Abstract
Objectives
This study evaluated the antibacterial effect and mechanical properties of composite resins (LCR, MCR, HCR) incorporating chitosan with three different molecular weights (L, Low; M, Medium; H, High).
Materials and Methods
Streptococcus (S). mutans 100 mL and each chitosan powder were inoculated in sterilized 10 mL Brain-Heart Infusion (BHI) solution, and was centrifuged for 12 hr. Absorbance of the supernatent was measured at OD660 to estimate the antibacterial activities of chitosan. After S. mutans was inoculated in the disc shaped chitosan-containing composite resins, the disc was cleansed with BHI and diluted with serial dilution method. S. mutans was spread on Mitis-salivarius bacitracin agar. After then, colony forming unit (CFU) was measured to verify the inhibitory effect on S. mutans biofilm. To ascertain the effect on the mechanical properties of composite resin, 3-point bending and Vickers hardness tests were done after 1 and 3 wk water storage, respectively. Using 2-way analysis of variance (ANOVA) and Scheffe test, statistical analysis was done with 95% significance level.
Results
All chitosan powder showed inhibition effect against S. mutans. CFU number in chitosan-containing composite resins was smaller than that of control resin without chitosan. The chitosan containing composite resins did not show any significant difference in flexural strength and Vickers hardness in comparison with the control resin. However, the composite resin, MCR showed a slightly decreased flexural strength and the maximum load than those of control and the other composite resins HCR and LCR.
Conclusions
LCR and HCR would be recommended as a feasible antibacterial restorative due to its antibacterial nature and mechanical properties.
Keywords: Antibacterial effect, Chitosan, Composite resin, Flexural strength, Vickers hardness
Introduction
Dental plaque is a tooth-associated biofilm consisting of microbial community and a matrix of polymer of bacterial and host origin.1 The bacteria in dental plaque play a primary role in dental caries and induce secondary caries through microleakage between the restoration and the tooth structure. Antibacterial effect of restorative material inactivates bacteria and prevents recurrent caries. The attempt to provide composite resins with antibacterial activity has been made by incorporating an antibacterial agent into the resin component. Adding soluble antibacterial agents into resin matrix is a simple way for the agents of the materials to be well released in wet environment.2 However, the resins containing soluble antibacterial agents show the release pattern, in which a large amount of the agent leached out of mass within a few days and resulted in a dramatic decrease in the concentration.3,4 Another problem for the incorporation of antibacterial agents into the monomer phase is an adverse influence on the mechanical properties.5 Furthermore, the antibacterial agent may have toxic effects and disrupt microbial homeostasis.6
Chitosan (2-amino-2-deoxy-β-D-glucan) is a naturally acquired polysaccharide that is prepared by the deacetylation of chitin, which is mainly obtained from crab and shrimp shells.7 It is classified in three types of chitosan L/M/H (L, Low; M, Medium; H, High) according to their molecular weights. Chitosan is generally regarded as non-toxic, biocompatible, biodegradable and is intrinsically antibacterial in nature.8,9 In dental field, chitosan has been used in studies for the prevention of dental caries as it provides bactericidal and/or bacteriostatic characteristics.9-11 Interaction between positively charged amino groups in chitosan with negatively charged microbial cell surfaces results in the loss of barrier function of microbial cell wall and the leakage of proteinaceous and other intracellular material.10-13 Chitosan has an in vitro antibacterial effect on Streptococcus (S) mutans, Aggregatibacter actinomycetemcomitans, and Porphyromonas gingivalis.8,14,15 It was also reported that low-molecular-weight chitosan prevented the adsorption of S. mutans to hydroxyapatite.16,17 Moreover, chitosan has been suggested as a bioadhesive polymer that provides an extended retention time on the oral mucosa.18
However, the antibacterial activity of chitosan is influenced by a number of factors including the species of bacteria, concentration, pH, solvent and molecular weight.19 Chitosan can only be dissolved when the pH is less than 6.5 in which its antibacterial activity is limited.20 The application of chitosan as a chemical agent for mouthwashes or dentifrices was limited because of its insolubility in water.21 Antibacterial properties and biocompatibility of chitosan are highly desirable in dental materials and chitosan could be maintained inside the materials in the oral cavity because of its insolubility in water. In this study, chitosan with three different molecular weights were incorporated into composite resin for antibacterial activity.
The purpose of this study was to evaluate the antibacterial effect and mechanical properties of composite resin incorporating chitosan with three different L/M/H molecular weights. The hypotheses were that antibacterial activities on S. mutans of the composite resins with three different types of chitosan are not unlike and that addition of chitosan into composite resin does not affect the mechanical properties.
