Abstract
Fatigue has been shown to alter the biomechanics of lower extremity during landing tasks. To date, no study has examined the effects of two types of fatigue on kinetics and kinematics.
Objectives
This study was conducted to assess biomechanical differences between two fatigue protocols [Slow Linear Oxidative Fatigue Protocol (SLO-FP) and Functional Agility Short-Term Fatigue Protocol (FAST-FP)].
Design
Single-group repeated measures design.
Methods
Fifteen female collegiate soccer players had to perform five successful trials of unanticipated sidestep cutting (SS) pre- and post-fatigue protocols. The SLO-FP consisted of an initial VO2peak test followed by 5-min rest, and a 30-min interval run. The FAST-FP consisted of 4 sets of a functional circuit. Biomechanical measures of the hip and knee were obtained at different instants while performing SS pre- and post-fatigue. Repeated 2 × 2 ANOVAs were conducted to examine task and fatigue differences. Alpha level set a priori at 0.05.
Results
During the FAST-FP, participants had increased knee internal rotation at initial contact (IC) (12.5 ± 5.9°) when compared to the SLO-FP (7.9 ± 5.4°, p < 0.001). For hip flexion at IC, pre-fatigue had increased angles (36.4 ± 8.4°) compared to post-fatigue (30.4 ± 9.3°, p = 0.003), also greater knee flexion during pre-fatigue (25.6 ± 6.8°) than post-fatigue (22.4 ± 8.4°, p = 0.022).
Conclusion
The results of this study showed that hip and knee mechanics were substantially altered during both fatigue conditions.
Keywords: Fatigue, SLO-FP, FAST-FP, Biomechanics, Lower extremity
1. Introduction
Non-contact anterior cruciate ligament (ACL) injuries remain a problem in the athletic population, particularly in females.1 Current research reports that an estimated 80,000 to more than 250,000 ACL injuries are occurring each year, with female athletes being 4–6 times more likely to sustain a serious knee injury than their male counterparts.2,3 Multiple negative health consequences have also been reported following ACL injury including early onset of arthritis, chondral surface or meniscal damage, and functional instability leading to a decrease in the activity level of the individual.4 Given the long-term implications, a great deal of research has been directed towards determining a link between potential risk factors and the biomechanics of movement patterns.5–7
Improper mechanics during dynamic maneuvers, such as the sidestep cut, have commonly been reported to place significant force and strain on the ACL.8,9 When combined with an unanticipated movement, the neuromuscular control and movement parameters are altered even further.10 Sidestep cutting task has been commonly utilized when investigating non-contact ACL injuries.7,9,11 Females have been shown to execute sidestep cutting maneuvers with less hip flexion and abduction, greater internal rotation, as well as less knee flexion and increased knee internal rotation, greater knee abduction and rearfoot pronation when compared to males.11 This detrimental position has been found to become more distinct in the presence of fatigue and with a decision process involved (e.g., unanticipated tasks).8–10
Fatigue is considered to be a main factor affecting the musculoskeletal system due to its association with decreased knee proprioception and increased joint laxity12 in turn decreasing the capability of the skeletal muscle to generate force production.13,14 Current research analyzing fatigue and its association with altered neuromuscular control strategies has focused on different types of fatigue protocols; either a short-term or a long-term.8,9,15 The short-term protocols have focused on inducing fatigue with a series of consecutive repetitions of explosive movements such as vertical jumps combined with short sprints,8 single-leg squats,15 or double-leg squats combined with a jump sequence.10 The long-term protocols have focused on inducing fatigue by performing a 60-min shuttle run consisting of 15-min blocks of walking, running, and sprinting.9 By utilizing a soccer-specific short-term fatigue protocol and examining both types of fatigue protocols, we aim to further understand the neuromechanical differences induced by each type of fatigue protocol. Therefore, the purpose of this study was to determine biomechanical differences between two fatigue protocols as measured by lower extremity biomechanics when performing an unanticipated sidestep cutting task.
2. Methods
Based on data from previous studies focusing on the effects of fatigue on lower extremity biomechanics8,10,16 and to achieve 80% statistical power with an alpha level of 0.05, a sample of convenience of fifteen NCAA Division I female soccer players (mean age = 19.2 ± 0.8 years; height = 1.67 ± 0.05 m; mass = 61.7 ± 8.1 kg) were selected to participate in this study. Institutional Review Board approval and participants written informed consent were obtained prior to testing. Participants were excluded if they suffered from a cardiovascular or respiratory disease, or had a previous injury that would prevent them from successfully completing the fatigue protocols or dynamics tasks.16 The dominant leg, defined as the leg that the participant would use to kick a soccer ball as far as possible, was used for analysis.
