allele ratios at multiple CSMD1 loci to determine allelic balance and infer loss of heterozygosity. Finally, we performed methylation-specific PCR on 76 colorectal tumors to determine DNA methylation status for CSMD1 and known methylation targets ALX4, RUNX3, NEUROG1, and CDKN2A.
Results
Using 454FLX sequencing and confirming with Sanger sequencing, 16 CSMD1 somatic mutations were identified in 6 of the 54 colorectal tumors (11%). The nonsynonymous to synonymous mutation ratio of the 16 somatic mutations was 15∶1, a ratio significantly higher than the expected 2∶1 ratio (p = 0.014). This ratio indicates a presence of positive selection for mutations in the CSMD1 protein sequence. CSMD1 allelic imbalance was present in 19 of 37 informative cases (56%). Patients with allelic imbalance and CSMD1 mutations were significantly younger (average age, 41 years) than those without somatic mutations (average age, 68 years). The majority of tumors were methylated at one or more CpG loci within the CSMD1 coding sequence, and CSMD1 methylation significantly correlated with two known methylation targets ALX4 and RUNX3. C:G>T:A substitutions were significantly overrepresented (47%), suggesting extensive cytosine methylation predisposing to somatic mutations.
Conclusions
Deep amplicon sequencing and methylation-specific PCR reveal that CSMD1 alterations can correlate with earlier clinical presentation in colorectal tumors, thus further implicating CSMD1 as a tumor suppressor gene.
Introduction
Colorectal cancer is the third most common cancer with approximately 1 million annual cases worldwide [1]. This complex disorder is normally characterized by an abundance of somatic mutations [2]. However, every tumor has its own unique mutational landscape [3], and the underlying mechanisms that give rise to this diverse landscape are poorly understood. Activating mutations in the adenomatous polyposis coli (APC), Kirsten ras (KRAS), and Phosphatidylinositol 3-kinase (PIK3CA) genes are very common in colorectal cancers [4]. It is likely that the right combination of mutations could give a particular clone of cells a proliferative advantage. Mutations that cause or contribute to tumor progression are commonly referred to as drivers, whereas mutations that offer no selective advantage are commonly referred to as passengers [5], [6], [7]. The majority of somatic mutations that accumulate in tumors are silent passengers [8], [9], whereas small subsets of mutations are actual drivers [10], [11]. By assuming that all silent (synonymous) mutations are passengers, the background rate of somatic mutations in colorectal cancers has been approximated to be 1 mutation per megabase [12]. Genes that are more frequently mutated than the predicted background rate may be drivers of neoplastic development. By assuming that all silent mutations are passengers and that non-silent (nonsynonymous) mutations may either be drivers or passengers, the overall ratio of nonsynonymous to synonymous (NS/S) mutations in a given gene can provide additional evidence as to whether that gene is under positive or negative selection for changes to the amino acid sequence. Genes that accumulate mutations, yet are under no selective pressure, have an expected nonsynonymous to synonymous (NS/S) ratio of approximately 2∶1. This expected ratio is based upon the first two nucleotide positions in the codon dictating the encoded amino acid and the third “wobble” position allowing for codon redundancy. This mechanistic setup of the genetic code creates twice as many opportunities for a given single nucleotide substitution to change the amino acid sequence as there are opportunities to substitute a nucleotide yet preserve the amino acid sequence. Genes with an overrepresentation of non-synonymous mutations have a NS/S ratio that is statistically significantly higher than the expected 2∶1 and can confidently be assumed to be under positive selective pressure to change the amino acid sequence during the process of tumor evolution [13]. Therefore, a high NS/S ratio of somatic mutations can provide statistical evidence to whether a mutated gene is a driver of tumor progression [3], [5].
The Cub and Sushi Multiple Domains 1 (CSMD1) gene is a novel candidate tumor suppressor gene located on the p arm of chromosome 8 (2792875…4852328). CSMD1 is frequently shown to be deleted [14], [15], [16], mutated [2], [10], [17], or methylated [14], [18] in many cancers. In fact, CSMD1 expression is frequently lost in breast cancer [19], whereas CSMD1 loses allelic balance in head and neck squamous cell carcinomas (HNSCC) and lung cancers [20]. CSMD1 has also shown to be methylated in HNSCC cell lines [21].
The first exon of CSMD1 harbors a methylated CpG island (Chromosome 8: 4848969–4852635) [21], a sequence rich in C:G base pairs contained within CpG or CpHpG contexts [22]. The CpG Island Methylator Phenotype (CIMP) [23] describes a subset of colorectal tumors that show high methylation frequency of specific CpG islands. These CIMP tumors have distinct clinical, pathologic, and molecular signatures such as proximal tumor location, poor differentiation, and microsatellite instability. Important clinical correlations with CIMP have also been observed in breast and brain tumors [24] indicating that the phenomenon is not just tissue specific. It is not yet clear if CIMP status causes or is merely associated with these phenotypes. Methylation of specific CIMP genes is only loosely correlated with repression of gene expression; therefore other mechanisms influencing clinical behavior of CIMP tumors may be important. Germline nucleotide substitutions that involve C:G>T:A transitions are thought to be catalyzed by cytosine methylation [25]. These substitutions lead to a genome-wide underrepresentation of CpG dinucleotides compared to what is expected by chance alone. Genome methylation has thus influenced genome sequence evolution and the polymorphism landscape of most vertebrates. By similar reasoning, it is possible that CIMP status of tumor cells or their pre-cancerous precursors (stem cells) may predispose methylated genes to accumulate C:G>T:A somatic mutations.
Somatic mutations in tumors may provide historical evidence for CSMD1 silencing by methylation in cancer progenitor cells. Colon stem cells located at the base of the crypts may be the primary targets for malignant transformation [26], [27]. Mutations that originate in stem cells [28], [29], [30], [31] have an opportunity to persist long enough for the accumulation of cooperating oncogenic mutations. Although epigenetic silencing of CSMD1 may contribute to the malignant transformed phenotype, [32], [33], [34], [35], [36], [37], somatic mutations that accumulate as a result of methylation may also contribute to malignancy by unknown mechanisms. By examining multiple methods of CSMD1 alterations (mutation, methylation, and allele loss), we observed significant correlations of CSMD1 loss of function with early age of diagnosis in colorectal cancer patients. The correlation between CSMD1 loss of function and clinical presentation may help provide insight into the neoplastic development of colorectal cancer.
Materials and Methods
Tumor Selection and DNA Isolation
De-identified surgical specimens were obtained from the South Carolina Biorepository System (Palmetto Health, Richland; Palmetto Health, Baptist, and Lexington Regional Medical Center, Lexington, South Carolina). This study was conducted with the approval of the Institutional Review Board of Palmetto Health, Lexington Medical Center, University of South Carolina, and Georgia Health Sciences University, and all written patient consents were obtained prior to study. De-identified clinical data was obtained from the tumor-registry, and the manual curation of pathology records was conducted by tissue bank personnel.
We chose 54 microsatellite-stable colorectal tumors for this study. All surgical specimens were fresh-frozen, embedded in Optimal Cutting Temperature compound (Sakura Finetek, Torrence, CA), and sectioned. The samples were cut into 10μm thick slices and fixed onto Sigma silane-prep ä slides. The slides were fixed using 75%, 95%, and 100% ethanol and xylene. The slices from the beginning and end of each tissue sample were stained with Mayer's Hematoxylin (Sigma, St. Louis, MO) and Eosin (Harleco, Lawrence, KS) solutions to specifically obtain the boundaries of tumor tissues. All patient sample data are provided in Table 1.
