Abstract
Background:
This randomized study was conducted to compare the hemodynamic changes and emergence characteristics of sevoflurane versus propofol anesthesia for microlaryngeal surgery.
Methods:
Forty adult patients undergoing microlaryngoscopy were randomly allocated into two groups. In propofol group, anesthesia was induced with 2-3 mg/kg propofol and maintained with propofol infusion 50-200 μg/kg/h. In sevoflurane group induction was carried out with 5-8% sevoflurane and maintained with sevoflurane in nitrous oxide and oxygen. The propofol and sevoflurane concentrations were adjusted to maintain the bispectral index of 40-60. All patients received fentanyl 2 μg/kg before induction and succinylcholine 2 mg/kg to facilitate tracheal intubation. The hemodynamic changes during induction and suspension laryngoscopy were compared. In addition, the emergence time, time to extubation, and recovery were assessed.
Results:
The changes in heart rate were comparable. The mean arterial pressure was significantly lower after induction and higher at insertion of operating laryngoscope in propofol group as compared to sevoflurane group. More patients in propofol group had episodes of hypotension and hypertension than sevoflurane group. The emergence time, extubation times, and recovery time were similar in both groups.
Conclusion:
We found that sevoflurane showed advantage over propofol in respect of intraoperative cardiovascular stability without increasing recovery time.
Keywords: General anesthesia, hemodynamic changes, microlaryngeal surgery, propofol, recovery, sevoflurane
INTRODUCTION
Microlaryngeal surgery is a stressful short surgical procedure for diagnosis and treatment of upper airway disorders, which produces an intense cardiovascular stimulation during suspension laryngoscopy.[1] The need for attenuation of cardiovascular responses and rapid emergence as well represent a dynamic clinical challenge for anesthesiologists.[2,3] Various anesthetic agents and a number of alternative anesthetic techniques have been tried with varying results.[4–6] The use of intravenous anesthesia with propofol during microlaryngeal surgery is in widespread clinical practice due to its rapidity and quality of awakening.[7–9]
Sevoflurane is a new inhaled anesthetic that also permits rapid emergence due to its low blood solubility. It has been successfully used as an alternative to propofol for various day care procedures.[10,11] Though, the use of sevoflurane in microlaryngeal surgery is not much evaluated. Combination of sevoflurane, nitrous oxide, and opioid for maintenance of anesthesia has been found to be effective in maintaining cardiovascular stability during microlaryngeal surgery.[12] This prospective, randomized study was designed to compare the effects of sevoflurane induction and maintenance of anesthesia with propofol intravenous anesthesia for hemodynamic responses and emergence characteristics in patients undergoing microlaryngeal surgery.
METHODS
After approval from institutional ethical committee, 60 adult day care patients of ASA grade I or II, undergoing microlaryngeal surgery were randomly allocated into two groups by using a computer generated random number table. Group P received propofol for induction and maintenance of anesthesia. Group S received sevoflurane-N2O-Oxygen for induction and maintenance of anesthesia. Patients with morbid obesity, having difficult airway or tracheostomy in situ were excluded. All patients were premedicated with diazepam 5 mg at night before surgery and ranitidine 150 mg with metoclopramide 10 mg in the morning of the surgery.
Standard monitoring of electrocardiogram (ECG), pulse oximetry (SpO2), non-invasive blood pressure (NIBP), capnography (ETCO2), and bispectral index (BIS) were used during intraoperative period. The patients received fentanyl 2 μg/kg 3 min before induction. In group P anesthetic induction was carried out with propofol in 20 mg increments every 5 s till the BIS value reached 60 and maintained with propofol infusion started at the rate of 200 μg/kg/min adjusted in the steps of 25 μg/ kg/ min to maintain the bispectral index between 40 and 60. In group S, anesthesia was induced with sevoflurane with 60% nitrous oxide in oxygen, with a total gas flow of 6 L/min. Sevoflurane was started at 5% then increased gradually up to 8% till BIS reached to 60. For maintenance of anesthesia 4% sevoflurane was given with 60% N2O in oxygen and adjusted in the steps of 0.4% to maintain BIS value of 40-60. Muscle relaxation was achieved with succinylcholine 2 mg/kg and additional boluses (0.5 mg/kg) were given if required. Endotracheal intubation was performed using small size (5.5/6.0 ID) cuffed microlaryngeal tube. Patients’ lungs were ventilated by intermittent positive pressure ventilation to maintain ETCO2 within 35-40 mmHg. Patient's heart rate and mean arterial pressure were recorded at pre-induction, after induction, after intubation, after insertion of operating laryngoscope, and then every 5 min till extubation. Any adverse occurrences (cough, laryngeal spasm, and bradycardia) were noted. Hypertension and hypotension were determined by a change in mean arterial pressure >20% of the pre-induction value. Hypotension was treated with ephedrine 5 mg boluses while hypertension and tachycardia (heart rate >100 beats/min) were managed with esmolol. The administration of sevoflurane and propofol was discontinued at the end of surgery. The endotracheal tube was removed when patients were conscious and breathing adequately. The duration of surgery, emergence time (time from the removal of operating laryngoscope to BIS 80), and the time to extubation were recorded.