Eight high-speed video cameras (Vicon, Oxford, England) were used to track marker trajectory at a sampling rate of 270 Hz, and two force plates (Bertec Corporation, Columbus OH, USA) with a sampling rate of 1080 Hz provided ground reaction force data. The participants wore spandex shorts, sports bras, or tight-fitting clothing. The team running shoes provided at the beginning of the season were used for the analysis (Adidas Supernova, AG, Herzogenaurach, Germany). Participants were given a 10-min warm-up period and then forty reflective markers were placed on specific anatomical landmarks. From those forty, ten were calibration markers, which included the bilateral greater trochanters, medial and lateral knee, and medial and lateral malleoli. The remaining markers consisted of the posterior and anterior superior iliac crests, marker clusters for the thighs and shanks, and five markers on each foot. A standing trial and a trial while moving the hips in a circular motion were obtained. After those trials, the calibration markers were removed. A Polar heart rate monitor was placed on the participant’s chest prior to calibration.
A visualization of two soccer scenarios, the ball cutting to one side and the ball stopping, were randomly generated and projected onto a screen in front of the participants.17 The unanticipation factor and the environment were intended to mimic a decision-making soccer movement task. A Brower Timing System (Brower Timing Systems, Draper, UT, USA) was used to control the approach speed. The sidestep cutting task consisted of a running approach, placement of the dominant foot on the force plate followed by a 45° cutting maneuver to the contralateral side of the foot.22 The participants performed five trials for each task pre- and post-fatigue. Prior to data collection, the participants practiced a minimum of three trials or until they felt comfortable with the tasks. There was a 1-min rest period between pre-fatigue trials to minimize fatigue.
Visual 3D (C-Motion, Germantown, MD, USA) was used to create a lower extremity kinematic model for each participant, taken from the standing trial. The kinematic model was used to quantify the motion at the hip, knee, and ankle joints utilizing standard inverse dynamics.18 The convention used for flexion-extension, abduction-adduction, and internal-external rotation was comparative to a joint coordinate system.19 An estimated functional hip joint center was established by using the standing trial with circular motion of the pelvis.20 Based on a power spectrum analysis, marker trajectory was filtered with a fourth-order Butterworth zero lag filter with a 7 Hz cutoff frequency and the ground reaction force data were filtered with a similar filter with a 25Hz cutoff frequency.
The Functional Agility Short-Term Fatigue Protocol (FAST-FP) was established by combining various agility movements in order to mimic multiple direction-changing and sprinting patterns that a soccer athlete would endure during a competitive match. The FAST-FP started with obtaining each participant’s maximum vertical jump by using measuring tape set up on a wall. A 30-cm high box was used to complete a series of step up and down movements against the wall for 20 s at 220 beats per minute (bpm) controlled by a metronome. Following the step up drill, one repetition of the “L-drill” was then performed between three cones that were set at a distance of five yards apart in the shape of an L. Participants began the drill by sprinting five yards to the first cone, sprinting back to the starting cone, and back to the previous cone where they ran around it and cut right to the third cone. Participants then ran in a circle around the third cone from the inside to the outside and ran around the second cone before running to the first cone. Immediately following the “L-drill”, participants performed five consecutive counter-movement jumps at the measuring tape set up on the wall making sure to stay within 78–82% of their maximum vertical jump recorded prior to the start of the protocol. Following the counter-movement jumps, the participants then ran down and back on an agility ladder. Participants ran in the forward direction making sure to touch both feet inside each space of the ladder the first and third times the protocol was completed. Participants had to perform four sets of the protocol with no rest in between, which took approximately 5 min per participant. The second and fourth time the protocol was completed the participant faced sideways down the agility ladder making sure to touch both feet inside the spaces of the ladder. The participants also performed the agility ladder to the rhythm of the metronome at 220 bpm so that the participant would maintain a constant speed throughout the protocol. The L drill and the ladder drill were both used in this protocol to imitate the functional demands of soccer. Completing the four tasks (step-up and down movements, L drill, vertical jumps, and agility ladder drill) counted as one set of the protocol.