Table 1. Clinical and genetic data of 54 colorectal tumors sequenced by 454FLX sequencing.
| Patient | Gender | Race | Age at Diagnosis | Stage | KRAS AA Change | KRAS Somatic% | Allelic Imbalance | CSMD1 Somatic Mutation | CSMD1 Somatic % | CSMD1 Methylation |
| 510 | F | AA | 68 | 1 | WT | 0% | Unbalanced | 0% | ||
| 517 | M | EA | 52 | 2A | WT | 0% | Unbalanced | yes | 47% | yes |
| 529 | F | EA | 52 | 2A | G12>D | 32% | Unbalanced | yes | 31% | yes |
| 535 | F | EA | 80 | 1 | G12>D | 47% | Balanced | 0% | yes | |
| 541 | F | EA | 84 | 3B | G13>D | 68% | Balanced | 0% | yes | |
| 562 | F | EA | 69 | 3B | WT | 0% | Unbalanced | 0% | ||
| 575 | F | EA | 73 | 3B | G12>V | 27% | Balanced | 0% | ||
| 587 | M | EA | 75 | 3B | WT | 0% | Balanced | yes | 46% | yes |
| 590 | F | EA | 69 | 2A | WT | 0% | Indeterminant | 0% | yes | |
| 591 | M | EA | 75 | 1 | G12>D | 68% | Unbalanced | 0% | yes | |
| 5102 | M | EA | 72 | 2A | WT | 0% | Balanced | 0% | ||
| 5143 | M | EA | 79 | 1 | WT | 0% | Indeterminant | 0% | yes | |
| 5155 | F | EA | 74 | 1 | WT | 0% | Unbalanced | 0% | ||
| 5156 | F | EA | 61 | 3B | G13>D | 35% | Balanced | 0% | ||
| 5161 | F | unk | 82 | 2A | WT | 0% | Balanced | 0% | yes | |
| 5166 | M | EA | 62 | 4 | WT | 0% | Balanced | 0% | ||
| 5176 | F | EA | 55 | 3C | WT | 0% | Indeterminant | 0% | yes | |
| 5179 | F | AA | 89 | 2A | WT | 0% | Indeterminant | 0% | yes | |
| 5190 | M | EA | 56 | 1 | G12>V | 17% | Balanced | 0% | yes | |
| 5191 | M | EA | 53 | 1 | WT | 0% | Indeterminant | 0% | ||
| 10158 | F | EA | 76 | 4 | WT | 0% | Indeterminant | 0% | yes | |
| 14000 | M | AA | 73 | 3B | G12>R | 24% | Balanced | 0% | yes | |
| 31380 | M | AA | 48 | 2A | WT | 0% | Indeterminant | 0% | yes | |
| 40099 | F | AA | 61 | 4 | WT | 0% | Balanced | 0% | ||
| 40131 | F | EA | 63 | 3B | G12>D | 50% | Unbalanced | 0% | ||
| 40195 | M | EA | 60 | 2A | WT | 0% | Indeterminant | 0% | ||
| 40395 | M | EA | 64 | 1 | G12>D | 15% | Balanced | yes | 33% | |
| 40415 | M | EA | 19 | 1 | WT | 0% | Unbalanced | yes | 35% | |
| 40417 | F | EA | 80 | 3A | G12>A | 25% | Unbalanced | 0% | yes | |
| 40530 | M | EA | 71 | 3B | WT | 0% | Balanced | yes | 49% | |
| 40532 | M | EA | 81 | 3B | WT | 0% | Indeterminant | 0% | yes | |
| 40599 | F | AA | 68 | 3B | WT | 0% | Unbalanced | 0% | ||
| 40651 | F | AA | 30 | 3B | G12>D | 42% | Unbalanced | 0% | yes | |
| 40686 | F | AA | 73 | 3A | WT | 0% | Indeterminant | 0% | yes | |
| 40694 | M | KA | 59 | 4 | WT | 0% | Unbalanced | 0% | ||
| 41043 | M | EA | 78 | 2A | WT | 0% | Balanced | 0% | ||
| 41044 | F | AA | 66 | 3B | G12>D | 61% | Indeterminant | 0% | yes | |
| 41065 | F | AA | 59 | 3B | G12>V | 16% | Indeterminant | 0% | yes | |
| 41084 | F | EA | 58 | 2A | WT | 0% | Unbalanced | 0% | ||
| 41091 | M | EA | 81 | 3B | WT | 0% | Indeterminant | 0% | yes | |
| 41098 | F | AA | 69 | 3B | G12>V | 49% | Unbalanced | 0% | yes | |
| 41104 | F | EA | 59 | 4 | G12>V | 34% | Balanced | 0% | ||
| 41126 | M | EA | 57 | 1 | WT | 0% | Unbalanced | 0% | ||
| 41127 | M | AI | 84 | 2A | WT | 0% | Indeterminant | 0% | ||
| 41132 | M | AA | 63 | 3A | G13>D | 43% | Unbalanced | 0% | yes | |
| 41136 | M | EA | 68 | 2A | WT | 0% | Unbalanced | 0% | ||
| 41141 | F | AA | 58 | 4 | G12>D | 75% | Indeterminant | 0% | ||
| 41142 | F | EA | 58 | 3A | G12>D | 18% | Balanced | 0% | yes | |
| 41149 | F | EA | 59 | 1 | G12>C | 24% | Balanced | 0% | ||
| 41150 | F | EA | 49 | 2B | WT | 0% | Unbalanced | 0% | ||
| 41162 | M | EA | 64 | 3C | WT | 0% | Indeterminant | 0% | yes | |
| 41163 | F | EA | 52 | 1 | G12>R | 47% | Indeterminant | 0% | yes | |
| 41180 | M | EA | 64 | ND | WT | 0% | Unbalanced | 0% | ||
| 41185 | F | EA | 77 | 3A | WT | 0% | Balanced | 0% |
Extractions of the tumor and normal epithelial cells from the tissue slices were performed using micro-dissection technique developed in our lab. The tumor and normal cells were identified for micro-dissection with the use of two prepared H&E slides. A pathologist was involved in the process of identification of tumor and normal tissues. Tumor epithelium was microdissected from sections to obtain approximately 100 μg of DNA. The genomic DNA was then isolated using DNAdvance kit (Agencourt, Beverly, MA).
Quantification of Genomic DNA
The quantification of the isolated genomic DNA was performed with a standard curve of a known concentration of human DNA and real-time polymerase chain reaction (PCR) primers for Long Interspersed Nuclear Element (LINE) sequences [58]. The primers consisted of a LINE (F) Forward – AAAGCCGCTCAACTACATGG and a LINE (R) Reverse – CTCTATTTCCTTCAGTTCTGCTC (Integrated DNA Technologies, Coralville, IA). Quantification of the DNA was prepared using 6.25 μl of iTaq SYBR green SuperMix (Bio-Rad, Hercules, CA), 1.25 μl of 2 μM LINE F, 1.25 μl of 2 μM LINE R, 2.5 μl of PCR water (Invitrogen, Carlsbad, CA), and 1.25 μl of DNA template. Amplification of the DNA was carried out through thermal cycling with the MyIQ Thermal iCycler (Bio-Rad, Hercules, CA) using the following protocol: denaturation at 95°C for 1 min; 60 cycles at 94°C for 10 sec, 62°C for 45 sec, and 62°C for 5 min. The final template concentrations of tumor and normal DNA were 3ng/μl.
Screening for Microsatellite Instability in Tumors
The detection of mismatch repair deficient tumors was performed through amplification of microsatellite locus, so that tumors showing hypermutator phenotype could be excluded. All tumors were initially pre-screened for microsatellite instability (MSI) using BAT26 primers, and those with instability were excluded. Subsequently, tumors with somatic mutations to CSMD1 were analyzed with three additional NCI MSI loci: BAT25, D2S123 and D17S250 primers. The primers used are listed in Table S1 in File S1 (Integrated DNA Technologies, Coralville, IA). None of the tumors showed instability at the BAT26 locus, and only one sample (Tumor ID 587) showed moderate microsatellite instability at BAT25 locus. The PCR amplicons were generated with the following protocol: PCR master mix was prepared by using 5 μl of KAPA 5x HiFi buffer (KAPA Biosystems Woburn, MA), 0.75 μl of 10 mM dNTPs, 3.00 μl of primers (final concentration 2.5 μM), 0.50 μl of KAPA HiFi HotStart polymerase (KAPA Biosystems Woburn, MA), 1.00 μl of 10X SYBR Green (Invitrogen, Carlsbad, CA), 8.75 μl of PCR Water (Invitrogen, Carlsbad, CA), and 1 μl of DNA template at 3ng/μl. Thermal cycling was performed on a MyIQ Thermal iCycler (Bio-Rad, Hercules, CA) using the following protocol: 1 cycle of 95°C for 2 min; 3 cycles of 63°C for 15 sec and 72°C for 15 sec; 3 cycles 98°C for 20 sec, 60°C for 15 sec, 72°C for 15 sec; 3 cycles of 98°C for 20 sec, 57°C for 15 sec, 72°C for 15 sec; 49 cycles of 98°C for 20 sec, 56°C for 15 sec, 72°C for 15 sec; 1 cycle 55°C for 30 sec; 80 cycles of 55°C for 30 sec. The PCR products were run on 10% TBE-Urea gels (BIO-RAD, California, USA) according to the manufacturers guidelines and photographed using an Alpha Imager and Quantity One™ software (Alpha Innotech, San Leandro, CA).
