Abstract:
Background:
Brain injuries are a significant public health problem, particularly among the pediatric population. Brain injuries account for a significant portion of pediatric injury deaths, and are the highest contributor to morbidity and mortality in the pediatric and young adult populations. Several studies focus on particular mechanisms of brain injury and the cost of treating brain injuries, but few studies exist in the literature examining the highest contributing mechanisms to pediatric brain injury and the billed charges associated with them.
Methods:
Data were extracted from the Pediatric Health Information System (PHIS) from member hospitals on all patients admitted with diagnosed head injuries and comparisons were made between ICU and non-ICU admissions. Collected data included demographic information, injury information, total billed charges, and patient outcome.
Results:
Motor vehicle collisions, falls, and assaults/abuse are the three highest contributors to brain injury in terms of total numbers and total billed charges. These three mechanisms of injury account for almost $1 billion in total charges across the five-year period, and account for almost half of the total charges in this dataset over that time period.
Conclusions:
Research focusing on brain injury should be tailored to the areas of the most pressing need and the highest contributing factors. While this study is focused on a select number of pediatric hospitals located throughout the country, it identifies significant contributors to head injuries, and the costs associated with treating them.
Keywords: Brain injury, Causes, Cost, Children
Introduction
Unintentional injuries are the fourth leading cause of death for all age groups,1,2 and the leading cause of death for individuals under the age of 19.1 Moreover, head and brain injuries account for approximately one-third of all injury deaths across all age groups,4,5 and are the most common cause of morbidity and mortality in children,6-8 representing almost ninety percent of all pediatric injury deaths.9
Brain injuries vary in severity and are generally measured on the Glasgow Coma Scale (GCS), a 12-point scale ranging from 3-15 measuring a person’s degree of lucidity and responsiveness. The GCS is the sum measurement of scores assigned to a person’s papillary reaction to light, motor movement response, and verbal appropriateness.9 Scores falling between 12 and 15 are generally considered mild brain injuries, scores between 9 and 12 are generally considered moderate brain injuries, and scores of 8 and below are generally considered severe brain injuries.6,10 No distinction of severity was made within the scope of this study beyond admission to the Intensive Care Unit of their respective hospitals, representing or serving as a proxy for more severe brain injuries.
The cost of treating traumatic brain injuries including hospital, extended care, other medical care, disability, and lost income was estimated at approximately $38 billion in 1985.11 More recent studies focusing specifically on pediatric brain injury estimated $1 billion annually in pediatric hospital charges,3 and almost $1 billion in billed charges in the year 2000.12 The biggest contributors to brain injuries in the pediatric population are falls and motor vehicle crashes.13-16
Previous literature on pediatric brain injury has focused on a wide variety of topics ranging from hospitalization trends and billing3,11,12 to the clinical management of head injuries,8 but very little data has been published from a public heath standpoint on the general health problem of head injuries in the pediatric population. Some studies have been published on the brain injuries across all age groups,11,17 but few studies specifically focus on the highest contributing mechanisms of head injury and the cost of treating head injuries based on the mechanism of injury.13 The purpose of this study was to ascertain and present a general public health perspective on head and brain injuries in the pediatric population, and to determine some degree of the economic burden of pediatric brain injuries.
Methods
Following Institutional Review Board approval, data were accessed via the Children’s Health Corporation of America (CHCA; Shawnee Mission, KS) Pediatric Health Information System (PHIS) database, a unique database which contains resource utilization data from 42 freestanding children’s hospitals and a capture rate of eighteen percent. Participating hospitals are located in non-competing markets of 27 states plus the District of Columbia. CHCA and participating hospitals jointly assure data quality and reliability as described previously.18,19The PHIS database includes demographic information such as patient age, gender, payor status, resident town size, and location of treating hospital. Injury information includes date of admission, discharge date and cause of injury and the outcome information includes length of stay, discharge disposition, and total billed charges.