For the Slow Linear Oxidative Fatigue Protocol (SLO-FP), height and mass were measured and body mass index (BMI) was calculated. Submaximal O2 consumption and VO2peak was measured using a SensorMedics Vmax 29c metabolic cart (Yorba Linda, CA) during pre- and post-testing sessions. VO2peak was calculated as the average of the three highest, continuous 20-s interval VO2 measurements. An incremental treadmill protocol that maintained a 0° incline was used throughout testing to more closely approximate the achievable maximal oxygen consumption during competitive play.21 Resting and exercise heart rate measurement were taken using the Polar heart rate monitor during all testing. The protocol was explained to the participant and the participant’s were fitted with the mouthpiece and headset, which they were required to wear for the VO2 max test. Participants began the fatigue protocol by performing a VO2 max test.21 The protocol used for the VO2 max test required the participants to run at a speed of 9 km/h for 5 min, followed by an increase in speed at 1 km increments every 2 min until maximally fatigued. When the participants felt as though they were maximally fatigued and could no longer continue running they were instructed to grab the sides of the treadmill, at which point the investigator slowed down the treadmill to a walk. The participants were considered maximally fatigued when two of the four following criteria were met: (1) participant’s heart rate reached 90% of their age calculated max heart rate, (2) respiratory quotient greater than 1.1, (3) plateau in the VO2 max curve, and/or (4) the participant was unable to continue running due to volitional exhaustion. Following the VO2 max test, the participants were given a 5-min rest period while the researchers calculated the running speeds for the 30-min treadmill run. During the 30-min treadmill run, the participants were required to run at a speed of 70% of their VO2 max for 4 min, followed by running for 1 min at 90% of their VO2 max.9 The participant’s continued to alternate between speeds until the 30 min had elapsed, mimicking an interval run.
Paired t-tests were used to compare pre-fatigue conditions (SLO-FP vs. FAST-FP). This was conducted to assess baseline assumption for possible comparison of the post-fatigue conditions between the SLO and FAST fatigue protocols. Fatigue protocol and time were treated as independent variables. A 2 (fatigue protocol; SLO-FP and FAST-FP) × 2 (time; pre- and post-fatigue) factor repeated measures analysis of variance (ANOVA) was conducted for each dependent variable at each time instant analyzed. The dependent variables used in this study include: knee flexion, knee abduction, knee rotation, hip flexion, hip abduction, hip