Abstract
Few recent reports have indicated that Mycobacterium massiliense causes various infections including respiratory infection. However, there is scarce information on the clinical significance, natural history of the infection, and therapeutic strategy. This report describes a case of an immunocompetent old man infected by M. massiliense that causes acute respiratory failure. In light of the general courses of non-tuberculous mycobacterium infections, rapid progression and fatality are very rare and odd. In addition, we discuss the biological and pathological properties of M. massiliense with the review of cases reported previously including our fatal one.
Keywords: Mycobacterium; Mycobacterium Infections, Nontuberculous; Respiratory Insufficiency
Introduction
Mycobacterium massiliense was originally classified as the Mycobacterium abscessus-chelonae complex1. Although, to date, the knowledge of clinical manifestations of the infectious diseases caused by M. massiliense is limited, M. massiliense is known to attack various organs in our body such as skin and lung1,2. As for the pulmonary infection, according to one recent study, microbiologic response to the antibiotic therapy was more favorable in patients with M. massiliense (88%) than in those with M. abscessus lung disease (25%)3. However, there are few reports describing the fatal case of pulmonary infection by M. massiliense.
Herein, we report a fatal case of acute respiratory failure in an immunocompetent old man infected by M. massiliense.
Case Report
A 75-year-old man visited our hospital to treat pulmonary non-tuberculous mycobacterium (NTM) disease. He had complained productive cough for two months, and his diagnosis was confirmed by bacteriological analysis using sputum specimen. He was non-smoker and had no specific history of chronic diseases. His vital signs were normal. On physical examination, inspiratory crackles were heard on the right lower lung field. The results of blood test showed no definitive abnormality. A serologic test for human immunodeficiency virus was negative.
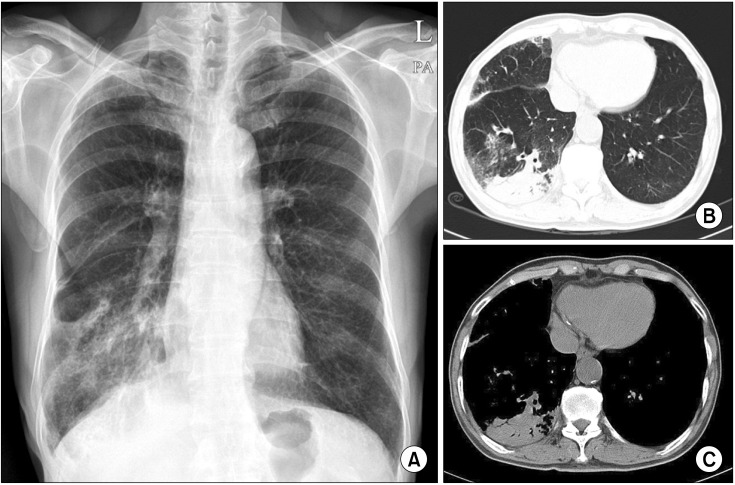
Chest X-ray revealed increased opacities in the right lower lobe (Figure 1A). Computed tomography scan of chest showed consolidation with air-bronchogram in the right lower lobe and focal centrilobular nodules on the right middle lobe (Figure 1B, C). On the bacteriological test, we verified the positive reactivity of acid fast staining in bronchial washing fluids. Moreover, we could find NTM DNA in the lung tissues obtained by percutaneous transthoracic needle biopsy using polymerase chain reaction. Finally, M. massiliense was identified from a sputum specimen and a bronchial washing sample, respectively, by a reverse blot hybridization assay. However, there was no evidence of growth for other bacteria, fungi, and virus in microbiological examination.
Figure 1.
(A) Chest X-ray showed increased opacities in the right lower lobe. (B, C) Contrast-enhanced computed tomography scan of chest demonstrated consolidation within air-bronchogram in the right lower lobe.
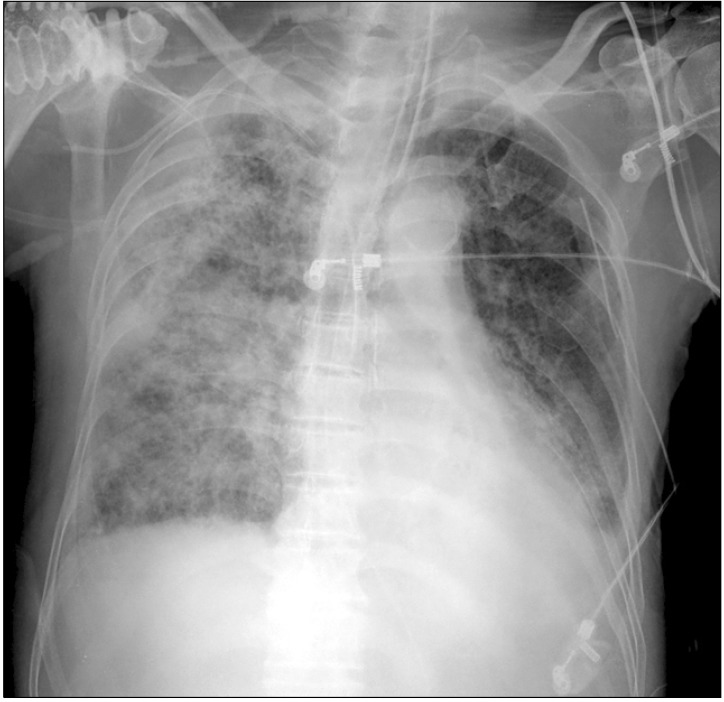
According to the diagnositc criteria provided by the American Thoracic Society4, he was diagnosed as M. massiliense pulmonary infection, and the treatment was started with clarithromycin, amikacin, imipenem, and doxycycline. But he rapidly developed a severe respiratory failure at 7 days after the initiation of medical treatment. Patient complained severe dyspnea with tachypnea, showing respiratory rate of 32 breaths per minute. Arterial blood gas analysis revealed that PO2, PCO2, pH, and PaO2/FiO2 ratio were 49.9 mm Hg, 25.4 mm Hg, 7.465, and 81 mm Hg, respectively. Chest X-ray showed diffuse bilateral infiltrates (Figure 2). No improvement of gas exchange was obtained despite the support of mechanical ventilation, moreover, respiratory acidosis worsened to extreme levels. On the day 25 of diagnosis, the patient progressed to multi-organ failure resulting in his death.