Patients were observed in the recovery area by an investigator who was blinded to the anesthesia technique used. The hemodynamic parameters, respiratory rate, and oxygen saturation were recoded at every 10 min intervals till complete recovery. Recovery was assessed by Aldrete scoring system.[13] The time at which the patient scored an Aldrete score of 9 was noted and this was taken as recovery time. Any adverse events like, sore throat, pain, dizziness, postoperative nausea, and vomiting were assessed and treated accordingly till discharge of the patient. Patients were asked whether they had any recall of the induction or maintenance periods.
The statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 17.0 for Windows). Parametric data were analyzed using paired and non-paired t-tests with Bonferroni corrections for multiple comparisons. Qualitative or categorical variables were compared using Chi-squared or Fisher's exact test. All statistical tests were two-sided and were performed at a significance level of α = 0.05. Sample size was determined to detect a difference of 25% in time to achieve an Aldrete score of 9 with a power of 80% and an alpha error of 0.05.
RESULTS
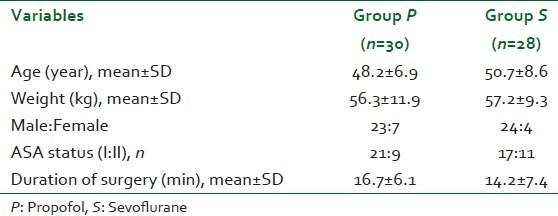
A total of 58 patients completed the study. Two patients were withdrawn from study. One patient had difficult intubation and one patient had undetected high blood pressure in sevoflurane group. The demographic variables were evenly distributed between the groups. The duration of surgery was also similar [Table 1]. Induction of anesthesia was smooth and uneventful in both the groups. Though, it was more rapid in propofol group as compared to sevoflurane group (63±11 s vs. 92±17 s, P<0.01). The bispectral index values were similar in both groups throughout the procedure.
Table 1.
Demographic data and duration of surgery
The two groups were comparable with respect to baseline heart rate and mean arterial pressure. Heart rate decreased after induction and increased after tracheal intubation in both the groups. Mean heart rate changed by 11±14 beats/min for propofol group and by 9±11 beats/min for sevoflurane group [Figure 1]. The changes in heart rate were comparable among groups. There was a significant decrease in mean arterial pressure after induction. The decrease in mean arterial pressure was 16±9 mmHg in the propofol group and 12±7 mmHg in the sevoflurane group (P<0.05). Eight patients in propofol group and two patients in sevoflurane group had transient hypotension. After tracheal intubation there was an increase in mean arterial pressure toward baseline. The mean arterial pressure was significantly higher in propofol group compared with the sevoflurane group (P<0.05) after intubation and insertion of operating laryngoscope which retuned to normal after 10 min [Figure 2].
Figure 1.
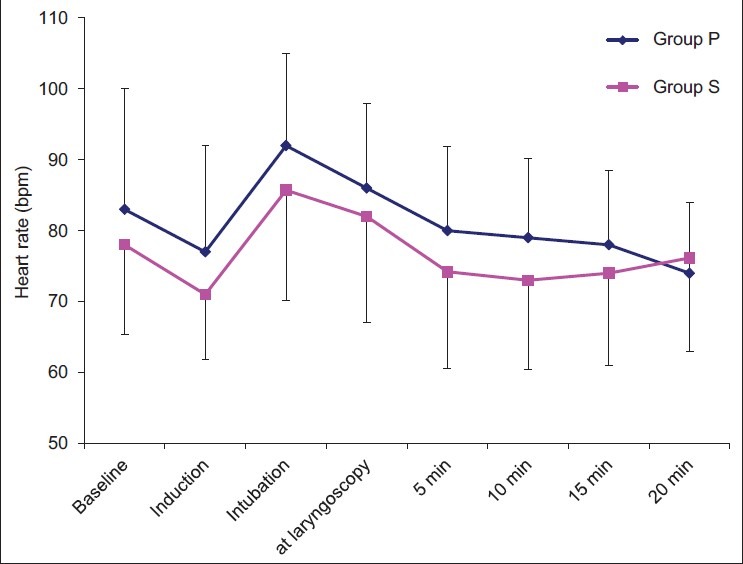
Data showing the mean heart rate in beats per min (bpm) on the y-axis in patients who received sevoflurane (group S) and propofol (group P) anesthesia. On the left of the x-axis, the time course from start of anesthesia until termination displayed in minutes. Bar indicates standard deviation
Figure 2.