Preparation of Amplicons for Sequencing
The exons for CSMD1 and KRAS genes were identified with the Sequence Viewer on the NCBI Website (http://www.ncbi.nlm.nih.gov/projects/sviewer). The PCR primers were designed for the 71 exons of CSMD1 and for 2 common hotspot mutations in KRAS (exon 2, codon 12 and 13) using the PRIMER3 open source software (http://frodo.wi.mit.edu/primer3/input.htm; (Table S1 in File S1). KRAS was sequenced only at the mutation hotspots due to sample constraints. Forward and reverse tag sequences, 454A and 454B, respectively were added to the primers as described in the Guide to Amplicon Sequencing (454 Life Sciences, Branford CT). PCR amplicons for 454 sequencing were generated using 7.5 μl of KAPA 5x HiFi buffer (KAPA Biosystems Woburn, MA), 1.125 μl of 10mM dNTPs, 2.25 μl of primers (final concentration 2.5 μM), 0.75 μl of KAPA HiFi HotStart polymerase (KAPA Biosystems Woburn, MA), and 1 μl of DNA template at 5ng/μl. Thermal cycling was performed using a MyIQ Thermal Cycler (Bio-Rad, Hercules CA) and the following touchdown protocol: One cycle, 95°C for 2 min; 3 cycles of 94°C for 10 sec, 64°C for 10 sec, 70°C for 30 sec; 3 cycles of 94°C for 10 sec, 61°C for 10 sec, 70°C for 30 sec; 3 cycles of 94°C for 10 sec, 58°C for 10 sec, 70°C for 30 sec; 50 cycles of 94°C for 10 sec, 57°C for 10 sec, 70°C for 30 sec. The PCR products were analyzed by electrophoresis on a 3% agarose gel and photographed using an Alpha Imager and Quantity One™ software (Alpha Innotech, San Leandro, CA). Amplicons were purified using SPRI Ampure beads (Agencourt, Beverly, MA) following the manufacturers protocol.
Sequencing with 454FLX Platform
The SPRI-Ampure bead purified PCR products (CSMD1 and KRAS) were quantified using the Quanti-iT PicoGreen dsDNA Assay (Invitrogen, Carlsbad, CA) and Fluoroskan Ascent FL (Thermo Fisher Scientific Inc., Waltham, MA). The amplicons were amplified by emulsion PCR using the emPCR Kite II and III (Roche Diagnostics, Indianapolis, IN) and bi-directionally sequenced on the 454 GS FLX genome sequencer (University of South Carolina Environmental Genomics Core Facility, Columbia, SC). Amplicons from each of the 54 tumors, as well as 2 paired normal samples, were sequenced to an average depth of 1800 fold with over 90% of the amplicons represented by greater than 300 sequence reads per sample. Over 500,000 individual sequencing reads were obtained from the amplicons.
Variant Detection Analysis
The 454FLX sequencing reads were aligned to the reference sequence from NCBI (hg19 Build 37) and analyzed using the software CLC Genomics Workbench 4 (CLC Bio, Aarhus, Denmark). We analyzed our sequencing data derived from colorectal tumors and matched normal samples by using the Probabilistic Variant Detection Tool provided by the Genomics Workbench. Mutations seen in the complementary normal tissue, the dbSNP database, or the 1000 Genomes Project were considered to be germline mutations. The remaining mutations were considered as likely somatic mutations. Our mutation calls were made under robust and stringent sequencing criteria set by the CLC Genomics Workbench with a probability call of 100 in order to delete any false mutation observations. Any homopolymer tracts were also excluded from our data analysis. We also excluded discovered insertion/deletion (INDEL) variants from our study, since 454FLX sequencing is not sensitive in detecting INDEL's.
Somatic Mutation Validation through Sanger Sequencing
Sanger sequencing of the high-concentration variants was performed in order to confirm the somatic mutations identified by the variant detection analysis. Beckman Coulter/Agencourt Genomic Services (Beverly, MA) and the core genomics facility at Georgia Health Sciences University performed the Sanger sequencing, utilizing the same 454A and B tags previously described with the 454FLX sequencing. The PCR amplicons were generated with the following protocol: PCR master mix was prepared by using 7 μl of PCR water (Invitrogen, Carlsbad, CA), 10 μl of 2X KAPA SYBR (KAPA Biosystems Woburn, MA), 2 μl of Primer mix (final concentration 2.5 μM), and 1 μl of DNA template at 3ng/μl. Thermal cycling was performed with the following protocol: 1 cycle of 98°C for 2 min; 3 cycles of 98°C for 10 sec, 63°C for 10 sec, 70°C for 30 sec; 3 cycles of 98°C for 10 sec, 60°C for 10 sec, 70°C for 30 sec; 3 cycles of 98°C for 10 sec, 57°C for 10 sec, 70°C for 30 sec; 49 cycles of 98°C for 10 sec, 56°C for 10 sec, 70°C for 30 sec; 1 cycle of 55°C for 30 sec; 80 cycles of 55°C for 80 cycles. Sanger chromatograms were analyzed using CLC Genomics Workbench 4. After being validated by Sanger sequencing, the CSMD1 somatic mutations were recorded and deposited in the Leiden Open Variation Database (LOVD) (Leiden University Medical Center, Netherlands).
Allelic Balance Testing from 454FLX CSMD1 Sequences
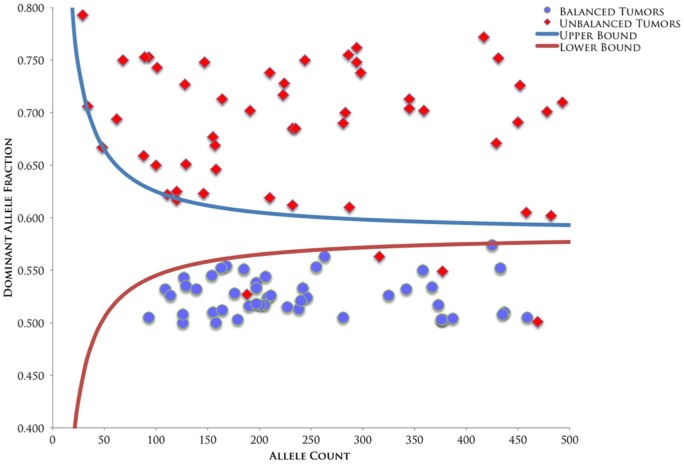
We used the Sequential Probability Ratio Test (SPRT) to detect statistically significant allelic imbalances in the tumor samples [39], [40]. The SPRT was designed to test two competing hypothesis using sequentially accrued observations over time against pre-specified upper and lower bounds of data [59]. Hypothesis 1 is that the alleles are balanced, so the expected allelic proportions at informative loci should be 50%. Hypothesis 2 is that one of the two alleles present in the normal sample is completely absent in the tumor, so the expected dominant allelic proportion at informative loci should be 100% for tumor samples uncontaminated with normal DNA. In cases undergoing LOH where the tumor DNA is contaminated with up to 50% normal DNA, the expected dominant allelic proportion is 66.7%. Confidence interval curves were constructed to correctly identify balanced and unbalanced alleles across the range of total allele counts observed in the 454FLX data, allowing for up to 50% contamination of tumor with normal DNA. The upper curve establishes the threshold for allelic imbalance, whereas the lower curve establishes the threshold for allelic balance. If a tumor's allele proportion exceeds the upper bound the tumor was classified as unbalanced. In contrast, if the allele proportion is less than the lower bound curve, the tumor was classified as balanced. If the observed allele proportion occurred between the two curves, the samples were classified as indeterminate. In all cases, two or more informative alleles were required to be out of balance to call a tumor imbalanced.