Patients were included in this study if they were diagnosed with a head injury using ICD-9 codes 800, 801, 803, 804, 850-854, and 959.01 between 1/1/2006 and 12/31/2010, and were flagged if they were treated in an Intensive Care Unit. The selected ICD-9 codes include fractures of the skull vault, fracture of the skull base, other and unqualified skull fractures, multiple fractures involving the skull or face with other bones, concussions, cerebral lacerations and contusions, subarachnoid, subdural, and extradural hemorrhage following injury, other intracranial hemorrhage following injury, intracranial injury of other nature, and unspecified injuries to the head or neck. The first ICD-9 code listed for the patient was used to determine whether the head injury was a primary or secondary injury.
E-codes and Mechanism of Injury
External cause of injury codes (E-codes) were used to determine the specific cause of injury for each of these patients. Patients coded with medical accidents, medication reactions, and poisonings were excluded from this analysis.
E-code groupings basically followed the recommendations of the MMWR report,20 but were coded to see causal factors at a finer level. Research on E-codes show difficulty in using broad-ranging categories21 due to coding complications.22 For this reason, we broke the E-codes into more narrowly-focused categories that allowed for better comparisons between groups. In classifying E-codes, the first E-code listed in the diagnosis list was the E-code that was used to identify the cause of injury. The breakdown for all E-codes used in this study is found in Appendix A.
Appendix A.E-code Table.
| Mechanism | E-codes |
|---|---|
| Motor Vehicle Accidents (MVC) | E810-813, E815-819, E822-825, E829, E846-848, E929.0, E988.5 |
| Motor Pedestrian Collisions (MPC) | E814 |
| ATV/Snowmobile | E820-821 |
| Watercraft Accident | E830-831, E838 |
| Aircraft Accident | E840-841, E844 |
| Railway Accident | E800-801, E805, E807 |
| Assault/Abuse | E928.3, E960, E963-969 |
| Self-Inflicted | E950, E953, E955, E957-959 |
| Neglect | E904 |
| Fall | E804, E834-835, E843, E880.0, E880.1, E880.9, E881.0, E882.0, 883.2, E883.9, E884, E885, E886.0, E886.9, E888, E929.3, E987 |
| Drowning/Submersion | E832, E910 |
| Other Asphyxiation* | E911-913, E983 |
| Animal Injury | E827-828, E905-906 |
| Burn/Scald | E837, E890-891, E893-894, E924, E926, E988.2 |
| Crush Injuries | E918 |
| Environmental Accidents | E900-901, E907-909, E928.8 |
| Explosion/Electrocution | E921, E925 |
| Firearms/ Explosives | E922-923, E985, E997 |
| Home Injuries | E013, E849.7 |
| Late Effects of Injuries | E929.1, E989 |
| Machinery Accident | E919-920.1 |
| Pedal Cycle Accident | E826 |
| Overexertion | E927 |
| Sports Accident | E006-007, E917.0, E917.5 |
| Winter Sports | E003 |
| Stab/Slice/Pierce | E914-915, E920.3, E920.4, E920.8, E920.9 |
| Struck by or Against Object | E916, E917.1, E917.2, E917.3, E917.4, E917.6, E917.7, E917.8, E917.9 |
| Other Accidents | E029.2, E883.0, E973 |
| Unspecified Accidents | E000, E029.9-030, E849.0, E849.3, E849.4, E849.5, E849.6, E849.8, E849.9, E887, E928.9, E929.9, E983.8, E987.0, E988.8-988.9 |
*Includes choking on food, choking on non-food items, other mechanical asphyxiation, and strangulation not able to be determined as accidental.
Injury Type: Accidental and Non-Accidental Injuries
Because non-accidental injuries generally have more severe injuries, longer hospital stays, and worse outcomes compared to accidental injuries,23 all violence-related non-accidental injuries were broken into a separate category called “abuse/assault,” and will be examined in more detail separately. Using E-codes, all injuries were broken down into accidental and non-accidental injuries regardless of the mechanism of injury. Those with an unknown causal factor were listed as unknown injuries. Self-inflicted injuries were kept as a separate category and not included in the non-accidental grouping.