Materials and Methods
Streptococcus Mutans
S. mutans ATCC 25175 was cultured from freeze-dried stocks into 10 mL of sterile triptic soy broth (Difco Laboratories, Detroit, MI, USA) aerobically at 37℃ incubator (Hi-Tec Model 1S-61, Yamato Incubator, Tokyo, Japan) for 24 hours.
Chitosan
According to different molecular weights (L, Low; M, Medium; H, High), Three kinds of chitosan powder (75 - 85% deacetylated, Sigma-Aldrich Co., St. Louis, MO, USA) were used.
1. Antibacterial activities of chitosan powder (L, M, H)
An overnight culture of S. mutans was adjusted to 1 × 106 colony forming unit (CFU)/mL using Petroff-Hauser counting chamber and 100 mL of bacterial culture was inoculated into 10 mL of BHI broth. 0.1 or 0.5 g of chitosan (L, M, H) powder were added in each BHI broth (n = 3). After aerobic incubation at 37℃ for 12 hours, the bacterial suspensions were centrifuged at 1,000 × g for 15 minutes and 300 mL of the supernatant was transferred into the each well of a 96 well plate. The absorbance (OD660) of the supernatant was measured using a spectrophotometer (Milton Roy Spectronic 20D, Milton Roy Company, PA, USA).
2. Inhibitory effect of chitosan-containing composite resin on S. mutans (LCR, MCR, HCR)
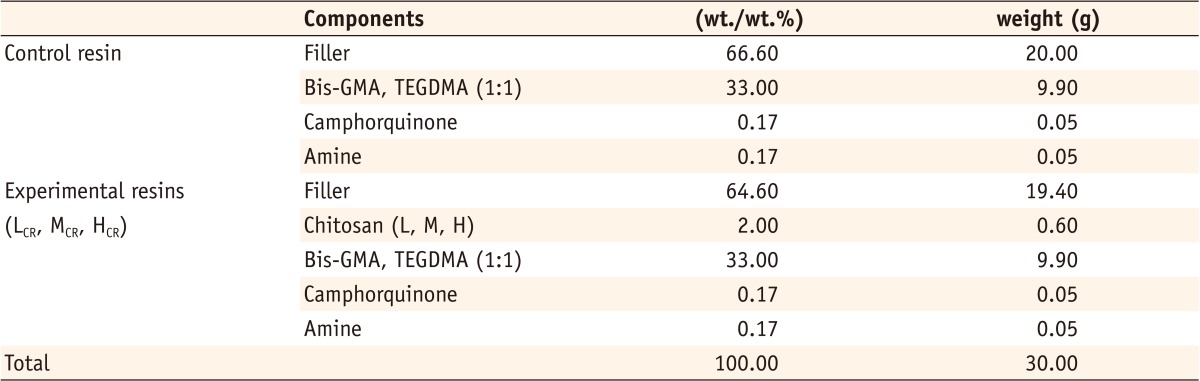
The compositions of experimental resin (LCR, MCR, HCR) and control resin (n = 3) used in this study are listed in Table 1. The powder and liquid of each experimental and control resins were mixed using laboratory mixer system (SpeedMixer, FlackTek Inc, Landrum, SC, USA). The mix was done twice for 10 seconds with 5 zirconia balls so that smooth mixture could be made. Composite resin was put into a teflon mold (10 mm diameter, 2 mm thickness) and was covered with a glass slide (0.15 mm thickness). The specimen was polymerized for 60 seconds using a LED curing unit (Elipar Freelight 2, 3M ESPE, St. Paul, MN, USA) on the top and bottom surfaces. The specimens were removed from the mold, and they were gently polished with 2,000 and 4,000 grit sandpaper sheets. Polished specimens were sterilized in Ethylene Oxide gas.
Table 1.
Compositions of experimental and control resins
The disk was suspended in 3 mL of BHI broth containing 2% sucrose and S. mutans suspensions of approximately 1 × 106 CFU/mL. After anaerobic incubation for 36 hours at 37℃, the disks were washed twice with BHI broth. Each specimen was immersed in 1 mL of BHI broth and was vortex-mixed for 30 seconds to collect the attached S. mutans. The bacterial suspension was transferred to 1.5 mL tube and was vortex mixed with glass bead for 30 seconds. The bacterial suspension was diluted serially from 10 fold to 106 fold by adding BHI broth and 50 mL of the bacterial suspension was spread onto Mitis-salivarius bacitracin agar plate. Plates were incubated anaerobically for 36 hours at 37℃ and the number of total CFU recovered was determined.
3. Mechanical properties of chitosan-containing composite resin (LCR, MCR, HCR)
Two types of teflon molds (2 × 2 × 25 mm for 3-point bending test and cylinders 6 mm in diameter by 4 mm in height for Vickers hardness) were prepared. The experimental or control resin with the same composition described above was put into a teflon mold and the surface was covered with a glass slide. Because of the large size of the specimens (n = 10), both top and bottom surfaces were light cured 5 times for 20 seconds each time, overlapping the previously light cured portion with half the size of the diameter of the light guide of LED curing unit (Elipar Freelight 2, 3M ESPE).