CSMD1 mRNA Expression Analysis in HCT116 WT and HCT116 DNMT1/DNMT3B DKO
Expression of CSMD1 mRNA was determined by performing quantitative real-time PCR on HCT116 WT and HCT116 DNMT1/3B DKO cDNA. HCT116 WT and DNMT1/3B DKO cDNA was generated by first isolating the mRNA of each using Dynabeads mRNA isolation kit (Invitrogen, Carlsbad, CA) and then was converted into cDNA using Superscript II Reverse Transcriptase (Invitrogen, Carlsbad, CA). The PCR amplicons were generated with the following protocol: PCR master mix was prepared by using 3 μl of PCR water (Invitrogen, Carlsbad, CA), 10μl of 2X KAPA SYBR (KAPA Biosystems Woburn, MA), 2 μl of Primer mix (final concentration 2.5 μM), and 5 μl of cDNA template. Thermal cycling was performed with the following protocol: 1 cycle of 98°C for 2 min; 3 cycles of 98°C for 10 sec, 64°C for 10 sec, 70°C for 30 sec; 3 cycles of 98°C for 10 sec, 61°C for 10 sec, 70°C for 30 sec; 3 cycles of 98°C for 10 sec, 58°C for 10 sec, 70°C for 30 sec; 40 cycles of 98°C for 10 sec, 57°C for 10 sec, 70°C for 30 sec; 1 cycle of 95°C for 30 sec; 80 cycles of touchdown gradient starting at 95°C and decreasing by −5°C each cycle.
Methylation Analysis using Methylation Specific PCR/High Resolution Melt Curve Analysis
We purified DNA from tumors and control cell lines by the Agencourt DNAdvance Kit (Beckman Coulter Genomics, Beverly, MA) according to manufacturer's instructions. Two hundred nanograms of genomic DNA was bisulfite modified by the EZ DNA Methylation – Gold Kit (Zymo Research), following the manufacturer's protocol. HCT116 and the HCT116-DNMT1/3B double knockout (DKO) DNA [43] were used as positive and negative controls for the methylation status of all genes examined. CSMD1 is methylated and not expressed in the wild-type HCT-116 cells. In contrast, CSMD1 is unmethylated and expressed in the DKO cells [60]. CSMD1 gene methylation was queried at 3 positions and were named CSMD1-1 (Chr8: 4852196–4852032), CSMD1-3 (4851450–4851301) and CSMD1-5 (4851422–4851291). The methylation specific PCR primers used are shown in Table S2 in File S1. Each tumor generated an authentic product either with methylated primers or with unmethylated primers, but never both. Instances where no product was observed with either primer pair were considered uninformative. The methylation results of the tumors are shown in Table S3 in File S1.
The methylation specific PCR/high resolution melt Curve Analysis was implemented according to previously described protocols [61]. The PCR reaction was performed using 3–6 ng of bisulfite modified DNA in a total volume of 20 μl, containing 12.5 μl of 2X KAPA SYBR FAST qPCR Master Mix (KAPA Biosystems Woburn, MA), (for analyzing genomic position 3265577 KAPA HRM fast PCR kit was used); and 2.5pmol of primers [62]. The reaction cycling conditions were 94°C for 10 min, followed by 45 cycles of 30 sec at 94°C, Gene-specific Annealing Temperature for 30 sec, extension at 72°C for 30 sec, and a data collection window at 76–77°C for 30 sec. Association curves were generated for all products, and the presence or absence of authentic products was determined by comparison to positive and negative controls. All reactions were performed using a MyIQ Single color Real-Time PCR Detection System (Bio-Rad).
Statistical Analysis
Binomial probability was used to compare the significance between nonsynonymous to synonymous somatic mutations of CSMD1 in colorectal patients. Comparison of average age of diagnosis or clinical presentation for genetically balanced and unbalanced patients with somatic mutations were done by the Mann-Whitney U test. Spearman Rank Correlation was used to compare the relationships between methylated loci.
Results
Frequencies and Character of Somatic Mutations
The CSMD1 gene spans 2.05 MB of genomic DNA on the p arm of chromosome 8. The coding sequence portion of the gene is 11,740 nucleotides (0.0234 Mb per diploid genome). We sequenced a total of 54 colorectal tumors equaling to 1.26 MB of CSMD1 CDS DNA. We identified and Sanger-verified 16 somatic mutations in 6 of the 54 colorectal tumors (11%) (Table 2). We then calculated a somatic mutation rate of 11.90 mutations/MB, a rate that is noticeably higher than the genome-wide background mutation rates of microsatellite-stable colorectal cancers [3], [38].
Table 2. Sanger-validated somatic mutations of CSMD1 in colorectal tumors.
| Patient | Chr | Position | Reference | Variants | Counts | Coverage | Frequencies | CDS | AA Change | Conservation score |
| 517 | 8 | 2813254 | G | G/A | 696/327 | 1090 | 63.9/30.0 | 9851C>T | Ala3284Val | 0.666 |
| 517 | 8 | 2823344 | C | C/T | 941/357 | 1425 | 66.0/25.1 | 9233G>A | Arg3078His | 0.221 |
| 517 | 8 | 2824162 | C | C/A | 454/172 | 686 | 66.2/25.1 | 9030G>T | Lys3010Asn | 0.932 |
| 517 | 8 | 3141735 | T | T/C | 828/331 | 1159 | 71.4/28.6 | 4084A>G | Asn1362Asp | 1 |
| 517 | 8 | 3141850 | G | G/A | 721/393 | 1159 | 62.2/33.9 | 3969C>T | 0.934 | |
| 517 | 8 | 3216691 | G | G/C | 638/486 | 1161 | 55.0/41.9 | 3287C>G | Pro1096Arg | 1 |
| 517 | 8 | 3265577 | C | C/T | 127/58 | 187 | 67.9/31.0 | 1915G>A | Ala639Thr | 0.073 |
| 517 | 8 | 3265665 | G | G/T | 71/29 | 101 | 70.3/28.7 | 1827C>A | Asn609Lys | 1 |
| 517 | 8 | 3889468 | C | C/T | 594/187 | 856 | 69.4/21.8 | 569G>A | Gly190Glu | 0.983 |
| 517 | 8 | 4851922 | C | C/A | 31/28 | 61 | 50.8/45.9 | 17G>T | Arg6Ile | 0.296 |
| 529 | 8 | 2967782 | A | A/G | 157/69 | 226 | 69.5/30.5 | 6506T>C | Leu2169Pro | 0.906 |
| 587 | 8 | 3165911 | G | G/T | 510/192 | 703 | 72.5/27.3 | 3746C>A | Ala1249Asp | 1 |
| 40395 | 8 | 3046419 | G | G/A | 76/38 | 118 | 64.4/32.2 | 5513C>T | Ser1838Leu | 0.866 |
| 40415 | 8 | 2944669 | C | C/T | 165/54 | 227 | 72.7/23.8 | 7424G>A | Arg2475Gln | 0.282 |
| 40415 | 8 | 3265619 | T | T/G | 57/30 | 89 | 64.0/33.7 | 1873A>C | Ile625Leu | 0.998 |
| 40530 | 8 | 3267040 | G | G/A | 196/189 | 385 | 50.9/49.1 | 1649C>T | Thr550Ile | 0.984 |
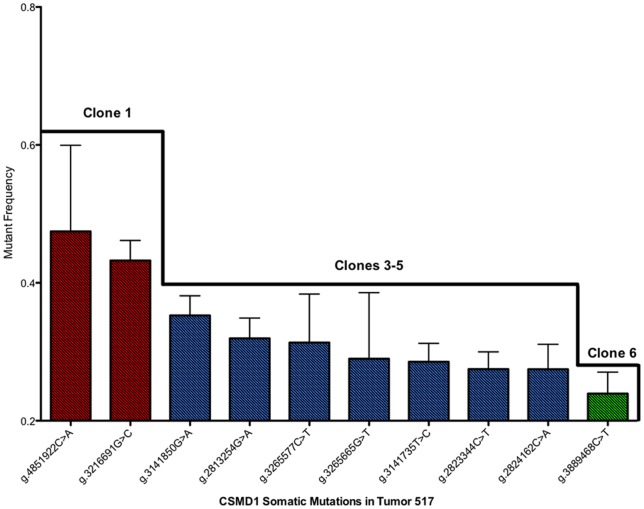
The somatic mutations were significantly enriched for nonsynonymous changes compared to synonymous changes. For the Sanger confirmed variants, we identified 15 nonsynonymous (NS) mutations and 1 synonymous (S) mutation, for a NS/S ratio of 15∶1. The probability of this many (or more) nonsynonymous mutations occurring by chance alone is 0.014, arguing against the hypothesis that CSMD1 is a passenger gene affected by a mutator phenotype. The more likely explanation is that nonsynonymous mutations are selected for during colorectal cancer development. It is important to note that tumor 517 had 10 somatic mutations to CSMD1, nine of which were nonsynonymous. The probability of this many nonsynonymous mutations occurring by chance alone is 0.1. The alternative hypothesis is that selective pressure drove the accumulation of multiple CSMD1 nonsynonymous variants within the same tumor, possibly residing in separate subclones. The varying subsets of mutation frequencies in CSMD1 allude to this belief that the multiple CSMD1 mutations arose from separate subclones in the same tumor population (Figure 1).