Town Size and Geographical Area
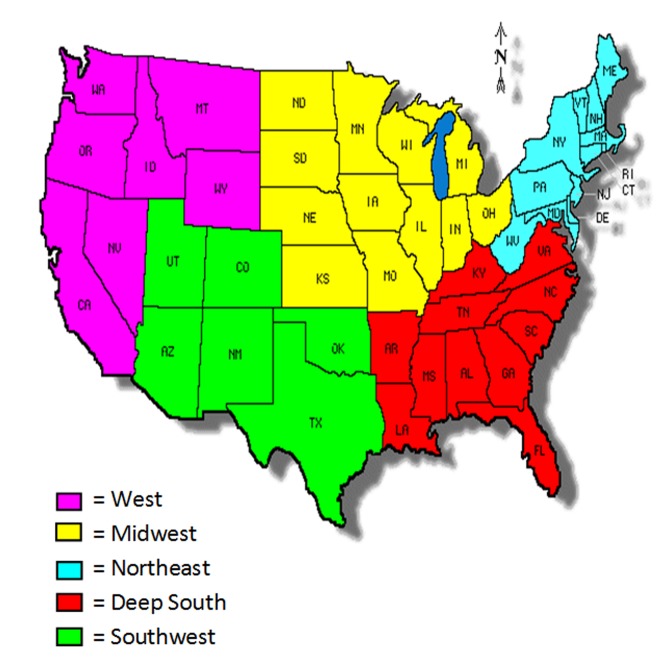
For geographical mapping purposes, the United States was categorized into five different geographical regions. To help maintain confidentiality of the hospitals, each region has at least two CHCA member hospitals. Town sizes were defined using the Second Edition Rural and Urban Commuting Area Code (RUCA 2) data, which bases town sizes from zip codes.24 Towns were then broken up using previously published data on town sizes4,23 to identify urban towns, large towns, small towns, and isolated towns. Due to confidentiality issues, the individual zip codes (which are encrypted in PHIS) were not provided to the researchers, but were linked to the RUCA 2 data by CHCA staff.
Billed Charges
The billed charges captured in this dataset are the actual charges billed by the hospital for the entire hospital stay. All billed charge data were converted to 2010 dollar values using a standard conversion calculation. The total billed charges for 2010 were divided by 1, 2009 values were divided by 0.967, and divided by 0.9370, 0.90376, and 0.8655 for 2008, 2007, and 2006 values, respectively.25 With a capture rate of eighteen percent, national projections were approximated by multiplying the total billed charges by five.
All data was analyzed using SPSS version 18 (SPSS, Chicago, IL).
Results
Demographics and Geographical Distribution
In all, 39,657 patients were included in the study, with 273 being excluded for medical accidents, medication errors, and poisonings. The remaining 39,384 were included in the analysis. Demographic information and regional breakdowns are found in Table 1 , and injury information is found in Table 2.
Table 1: Patient Demographic Information.
| ICU Admits | Non-ICU Admits | Total | |
|---|---|---|---|
| Total N | 11,245 | 28,139 | 39384* |
| Male | 7,210 (64%) | 17,977 (63%) | 25,187 (64%) |
| Female | 4,024 (35%) | 10,150 (36%) | 14,174 (36%) |
| Mean Age (in years) | 6.32 (± 5.6) | 6.26 (± 5.7) | 6.28 (± 5.7) |
| Regional Distribution | |||
| Deep South | 2,540 (23%) | 6,960 (25%) | 9,500 (24%) |
| Midwest | 2,972 (26%) | 6,307 (22%) | 9,279 (24%) |
| Northeast | 1,880 (17%) | 5,561 (20%) | 7,441 (19%) |
| Southwest | 2,274 (20%) | 4,755 (17%) | 7,029 (18%) |
| West | 1,579 (14%) | 4,556 (16%) | 6,135 (15%) |
| Town Size | |||
| Urban | 8,494 (75%) | 22,571 (80%) | 31,065 (79%) |
| Large Town | 1,250 (11%) | 2,446 (9%) | 3,696 (9%) |
| Small Town | 671 (6%) | 1,244 (4%) | 1,915 (5%) |
| Isolated Town | 409 (4%) | 814 (3%) | 1,223 (3%) |
| Not Listed | 421 (4%) | 1,064 (4%) | 1,485 (4%) |
| Payor Source | |||
| Government Insurance | 4,901 (44%) | 11,317 (40%) | 16,218 (41%) |
| Private Insurance | 3,064 (27%) | 8,931 (32%) | 11,995 (30%) |
| Other Insurance | 1,846 (16%) | 4,660 (17%) | 6,506 (17%) |
| Not Listed | 1,434 (13%) | 3,231 (11%) | 4,665 (12%) |
Data collected from 39,384 cases nationwide
Data represent n (%) or mean (± standard deviation)
*Sex was not listed in 23 patients
Table 2: Injury and Accident Information.
