Abstract:
Background:
Intimate partner violence (IPV) is an important health issue. Many medical students and residents have received training relating to IPV, but previous studies show that many students feel that their training has been inadequate. Our objective was to assess the knowledge, attitudes and perceptions about IPV among university medical students and surgical residents.
Methods:
We administered an online survey to a sample of Ontario medical students and surgical residents. The survey instrument was a modified version of the Provider Survey.
Results:
Two hundred medical students and surgical residents participated in the survey (response rate: 29%). Misperceptions about IPV among respondents included the following: 1) victims must get something from the abusive relationships (18.2%), 2) physicians should not interfere with a couple’s conflicts (21%), 3) asking about IPV risks offending patients (45%), 4) Victims choose to be victims (11.1%), 5) it usually takes ‘two to tango’ (18.3%), and 6) some patients’ personalities cause them to be abused (41.1%). The majority of respondents (75.0%) believed identifying IPV was very relevant to clinical practice. The majority of medical students (91.2%) and surgical residents (96.9%) estimated the IPV prevalence in their intended practice to be 10% or less. Most of the medical students (84%) and surgical residents (60%) felt that their level of training on IPV was inadequate and over three quarters of respondents (77.2%) expressed a desire to receive additional education and training on IPV.
Conclusions:
There are misconceptions among Canadian medical students and surgical residents about intimate partner violence. These misconceptions may stem from lack of education and personal discomfort with the issue or from other factors such as gender. Curricula in medical schools and surgical training programs should appropriately emphasize educational opportunities in the area of IPV.
Keywords: Intimate Partner Violence, Violence prevention, Cross-sectional survey, Medical education
Introduction
Intimate partner violence (IPV) is a serious public health concern that is receiving increasing attention in medical research.1The definition includes physical, sexual and/or psychological/ emotional forms of abuse between past or present heterosexual or homosexual partners.2Intimate partner violence occurs across all racial, ethnic, regional, and socioeconomic boundaries.3 Women are more likely than men to be victims of IPV,4 and it is estimated that one in four American women have been victims of IPV in their lifetime.5 Richardson et al. found that only 17% of physical abuse victims have ever had it documented in a general practice medical chart, highlighting the serious problem of underreporting of IPV in healthcare.6
Intimate partner violence victimization has been reported to impact health and lead to increased use of healthcare services.7,8 Intimate partner violence has been linked to mental health disorders such as depression, suicide, and post-traumatic stress disorder.8 In a large multinational study by the World Health Organization (WHO), 24 000 women in 10 countries were interviewed about their experiences and beliefs surrounding IPV.9 The study found that for all settings combined, women who reported physical violence at least once in their lifetime reported significantly more emotional distress, suicidal thoughts, and suicide attempts than non-abused women.7 (Victims of IPV have a 50 to 70% higher chance of having gynecological, central nervous system, and stress-related health problems.10 Bonomi et al. found that currently or recently physically abused women have higher total annual health care costs and use more emergency, hospital outpatient, primary care, pharmacy, and specialty services than non-abused women. Mental health service utilization was found to be higher among women abused both physically and non-physically.10It is evident that the identification and treatment of IPV victims is highly relevant to healthcare, in which physicians have a key role to play.
A national survey of US medical students identified, 91% of senior students as having had training on IPV, but only one third feeling highly confident in having discussions about IPV with patients.11 We conducted a survey with the primary aim of determining medical students’ and surgical residents’ attitudes, beliefs, and perceptions regarding IPV screening, victims, and perpetrators. Secondary aims include examining the level of IPV education/training medical students and surgical residents have received, and exploring how gender and level of education (resident vs. medical student) are related to perceptions of IPV.
Methods
Survey Instrument
Due to the lack of literature on the views and/or knowledge of medical students and surgical residents regarding IPV, we chose to use a modified version of the Provider Survey for our study. The Provider Survey is an instrument intended to measure healthcare providers’ attitudes, beliefs, and self-reported behaviours related to the identification and management of IPV. The Provider Survey is reliable and has been proven valid.12Wording modifications were made to the survey to make the questions applicable to medical students and surgical residents. Two versions of the survey were developed; one for medical students and the other for surgical residents. In addition to the Provider Survey, participants were asked to complete questions on their demographics as well as their current perceptions, knowledge and education on IPV. These questions were modified from ones used in recent IPV surveys of medical students, Canadian Orthopaedic Association members and chiropractors.11,13,14
There were 23 items in the medical student version of the survey, and 30 items in the surgical resident version. The residents’ survey included questions relevant to their current and previous practice. The medical students’ survey did not include these questions due to their lack of clinical practice experience. Questions were primarily either multiple choices or presented as a series of statements with an associated Likert Scale ranging from strongly disagree to strongly agree. Items were grouped into three categories: 1) demographic information, 2) attitudes, knowledge and education, and 3) clinical relevance of IPV.