Figure 1. CSMD1 mutation frequencies of somatic variants in Tumor 517.
Ten CSMD1 somatic mutation were found in Tumor 517. However, these particular mutations occur at varying subsets of concentrations, indicating that each subset may have arisen from an independent clone within the tumor population.
Since progression of adenocarcinoma can be driven by mutations to the KRAS oncogene, we analyzed the mutation hotspots at codons 12 and 13 of exon 2 using Sanger sequencing of PCR products. KRAS hotspot somatic mutations were seen in 21 of the 54 colorectal tumors (∼39%). Three tumors contained somatic mutations in both CSMD1 and KRAS, with two of the three tumors showing a higher CSMD1 mutant allele frequency than the KRAS mutant allele (Table 1). This result may indicate that the CSMD1 somatic mutations predate KRAS somatic mutations, which are thought to occur early during colorectal tumor progression. One tumor did have CSMD1 mutation allele concentrations that were less than the KRAS mutant allele concentration, perhaps indicating that the CSMD1 mutations in this tumor occurred after the KRAS mutations. Still, the clone harboring the CSMD1 mutant allele expanded sufficiently to allow the CSMD1 mutant allele to be detected, demonstrating that this expansion was not driven by the mutant KRAS allele. In order to properly determine the timelines for CSMD1 and KRAS mutations, carful sequence analysis of early lesions such as adenomas will be required. Nevertheless, our observations indicate that CSMD1 nonsynonymous mutations provide tumor cells with a selective advantage, which operates independently of the advantage provided by KRAS mutations.
Colorectal Tumors with CSMD1 LOH and Somatic Mutations Show Early Clinical Presentation
Out of the 54 tumors sequenced, Thirty-seven had two or more loci that were heterozygous for germline variants and could therefore be assessed for CSMD1 allelic imbalance by the Sequential Probability Ratio Test [39], [40]. Fifty-one percent (19/37) of the colorectal tumors were unbalanced at two or more contiguous CSMD1 loci (Figure 2, Table 1), indicating that CSMD1 loss of heterozygosity could have occurred in these tumors. Although the difference was not statistically significant, the average age of diagnosis for patients with CSMD1 allelic imbalance was younger than those with balanced alleles (60 years vs. 69 years, Mann-Whitney p = 0.052). The average age at diagnosis for patients with CSMD1 somatic mutations was also younger than for those without somatic mutations (58 years vs. 66 years), though this difference was also not statistically significant. Loss of heterozygosity is a mechanism that cooperates with somatic mutation to inactivate tumor suppressor genes. We observed that patients with both unbalanced and mutated CSMD1 alleles were significantly younger at age of diagnosis (41 years) than patients with balanced and wild type CSMD1 (68 years, Mann-Whitney p = 0.0077). In contrast to our earlier studies [17], we did not observe a significant relationship between CSMD1 somatic mutation status and tumor stage in this series of samples. Nevertheless, the statistical evidence regarding clinical presentation coincides with recent studies conducted by The Cancer Genome Atlas (TCGA). Based on a Kaplan-Meier Survival Analysis, TCGA sequencing data revealed that colorectal cancer patients with CSMD1 alterations have a significantly lower probability of survival than patients without CSMD1 alterations (log-rank test p = .000565) [41]. With such evidence, the identification of CSMD1 alterations has the potential to be used as markers in colorectal cancer prognosis.
Figure 2. Sequential Probability Ratio Test (SPRT) analysis of CSMD1 based on digital allele counting.
The upper bound curve shown in the graph demonstrates the 95% CI threshold of CSMD1 loci being classified as unbalanced, whereas the lower bound curve demonstrates the 95% CI threshold of CSMD1 loci being classified as balanced. Tumors with two or more contiguous loci that were imbalanced were classified as having undergone loss of heterozygosity. Loci that fell between the two thresholds were deemed indeterminate for allelic characterization. Certain loci in CSMD1 demonstrated allelic balance, though they resided in tumors that were unbalanced for CSMD1. This result alludes to chromosomal breaks that occur within the CSMD1 gene sequence, downstream of the examined loci.
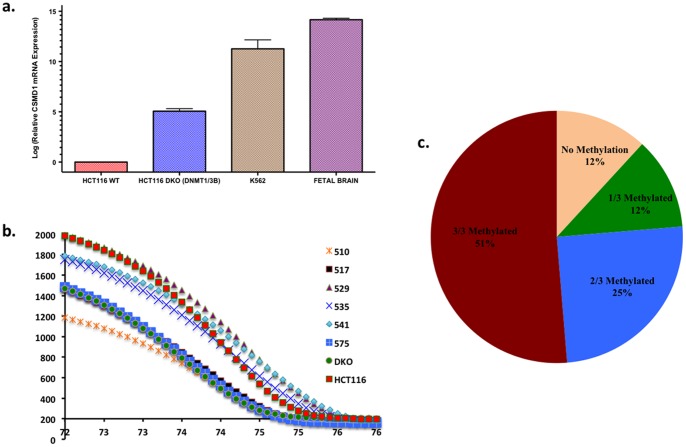
Excess of CG>TA Mutations and CSMD1 Methylation
Exome sequencing of colorectal cancers has revealed that several tumors have global excess of CG>TA somatic mutations [2], [3]. We observed 7 out of 15 (46.7%) CSMD1 somatic mutations were CG>TA transitions (Table 2). This class of mutation arises from non-enzymatic deamination of 5′-methylcytosine to produce thymidine. Constitutively methylated CpG dinucleotides have been shown to be mutation hotspots in the retinoblastoma gene (RB1) [42]. Of the CG>TA somatic mutations, 4 were C>T and 3 were G>A (which is assumed to have arisen by C>T on the opposing strand). The even distribution of CG>TA mutations between the transcribed and non-transcribed strands of the CSMD1 gene argues against active transcription-coupled repair occurring during the accumulation of the mutations. A simple explanation for this result could be that the mutations to CSMD1 occurred in a cell type in which the gene is silenced through DNA methylation. By performing quantitative RT-PCR on HCT116 wildtype and HCT116 DNA methyltransferase 1/DNA methyltransferase 3B double-knockout (DNMT1/3B DKO) cell line [43] cDNA (as well as K562 cell line and fetal brain cDNA), we were able to demonstrate that over a 30 fold increase in CSMD1 mRNA expression in HCT116 DNMT1/3B DKO cells compared to their wildtype counterparts. This increase in mRNA expression indicates that DNA methylation, a mechanism depleted by the knockout of both DNMT1 and DNMT3B in HCT116 cells, has an inhibitory effect on CSMD1 expression (Figure 3a). Based on the results of the RT-PCR assay, we wanted to understand the potential correlation between DNA methylation and CG>TA mutations in CSMD1. To do this, we analyzed the genomic position 3265577, which contained a somatic mutation in a C:G context (Tumor 517) and is a part of two neighboring CpG sites (Chr8:3265572-3265582, sequence GACCGCGAGAA). We designed PCR primers specific for bisulfite converted sequences flanking the core CGCG (Table S2 in File S1) and confirmed whether this site is methylated in non-mutated tumors by performing a high-resolution melt association curve analysis (Figure 3b) (Table S3 in File S1). HCT116 WT and HCT116 DNMT1/3B DNA were used as positive and negative controls, respectively, to determine DNA methylation in each tumor sample.