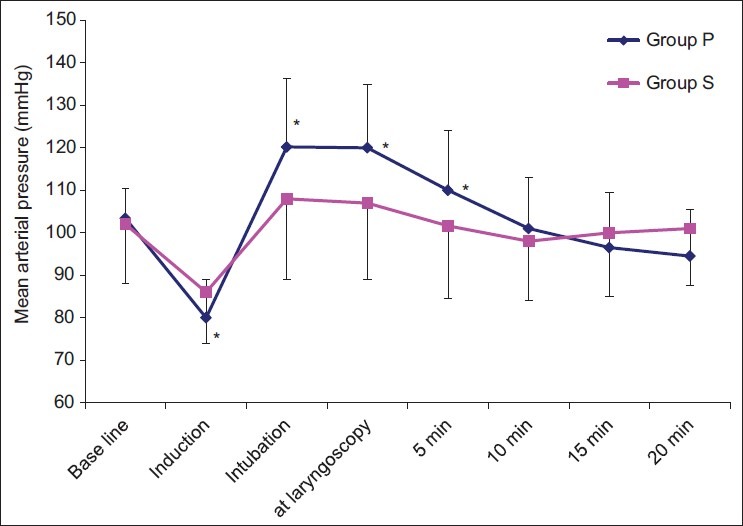
Data showing the mean arterial pressure (MAP) in mmHg on the y-axis in patients who received sevoflurane (group S) and propofol (group P) anesthesia. Values are in mean, bar indicates standard deviation. On the left of the x-axis, the time course from start of anesthesia until termination displayed in minutes. The asterisks indicate differences in MAP at the distinct time points between groups (P<0.05)
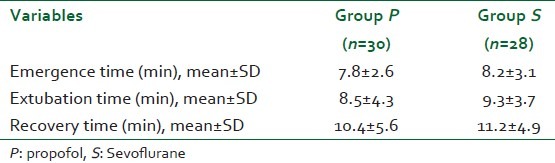
The emergence times and extubation time were not significantly different between groups [Table 2]. The recovery time to Aldrete score 9 was also similar among groups (9.4±5.6 in propofol group and 11.2±4.9 in sevoflurane group). There was no difference in postoperative heart rate, blood pressure, and oxygen saturation. The patients were comfortable during postoperative period and discharged within 4-6 h. Two patients in sevoflurane group and four patients in propofol group complained of sore throat. Three patients in sevoflurane group and one patient in propofol group had nausea. No other postoperative complication was reported. None of the patient experienced unpleasant memories or discomfort during anesthesia.
Table 2.
Recovery characteristics
DISCUSSION
The present study investigated the hemodynamic responses and recovery profile of inhalational anesthesia with sevoflurane and intravenous anesthesia with propofol in patients undergoing microlaryngeal surgery. Our results suggest that rapid recovery can be achieved with both the techniques while maintaining intra-operatively a similar degree of hypnosis in both groups. However, sevoflurane provided better intraoperative hemodynamic stability than propofol during microlaryngeal surgery. Mean arterial pressure was better maintained with sevoflurane compared with propofol. Though the difference may be of limited significance for healthy patients, it may be advantageous in elderly patients with coronary artery disease.