For 3-point bending test, the diameters of both supports and a loading plunger were 2 mm as required by the ISO 4049 standard. Both supports were mounted parallel with their centers being 20 mm away to each other (support span 20 mm). The 3-point bending loads were applied using a Universal testing machine (Instron 3344, Instron, Norwood, MA, USA) with a crosshead speed of 1 mm/minute.
Twenty specimens in each group were prepared for Vickers hardness test and stored at 37℃ in sterile water for 1 or 3 weeks. Half of the specimens of each group were submitted to Vickers hardness test after 1 week storage time and the rest specimens were tested after 3 weeks storage. The Vickers hardness was measured using a microhardness tester (Akashi HM-122, Mithtoyo, Akashi, Japan). In previous calibration, a 300 g load was applied for 15 seconds. Indentations were randomly distributed on the surface of the specimens.
4. Statistical Analyses
The data were analyzed with two-way analysis of variance (ANOVA), followed by Scheffe's multiple comparison test. Statistical analysis was performed using SPSS 13.0 software (SPSS Inc., Chicago, IL, USA). Significance of difference between groups were accepted at 95% level of confidence.
Results
1. Antibacterial activities of chitosan powder
Table 2 shows the absorbance (OD660) of the S. mutans suspensions containing chitosan powder with three different molecular weights (L, M, H). The OD660 of the suspensions containing chitosan powder except 0.1 g chitosan L were significantly lower than that of control group (p < 0.001). Table 3 shows significant differences in the absorbance (OD660) among molecular weights (F = 218.042, p < 0.0001) and the amount (F = 123.772, p < 0.0001) of incorporated chitosan. A significant twoway interaction was also observed between the molecular weight and the amount of incorporated chitosan (F = 32.411, p < 0.0001). The OD660 of the suspension containing chitosan powder significantly decreased as the molecular weight of chitosan increased (p < 0.001). The OD660 of the suspension containing 0.5 g chitosan powder was significantly lower than that of the suspension containing 0.1 g chitosan powder in all groups (p < 0.001).
Table 2.
Bacterial growth (OD660) of 0.1 g and 0.5 g chitosan powder (L, M, H)
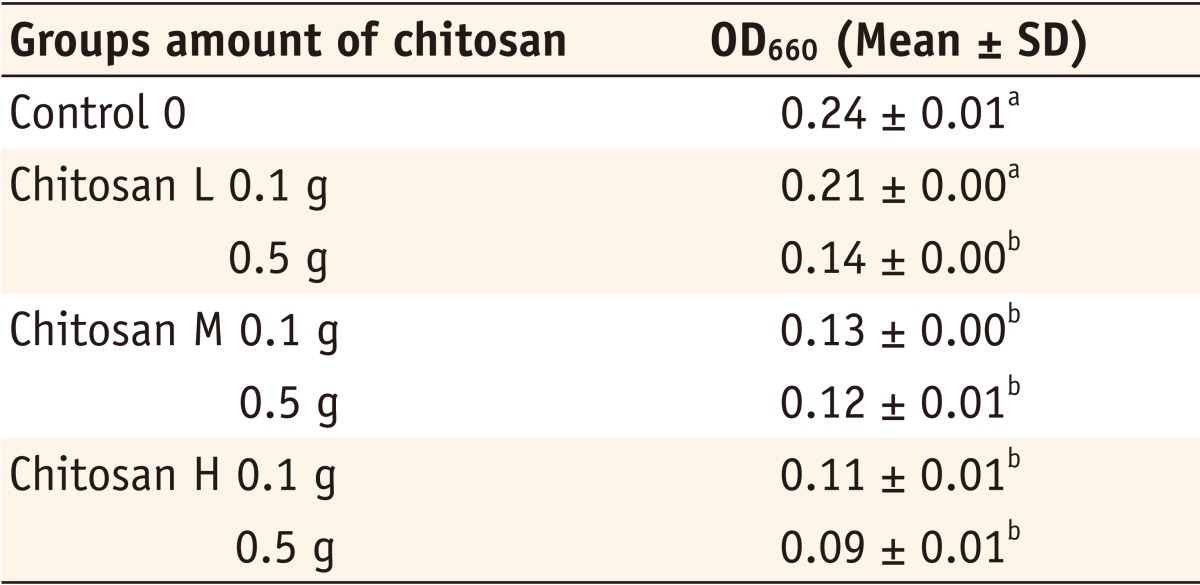
Chitosan L, low molecular weight chitosan powder; Chitosan M, medium molecular weight chitosan powder; Chitosan H, high molecular weight chitosan powder
*The same superscripts represent that there was no statistically significant difference (p > 0.05).