Figure 3. Determining CSMD1 methylation in colorectal tumors.
a.) CSMD1 mRNA expression comparison in HCT116 WT and HCT116 DNMT1/3B DKO cDNA along with K562 and fetal brain cDNA. b.) The high-resolution melt curve analysis distinguishes between methylated and unmethylated CG at Reference position 3265577 based upon their melt temperature. Tumor 517 was mutated at CG3265577 so the melt peak coincided with HCT-DKO whereas methylated tumors coincided with the HCT-116 peaks, which is our positive control c.) The percentage of colorectal tumors methylated at CSMD1 loci determined by methylation specific PCR melt curve analysis.
We then analyzed the publicly available data reported by Kim et al. [44] in GSE17648 and found CSMD1 hypermethylation at CG22619018 in the colorectal tumors compared to the adjacent patient-matched normal colonic mucosa (paired t-test, p = 3.59E-08). Although it is impossible to query the methylation status of CSMD1 within the stem cells that gave rise to the tumors, we obtained direct evidence that CSMD1 remains heavily methylated in developed colorectal tumors. We performed methylation-specific PCR on three CSMD1 loci (Chr8: 4852196–4852032; Chr8: 4851450–4851301; Chr8: 4851422–4851291) (Figure S1a & b) and four known CpG Island Methylator Phenotype (CIMP) genes: ALX4 (Chr11: 44282278–44331716), RUNX3 (Chr1: 25226002–25291501), NEUROG1 (Chr5: 134,870741–134,872051) and CDKN2A (Chr9: 21967751–21975132). Remarkably, 90% of tumors examined were methylated in at least one of these three CSMD1 loci, and 50% of tumors were methylated at all three loci (Figure 3c). The frequency of CSMD1 methylation exceeded that of the established CIMP markers. Methylation at all three CSMD1 loci was also significantly positively correlated with RUNX3, whereas CSMD1-3 also significantly correlated with ALX4 (p = 0.001, R = .4206). Although NEUROG1 and CDKN2A have shown to be methylated in colorectal cancers [45], [46], CSMD1-3 methylation did not correlate with NEUROG1 (p = 0.432, R = .1081) or CDKN2A (p = 0.537, R = .08488) methylation, though these two markers did positively correlate with each other (p<0.01) (Table 3 & Table 4). Interestingly, the data from Ben-Porath et al [47] showed that ALX4 and CSMD1 are bound by members of the Polycomb Repressor Complex 2 (PRC2), a complex that silences gene expression through histone modification and predisposes genes to DNA methylation. Our data also show that CSMD1 DNA methylation is significantly positively correlated with both methylated ALX4 and the known PRC2 target RUNX3. Observing RUNX3 methylation in our data coincides with others who have reported that 21% of colorectal cancer have RUNX3 hypermethylation [48]. We conclude that CSMD1 silencing by PRC2-mediated histone modifications may have impacted the somatic mutation landscape through acquired DNA methylation [49], [50].
Table 3. Spearman Rank correlation p values of CSMD1 loci analyzed for DNA methylation.
| CSMD1-3 | CSMD1-5 | ALX4 | RUNX3 | NEUROG1 | CDKN2A | |
| CSMD1-1 | 0.001 | 0.001 | 0.593 | 0.05 | 0.614 | 0.348 |
| CSMD1-3 | 0.001 | 0.001 | 0.001 | 0.432 | 0.537 | |
| CSMD1-5 | 0.179 | 0.015 | 0.681 | 0.284 | ||
| ALX4 | 0.001 | 0.03 | 0.006 | |||
| RUNX3 | 0.03 | 0.006 | ||||
| NEUROG1 | 0.001 |
Table 4. Spearman Rank R values of CSMD1 loci analyzed for DNA methylation.
| CSMD1-3 | CSMD1-5 | ALX4 | RUNX3 | NEUROG1 | CDKN2A | |
| CSMD1-1 | 0.4135 | 0.4292 | 0.06131 | 0.2141 | 0.05794 | 0.1078 |
| CSMD1-3 | 0.3654 | 0.4206 | 0.546 | 0.1081 | 0.08488 | |
| CSMD1-5 | 0.1538 | 0.2728 | 0.04725 | 0.1226 | ||
| ALX4 | 0.491 | 0.2362 | 0.3066 | |||
| RUNX3 | 0.2371 | 0.3077 | ||||
| NEUROG1 | 0.4693 |
These results document that several CpG islands within CSMD1 are indeed methylated within tumors. The excess of CG>TA somatic mutations may indicate that the methylation de-stabilized the CSMD1 coding sequence, predisposing it to CG>TA transition mutations. This speculation is supported by the observation that genomic position 3265577 is methylated in colorectal tumors, and was a site of somatic mutation in Sample 517.
Discussion
We previously reported frequent mutations of CSMD1 in colorectal cancers [17]. In this follow-up study, we used next generation sequencing to further confirm the important role of CSMD1 mutations in colorectal cancer progression. We observed that the CSMD1 somatic mutations are enriched for nonsynonymous changes. We interpret this to indicate that CSMD1 mutation provides a proliferative advantage, even in tumors that have mutations in strong driver genes such as KRAS, PIK3CA, and APC. Functional studies of CSMD1 will be required to further understand the mechanism by which CSMD1 mutations offer a selected advantage during tumor formation. However, the high NS/S ratio of CSMD1 mutations alone highlights the importance of this gene during colorectal tumor development. This high NS/S ratio in CSMD1 mutant alleles (15∶1) approaching clonal dominance is consistent with the Darwinian model of tumor sub-clone development and positive Darwinian selection for nonsynonymous mutations within the primary tumor. Tumor suppressor genes are inactivated in cancer by deletion, mutation, or, in some cases, DNA methylation. Interestingly, some tumor suppressor genes that normally are seen methylated can also be somatically mutated [51]. Our data suggests that CSMD1 is a tumor suppressor gene that can be silenced by multiple mechanisms. CSMD1 variant allele sampling by deep sequencing may be an attractive method for identifying early-stage neoplasia. Variants that lead to frame shifts, nonsense, or non-conservative missense mutations may represent novel reporters foreshadowing poor clinical outcome. Molenaar et al., [52] recently reported recurrent mutations in CSMD1 in neuroblastoma tumors and demonstrated that other genes involved in neuronal cone growths are silenced in neuroblastoma.
Within the somatic mutations discovered, we found a high prevalence of CG>TA mutations, a well as frequent DNA methylation. Cancer-specific hypermethylation of CSMD1 or other methylation markers could result from a particular mutational mechanism. A recent study showed that mutations arising from a mutator phenotype have the most influence on cancer development when mutations occur at early stages during carcinogenesis [53]. Nevertheless, though it is difficult to measure the methylation status of normal intestinal stem cells, the CG>TA mutation excess frames a historical record of the methylation environment present in the progenitor population. Whether or not the cancer methylator phenotype itself is encoded by germline or somatic mutation patterns in the tumor may become apparent as additional methylation targets are sequenced for somatic mutations.
It has been shown in hereditary nonpolyposis colorectal cancer (HNPCC) tumors that promoter hypermethylation may be a likely mechanism to accomplish biallelic inactivation. A study by Rai et al., [54] proposed a model where APC controls intestinal cell fate through DNA methylation. APC and retinoic acid downregulates the demethylases, thereby methylating key genes and committing cells to differentiation. Indeed, we discovered that the differentiated tumors were methylated at one or more loci studied.
Aggressive tumors have an embryonic stem cell-like gene expression signature [55]. Colon epithelial cells arise from intestinal stem cells located in the base of intestinal crypts. Each stem cell divides asymmetrically in order to produce a subsequent stem cell and a transitional amplifying cell that migrates up the crypt-to-tip axis and eventually differentiates [27]. Based on this understanding, we postulate that somatic mutations in CSMD1 accumulate in the stem cell compartment and disrupt CSMD1 expression prior to cancer development. This idea of diminished CSMD1 expression has previously been demonstrated in glioblastoma stem cell lines compared to its normal neuronal stem cell counterpart [56]. Thus, these inactivating CSMD1 mutations may possibly reveal their apparent phenotypic influence on tumor pathology only after mutations in critical gatekeeper genes produce a cell population in which the absence of normal CSMD1 creates a pathophysiological effect.