Induction with both sevoflurane and propofol was well tolerated by the patients. Though the inhalational induction with sevoflurane was slower (92 s) than intravenous induction with propofol (63 s), this is clinically acceptable. The induction time of sevoflurane varies from 84 to 186 s depending upon the use of concentration of sevoflurane and technique of induction.[14–16] The ability to administer nitrous oxide and up to 8% sevoflurane allowed for a rapid induction in present study. Our induction time with propofol was similar as reported in previous studies.[14,15]
In the present study, heart rate did not differ significantly between the groups but it decreased after induction in both the groups compared with baseline. The mean arterial pressure was more stable in the sevoflurane than propofol group. Induction of anesthesia with propofol was associated with a decrease of approximately 21 mm Hg in mean arterial pressure. In contrast, the decrease in mean arterial pressure with sevoflurane was only 14 mm Hg. Previous investigators also have shown a greater decrease in mean arterial pressure after induction of anesthesia with propofol than with sevoflurane.[14,17,18] Propofol has a direct arterial vasodilator effect, responsible at least in part for the decrease in arterial pressure when it is administered during anesthetic induction. Sevoflurane maintains cardiovascular stability better then propofol even when used in higher concentrations. Husedzinovic et al.,[19] compared the effect of sevoflurane and propofol anesthesia on myocardial contractility using transesophageal echo-Doppler and found that stroke volume was significantly higher in the sevoflurane than in the propofol group (P<0.05) after induction of anesthesia. In older patients and in those with hypertension, the hemodynamic effects of the induction of anesthesia with 8% sevoflurane were found similar to those with propofol 1.2 mg/kg,[20] in contrast to a larger dose of propofol (2.3 mg/kg) in healthy patients. In our study the mean arterial pressure also differed between the groups after insertion of rigid laryngoscope, whereas mean arterial pressure was more in propofol group. Microlaryngoscopy leads to intense adrenergic stimulation resulting in marked fluctuations in blood pressure. Sevoflurane can block the adrenergic reflexes and hemodynamic consequences during surgery. When used with N2 O, 1.5 minimum alveolar anesthetic concentration of sevoflurane can prevent the hemodynamic response to skin incision.[21] Watson et al.,[15] reported significantly higher consumption of alfentanil during intraoperative period in patients receiving total intravenous anesthesia with propofol compared to sevoflurane nitrous oxide group.
The doses of sevoflurane and propofol infusion were titrated according to the bispectral index monitoring for keeping an adequate depth of anesthesia. The use of small, cuffed endotracheal tube instead of jet ventilation permitted the administration of sevoflurane anesthesia without any difficulty during surgical procedure. We used fentanyl instead of remifentanil in our study because fentanyl was found effective in abolishing cardiovascular reactivity to laryngoscopy in microlaryngeal surgery[7] and more cost effective than remifentanil infusion.[22] The incidence of bradycardia and postoperative pain are also high with remifentanil.[12] Our emergence times were equally rapid in both the groups and comparable with previous studies using remifentanil and alfentanil based anesthesia for ear-nose-throat surgery.[8,12] Our incidence of postoperative nausea and vomiting were less in both the groups. This is probably due to the administration of antiemetic premedication to the patients. No other significant adverse effect was reported.
In conclusion, inhalational anesthesia with sevoflurane and intravenous anesthesia with propofol both provided early recovery after microlaryngeal surgery. Sevoflurane showed advantage over propofol in respect of better intraoperative hemodynamic stability. Sevoflurane provides a suitable alternative to propofol for anaesthesia in patients undergoing microlaryngeal surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Strong MS, Vaughan CW, Mahler DL, Jaffe DR, Sullivan RC. Cardiac complications of microsurgery of the larynx: Etiology, incidence and prevention. Laryngoscope. 1974;84:908–20. doi: 10.1288/00005537-197406000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin B. Anesthesia for laryngoscopy. Ann Otol Rhinol Laryngol. 1984;93:338–42. doi: 10.1177/000348948409300411. [DOI] [PubMed] [Google Scholar]
- 3.Ayuso A, Luis M, Sala X, Sanchez J, Trassera J. Effects of anesthetic technique on the hemodynamic response to microlaryngeal surgery. Ann Otol Rhinol Laryngol. 1997;106:863–8. doi: 10.1177/000348949710601010. [DOI] [PubMed] [Google Scholar]