Table 3.
Statistical analysis (two-way ANOVA) of Streptococcus mutans growth explained by two factors of molecular weight and amount of incorporated chitosan
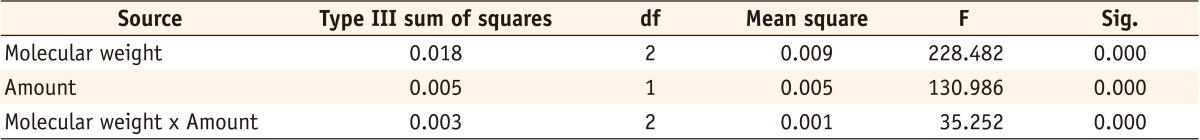
*R Squared = 0.989 (Adjusted R Squared = 0.985)
2. Inhibitory effect of resins incorporating chitosan on S. mutans biofilms
The number of CFU in control resin was significantly larger than that of experimental resins (p < 0.001). However, there was no significant difference among resins incorporating chitosan with three different molecular weights (p > 0.05). Table 4 and Figure 1 show the number and photographs of the colonies formed by S. mutans on the Mitis-salivarius bacitracin agar plate in each group.
Table 4.
The number of the colonies formed by Streptococcus mutans on the Mitis-salivarius bacitracin agar plate in each group
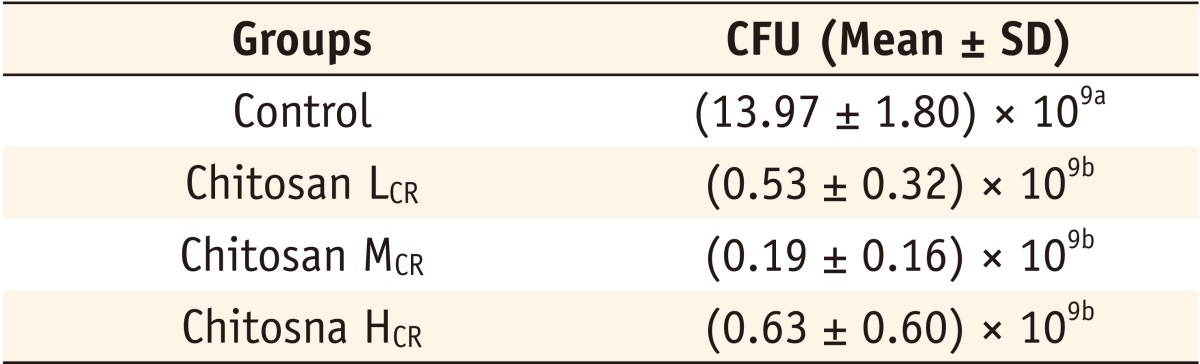
Chitosan LCR, composite resin containing low molecular weight chitosan; Chitosan MCR, composite resin containing medium molecular weight chitosan; Chitosan HCR, composite resin containing high molecular weight chitosan.
*The same superscripts represent that there was no statistically significant difference (p > 0.05).
CFU, colony forming unit.
Figure 1.
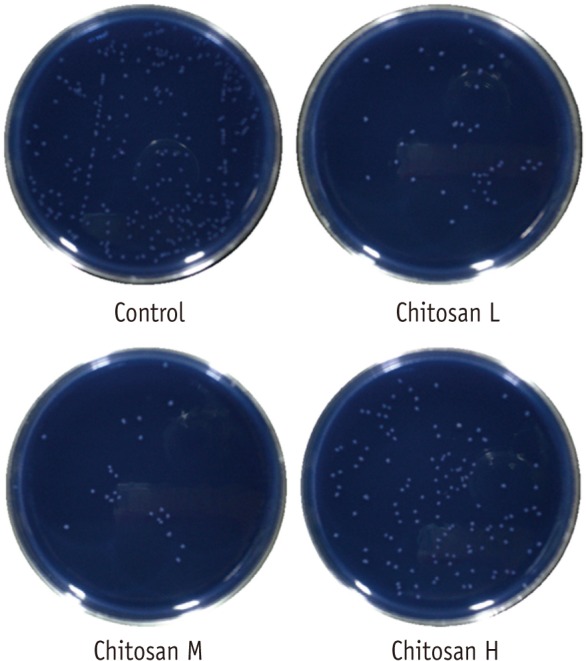
The colonies of Streptococcus mutans on the Mitis-salivarius bacitracin agar plate in each group: control, 106 dilution; Chtosan L, M, and H, 105 dilution.