Sampling Frame
The sampling frame included all medical students and surgical residents currently enrolled at McMaster University, Hamilton, Ontario. We chose to include surgical residents because of our interest in promoting IPV screening in surgical programs. We are unaware of any literature evaluating the attitudes of surgical residents toward IPV. We chose to exclude attending surgeons in our study because the attitudes of attending surgeons have been previously documented.13E-mail lists of McMaster University medical students and surgical residents from all years of study were obtained with permission from McMaster University’s Undergraduate Medical Program Office and contacts in the Department of Surgery Residency Programs. Surveys were not sent to students or residents studying outside of McMaster University.
Survey Administration
We used Survey Monkey, online survey software, to administer the survey and its cover letter in electronic form. We chose Survey Monkey because it is easy to use for both administrators and participants. Following the initial emailing, three rounds of follow-up emails were sent out to the students. Participants were provided with the opportunity to withdraw at any time.
Statistical Analysis
For statistical significance to be reached, 193 trainees were needed for the study sample size. This was based on a population of approximately 700 medical students and surgical trainees at McMaster University, with an error level of 6% and a 95% confidence interval (http://www.custominsight.com/articles/random-sample-calculator.asp).
Survey data were analyzed using PASW version 18.0 (Chicago, IL). Descriptive analyses, including frequency counts and percentages, were performed for all collected data. We conducted Chi-squared tests to determine if there were differences in responses between the surgical residents and medical students using the Contingency Table Calculator.15We also conducted a subgroup analysis looking at differences in responses between males and females using chi-squared tests. Surveys with missing data were included in the analysis.
Results
Response Rate
Two hundred trainees responded (29%), meeting the sample size requirements for this study. The response rate for medical students was 23% (127/542) and 49% (73/150) for surgical residents. No information was available about non-respondents, so we are unable to evaluate differences between those who did and did not participate. The survey was administered in the winter term. The lower medical student response rate may be due to possible interference with exam time. Fifteen medical students and eleven surgical residents started the survey but did not complete it. All data collected from incomplete surveys was used in the analysis. There were no withdrawals from the study.
Respondent Characteristics
Respondents ranged in age from 20 to 45 years (mean age = 26± 4.5 years). The majority of the respondents were female (58.3%), which is approximately representative of the population of medical students and surgical residents at McMaster University, and 5% reported a history of IPV (personal history or family history). The top intended specialties for medical students were family medicine (30.8%) and surgery (12.3%). Over two thirds of the surgical residents were specializing in orthopedics (41.1%) or general surgery (27.1%) (Table 1).
Table 1:Respondent Demographics.
| Demographic | Overall N (%) | Medical Students N (%) | Surgical Residents N (%) |
|---|---|---|---|
| Mean Age ± Standard Deviation | 26.5±4.5 | 24.5±3.2 | 30.2±4.2 |
| Gender | |||
| Male | 82 (41.4%) | 33 (26.2%) | 49 (68.1%) |
| Female | 115 (58.1%) | 92 (73.0%) | 23 (31.9%) |
| Transgender | 1 (0.5%) | 1 (0.8%) | 0 (0%) |
| Year | |||
| 1 | 74 (37.9%) | 56 (44.1%) | 18 (26.5%) |
| 2 | 60 (30.8%) | 47 (37.0%) | 13 (19.1%) |
| 3 | 39 (20.0%) | 24 (18.9%) | 15 (22.1%) |
| 4 | 12 (6.2%) | N/A | 12 (17.6%) |
| 5 | 10 (5.1%) | N/A | 10 (14.7%) |
| Intended Medical Specialty for Medical Students | |||
| Family Medicine | 40 (30.8%) | ||
| Surgery | 16 (12.3%) | ||
| Internal Medicine | 13 (10.0%) | ||
| Obstetrics/Gynecology | 8 (6.2%) | ||
| Pediatrics | 7 (5.4%) | ||
| Psychiatry | 6 (4.6%) | ||
| Emergency Medicine | 6 (4.6%) | ||
| Anesthesiology | 3 (2.3%) | ||
| Neurology | 2 (1.5%) | ||
| Unsure | 14 (10.8%) | ||
| Other | 15 (11.5%) | ||
| Surgical Specialty for Surgical Residents | |||
| Orthopedics | 29 (41.4%) | ||
| General Surgery | 19 (27.1%) | ||
| Plastic Surgery | 7 (10.0%) | ||
| Ophthalmology | 4 (5.7%) | ||
| Urology | 4 (5.7%) | ||
| Neurosurgery | 3 (4.3%) | ||
| Pediatric General Surgery | 2 (2.9%) | ||
| Cardiac Surgery | 1 (1.4%) | ||
| Otolaryngology/Head/Neck Surgery | 1 (1.4%) |
Totals may not add to 200 participants due to missing data.