rotation, vertical and posterior ground reaction forces, knee flexion-extension moment, knee abduction-adduction moment, and hip abduction moment. These variables were measured at different time instants that include: initial contact, peak vertical and posterior ground reaction forces, peak knee flexion, and peak stance phase. Each trial was normalized to 100% of stance phase (101 data points); defined as initial contact to toe off from the force plate.16,22 Initial contact was defined as the time instant where vertical ground reaction force is higher than 10 N, whereas peak stance is defined as the maximum value for each dependent variable within the first 50% of the stance phase. All data were reduced using a custom Matlab (Math Works, Inc., Natick, MA, USA) program and Visual 3D to export into a Microsoft Excel spreadsheet. Each of the five trials were averaged and exported into SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) for data analysis with alpha level being set a priori at 0.05.
3. Results
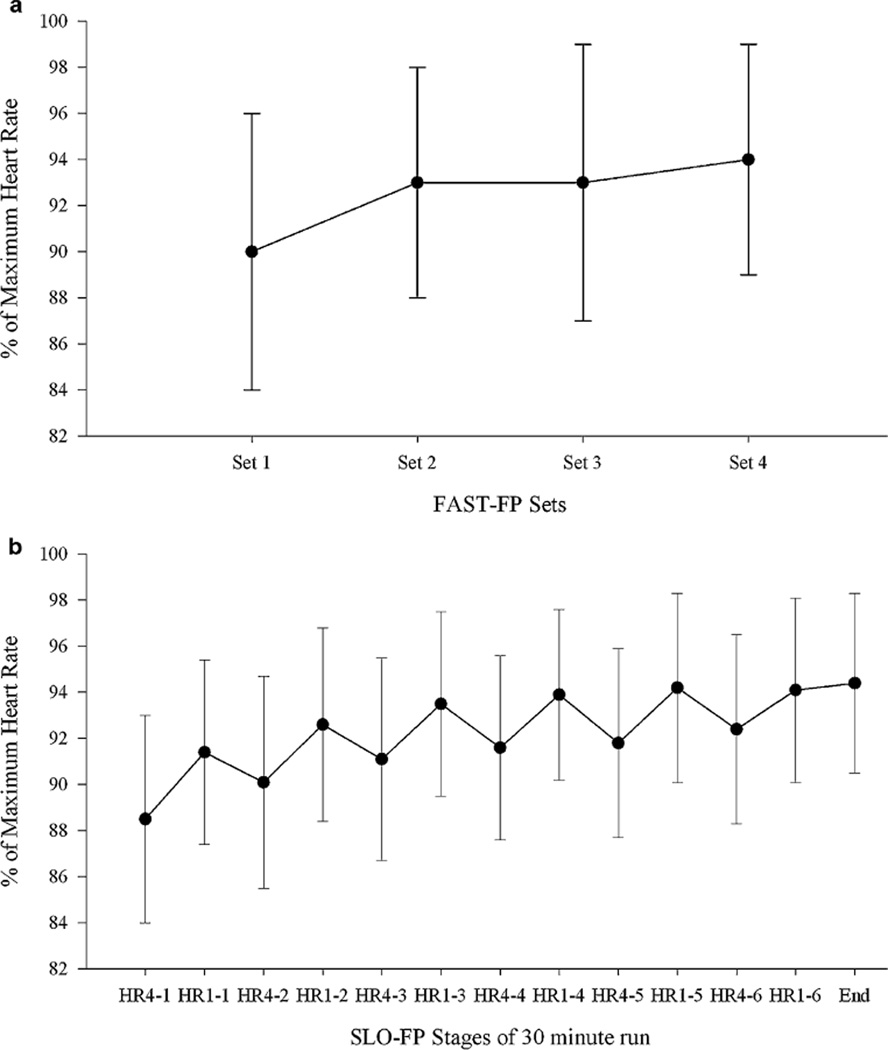
Descriptive statistics for kinematic and kinetic data are presented in Tables 1 and 2. The participants had an approach speed of 3.72 m/s (SD 0.27) pre-SLO, 3.62 m/s (SD 0.13) post-SLO, 3.64 m/s (SD 0.13) pre-FAST and 3.51 m/s (SD 0.17) post-FAST. Speeds were not significantly different, p > 0.05. Participants involved in this study were working at approximately 89.6% of their maximum heart rate, meaning they had reached their anaerobic threshold in both the FAST-FP and SLO-FP (Fig. 1).23
Table 1.
Descriptive statistics (mean, standard deviation) for kinematic variables between two fatigue protocols at initial contact, peak vertical ground reaction force (PVGRF), peak posterior ground reaction force (PPGRF), peak knee flexion (PKF), and peak stance. All variables measured in degrees.
| SLO-FP | FAST-FP | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | |||||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | |
| Initial contact | ||||||||||||
| Knee flexion (−)/extension (+) | −25.8 | 5.7 | −28.9, −22.6 | −22.6 | 9.7 | −28.0, −17.3 | −25.5 | 8.0 | −29.9, −21.1 | −22.3 | 7.1 | −26.2, −18.3 |
| Knee abduction (−)/adduction (+) | −1.1 | 3.0 | −2.7, 0.6 | −1.9 | 2.8 | −3.4, −0.3 | −2.0 | 2.5 | −3.4, −0.6 | −2.4 | 3.7 | −4.4, −0.4 |
| Knee external (−)/internal rotation (+) | 7.6 | 6.3 | 4.1, 11.1 | 8.4 | 4.5 | 5.9, 10.9 | 14.2 | 6.2 | 4.7, 11.2 | 10.9 | 5.6 | 7.8, 14.0 |
| Hip flexion (+)/extension (−) | 36.2 | 8.7 | 31.4, 41.1 | 32.6 | 9.3 | 27.5, 37.7 | 36.5 | 8.0 | 32.1, 41.0 | 28.1 | 9.3 | 23.0, 33.3 |
| Hip external (−)/internal rotation (+) | 13.2 | 9.4 | 7.9, 18.4 | 10.1 | 8.3 | 4.3, 15.9 | 9.7 | 6.6 | 6.0, 13.4 | 5.7 | 9.4 | 0.4, 10.9 |
| PVGRF | ||||||||||||