3. Mechanical properties of resins incorporating chitosan (L, M, H)
Table 5 and 6 show the flexural strength, flexural modulus and the Vickers hardness of control resins and experimental resins incorporating chitosan (L, M, H). There was no significant difference in flexural modulus and Vickers hardness between control resin and experimental resins incorporating chitosan (L, M, H). But, the maximum load and flexural strength of resin (MCR) incorporating chitosan M were significantly lower than those of control resin and resins incorporating chitosan L (LCR) and H (HCR). (p = 0.031, p = 0.032, and p = 0.022, respectively)
Table 5.
Maximum load, flexural strength, flexural modulus of control resin and experimental resins incorporating chitosan
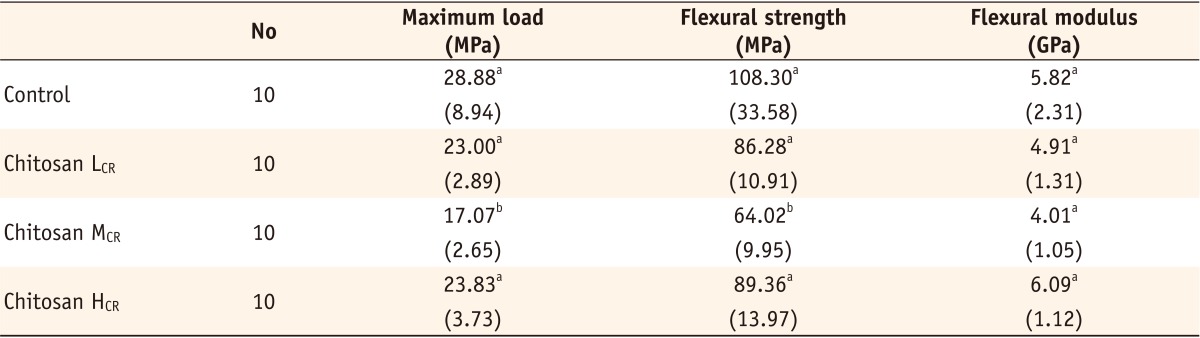
Chitosan LCR, composite resin containing low molecular weight chitosan; Chitosan MCR, composite resin containing medium molecular weight chitosan; Chitosan HCR, composite resin containing high molecular weight chitosan.
The numbers in parentheses were standard deviations.
*The same superscripts in the same column represent that there was no statistically significant difference (p > 0.05).
Table 6.
Vickers hardness (Unit: kgf/cm2; n = 10) of control resin and experimental resins incorporating chitosan (L, M, H) after 1 or 3 weeks
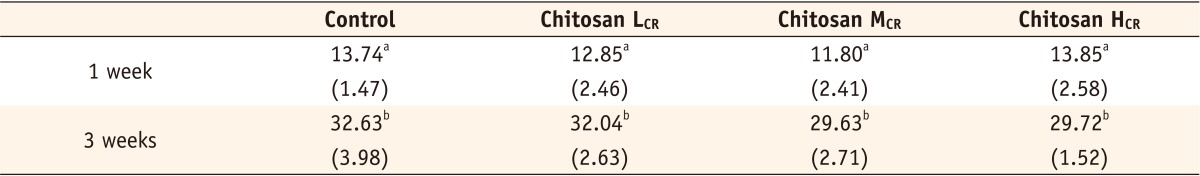
Chitosan LCR, composite resin containing low molecular weight chitosan; Chitosan MCR, composite resin containing medium molecular weight chitosan; Chitosan HCR, composite resin containing high molecular weight chitosan.
The numbers in parentheses were standard deviations.
*The same superscripts in the same column represent that there was no statistically significant difference (p > 0.05)
Discussion
Chitosan is safe and nontoxic in the body and it is capable of promoting regeneration of oral soft tissue and alveolar bone. Chitosan also has bactericidal effect against bacteria and fungi. The mechanism of this bactericidal effect is related with the inactivation of enzyme, substitution of metal ion, lipopolysaccharides, and also the formation of acidic polymer such as teichoic acid which is formed on the cell surface and polyelectrolyte complex. Recently, chitosan is actively being studied in bio-medical field e.g. being applied in the field of drug delivery carrier-heavy metal removing carrier, separation membrane etc.16,17,22,23
There are many kinds of bacteria in the oral cavity. It can be said that the first step for plaque formation is attachment of micro-organisms to tooth, restoration and acquired pellicle covering dental prosthesis.24-27 It is known that hydrophobic property and ionic bond act in these processes. Among these bacteria, S. mutans is known to play a very important role in the formation of plaque and caries. Therefore, S. mutans was chosen for the subject of the experiment on antimicrobial property in this study.