Misperceptions about IPV
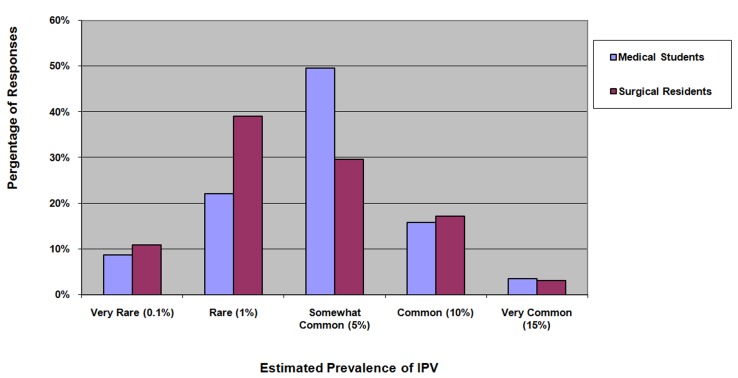
Most respondents (91.2% of medical students and 96.9% of surgical residents) estimated the IPV prevalence in their intended practice to be 10% or less (Figure 1).Respondents held misperceptions about the following issues: 1) victims must get something from the abusive relationships (18.2%), 2) physicians should not interfere with a couple’s conflicts (21%), 3) asking about IPV risk offending patients (45%), 4) victims choose to be victims (11.1%), 5) it usually takes ‘two to tango’ (18.3%), and 6) some patients’ personalities cause them to be abused (41.1%) (Appendix A).
Figure 1: Medical Students' and Surgical Residents' Estimated Prevalence of IPV in their Practice.
Surgical residents were significantly more likely to hold misperceptions about a victim’s role in their abuse (‘it takes two to tango’) compared to medical students (28.2% vs. 12.9%, p=0.038) (Table 2). Males were significantly less likely to disagree with victim-blaming statements than females, such as “People are only victims if they choose to be” (77.8% vs. 96.2% strongly disagree/disagree, p<0.001) and “Women who choose to step out of traditional roles are a major cause of IPV” (75.3% vs. 93.4% strongly disagree/disagree, p=0.001) (Table 3).Many respondents were concerned for their personal safety when asking a patient battering (32.6% strongly agree/agree), and nearly one quarter of respondents fear that they will offend patients if they ask about IPV (22.8% strongly agree/agree) (Table 2).Many respondents has misconceptions about batterers, for example, the abuse would stop if the batterer stopped using alcohol (34.9% agree/strongly agree) (Appendix B).
Table 2:General Knowledge, Personal Comfort and Attitudes.
| Overall N (%) | Medical Students N (%) | Surgical Residents N (%) | P Value* | |
|---|---|---|---|---|
| I am (or would be) afraid of offending the patient if I ask about IPV. | 0.082 | |||
| Strongly agree/ agree | 41 (22.8%) | 32 (27.6%) | 9 (14%) | |
| Neutral | 40 (22.2%) | 22 (19.0%) | 18 (28.1%) | |
| Disagree/Strongly Disagree | 99 (55.0%) | 62 (53.5%) | 37 (57.8%) | |
| I don’t know how to ask about the possibility of IPV. | <0.001** | |||
| Strongly agree/ agree | 50 (27.8%) | 44 (37.6%) | 6 (9.5%) | |
| Neutral | 42 (23.3%) | 25 (21.4%) | 17 (27.0%) | |
| Disagree/Strongly Disagree | 88 (48.9%) | 48 (41%) | 40 (63.4%) | |
| When it comes to domestic violence, it usually “takes two to tango.” | 0.033** | |||
| Strongly agree/ agree | 7 (3.9%) | 3 (2.6%) | 4 (6.3%) | |
| Neutral | 26 (14.4%) | 12 (10.3%) | 14 (21.9%) | |
| Disagree/Strongly Disagree | 148 (81.8%) | 102 (87.2%) | 46 (71.9%) | |
| I am (or would be) reluctant to ask batterers about their abusive behavior out of concern for my personal safety. | 0.497 | |||
| Strongly agree/ agree | 57 (32.6%) | 38 (34.0%) | 19 (30.2%) | |
| Neutral | 42 (24.0%) | 29 (25.9%) | 13 (20.6%) | |
| Disagree/Strongly Disagree | 76 (43.4%) | 45 (40.2%) | 31 (49.2%) | |
| I am (or would be) afraid of offending patients if I ask about their abusive behavior. | 0.012 | |||
| Strongly agree/ agree | 78 (44.6%) | 59 (52.7%) | 19 (30.1%) | |
| Neutral | 37 (21.1%) | 22 (19.6%) | 15 (23.8%) | |
| Disagree/Strongly Disagree | 60 (34.3%) | 31 (27.7%) | 29 (46.1%) | |
| I am afraid that talking to the batterer will increase risk for the victim. | 0.009 | |||
| Strongly agree/ agree | 107 (61.1%) | 78 (69.6%) | 29 (46.1%) | |
| Neutral | 44 (25.1%) | 22 (19.6%) | 22 (34.9%) | |
| Disagree/Strongly Disagree | 24 (13.7%) | 12 (10.7%) | 12 (19.1%) | |
| I feel I can effectively discuss issues of battering and abuse with a battering patient. | 0.016 | |||
| Strongly agree/ agree | 19 (10.9%) | 10 (8.9%) | 9 (14.3%) | |
| Neutral | 48 (27.4%) | 24 (21.4%) | 24 (38.1%) | |
| Disagree/Strongly Disagree | 108 (61.7%) | 78 (69.7%) | 30 (47.6%) | |
| Time constraints | 0.004 | |||