| Knee flexion (−)/extension (+) | −41.9 | 8.2 | −46.4, −37.3 | −40.1 | 7.3 | −44.1, −36.1 | −41.6 | 7.7 | −45.9, −37.3 | −37.4 | 6.8 | −41.2, −33.6 |
| Knee abduction (−)/adduction (+) | −2.0 | 5.3 | −4.9, 1.0 | −3.0 | 5.3 | −5.9, 0.0 | −3.7 | 4.0 | −5.9, −1.5 | −3.4 | 6.2 | −6.8, 0.0 |
| Knee external (−)/internal rotation (+) | 14.1 | 6.0 | 10.8, 17.4 | 14.7 | 4.7 | 12.3, 17.3 | 14.2 | 6.2 | 10.8, 17.6 | 17.5 | 5.6 | 14.4 |
| Hip flexion (+)/extension (−) | 31.8 | 10.6 | 25.9, 37.6 | 28.0 | 10.8 | 22.1, 34.0 | 32.1 | 9.0 | 27.1, 37.1 | 23.2 | 10.9 | 17.2, 29.3 |
| Hip external (−)/internal rotation (+) | 7.8 | 9.4 | 2.7, 13.0 | 3.8 | 10.9 | −2.2, 9.8 | 4.4 | 7.5 | 0.2, 8.5 | 0.3 | 8.9 | −4.6, 5.3 |
| PPGRF | ||||||||||||
| Knee flexion (−)/extension (+) | −36.8 | 5.0 | −39.6, −34.1 | −36.2 | 8.2 | −40.7, −31.6 | −34.2 | 8.6 | −39.0, −29.5 | −31.2 | 7.7 | −35.5, −26.9 |
| Knee external (−)/internal rotation (+) | 12.8 | 5.9 | 9.5, 16.0 | 14.1 | 5.2 | 11.2, 17.0 | 11.4 | 5.2 | 8.6, 14.3 | 15.1 | 4.8 | 12.4, 17.7 |
| Knee external (−)/internal rotation (+) | 12.8 | 5.9 | 9.5, 16.0 | 14.1 | 5.2 | 11.2, 17.0 | 11.4 | 5.2 | 8.6, 14.3 | 15.1 | 4.8 | 12.4, 17.7 |
| Hip flexion (+)/extension (−) | 35.2 | 8.8 | 30.3, 30.0 | 31.0 | 9.4 | 25.8, 36.2 | 35.6 | 8.2 | 31.1, 40.2 | 26.5 | 9.8 | 21.1, 31.9 |
| Hip external (−)/internal rotation (+) | 10.5 | 9.5 | 5.2, 15.8 | 6.2 | 10.5 | 0.4, 12.0 | 8.2 | 6.5 | 4.6, 11.8 | 3.1 | 9.1 | −1.9, 8.1 |
| PKF | ||||||||||||
| Knee flexion (−)/extension (+) | −54.53 | 5.14 | −57.4, −51.7 | −51.19 | 6.38 | −54.6, −47.6 | −53.07 | 7.04 | −57.0, −49.2 | −48.28 | 7.36 | −52.4, −44.2 |
| Knee abduction (−)/adduction (+) | −3.45 | 6.20 | −6.9, 0.0 | −4.60 | 6.30 | −8.1, −1.1 | −6.10 | 5.33 | −9.0, −3.1 | −5.58 | 7.63 | −9.8, 1.4 |
| Knee external (−)/internal rotation (+) | 16.59 | 6.33 | 13.1, 20.1 | 17.36 | 5.67 | 14.2, 20.5 | 17.22 | 6.64 | 13.5, 20.9 | 19.80 | 6.32 | 16.3, 23.3 |
| Peak stance | ||||||||||||
| Hip flexion (+)/extension (−) | 38.19 | 9.18 | 33.1, 43.3 | 33.89 | 9.49 | 28.6, 39.1 | 38.31 | 8.81 | 33.4, 43.2 | 29.34 | 9.73 | 24.0, 34.7 |
| Hip external (−)/internal rotation (+) | 3.14 | 9.92 | −2.4, 8.6 | −0.75 | 11.35 | −7.0, 5.5 | −0.48 | 7.60 | −4.7, 3.7 | −4.46 | 8.16 | −9.0, 0.1 |
| Knee abduction (−)/adduction (+) | −5.44 | 5.20 | −8.3, −2.6 | −6.23 | 5.00 | −9.0, −3.5 | −7.11 | 4.80 | −9.8, −4.5 | −7.18 | 6.36 | −10.7, −3.7 |
Table 2.
Descriptive statistics (mean, standard deviation) for kinetic variables between two fatigue protocols at initial contact, peak vertical ground reaction force (PVGRF), peak posterior ground reaction force (PPGRF), peak knee flexion (PKF), and peak stance. Ground reaction forces measures in multiples of body weight; internal moments measures in Nm/kg.