- 4.De Grood PM, Mitsukuri S, Van Egmond J, Rutten JM, Crul JF. Comparison of etomidate and propofol for anesthesia in microlaryngeal surgery. Anaesthesia. 1987;42:366–72. doi: 10.1111/j.1365-2044.1987.tb03976.x. [DOI] [PubMed] [Google Scholar]
- 5.Best N, Traugott F. Comparative evaluation of propofol or methohexitone as the sole anesthetic agent for microlaryngeal surgery. Anaesth Intensive Care. 1991;19:50–6. doi: 10.1177/0310057X9101900109. [DOI] [PubMed] [Google Scholar]
- 6.Bacher A, Pichler K, Aloy A. Supraglottic combined frequency jet ventilation versus subglottic monofrequent jet ventilation in patients undergoing microlaryngeal surgery. Anesth Analg. 2000;90:460–5. doi: 10.1097/00000539-200002000-00041. [DOI] [PubMed] [Google Scholar]
- 7.Ewalenko P, Deloof T, Gerin M, Delmotte JJ, Byttebier G. Propofol infusion with or without fentanyl supplementation for microlaryngoscopy. Acta Anaesthesiol Belg. 1990;41:297–306. [PubMed] [Google Scholar]
- 8.Wuesten R, Van Aken H, Glass PS, Buerkle H. Assessment of depth of anesthesia and postoperative respiratory recovery after remifentanil- versus alfentanil-based total intravenous anesthesia in patients undergoing ear–nose–throat surgery. Anesthesiology. 2001;94:211–7. doi: 10.1097/00000542-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Quezado ZM, Groblewski JC, Gelfand HJ, Shah RK. Dexmedetomidine and propofol in complex microlaryngeal surgery in infants. Int J Pediatr Otorhinolaryngol. 2009;73:1311–2. doi: 10.1016/j.ijporl.2009.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Philip BK, Lombard LL, Roaf ER, Drager LR, Calalang I, Philip JH. Comparison of vital capacity induction with sevoflurane to intravenous induction with propofol for adult ambulatory anesthesia. Anesth Analg. 1999;89:623–7. doi: 10.1097/00000539-199909000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Fish WH, Hobbs AJ, Daniels MV. Comparison of sevoflurane and total intravenous anaesthesia for daycare urological surgery. Anaesthesia. 1999;54:999–1006. doi: 10.1046/j.1365-2044.1999.01005.x. [DOI] [PubMed] [Google Scholar]
- 12.Pandazi AK, Louizos AA, Davilis DJ, Stivaktakis JM, Georgiou LG. Inhalational anesthetic technique in microlaryngeal surgery: A comparison between sevoflurane-remifentanil and sevoflurane-alfentanil anesthesia. Ann Otol Rhinol Laryngol. 2003;112:373–8. doi: 10.1177/000348940311200414. [DOI] [PubMed] [Google Scholar]
- 13.Aldrete JA, Kroulik D. A post anesthetic recovery score. Anesth Analg. 1970;49:924–34. [PubMed] [Google Scholar]
- 14.Thwaites A, Edmends S, Smith I. Inhalation induction with sevoflurane: A double-blind comparison with propofol. Br J Anaesth. 1997;78:356–61. doi: 10.1093/bja/78.4.356. [DOI] [PubMed] [Google Scholar]
- 15.Watson KR, Shah MV. Clinical comparison of single agent anesthesia with sevoflurane versus target controlled infusion of propofol. Br J Anaesth. 2000;85:541–6. doi: 10.1093/bja/85.4.541. [DOI] [PubMed] [Google Scholar]
- 16.Jellish WS, Lien CA, Fontenot HJ, Hall R. The comparative effects of sevoflurane versus propofol in the induction and maintenance of anesthesia in adult patients. Anesth Analg. 1996;82:479–85. doi: 10.1097/00000539-199603000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Gilles Godet G, Watremez C, El Kettani C, Soriano C, Coriat P. A comparison of sevoflurane, target-controlled infusion propofol, and propofol/isoflurane anesthesia in patients undergoing carotid surgery: A quality of anesthesia and recovery profile. Anesth Analg. 2001;93:560–5. doi: 10.1097/00000539-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Smith I, Ding Y, White PF. Comparison of induction, maintenance, and recovery characteristics of sevoflurane-N2O and propofol-sevoflurane-N2O with propofol-isoflurane-N2O anesthesia. Anesth Analg. 1992;74:253–9. doi: 10.1213/00000539-199202000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Husedzinovic I, Tonkovic D, Barisin S, Bradic N, Gasparovic S. Hemodynamic differences in sevoflurane versus propofol anesthesia. Coll Antropol. 2003;27:205–12. [PubMed] [Google Scholar]
- 20.Katoh T, Suguro Y, Ikeda T. Influence of age on awakening concentrations of sevoflurane and isoflurane. Anesth Analg. 1993;76:348–52. [PubMed] [Google Scholar]
- 21.Inada T, Inada K, Kawachi S, Takubo K, Tai M, Yasuqi H. Haemodynamic comparison of sevoflurane and isoflurane anaesthesia in surgical patients. Can J Anaesth. 1999;44:140–5. doi: 10.1007/BF03013001. [DOI] [PubMed] [Google Scholar]
- 22.Loop T, Priebe HJ. Prospective, randomized cost analysis of anesthesia with remifentanil combined with propofol, desflurane or sevoflurane for otorhinolaryngeal surgery. Acta Anaesthesiol Scand. 2002;46:1251–60. doi: 10.1034/j.1399-6576.2002.461013.x. [DOI] [PubMed] [Google Scholar]