| Strongly agree/ agree | 160 (82.9%) | 111 (89.5%) | 49 (71.0%) | |
| Neutral | 16 (8.3%) | 7 (5.6%) | 9 (13.0%) | |
| Disagree/Strongly Disagree | 17 (8.8%) | 6 (4.8%) | 11 (15.9%) | |
| Lack of knowledge of what to ask | 0.010 | |||
| Strongly agree/ agree | 129 (66.8%) | 91 (73.4%) | 38 (55.1%) | |
| Neutral | 29 (15.0%) | 18 (14.5%) | 11 (15.9%) | |
| Disagree/Strongly Disagree | 35 (18.1%) | 15 (12.1%) | 20 (28.9%) | |
| Lack of knowledge of what to do if patient says “yes” to inquiry | <0.001 | |||
| Strongly agree/ agree | 121 (62.7%) | 90 (72.5%) | 31 (44.9%) | |
| Neutral | 26 (13.5%) | 17 (13.7%) | 9 (13%) | |
| Disagree/Strongly Disagree | 46 (23.8%) | 17 (13.7%) | 29 (42%) | |
| Personal discomfort with the issue | 0.003 | |||
| Strongly agree/ agree | 102 (52.8%) | 77 (62.1%) | 25 (36.2%) | |
| Neutral | 37 (19.2%) | 19 (15.3%) | 18 (26.1%) | |
| Disagree/Strongly Disagree | 54 (28.0%) | 28 (22.6%) | 26 (37.6%) | |
| Lack of knowledge of community resources | 0.754 | |||
| Strongly agree/ agree | 135 (69.9%) | 88 (71.0%) | 47 (68.1%) | |
| Neutral | 32 (16.6%) | 21 (16.9%) | 11 (15.9%) | |
| Disagree/Strongly Disagree | 26 (13.5%) | 15 (12.1%) | 11 (15.9%) |
* Chi-Squared test
** Fisher’s exact test (Has an expected value of less than 5).
Totals may not add to 200 participants due to missing data.
Table 3:Responses of Male versus Female Respondents.
| Question | Males N (%) | Females N (%) | P Value* |
|---|---|---|---|
| History of IPV | 2 (2.4%) | 8 (7.0%) | |
| Personal | 0 (0%) | 5 (62.5%) | |
| Family | 2 (100%) | 3 (37.5%) | |
| Amount of IPV training/education received | 0.045 | ||
| None | 28 (34.6%) | 54 (49.1%) | |
| Any | 53 (65.4%) | 56 (50.9%) | |
| It is demeaning to patients to question them about abuse. | 0.051** | ||
| Strongly agree/ agree | 3 (4.2%) | 2 (1.9%) | |
| Neutral | 15 (20.5%) | 10 (9.4%) | |
| Disagree/Strongly Disagree | 54 (75.0%) | 94 (88.7%) | |
| People are only victims if they choose to be. | <0.001** | ||
| Strongly agree/ agree | 6 (8.3%) | 0 (0%) | |
| Neutral | 10 (13.9%) | 4 (3.8%) | |
| Disagree/Strongly Disagree | 56 (77.8%) | 102 (96.2%) | |
| Women who choose to step out of traditional roles are a major cause of IPV. | <0.001** | ||
| Strongly agree/ agree | 3 (4.2%) | 0 (0%) | |
| Neutral | 15 (20.5%) | 7 (6.6%) | |
| Disagree/Strongly Disagree | 54 (75.3%) | 99 (93.4%) |
* Chi-Squared test
**Has an expected value of less than 5
Totals may not add to 200 participants due to missing data.
Barriers to Assessment of IPV
Key barriers to IPV assessment perceived by respondents included lack of time (82.9%), lack of knowledge of what to ask (66.8%), lack of knowledge of community resources (69.9%), and personal discomfort (52.8%) (Table 2). Medical students were significantly more likely to have issues with lack of time (89.5% vs. 71.0%, p=0.004), lack of knowledge of what to say (73.4% vs. 55.1%, p=0.010), lack of knowledge of what to do if a patient is abused (72.5% vs. 44.9%, p<0.001), and personal discomfort (62.1% vs. 36.2%, p=0.003) when compared to surgical residents (Table 2).42% of respondents reported that the main barrier to screening for IPV is a lack of training (Appendix C).
Need for Education and Training
Most respondents identified IPV identification as relevant in their practice (89%) but many were unsure or incorrect about legal reporting requirements (20.0% unsure, 12.1% incorrect) (Table 4). Almost all respondents had little or no previous IPV training (99%), yet only 75% believed their education was inadequate. Most trainees supported additional training and educational initiatives in IPV (77.2%), and 42% cited their lack of education and training as the primary barrier to routine assessment (Table 4). Medical students were significantly more likely to report a lack of training (83.9% vs. 60.3%, p=0.001) and desire for increased IPV education (87.9% vs. 58.0%, p=0.062).