| SLO-FP | FAST-FP | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | |||||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | |
| Initial contact | ||||||||||||
| Knee flexion (−)/extension (+) moment | −0.020 | 0.170 | −0.120, 0.070 | 0.010 | 0.190 | −0.100, 0.110 | 0.000 | 0.170 | −0.100, 0.100 | 0.080 | 0.240 | −0.050, 0.210 |
| Knee abduction (−)/adduction (+) moment | 0.060 | 0.060 | 0.020, 0.910 | 0.050 | 0.060 | 0.020, 0.080 | 0.070 | 0.090 | 0.030, 0.120 | 0.070 | 0.080 | 0.020, 0.110 |
| Hip abduction (−)/adduction (+) moment | 0.080 | 0.130 | 0.010, 0.150 | 0.060 | 0.150 | −0.020, 0.150 | 0.120 | 0.170 | 0.020, 0.210 | 0.120 | 0.160 | 0.030, 0.210 |
| Posterior ground reaction force | 0.1 | 0.1 | 0.1, 0.2 | 0.1 | 0.1 | 0.1, 0.2 | 0.2 | 0.1 | 0.1, 0.2 | 0.2 | 0.1 | 0.1, 0.2 |
| PVGRF | ||||||||||||
| Vertical ground reaction force | 2.6 | 0.3 | 2.5, 2.8 | 2.7 | 0.4 | 2.5, 2.9 | 2.7 | 0.5 | 2.4, 2.9 | 2.8 | 0.4 | 2.5, 3.0 |
| PPGRF | ||||||||||||
| Posterior ground reaction force | 0.8 | 0.2 | 0.7, 0.9 | 0.7 | 0.2 | 0.6, 0.8 | 0.7 | 0.2 | 0.6, 0.8 | 0.7 | 0.2 | 0.6, 0.8 |
| PKF | ||||||||||||
| Posterior ground reaction force | 0.2 | 0.1 | 0.2, 0.3 | 0.3 | 0.1 | 0.2, 0.3 | 0.2 | 0.1 | 0.1, 0.3 | 0.2 | 0.1 | 0.2, 0.3 |
| Peak stance | ||||||||||||
| Knee flexion (−)/extension (+) moment | 2.110 | 0.300 | 1.940, 2.280 | 1.950 | 0.270 | 1.800, 2.090 | 1.920 | 0.280 | 1.770, 2.070 | 1.880 | 0.290 | 1.720, 2.040 |
| Knee abduction (−)/adduction (+) moment | 0.420 | 0.400 | 0.200, 0.640 | 0.290 | 0.160 | 0.200, 0.380 | 0.430 | 0.360 | 0.230, 0.640 | 0.370 | 0.270 | 0.230, 0.520 |
Fig. 1.
(a) Average percentage of estimated maximum heart rate for participants in each set of the functional agility short-term fatigue protocol; (b) average percentage of maximum heart rate for participants during the slow linear oxidative fatigue protocol. HR4-1 – heart rate during 4 min at 70% of their maximum speed set 1; HR1-1 – heart rate during 1 min at 90% of their maximum speed at set 1.
At initial contact, the primary changes were observed for overall fatigue despite the protocol used. The majority of the dependent measures presented higher values at pre-fatigue than post-fatigue, which demonstrates a detrimental effect of fatigue. This was specifically obtained for knee flexion (F1,14 = 6.669, p = 0.022, d = 0.38), hip flexion (F1,14 = 13.373, p = 0.003, d = 0.65), and hip internal rotation (F1,14 = 5.724, p = 0.031, d = 0.35). The only exception noted between protocols was that throughout the FAST-FP participants had increased internal knee rotation [mean 12.5° (SD 5.9)] when compared to the SLO-FP [7.9° (SD 5.4)], F1,14 = 20.890, p < 0.001, d = 0.78.
A similar pattern was observed at peak posterior and vertical ground reaction forces and peak stance for most dependent variables. Both fatigue protocols resulted in altered biomechanical patterns between pre- and post-fatigue time, with pre-fatigue presenting increased values than post-fatigue. This was noted for knee flexion (F1,14 = 7.295, p = .017, d = 0.38), and hip internal rotation (F1,14 = 7.219, p = .018, d = 0.40) at peak vertical ground reaction. Furthermore, at peak posterior ground reaction the changes were observed for knee internal rotation (F1,14 = 5.296, p = .037, d = 0.45), and hip internal rotation (F1,14 = 11.313, p = .005, d = 0.49). Lastly, at peak stance fatigue differences were attained for knee flexion (F1,14 = 17.484, p = .001, d = 0.59), hip internal rotation (F1,14 = 10.110, p = .007, d = 0.20), hip flexion (F1,14 = 16.261, p = .001, d = 0.73), and peak knee extension moment (F1,14 = 7.720, p = .015, d = 0.34).
4. Discussion
The most important finding of this study was that female soccer athletes altered their hip and knee mechanics in as little as 5 min of physical activity. The SLO-FP and the FAST-FP elicited similar kinematic and kinetic changes to the lower extremity during the sidestep cutting task. Specifically, participants landed with decreased hip flexion, and increased hip internal rotation, as well as decreased knee flexion and decreased knee internal rotation. Regardless of the type of fatigue protocol instituted, changes in sagittal plane kinematics leading to a more extended lower extremity position at various time instants during the stop jump phase occurred. It was initially hypothesized that the agility drills used during the FAST-FP would produce a greater demand on the lower extremity compared to the SLO-FP. However, regardless of the type of protocol used, both the SLO-FP and FAST-FP resulted in the similar neuromuscular adaptations. This implies that the design of fatigue studies to modify biomechanical risk factors should be further explored by the introduction of FAST-FP or similar protocols. This protocol utilizes athletic drills to induce fatigue within a short period of time without complex clinical instruments (e.g., metabolic cart, treadmill).