In conclusion, our study indicates that CSMD1 is highly mutated in colorectal cancer with a C:G bias, suggesting that methylation may contribute to the gene-specific hypermutator phenotype. A recent review by Peltomaki [57] stresses Knudson's two hit theory in which the first hit either occurs in somatic cells, leading to sporadic cancer or in the germline, leading to hereditary cancers. However, the second hit is always somatic in nature. The review continues to discuss how DNA methylation may drive somatic events with age progression and cause defectiveness in the bowel mucosa. Kashuba et al. [51] also alludes to this mutator phenotype by discovering multiple mutations in RASSF1A, a tumor suppressor gene that is commonly methylated. Therefore, based on our results and the validation of future studies, CSMD1 methylation may be identified as an instrumental mechanism in driving somatic mutations in CSMD1, indicating itself as an underlying agent in early colorectal cancer development.
Supporting Information
Table S1. Primer sequences for PCR amplification. Table S2. List of methylation specific primers. Table S3. Methylation landscape of CSMD1 studied in tumors.
(XLSX)
Characterization of CSMD1 methylation in colorectal tumors. a.) A demonstration of methylation-specific PCR melt curve analysis peaks that differentiate between methylated and unmethylated ALX4 in colorectal cancer tumors studied. b.) A demonstration of methylation-specific PCR melt curve analysis peaks that differentiate between methylated and unmethylated peaks in CSMD1 at position CG3265577 in the colorectal tumors studied.
(TIF)
Funding Statement
Support for this project was provided by National Institutes of Health grant 7R21CA127683. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Jemal A, Bray F (2011) Center MM, Ferlay J, Ward E, et al (2011) Global cancer statistics. CA: a cancer journal for clinicians 61: 69–90. [DOI] [PubMed] [Google Scholar]
- 2. Wood LD, Parsons DW, Jones S, Lin J, Sjoblom T, et al. (2007) The genomic landscapes of human breast and colorectal cancers. Science 318: 1108–1113. [DOI] [PubMed] [Google Scholar]
- 3. Sjoblom T, Jones S, Wood LD, Parsons DW, Lin J, et al. (2006) The consensus coding sequences of human breast and colorectal cancers. Science 314: 268–274. [DOI] [PubMed] [Google Scholar]
- 4. Benvenuti S, Frattini M, Arena S, Zanon C, Cappelletti V, et al. (2008) PIK3CA cancer mutations display gender and tissue specificity patterns. Human mutation 29: 284–288. [DOI] [PubMed] [Google Scholar]
- 5. Greenman C, Stephens P, Smith R, Dalgliesh GL, Hunter C, et al. (2007) Patterns of somatic mutation in human cancer genomes. Nature 446: 153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stratton MR, Futreal PA (2004) Cancer: understanding the target. Nature 430: 30. [DOI] [PubMed] [Google Scholar]
- 7. Vogelstein B, Kinzler KW (2004) Cancer genes and the pathways they control. Nature medicine 10: 789–799. [DOI] [PubMed] [Google Scholar]
- 8. Bozic I, Antal T, Ohtsuki H, Carter H, Kim D, et al. (2010) Accumulation of driver and passenger mutations during tumor progression. Proceedings of the National Academy of Sciences of the United States of America 107: 18545–18550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Siegmund KD, Marjoram P, Tavare S, Shibata D (2011) High DNA methylation pattern intratumoral diversity implies weak selection in many human colorectal cancers. PloS one 6: e21657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bignell GR, Greenman CD, Davies H, Butler AP, Edkins S, et al. (2010) Signatures of mutation and selection in the cancer genome. Nature 463: 893–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pleasance ED, Cheetham RK, Stephens PJ, McBride DJ, Humphray SJ, et al. (2010) A comprehensive catalogue of somatic mutations from a human cancer genome. Nature 463: 191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bardelli A, Parsons DW, Silliman N, Ptak J, Szabo S, et al. (2003) Mutational analysis of the tyrosine kinome in colorectal cancers. Science 300: 949. [DOI] [PubMed] [Google Scholar]
- 13. Nikolaev SI, Rimoldi D, Iseli C, Valsesia A, Robyr D, et al. (2012) Exome sequencing identifies recurrent somatic MAP2K1 and MAP2K2 mutations in melanoma. Nature genetics 44: 133–139. [DOI] [PubMed] [Google Scholar]
- 14. Hogan LE, Meyer JA, Yang J, Wang J, Wong N, et al. (2011) Integrated genomic analysis of relapsed childhood acute lymphoblastic leukemia reveals therapeutic strategies. Blood 118: 5218–5226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sun PC, Uppaluri R, Schmidt AP, Pashia ME, Quant EC, et al. (2001) Transcript map of the 8p23 putative tumor suppressor region. Genomics 75: 17–25. [DOI] [PubMed] [Google Scholar]
- 16. Toomes C, Jackson A, Maguire K, Wood J, Gollin S, et al. (2003) The presence of multiple regions of homozygous deletion at the CSMD1 locus in oral squamous cell carcinoma question the role of CSMD1 in head and neck carcinogenesis. Genes, chromosomes & cancer 37: 132–140. [DOI] [PubMed] [Google Scholar]
- 17. Farrell C, Crimm H, Meeh P, Croshaw R, Barbar T, et al. (2008) Somatic mutations to CSMD1 in colorectal adenocarcinomas. Cancer biology & therapy 7: 609–613. [DOI] [PubMed] [Google Scholar]
- 18. Kraus DM, Elliott GS, Chute H, Horan T, Pfenninger KH, et al. (2006) CSMD1 is a novel multiple domain complement-regulatory protein highly expressed in the central nervous system and epithelial tissues. Journal of immunology 176: 4419–4430. [DOI] [PubMed] [Google Scholar]
- 19. Kamal M, Shaaban AM, Zhang L, Walker C, Gray S, et al. (2010) Loss of CSMD1 expression is associated with high tumour grade and poor survival in invasive ductal breast carcinoma. Breast cancer research and treatment 121: 555–563. [DOI] [PubMed] [Google Scholar]
- 20. Ma C, Quesnelle KM, Sparano A, Rao S, Park MS, et al. (2009) Characterization CSMD1 in a large set of primary lung, head and neck, breast and skin cancer tissues. Cancer biology & therapy 8: 907–916. [DOI] [PubMed] [Google Scholar]
- 21. Richter TM, Tong BD, Scholnick SB (2005) Epigenetic inactivation and aberrant transcription of CSMD1 in squamous cell carcinoma cell lines. Cancer cell international 5: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dyachenko OV, Schevchuk TV, Kretzner L, Buryanov YI, Smith SS (2010) Human non-CG methylation: are human stem cells plant-like? Epigenetics: official journal of the DNA Methylation Society 5: 569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weisenberger DJ, Siegmund KD, Campan M, Young J, Long TI, et al. (2006) CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nature genetics 38: 787–793. [DOI] [PubMed] [Google Scholar]
- 24. Fang F, Turcan S, Rimner A, Kaufman A, Giri D, et al. (2011) Breast cancer methylomes establish an epigenomic foundation for metastasis. Science translational medicine 3: 75ra25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cooper DN, Chen JM, Ball EV, Howells K, Mort M, et al. (2010) Genes, mutations, and human inherited disease at the dawn of the age of personalized genomics. Human mutation 31: 631–655. [DOI] [PubMed] [Google Scholar]
- 26. Feinberg AP, Ohlsson R, Henikoff S (2006) The epigenetic progenitor origin of human cancer. Nature reviews Genetics 7: 21–33. [DOI] [PubMed] [Google Scholar]
- 27. van der Flier LG, Clevers H (2009) Stem cells, self-renewal, and differentiation in the intestinal epithelium. Annual review of physiology 71: 241–260. [DOI] [PubMed] [Google Scholar]
- 28. Ashkenazi R, Gentry SN, Jackson TL (2008) Pathways to tumorigenesis – modeling mutation acquisition in stem cells and their progeny. Neoplasia 10: 1170–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pardal R, Clarke MF, Morrison SJ (2003) Applying the principles of stem-cell biology to cancer. Nature reviews Cancer 3: 895–902. [DOI] [PubMed] [Google Scholar]
- 30. Reya T, Morrison SJ, Clarke MF, Weissman IL (2001) Stem cells, cancer, and cancer stem cells. Nature 414: 105–111. [DOI] [PubMed] [Google Scholar]