Table 4:Relevance and Education.
| Overall N (%) | Medical Students N (%) | Surgical Residents N (%) | P Value* | ||
|---|---|---|---|---|---|
| Relevance of identifying IPV victims in practice | Not at all relevant | 2 (1.0%) | 1 (0.8%) | 1 (1.5%) | NA |
| Possibly relevant | 15 (7.8%) | 11 (8.9%) | 4 (5.9%) | ||
| Somewhat relevant | 27 (14.0%) | 18 (14.5%) | 9 (13.2%) | ||
| Very relevant | 144 (75.0%) | 94 (75.8%) | 50 (73.5%) | ||
| Depends on Specialty | 4 (2.1%) | ----*** | 4 (5.9%) | ||
| Level of comfort asking a woman about abuse | Very uncomfortable | 4 (2.1%) | 1 (0.8%) | 3 (4.3%) | 0.023** |
| Uncomfortable | 31 (16.1%) | 24 (19.4%) | 7 (10.1%) | ||
| Somewhat comfortable | 91 (47.2%) | 64 (51.6%) | 27(39.1%) | ||
| Comfortable | 57 (29.5%) | 29 (23.4%) | 28 (40.6%) | ||
| Very comfortable | 10 (5.2%) | 6 (4.8%) | 4 (5.8%) | ||
| Is health care provider reporting of intimate partner violence mandatory in Canada? | Yes | 23 (12.1%) | 16 (12.9%) | 7 (10.6%) | 0.877 |
| No | 129 (67.9%) | 84 (67.7%) | 45 (68.2%) | ||
| Unsure | 38 (20.0%) | 24 (19.4%) | 14 (21.2%) | ||
| Amount of IPV education/training received | None | 83 (43.0%) | 66 (53.2%) | 17 (24.6%) | <0.001** |
| Some | 108 (56.0%) | 56 (45.2%) | 52 (75.4%) | ||
| Extensive | 2 (1.0%) | 2 (1.6%) | 0 (0.0%) | ||
| Adequate amount of IPV training received thus far | Yes | 21 (10.9%) | 8 (6.5%) | 13 (19.1%) | 0.001 |
| No | 145 (75.5%) | 104 (83.9%) | 41 (60.3%) | ||
| Unsure | 26 (13.5%) | 12 (9.7%) | 14 (20.6%) | ||
| Desire for additional training on the assessment and treatment of IPV | Yes | 149 (77.2%) | 109 (87.9%) | 40 (58.0%) | <0.001** |
| No | 16 (8.3%) | 4 (3.2%) | 12 (17.4%) | ||
| Unsure | 22 (11.4%) | 7 (5.6%) | 15 (21.7%) | ||
| Not relevant to my intended practice | 6 (3.1%) | 4 (3.2%) | 2 (2.9%) | ||
| Providing medical students with more education/training on intimate partner violence would help increase the number of physicians that screen for it | Strongly agree | 47 (24.4%) 110 | 28 (22.6%) | 19 (27.5%) | 0.032** |
| Agree | (57.0%) | 79 (63.7%) | 31 (44.9%) | ||
| Unsure | 26 (13.5%) | 11 (8.9%) | 15 (21.7%) | ||
| Disagree | 10 (5.2%) | 6 (4.8%) | 4 (5.8%) | ||
| Strongly Disagree | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
* Chi-Squared test
** Has an expected value of less than 5
Totals may not add to 200 participants due to missing data.
Clinical Assessment of IPV
When considering the last few months of clinical practice, trainees reported seldom or rarely asking patients about IPV with injuries (66.1%), pelvic pain (33.8%), irritable bowel syndrome (45.1%), headaches (46.8%), depression/anxiety (33.9%), or high blood pressure (59%) (Appendix D).
Many surgical residents (48.4%) reported that they had identified a victim of IPV and 27.4% of residents reported that they had identified a batterer. Only 9.7% of surgical residents reported that their clinical setting has guidelines for detecting and managing IPV, and over one quarter (25.8%) were unsure if there are guidelines in their clinical setting (Appendix D).
Discussion
In this survey of 200 Canadian medical students and surgical residents, our findings suggest that medical students and surgical residents have multiple misperceptions about IPV and have not received adequate training on the identification and treatment of IPV. Most respondents underestimated the IPV prevalence in their intended practice. Despite having misconceptions about IPV and underestimating its prevalence, the majority of respondents believed identifying IPV was very relevant to clinical practice. In addition, most of the respondents acknowledged that their level of training on IPV was inadequate and over three quarters of respondents would like to receive additional education and training on IPV.
Medical student and surgical trainees incorrectly believed that the prevalence of IPV is 10% or less. These results are similar to the findings of two previous surveys of health care practitioners. In a recent survey of orthopaedic surgeons, most respondents indicated that the prevalence of IPV in their practice was rare (<1%).13 In a similar study of Ontario chiropractors, the majority of respondents indicated that the prevalence of IPV in their practice was between 0.1% and 1%.14 In contrast to the survey findings, multiple prevalence studies have shown that the lifetime prevalence of IPV is much higher. For example, several American, Australian, and Canadian studies have found that IPV prevalence is well over 10% in both emergency medicine16-20 and family medicine.21-25 In addition, the PRAISE Investigators26 recently found that the 12 month prevalence of IPV in orthopaedic fracture clinics, one of the most common specialties among our respondents, was over 30%.