The results of the current study, in which participants landed in a more erect posture post-fatigue, are consistent with previous research.8,10,15 Chappell et al. found that participants landed with decreased knee flexion while performing a stop-jump task. Our participants landed with decreased knee flexion but to a lesser degree than to the participant population in Chappell et al. One theory for this is because our study included highly conditioned collegiate soccer players whereas Chappell et al. used similarly aged individuals but they were possibly at a lower level of physical training and neuromuscular control as compared to our athletes. It is possible that our participants were used to placing higher demands on the lower extremity and could adapt to fatigue better than the recreational athletes. Another factor is that the tasks used between both studies differ; Chappell et al. analyzed a running stop-jump task, whereas we utilized a sidestep cutting task.
An extended position at landing has been associated with increased ACL load, and with increased anterior tibial shear force due to increased patellar tendon-tibia shaft angle.24,25 In a cadaveric study, it was noted that anterior tibial displacement is augmented between 15 and 45° of knee flexion, with its peak occurring at 30°.26 At initial contact, our participants were within the range that is thought to increase anterior tibial displacement, and consequently place higher stress on the ACL. We speculate that our participants had increased load on the ACL due to their erect posture at post-fatigue. This is most likely due to the mechanical disadvantage experienced by the hamstring muscles.27 Previous researchers have reported altered movement patterns during post-fatigue; specifically increased knee abduction and internal rotation angles,10,15,16 increased hip rotation angles,10,15,28 hip internal rotation moments,15 and decreased knee flexion angles.8 Specifically, knee motion resulting in increased internal tibial rotation angles have been shown to increase the load placed on the ACL.29 Our participants presented an internally rotated tibia, which might have augmented their ACL load. This fact combined with extended position may represent that fatigue induces a biomechanical position that can increase the risk for injury.
Our study presents some limitations that we cautious the reader to consider. Our participants attained a similar % of HR as previously reported during a soccer match (Fig. 1). However, the fatigue protocols may not represent a similar pattern of fatigue as the one that occur during a match. Further, we cannot precisely quantify the fatigue level presented by the participants. We used heart rate as a measure of effort and its relation with anaerobic threshold. Though, further studies should incorporate blood lactate measures and rate of perceived exertion scales to objectively quantify the level of fatigue experience throughout the protocol(s).
5. Conclusion
Based on the research of this study, female soccer players can negatively alter their mechanics in 5 min according to the similarities seen between the SLO-FP and FAST-FP. It is important to note the types of exercises that were being completed during the FAST-FP. These exercises involved quick agility movements, sprinting, cutting, jumping, and squatting at varying intensities. This information can be useful for future ACL prevention programs as well, noting how quickly athletes can alter their joint position. It is important to encourage proper mechanics when instructing prevention programs throughout the practice and not only at early stages.
Practical implications.
After 5 min of a fatigue protocol changes are observed in the lower extremity that can place an athlete at higher risk for injury.
Intervention programs should be designing to take into account the effects of fatigue on lower body mechanics.
Pre-season sport specific assessment programs should be established utilizing baseline and short-term fatigue protocols to evaluate individuals potentially at-risk for injury.
Acknowledgments
The authors gratefully acknowledge the research support from National Institute of Health (1R03AR054031-01), and the Portuguese Foundation for Science and Technology (SFRH/BD/28046/2006).