Some papers have reported that composite resins tend to accumulate more bacteria or plaque than other restorative materials in vitro or in vivo.28,29 Therefore, many efforts to reduce the incidence of secondary caries in resin restoration have been made in the dental field. Two typical methods among these efforts are incorporating antibacterial material into the bonding material, and incorporating antibacterial material into the composite. This could be an alternative restorative for the prevention of secondary caries and root caries as well. As an example for the first method, Imazato et al. drew an excellent result by incorporating MDPB (methacryloyloxydodecy lpyridinium bromide) into the self-etching primer and adhesive resin.6 Recently second method is also being studied substantially and several bio-active materials such as MDPB, CHX (chlorhexidine diacetate), Triclosan, silver-containing material (Navaron, Amenitop), cetylpyridium chloride etc. are being introduced. But chitosan is the one which is on the rising interests in the dental field. Chitosan is one of the most abundant substances in nature. It is water insoluble and has a low melting temperature. It is shown that these properties of chitosan would be a great benefit for chitosan to be maintained in the oral cavity for a long period of time unlike CHX which gets released and disappears in early phase.24
In this report, an minimum inhibitory concentration (MIC) method and CFU counting were used to assess the antimicrobial properties of chitosan itself and chitosan containing composite resin. Also, it was said that antimicrobial effects of chitosan varies depending on the degree of de-acetylation and molecular weights in a previous chitosan-related study.30 Therefore, three kinds of chitosans with different molecular weights were used in this study. In the experiment 1, where OD660 against S. mutans was examined, there was a significant anti-microbial effect in the experimental group of chitosan powder. Three kinds of chitosan with different molecular weights were used in this experiment. In the experiment done by Chen et al. it was reported that the heavier the molecular weight and the higher the degree of de-acetylation were, the higher the antimicrobial effect was.31 On the other hand, it was insisted that low molecular weight showed higher effectiveness in the experiment by Tarsi et al.16,17 In this experiment, however, all the three groups showed antimicrobial effect and its effectiveness was excellent with significant difference compared with the control group. In the experiment 2, where CFUs of the experimental groups and the control group were compared, the number of the bacterial colonies of the experimental groups was significantly small irrespective of their molecular weights. This unit shows the degree of bacterial attachment, therefore it can be related to plaque accumulation.
The ability of plaque organisms to attach onto the tooth surfaces or gingival tissues is commonly acknowledged to be a first step in the progression of oral diseases. The nature of this attachment appears to be complex and is ascribed, at least in part, to electrostatic and hydrophobic interactions. The inhibition of the adsorption of the bacteria to the oral tissues could be a promising approach to prevent their colonization and the progression of disease. This goal may be accomplished, to some extent, by either ionic or non-ionic compounds such as alkyl phosphates, poly-L glutamic acid, phytate, surfolane, and non-ionic propoxylated surfactants, which modify the hydroxyapatite surface, thus reducing oral bacterial adsorption.30,32 Tarsi et al. suggested that the mechanism of anti-adherence activity of chitosan involved bacterial surface modifications, alterations in the expression levels of bacterial surface ligands, and chitosan adsorption to host surfaces to change in hydroxyapatite ionic properties.16
In the meantime, Imazato et al. reported that although composite resin showed strong bactericidal activity when MDPB was added, the mechanical properties were not influenced.6 Since there is no study in which the change of the hardness of resin when chitosan was added, the mechanical properties along with antibacterial effect as well was measured in this study. When flexural strength (3-point bending) was measured, no significant change of the mechanical property in 3 kinds of experimental groups was shown compared with the control group. But chitosan M containing composite resin showed significantly lower values in the properties of maximum load and flexural strength than those of experimental group which contained H and control group.
In measuring Vickers hardness as well, 1 and 3 weeks time lag was given for measuring the change of the rigidity. In the result, there was no significant difference between groups and it was the same even when 3 weeks has passed. This means that the rigidity did not decrease with time in the oral cavity. In conclusion, chitosan has antimicrobial effect and does not influence on the rigidity that it can be said that chitosan is an excellent antimicrobial material to be incorporated to resin composite. It can be said that composite resin including chitosan L and H are more recommended than chitosan M. However, the experimental period was short and there also was a lack of studies on molecular weights. As mentioned above, studies on the long term data, color stability and stability during light curing process are necessary.
Conclusions
In this study, chitosan powder groups except 0.1 g chitosan L showed its antibacterial characteristics with the low OD660 value and this value decreased as the molecular weight and the incorporated amount of chitosan increased. Also the composite resins containing chitosan showed smaller CFUs than the one without chitosan irrespective of its molecular weight. Although the chitosan-containing composite resins (LCR, MCR, HCR) did not show any significant difference in flexural modulus and Vickers hardness in comparison with the control composite resin without chitosan, the maximum load and flexural strength of composite resin (MCR) incorporating chitosan M were significantly lower than those of control resin without chitosan and composite resins incorporating chitosan L (LCR) and H (HCR). Overall, composite resins (LCR, HCR) with chitosan L or H would be recommended as an practicable antibacterial restorative when considering its antibacterial nature and mechanical properties.