Almost half of the respondents held the misconception that patients would be offended if they were asked about IPV. This finding is similar to a survey of Ontario chiropractors, which shows that almost half of chiropractors were afraid of offending patients when asking about IPV.14 This finding contradicts other research by Hurley et al.27 who found that 86% of men and women presenting to Canadian emergency departments agreed that health care providers should screen for IPV. Similarly, Caralis et al.28 established that the majority of American survey respondents believe doctors should screen for abuse in their practices. In addition, Feder et al.29 conducted a meta-analysis that showed women who have been abused support screening programs for IPV in a health care setting. Dispelling the misconception that women do not wish to be screened for IPV and providing additional education on IPV could help ensure additional screening for IPV among future health care practitioners.
Education in IPV was valued among respondents; however, most reported feeling that they have received an inadequate level of education and training on IPV and have a desire to receive additional training on the assessment and treatment of IPV. Both of these results were higher for medical students, which we speculate is attributed to their shorter time in the medical curriculum. These results are similar to a survey of American medical students that concluded that despite national interest in IPV issues, efforts in U.S. medical schools to increase IPV screening and prevention have not achieved saturation.11 Similarly, a recent report from the Association of American Medical Colleges found that 20% of U.S. graduating physicians in 2004 believed that the curriculum time dedicated to IPV was inadequate.30 Hamberger31 has suggested that, although most medical schools educate students on IPV in some form, the teaching is mainly done in a basic science module as opposed to in a clinical setting. Edwardsen et al.32 have showed that a structured IPV training program with use of mnemonics and clinical role-playing can help medical students to ask their patients questions about their history of IPV. In addition, Chapin et al. revealed that emergency medical personnel who received IPV training from a domestic violence center were better informed about IPV services and the obstacles faced by victims.33 One clinic-based IPV education program for pediatric residents has increased IPV screening from less than 1% to over 30% 8 months after program completion.34 We suggest that IPV education be included in both medical and residency training and that it should focus on clinic-based practical exercises.
Nearly one third of respondents were either incorrect or unsure when asked if health care provider reporting of IPV is mandatory in Canada. Reporting of IPV is not mandatory in Canada,34 but it is mandatory in some American states.35 Most surgical residents reported screening for IPV only seldom or never, which is consistent with the findings of a recent survey of orthopaedic surgeons13 and of U.S. medical residents.11 In addition, it was very uncommon for surgical residents to screen patients with illnesses linked to IPV such as hypertension/ coronary artery disease, irritable bowel syndrome, or headaches, indicating a need for additional education on the identification and screening of IPV. The survey found that residents were more likely to screen patients with injuries for IPV. This is consistent with a study of U.S. residents36 and of primary care physicians.37
Medical students were more likely to report that they felt time constraints, lack of knowledge, and personal discomfort compared to residents. Residents may have had more opportunities to come across abused women due to increased time in clinical settings compared to medical students. Perhaps some of the residents’ knowledge comes not from formal academic training, as in medical school, but from experiential learning in a clinical setting.
In previous studies, IPV training has been proven successful in raising awareness as well as improving the ability of healthcare professionals to detect IPV. Warburton et al.38 reported that a brief IPV educational program improved dental hospital staff’s attitudes and knowledge about IPV. As well, an educational program for internal medicine residents was both well received and effective at improving detection of IPV victims.39 Three key questions aimed at raising suspicion of IPV were included in a questionnaire; 54% of the intervention group were able to answer at least two out of three questions correctly compared to 20% of the control group.39
This study has provided valuable insight into the knowledge, education, attitudes and perceptions of medical students and surgical residents regarding the topic of IPV. One of the strengths of the study is the survey instrument, which was created by domestic violence experts and validated in IPV surveys of health care providers. It has met basic face and basic content validity, although we did use a slightly modified version of the Provider Survey for students and residents which have not been validated. The survey also had an adequate sample size. However, the study also had some limitations. Our survey had a relatively low response rate, which may be a potential source of bias. It is possible that responders differed in some characteristics compared to non-responders. For example, non-responders could be more likely than responders to have experienced IPV, which would influence many of the results. Our survey was restricted to only medical students and surgical residents from McMaster University who could be contacted via email. It remains unclear whether our findings are generalizable to other universities and jurisdictions. This study was a descriptive, cross-sectional study that can only be used to identify perceptions and barriers regarding IPV inquiry. Causal inferences about specific variables and outcomes cannot be made.
Conclusion
Misconceptions exist among one Canadian medical school’s medical students and surgical residents about IPV and may be related to lack of education and low self-efficacy, or possibly to other factors such as gender. Curricula in medical schools and surgical training programs should appropriately emphasize educational opportunities in the area of IPV. Future research should explore the most optimal methods of disseminating IPV information among students and health care providers in order to increase awareness of IPV and reduce these misconceptions. It is anticipated that increased awareness of IPV among health care providers will motivate them to seek additional IPV knowledge and training, and ultimately increase screening and care of patients experiencing IPV in their practice.
Footnotes
Funding:No funding was received for the completion of this manuscript. Dr. Mohit Bhandari is funded in part by a Canada Research Chair.
Competing interests:None declared
Ethical approval:We received ethical approval from McMaster University /Hamilton Health Sciences Research Ethics Board (#09-497).