Figure 2.
Chest X-ray during medical treatment in the intensive care unit showed diffuse bilateral infiltration.
Discussion
NTM are found in the environment ubiquitously and are formerly considered to be minor clinical significance4. Recently, the incidence of diseases caused by NTM is increased and they relatively often cause pulmonary infection than other organ infection. Lung disease by NTM has been reported to progress very slowly, and the majority of pulmonary NTM diseases can resolve spontaneously without specific treatment. In addition, most of patients susceptible to NTM are in an immunocompromised state or have underlying structural disease of lung such as bronchiectasis.
M. massiliense is newly classified into rapid growing NTM, sharing an identical 16S rRNA sequence with M. abscessus. A study showed that nearly half (47%) of all M. abscessus complex are identified as M. massiliense2. However, to date, the clinical manifestations of the M. massiliense infection are not well known. As for the therapeutic response rate to clarithromycin-based antibiotic therapy, it is higher in patients infected with M. massiliense than in those with M. abscessus3. Actually, pneumonia of an immunocompetent patient caused by M. massiliense improved after treatment with clarithromycin and minocycline5. On the other hand, a fatal case of bacteremia caused by M. massiliense was also reported6. In this case, M. massiliense was isolated from the blood of a kidney transplant patient, and the M. massiliense bacteremia leaded to sudden death of the patient like our current case. Therefore, the clinical manifestations of M. massiliense infection, in particular pulmonary infection, seem to be a precautious issue.
In light of the general courses of NTM infection, our current case is not only very unfamiliar but also fatal. His pulmonary disease progressed very fast and showed no response to any antibiotic therapy including clarithromycin. This unusual case indicates that specialized physicians for respiratory and/or infectious diseases should pay attention for the possibility of a fatal course of the NTM pulmonary disease even in an immunocompetent and relatively healthy subject although this entity of NTM infection has a favorable prognosis in general.
Acknowledgements
We thank Professor Mie-Jae Im (Chonbuk National University Medical School, Jeonju, Korea) for critical readings of the manuscript. This work was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health and Welfare, Republic of Korea (A084144) and by fund of Biomedical Research Institute, Chonbuk National University Hospital.
References
- 1.Kim HY, Yun YJ, Park CG, Lee DH, Cho YK, Park BJ, et al. Outbreak of Mycobacterium massiliense infection associated with intramuscular injections. J Clin Microbiol. 2007;45:3127–3130. doi: 10.1128/JCM.00608-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim HY, Kook Y, Yun YJ, Park CG, Lee NY, Shim TS, et al. Proportions of Mycobacterium massiliense and Mycobacterium bolletii strains among Korean Mycobacterium chelonae-Mycobacterium abscessus group isolates. J Clin Microbiol. 2008;46:3384–3390. doi: 10.1128/JCM.00319-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koh WJ, Jeon K, Lee NY, Kim BJ, Kook YH, Lee SH, et al. Clinical significance of differentiation of Mycobacterium massiliense from Mycobacterium abscessus. Am J Respir Crit Care Med. 2011;183:405–410. doi: 10.1164/rccm.201003-0395OC. [DOI] [PubMed] [Google Scholar]
- 4.Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367–416. doi: 10.1164/rccm.200604-571ST. [DOI] [PubMed] [Google Scholar]
- 5.Adekambi T, Reynaud-Gaubert M, Greub G, Gevaudan MJ, La Scola B, Raoult D, et al. Amoebal coculture of "Mycobacterium massiliense" sp. nov. from the sputum of a patient with hemoptoic pneumonia. J Clin Microbiol. 2004;42:5493–5501. doi: 10.1128/JCM.42.12.5493-5501.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tortoli E, Gabini R, Galanti I, Mariottini A. Lethal Mycobacterium massiliense sepsis, Italy. Emerg Infect Dis. 2008;14:984–985. doi: 10.3201/eid1406.080194. [DOI] [PMC free article] [PubMed] [Google Scholar]