- 31. Siegmund KD, Marjoram P, Woo YJ, Tavare S, Shibata D (2009) Inferring clonal expansion and cancer stem cell dynamics from DNA methylation patterns in colorectal cancers. Proceedings of the National Academy of Sciences of the United States of America 106: 4828–4833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Beuten J, Gelfond JA, Martinez-Fierro ML, Weldon KS, Crandall AC, et al. (2009) Association of chromosome 8q variants with prostate cancer risk in Caucasian and Hispanic men. Carcinogenesis 30: 1372–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hornstein M, Hoffmann MJ, Alexa A, Yamanaka M, Muller M, et al. (2008) Protein phosphatase and TRAIL receptor genes as new candidate tumor genes on chromosome 8p in prostate cancer. Cancer genomics & proteomics 5: 123–136. [PubMed] [Google Scholar]
- 34. Kuo KT, Guan B, Feng Y, Mao TL, Chen X, et al. (2009) Analysis of DNA copy number alterations in ovarian serous tumors identifies new molecular genetic changes in low-grade and high-grade carcinomas. Cancer research 69: 4036–4042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lau WL, Scholnick SB (2003) Identification of two new members of the CSMD gene family small star, filled. Genomics 82: 412–415. [DOI] [PubMed] [Google Scholar]
- 36. Midorikawa Y, Yamamoto S, Tsuji S, Kamimura N, Ishikawa S, et al. (2009) Allelic imbalances and homozygous deletion on 8p23.2 for stepwise progression of hepatocarcinogenesis. Hepatology 49: 513–522. [DOI] [PubMed] [Google Scholar]
- 37. Scholnick SB, Richter TM (2003) The role of CSMD1 in head and neck carcinogenesis. Genes, chromosomes & cancer 38: 281–283. [DOI] [PubMed] [Google Scholar]
- 38. Zeitoun G, Mourra N, Blanche-Koch H, Thomas G, Olschwang S (2008) Genomic profile of colon cancer metastases. Anticancer research 28: 3609–3612. [PubMed] [Google Scholar]
- 39. Zhou W, Galizia G, Lieto E, Goodman SN, Romans KE, et al. (2001) Counting alleles reveals a connection between chromosome 18q loss and vascular invasion. Nature biotechnology 19: 78–81. [DOI] [PubMed] [Google Scholar]
- 40. Zhou W, Goodman SN, Galizia G, Lieto E, Ferraraccio F, et al. (2002) Counting alleles to predict recurrence of early-stage colorectal cancers. Lancet 359: 219–225. [DOI] [PubMed] [Google Scholar]
- 41. Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, et al. (2012) The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer discovery 2: 401–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mancini D, Singh S, Ainsworth P, Rodenhiser D (1997) Constitutively methylated CpG dinucleotides as mutation hot spots in the retinoblastoma gene (RB1). American journal of human genetics 61: 80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rhee I, Bachman KE, Park BH, Jair KW, Yen RW, et al. (2002) DNMT1 and DNMT3b cooperate to silence genes in human cancer cells. Nature 416: 552–556. [DOI] [PubMed] [Google Scholar]
- 44. Kim YH, Lee HC, Kim SY, Yeom YI, Ryu KJ, et al. (2011) Epigenomic analysis of aberrantly methylated genes in colorectal cancer identifies genes commonly affected by epigenetic alterations. Annals of surgical oncology 18: 2338–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Herbst A, Rahmig K, Stieber P, Philipp A, Jung A, et al. (2011) Methylation of NEUROG1 in serum is a sensitive marker for the detection of early colorectal cancer. The American journal of gastroenterology 106: 1110–1118. [DOI] [PubMed] [Google Scholar]
- 46. Zou H, Yu B, Zhao R, Wang Z, Cang H, et al. (2002) Detection of aberrant p16 methylation in the serum of colorectal cancer patients. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine] 36: 499–501. [PubMed] [Google Scholar]
- 47. Ben-Porath I, Thomson MW, Carey VJ, Ge R, Bell GW, et al. (2008) An embryonic stem cell-like gene expression signature in poorly differentiated aggressive human tumors. Nature genetics 40: 499–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kodach LL, Jacobs RJ, Heijmans J, van Noesel CJ, Langers AM, et al. (2010) The role of EZH2 and DNA methylation in the silencing of the tumour suppressor RUNX3 in colorectal cancer. Carcinogenesis 31: 1567–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hashimoto H, Vertino PM, Cheng X (2010) Molecular coupling of DNA methylation and histone methylation. Epigenomics 2: 657–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cheng X, Blumenthal RM (2011) Introduction – Epiphanies in epigenetics. Progress in molecular biology and translational science 101: 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kashuba VI, Pavlova TV, Grigorieva EV, Kutsenko A, Yenamandra SP, et al. (2009) High mutability of the tumor suppressor genes RASSF1 and RBSP3 (CTDSPL) in cancer. PloS one 4: e5231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Molenaar JJ, Koster J, Zwijnenburg DA, van Sluis P, Valentijn LJ, et al. (2012) Sequencing of neuroblastoma identifies chromothripsis and defects in neuritogenesis genes. Nature 483: 589–593. [DOI] [PubMed] [Google Scholar]
- 53. Beckman RA, Loeb LA (2006) Efficiency of carcinogenesis with and without a mutator mutation. Proceedings of the National Academy of Sciences of the United States of America 103: 14140–14145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Rai K, Sarkar S, Broadbent TJ, Voas M, Grossmann KF, et al. (2010) DNA demethylase activity maintains intestinal cells in an undifferentiated state following loss of APC. Cell 142: 930–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mizuno H, Spike BT, Wahl GM, Levine AJ (2010) Inactivation of p53 in breast cancers correlates with stem cell transcriptional signatures. Proceedings of the National Academy of Sciences of the United States of America 107: 22745–22750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lang MF, Yang S, Zhao C, Sun G, Murai K, et al. (2012) Genome-wide profiling identified a set of miRNAs that are differentially expressed in glioblastoma stem cells and normal neural stem cells. PloS one 7: e36248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Peltomaki P (2012) Mutations and epimutations in the origin of cancer. Experimental cell research 318: 299–310. [DOI] [PubMed] [Google Scholar]
- 58. Pavlicek A, Paces J, Zika R, Hejnar J (2002) Length distribution of long interspersed nucleotide elements (LINEs) and processed pseudogenes of human endogenous retroviruses: implications for retrotransposition and pseudogene detection. Gene 300: 189–194. [DOI] [PubMed] [Google Scholar]
- 59. Shih IM, Zhou W, Goodman SN, Lengauer C, Kinzler KW, et al. (2001) Evidence that genetic instability occurs at an early stage of colorectal tumorigenesis. Cancer research 61: 818–822. [PubMed] [Google Scholar]
- 60. Schuebel KE, Chen W, Cope L, Glockner SC, Suzuki H, et al. (2007) Comparing the DNA hypermethylome with gene mutations in human colorectal cancer. PLoS genetics 3: 1709–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Chan MW, Chu ES, To KF, Leung WK (2004) Quantitative detection of methylated SOCS-1, a tumor suppressor gene, by a modified protocol of quantitative real time methylation-specific PCR using SYBR green and its use in early gastric cancer detection. Biotechnology letters 26: 1289–1293. [DOI] [PubMed] [Google Scholar]
- 62. Lorente A, Mueller W, Urdangarin E, Lazcoz P, von Deimling A, et al. (2008) Detection of methylation in promoter sequences by melting curve analysis-based semiquantitative real time PCR. BMC cancer 8: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Primer sequences for PCR amplification. Table S2. List of methylation specific primers. Table S3. Methylation landscape of CSMD1 studied in tumors.
(XLSX)
Characterization of CSMD1 methylation in colorectal tumors. a.) A demonstration of methylation-specific PCR melt curve analysis peaks that differentiate between methylated and unmethylated ALX4 in colorectal cancer tumors studied. b.) A demonstration of methylation-specific PCR melt curve analysis peaks that differentiate between methylated and unmethylated peaks in CSMD1 at position CG3265577 in the colorectal tumors studied.
(TIF)