References
- 1.McClennan S, Worster A, MacMillan H. Caring for victims of intimate partner violence: a survey of Canadian emergency departments. CJEM. 2008 Jul;10(4):325–8. doi: 10.1017/s1481803500010290. [DOI] [PubMed] [Google Scholar]
- 2.Zolotor AJ, Denham AC, Weil A. Intimate partner violence. Prim Care. 2009 Mar;36(1):167–79. doi: 10.1016/j.pop.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Gunter J. Intimate partner violence. Obstet Gynecol Clin North Am. 2007 Sep;34(3):367–88. doi: 10.1016/j.ogc.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Roberts GL, O'Toole BI, Raphael B, Lawrence JM, Ashby R. Prevalence study of domestic violence victims in an emergency department. Ann Emerg Med. 1996 Jun;27(6):741–53. doi: 10.1016/s0196-0644(96)70194-4. [DOI] [PubMed] [Google Scholar]
- 5. Tjaden P, Thoennes P. Extent, nature, and consequences of intimate partner violence: findings from the National Violence Against Women Survey. Washington (DC): Department of Justice (US), 2000. [Google Scholar]
- 6.Richardson J, Coid J, Petruckevitch A, Chung WS, Moorey S, Feder G. Identifying domestic violence: cross sectional study in primary care. BMJ. 2002 Feb 2;324(7332):274. doi: 10.1136/bmj.324.7332.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonomi AE, Anderson ML, Rivara FP, Thompson RS. Health care utilization and costs associated with physical and nonphysical-only intimate partner violence. Health Serv Res. 2009 Jun;44(3):1052–67. doi: 10.1111/j.1475-6773.2009.00955.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Golding JM. Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J FamViolence. 1999;14(2):99–132. [Google Scholar]
- 9.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. WHO Multi-country Study on Women's Health and Domestic Violence against Women StudyTeam. Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet. 2008 Apr 5;371(9619):1165–72. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- 10.Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O'Campo P, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002 May 27;162(10):1157–63. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- 11.Frank E, Elon L, Saltzman LE, Houry D, McMahon P, Doyle J. Clinical and personal intimate partner violence training experiences of U.S.medical students. J Womens Health(larchmt) 2006 Nov;15(9):1071–9. doi: 10.1089/jwh.2006.15.1071. [DOI] [PubMed] [Google Scholar]
- 12.Maiuro RD, Vitaliano PP, Sugg NK, Thompson DC, Rivara FP, Thompson RS. Development of a health care provider survey for domestic violence: psychometric properties. Am J Prev Med. 2000 Nov;19(4):245–52. doi: 10.1016/s0749-3797(00)00230-0. [DOI] [PubMed] [Google Scholar]
- 13.Bhandari M, Sprague S, Tornetta P, D'Aurora V, Schemitsch E, Shearer H, et al. (Mis)perceptions about intimate partner violence in women presenting for orthopaedic care: a survey of Canadian orthopaedic surgeons. J Bone and Joint Surg Am. 2008 Jul;90(7):1590–7. doi: 10.2106/JBJS.G.01188. [DOI] [PubMed] [Google Scholar]
- 14.Shearer HM, Forte ML, Dosanjh S, Mathews DJ, Bhandari M. Chiropractors' perceptions about intimate partner violence: a Cross-Sectional Survey. J Manipulative Physiol Ther. 2006 Jun;29(5):386–92. doi: 10.1016/j.jmpt.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 15. Kirkman TW. Statistics to Use.1996, http://www.physics.csbsju.edu/stats/, accesses 10 August 2010. [Google Scholar]
- 16.Abbott J, Johnson R, Koziol-McLain J, Lowenstein SR. Domestic violence against women. Incidence and prevalence in an emergency department population. JAMA. 1995 Jun 14;273(22):1763–7. doi: 10.1001/jama.273.22.1763. [DOI] [PubMed] [Google Scholar]
- 17.Cox J, Bota GW, Carter M, Bretzlaff-Michaud JA, Sahai V, Rowe BH. Domestic violence. Incidence and prevalence in a northern emergency department. Can Fam Physician. 2004 Jan;50:90–7. [PMC free article] [PubMed] [Google Scholar]
- 18.El-Bassel N, Gilbert L, Wu E, Chang M, Gomes C, Vincour D, et al. Intimate partner violence prevalence and HIV risks among women receiving care in emergency departments: implications for IPV and HIV screening. Emerg Med J. 2007 Apr;24(4):255–9. doi: 10.1136/emj.2006.041541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McLaughlin SA, Crandall CS, Fullerton L, Brokaw J, Olson LM, Sklar DP. Comparison of intimate partner violence reporting between an emergency department and a clinic setting. Acad Emerg Med. 1999 Dec;6(12):1292–5. doi: 10.1111/j.1553-2712.1999.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 20.Roche M, Moracco KE, Dixon KS, Stern EA, Bowling JM. Correlates of intimate partner violence among female patients at a North Carolina emergency department. N C Med J. 2007 Mar;68(2):89–94. [PubMed] [Google Scholar]