Footnotes
The current research was conducted by the Research Fund of Dankook University in 2011.
No potential conflict of interest relevant to this article was reported.
References
- 1.Kato K, Fukui K, Nakagaki H, Sato T, Takahashi N. Density profiles of total bacteria and S. mutans within dental plaque treated with stannous fluoride gel. Int Congr Ser. 2005;1284:185–186. [Google Scholar]
- 2.Imazato S. Antibacterial properties of resin composites and dentin bonding systems. Dent Mater. 2003;19:449–457. doi: 10.1016/s0109-5641(02)00102-1. [DOI] [PubMed] [Google Scholar]
- 3.Addy M, Thaw M. In vitro studies into the release of chlorhexidine acetate, prednisolone sodium phosphate, and prednisolone alcohol from cold cure denture base acrylic. J Biomed Mater Res. 1982;16:145–157. doi: 10.1002/jbm.820160207. [DOI] [PubMed] [Google Scholar]
- 4.Wilson SJ, Wilson HJ. The release of chlorhexidine from modified dental acrylic resin. J Oral Rehabil. 1993;20:311–319. doi: 10.1111/j.1365-2842.1993.tb01613.x. [DOI] [PubMed] [Google Scholar]
- 5.Jedrychowski JR, Caputo AA, Kerper S. Antibacterial and mechanical properties of restorative materials combined with chlorhexidines. J Oral Rehabil. 1983;10:373–381. doi: 10.1111/j.1365-2842.1983.tb00133.x. [DOI] [PubMed] [Google Scholar]
- 6.Imazato S, Russell RR, McCabe JF. Antibacterial activity of MDPB polymer incorporated in dental resin. J Dent. 1995;23:177–181. doi: 10.1016/0300-5712(95)93576-n. [DOI] [PubMed] [Google Scholar]
- 7.Uragami T, Yamamoto S, Miyata T. Dehydration from alcohols by polyion complex cross-linked chitosan composite membranes during evapomeation. Biomacromolecules. 2003;4:137–144. doi: 10.1021/bm025642o. [DOI] [PubMed] [Google Scholar]
- 8.Ikinci G, Senel S, Akincibay H, Kaş S, Erciş S, Wilson CG, Hincal AA. Effect of chitosan on a periodontal pathogen Porphyromonas gingivalis. Int J Pharm. 2002;235:121–127. doi: 10.1016/s0378-5173(01)00974-7. [DOI] [PubMed] [Google Scholar]
- 9.Chung YC, Wang HL, Chen YM, Li SL. Effect of abiotic factors on the antibacterial activity of chitosan against waterborne pathogens. Bioresour Technol. 2003;88:179–184. doi: 10.1016/s0960-8524(03)00002-6. [DOI] [PubMed] [Google Scholar]
- 10.Helander IM, Nurmiaho-Lassila EL, Ahvenainen R, Rhoades J, Roller S. Chitosan disrupts the barrier properties of the outer membranes of gram-negative bacteria. Int J Food Microbiol. 2001;71:235–244. doi: 10.1016/s0168-1605(01)00609-2. [DOI] [PubMed] [Google Scholar]
- 11.Rabea EI, Badawy ME, Stevens CV, Smagghe G, Steurbaut W. Chitosan as antimicrobial agent: applications and mode of action. Biomacromolecules. 2003;4:1457–1465. doi: 10.1021/bm034130m. [DOI] [PubMed] [Google Scholar]
- 12.Chung YC, Su YP, Chen CC, Jia G, Wang HL, Wu JC, Lin JG. Relationship between antibacterial activity of chitosan and surface characteristics of cell wall. Acta Pharmacol Sin. 2004;25:932–936. [PubMed] [Google Scholar]
- 13.Decker EM, von Ohle C, Weiger R, Wiech I, Brecx M. A synergistic chlorhexidine/chitosan combination for improved antiplaque strategies. J Periodontal Res. 2005;40:373–377. doi: 10.1111/j.1600-0765.2005.00817.x. [DOI] [PubMed] [Google Scholar]
- 14.Choi BK, Kim KY, Yoo YJ, Oh SJ, Choi JH, Kim CY. In vitro antimicrobial activity of a chitooligosaccharide mixture against Actinobacillus actinomycetemcomitans and Streptococcus mutans. Int J Antimicrob Agents. 2001;18:553–557. doi: 10.1016/s0924-8579(01)00434-4. [DOI] [PubMed] [Google Scholar]
- 15.Fujiwara M, Hayashi Y, Ohara N. Inhibitory effect of water-soluble chitosan on growth of Streptococcus mutans. New Microbiol. 2004;27:83–86. [PubMed] [Google Scholar]
- 16.Tarsi R, Muzzarelli RA, Guzmán CA, Pruzzo C. Inhibition of Streptococcus mutans adsorption to hydroxyapatite by low-molecular-weight chitosans. J Dent Res. 1997;76:665–672. doi: 10.1177/00220345970760020701. [DOI] [PubMed] [Google Scholar]