References
- 1.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33(4):524–530. doi: 10.1177/0363546504269937. [DOI] [PubMed] [Google Scholar]
- 2.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Hewett TE, Lindenfeld TN, Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 4.Yu B, Garrett WE. Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;41(Suppl. 1):i47–i51. doi: 10.1136/bjsm.2007.037192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford KR, Myer GD, Toms HE, et al. Gender differences in the kinematics of unanticipated cutting in young athletes. Med Sci Sports Exerc. 2005;37(1):124–129. [PubMed] [Google Scholar]
- 6.McLean SG, Neal RJ, Myers PT, et al. Knee joint kinematics during the sidestep cutting maneuver: potential for injury in women. Med Sci Sports Exerc. 1999;31(7):959–968. doi: 10.1097/00005768-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Pollard CD, Davis IM, Hamill J. Influence of gender on hip and knee mechanics during a randomly cued cutting maneuver. Clin Biomech (Bristol, Avon) 2004;19(10):1022–1031. doi: 10.1016/j.clinbiomech.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Chappell JD, Herman DC, Knight BS, et al. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33(7):1022–1029. doi: 10.1177/0363546504273047. [DOI] [PubMed] [Google Scholar]
- 9.Sanna G, O’Connor KM. Fatigue-related changes in stance leg mechanics during sidestep cutting maneuvers. Clin Biomech (Bristol, Avon) 2008;23(7):946–954. doi: 10.1016/j.clinbiomech.2008.03.065. [DOI] [PubMed] [Google Scholar]
- 10.Borotikar BS, Newcomer R, Koppes R, et al. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clin Biomech (Bristol, Avon) 2008;23(1):81–92. doi: 10.1016/j.clinbiomech.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 11.McLean SG, Lipfert SW, van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36(6):1008–1016. doi: 10.1249/01.mss.0000128180.51443.83. [DOI] [PubMed] [Google Scholar]
- 12.Rozzi SL, Lephart SM, Fu FH. Effects of muscular fatigue on knee joint laxity and neuromuscular characteristics of male and female athletes. J Athl Train. 1999;34(2):106–114. [PMC free article] [PubMed] [Google Scholar]
- 13.Enoka RM, Stuart DG. Neurobiology of muscle fatigue. J Appl Physiol. 1992;72(5):1631–1648. doi: 10.1152/jappl.1992.72.5.1631. [DOI] [PubMed] [Google Scholar]
- 14.Hakkinen K, Komi PV. Changes in neuromuscular performance in voluntary and reflex contraction during strength training in man. Int J Sports Med. 1983;4(4):282–288. doi: 10.1055/s-2008-1026051. [DOI] [PubMed] [Google Scholar]
- 15.McLean SG, Samorezov JE. Fatigue-induced ACL injury risk stems from a degradation in central control. Med Sci Sports Exerc. 2009;41(8):1661–1672. doi: 10.1249/MSS.0b013e31819ca07b. [DOI] [PubMed] [Google Scholar]
- 16.McLean SG, Felin RE, Suedekum N, et al. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc. 2007;39(3):502–514. doi: 10.1249/mss.0b013e3180d47f0. [DOI] [PubMed] [Google Scholar]
- 17.Cortes N, Blount E, Ringleb S, et al. Soccer-specific video simulation for improving movement assessment. Sports Biomech/Int Soc Biomech Sports. 2011;10(1):12–24. doi: 10.1080/14763141.2010.547591. [DOI] [PubMed] [Google Scholar]
- 18.Winter DA. Biomechanics and motor control of human movement. Third ed. West Sussex: John Wiley & Sons, Inc.; 2005. pp. 75–102. [Google Scholar]
- 19.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 20.Begon M, Monnet T, Lacouture P. Effects of movement for estimating the hip joint centre. Gait Posture. 2007;25(3):353–359. doi: 10.1016/j.gaitpost.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Flouris AD, Metsios GS, Koutedakis Y. Contribution of muscular strength in cardiorespiratory fitness tests. J Sports Med Phys Fitness. 2006;46(2):197–201. [PubMed] [Google Scholar]
- 22.McLean SG, Huang X, van den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech (Bristol, Avon) 2005;20(8):863–870. doi: 10.1016/j.clinbiomech.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Koutedakis Y, Sharp NC. Lactic acid removal heart rate frequencies during recovery after strenuous rowing exercise. Br J Sports Med. 1985;19(4):199–202. doi: 10.1136/bjsm.19.4.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu B, Lin CF, Garrett WE. Lower extremity biomechanics during the landing of a stop-jump task. Clin Biomech (Bristol Avon) 2006;21(3):297–305. doi: 10.1016/j.clinbiomech.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Hughes G, Watkins J. A risk-factor model for anterior cruciate ligament injury. Sports Med. 2006;36(5):411–428. doi: 10.2165/00007256-200636050-00004. [DOI] [PubMed] [Google Scholar]
- 26.Hirokawa S, Solomonow M, Lu Y, et al. Anterior–posterior and rotational displacement of the tibia elicited by quadriceps contraction. Am J Sports Med. 1992;20(3):299–306. doi: 10.1177/036354659202000311. [DOI] [PubMed] [Google Scholar]
- 27.Pandy MG, Shelburne KB. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech. 1997;30(10):1015–1024. doi: 10.1016/s0021-9290(97)00070-5. [DOI] [PubMed] [Google Scholar]
- 28.Baca A. A comparison of methods for analyzing drop jump performance. Med Sci Sports Exerc. 1999;31(3):437–442. doi: 10.1097/00005768-199903000-00013. [DOI] [PubMed] [Google Scholar]
- 29.Markolf KL, Burchfield DM, Shapiro MM, et al. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]