- 21.Elliott BA, Johnson MM. Domestic violence in a primary care setting. patterns and prevalence. Arch Fam Med. 1995 Feb;4(2):113–9. doi: 10.1001/archfami.4.2.113. [DOI] [PubMed] [Google Scholar]
- 22.Hegarty KL, Bush R. Prevalence and associations of partner abuse in women attending general practice: a cross-sectional survey. Aust N Z J Public Health. 2002 Oct;26(5):437–42. doi: 10.1111/j.1467-842x.2002.tb00344.x. [DOI] [PubMed] [Google Scholar]
- 23.Johnson M, Elliott BA. Domestic violence among family practice patients in midsized and rural communities. J Fam Pract. 1997 Apr;44(4):391–400. [PubMed] [Google Scholar]
- 24.Ruiz-Perez I, Plazaola-Castano J, Alvarez-Kindelan M, Palomo-Pinto M, Arnalte-Barrera M, Bonet-Pla A, et al. Sociodemographic associations of physical, emotional, and sexual intimate partner violence in spanish women. Ann Epidemiol. 2006 May;16(5):357–63. doi: 10.1016/j.annepidem.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Wagner PJ, Mongan P, Hamrick D, Hendrick LK. Experience of abuse in primary care patients. Racial and rural differences. Arch Fam Med. 1995 Nov;4(11):956–62. doi: 10.1001/archfami.4.11.956. [DOI] [PubMed] [Google Scholar]
- 26.Bhandari M, Sprague S, Dosanjh S, Petrisor B, Resendes S, Madden K, et al. The prevalence of intimate partner violence across orthopaedic fracture clinics in ontario. J Bone Joint Surg Am. 2011 Jan 19;93(2):132–41. doi: 10.2106/JBJS.I.01713. [DOI] [PubMed] [Google Scholar]
- 27.Hurley KF, Brown-Maher T, Campbell SG, Wallace T, Venugopal R, Baggs D. Emergency department patients' opinions of screening for intimate partner violence among women. Emerg Med J. 2005 Feb;22(2):97–8. doi: 10.1136/emj.2002.002626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Caralis PV, Musialowski R. Women’s experiences with domestic violence and their attitudes and expectations regarding medical care of abuse victims. South Med J. 1997 Nov;90(11):1075–80. doi: 10.1097/00007611-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Feder GS, Hutson M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med. 2006 Jan 9;166(1):22–37. doi: 10.1001/archinte.166.1.22. [DOI] [PubMed] [Google Scholar]
- 30. Medical school questionnaire. All school report. Association of American Medical Colleges, www.aamc.org/data/gq/allschoolsreports/2004.pdf, accessed 30 September 2010. [Google Scholar]
- 31.Hamberger LK. Preparing the next generation of physicians: medical school and residency-based intimate partner violence curriculum and evaluation. Trauma Violence Abuse. 2007 Apr;8(2):214–25. doi: 10.1177/1524838007301163. [DOI] [PubMed] [Google Scholar]
- 32.Edwardsen EA, Morse DS, Frankel RM. Structured practice opportunities with a mnemonic affect medical student interviewing skills for intimate partner violence. Teach Learn Med. 2006 Feb;18(1):62–8. doi: 10.1207/s15328015tlm1801_13. [DOI] [PubMed] [Google Scholar]
- 33.Chapin JR, Coleman G, Varner E. Yes we can! Improving medical screening for intimate partner violence through self-efficacy. J Inj Violence Res. 2011 Jan;3(1):19–23. doi: 10.5249/jivr.v3i1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McColgan MD, Cruz M, McKee J, Dempsey SH, Davis MB, Barry P, et al. Results of a multifaceted Intimate Partner Violence training program for pediatric residents. Child Abuse Negl. 2010 Apr;34(4):275–83. doi: 10.1016/j.chiabu.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 35.Rodriguez MA, McLoughlin E, Nah G, Campbell JC. Mandatory reporting of domestic violence injuries to the police:what do emergency department patients think? JAMA. 2001 Aug 1;286(5):580–3. doi: 10.1001/jama.286.5.580. [DOI] [PubMed] [Google Scholar]
- 36. Jonassen JA, Mazor KM.Identification of physician and patient attributes that influence the likelihood of screening for intimate partner violence. Acad Med. 2003 Oct;78(10 Suppl):S20-3. [DOI] [PubMed] [Google Scholar]
- 37.Rodriguez MA, Bauer HM, McLoughlin E, Grumbach K. Screening and intervention for intimate partner abuse: practices and attitudes of primary care physicians. JAMA. 1999 Aug 4;282(5):468–74. doi: 10.1001/jama.282.5.468. [DOI] [PubMed] [Google Scholar]
- 38.Warburton AL, Hanif B, Roswell C, Coulthard P. Changes in the levels of knowledge and attitudes of dental hospital staff about domestic violence following attendance at an awareness raising seminar. Br Dent J. 2006 Nov 25;201(10):653–9. doi: 10.1038/sj.bdj.4814232. [DOI] [PubMed] [Google Scholar]
- 39.Korenstein D, Thomas DC, Foldes C, Ross J, Halm E, McGinn T. An evidence-based domestic violence education program for internal medicine residents. Teach Learn Med. 2003 Oct;15(4):262–6. doi: 10.1207/S15328015TLM1504_09. [DOI] [PubMed] [Google Scholar]