- 17.Tarsi R, Corbin B, Pruzzo C, Muzzarelli RA. Effect of low-molecular-weight chitosans on the adhesive properties of oral streptococci. Oral Microbiol Immunol. 1998;13:217–224. doi: 10.1111/j.1399-302x.1998.tb00699.x. [DOI] [PubMed] [Google Scholar]
- 18.Miyazaki S, Nakayama A, Oda M, Takada M, Attwood D. Chitosan and sodium alginate based bioadhesive tablets for intraoral drug delivery. Biol Pharm Bull. 1994;17:745–747. doi: 10.1248/bpb.17.745. [DOI] [PubMed] [Google Scholar]
- 19.Hernández-Lauzardo AN, Bautista-Baños S, Velázquezdel Valle MG, Méndez-Montealvo MG, Sánchez-Rivera MM, Bello-Pérez LA. Antifungal effects of chitosan with different molecular weights on in vitro development of Rhizopus stolonifer (Ehrenb.:Fr.) Vuill. Carbohydr Polym. 2008;73:541–547. doi: 10.1016/j.carbpol.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 20.Madihally SV, Matthew HW. Porous chitosan scaffolds for tissue engineering. Biomaterials. 1999;20:1133–1142. doi: 10.1016/s0142-9612(99)00011-3. [DOI] [PubMed] [Google Scholar]
- 21.Bae K, Jun EJ, Lee SM, Paik DI, Kim JB. Effect of water-soluble reduced chitosan on Streptococcus mutans, plaque regrowth and biofilm vitality. Clin Oral Investig. 2006;10:102–107. doi: 10.1007/s00784-006-0038-3. [DOI] [PubMed] [Google Scholar]
- 22.Kaş HS. Chitosan: properties, preparations and application to microparticulate systems. J Microencapsul. 1997;14:689–711. doi: 10.3109/02652049709006820. [DOI] [PubMed] [Google Scholar]
- 23.Sano H, Matsukubo T, Shibasaki K, Itoi H, Takaesu Y. Inhibition of adsorption of oral streptococci to saliva treated hydroxyapatite by chitin derivatives. Bull Tokyo Dent Coll. 1991;32:9–17. [PubMed] [Google Scholar]
- 24.Tanzer JM. Microbiology of dental caries. In: Slots J, Taubman M, editors. Contemporary oral microbiology and immunology. St. Louis: Mosby; 1992. pp. 377–424. [Google Scholar]
- 25.Slots J, Gibbons RJ. Attachment of Bacteroides melaninogenicus subsp. asaccharolyticus to oral surfaces and its possible role in colonization of the mouth and of periodontal pockets. Infect Immun. 1978;19:254–264. doi: 10.1128/iai.19.1.254-264.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wise MD, Dykema RW. The plaque-retaining capacity of four dental materials. J Prosthet Dent. 1975;33:178–190. doi: 10.1016/s0022-3913(75)80108-9. [DOI] [PubMed] [Google Scholar]
- 27.Frank RM, Steuer P. Transmission electron microscopy of plaque accumulations in denture stomatitis. J Prosthet Dent. 1985;53:115–124. doi: 10.1016/0022-3913(85)90079-4. [DOI] [PubMed] [Google Scholar]
- 28.Skjörland KK. Plaque accumulation on different dental filling materials. Scand J Dent Res. 1973;81:538–542. doi: 10.1111/j.1600-0722.1973.tb00362.x. [DOI] [PubMed] [Google Scholar]
- 29.Skjørland KK, Sønju T. Effect of sucrose rinses on bacterial colonization on amalgam and composite. Acta Odontol Scand. 1982;40:193–196. doi: 10.3109/00016358209019811. [DOI] [PubMed] [Google Scholar]
- 30.Sano H, Shibasaki K, Matsukubo T, Takaesu Y. Effect of chitosan rinsing on reduction of dental plaque formation. Bull Tokyo Dent Coll. 2003;44:9–16. doi: 10.2209/tdcpublication.44.9. [DOI] [PubMed] [Google Scholar]
- 31.Chen YM, Chung YC, Wang LW, Chen KT, Li SY. Antibacterial properties of chitosan in waterborne pathogen. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2002;37:1379–1390. doi: 10.1081/ese-120005993. [DOI] [PubMed] [Google Scholar]
- 32.Busscher HJ, Engels E, Dijkstra RJ, van der Mei HC. Influence of a chitosan on oral bacterial adhesion and growth in vitro. Eur J Oral Sci. 2008;116:493–495. doi: 10.1111/j.1600-0722.2008.00568.x. [DOI] [PubMed] [Google Scholar]