| ICU Admits | Non-ICU Admits | N | |
|---|---|---|---|
| Injury | |||
| Primary | 8,336 (74%) | 21,725 (77%) | 30,061 (76%) |
| Secondary | 2,909 (26%) | 6,414 (23%) | 9,323 (24%) |
| Injury Type | |||
| Accidental | 7,145 (64%) | 20,461 (73%) | 27,606 (70%) |
| Non-Accidental | 1,306 (12%) | 2,072 (7%) | 3,378 (9%) |
| Unknown | 146 (1%) | 346 (1%) | 492 (1%) |
| Not Listed | 2,648 (23%) | 5,260 (19%) | 7,908 (20%) |
| Discharge Information | |||
| Home | 9,261 (82%) | 26,870 (95%) | 36,131 (92%) |
| Other | 680 (6%) | 521 (2%) | 1,201 (3%) |
| Died | 767 (7%) | 406 (1%) | 1,173 (3%) |
| Skilled Facility | 326 (3%) | 162 (1%) | 488 (1%) |
| Home Health Service | 211 (2%) | 180 (1%) | 391 (1%) |
Data collected from 39,384 cases nationwide
All patients included in this study were under the age of 18, with an average age of 6.28 years (standard deviation of 5.7). Over the five year period, sixty-four percent of the population was male (n = 25,187). The majority of the patients in the sample had government health insurance (n = 16,218), thirty-one percent were on private insurance (n = 11,995), almost seventeen percent were on “other insurance” (n = 6,506), and almost twelve percent did not have listed insurance status (n = 4,665).
The majority of the patients lived in urban towns (79%, n = 31,065), followed by large towns (9%, n = 3,696), small towns (5%, n = 1,915), and then isolated towns (3%, n = 1,223). Resident town size was not listed in almost four percent of the sample (n = 1,485). A map of the regional breakdown is found in Figure 1.
Figure 1: United States Regional Map.
Injury Status, Outcome, and Accident Information
Over three-quarters of the patients captured in this dataset were diagnosed with a head injury as the primary diagnosis (n = 30,061), and almost one-quarter of the patients had diagnosed head injuries secondary to another injury (n = 9,323).
Almost seventy percent of the patient population was injured through an accidental mechanism (n = 27,606), and almost nine percent were injured through non-accidental means (n = 3,378). Approximately twenty-one percent of the patients had an unknown causal type or the cause was not listed (n = 492 and 7,908, respectively).
A majority of the patients were discharged home (92%, n = 36,131), with “other” as the next most common discharge disposition (3.0%, n = 1,201). Three percent of the population died (n = 1,173), and one percent went to a skilled facility at discharge (n = 488). One percent of the patient population were also discharged into a Home Heath Service (n = 391).
Chi-square analysis further yields significant differences for type of diagnosed head injury (primary or secondary), type of injury, and discharge disposition (p < 0.01). Patient Injury Status and Outcome information can be found in Table 2.
Mechanism of Injury and Billed Charges
Twenty percent of the population did not have an identifiable e-code listed (n = 7,908). However, the most common mechanisms of injuries were falls (n = 11,535), all motor vehicle-related crashes (n = 8,251), and abuse/assaults (n = 3,299). These three mechanism areas represent almost fifty-nine percent of the total injuries. In this instance, motor vehicle-related crashes included motor vehicle collisions, motor vehicle accidents, motor pedestrian collisions, and “other motor vehicle accidents.”
Overall, the total billed charge for these patients was $1.73 billion dollars over the past five-year period. Approximately six percent of the population had no billed charges listed (n = 2,354), and one patient had a billed credit. Excluding these patients from the analysis, the average billed charges in treating these patients was $46,784 (Md $18,369). The average length of ICU stay for these patients was 5.3 days (Md 2 days), ranging from 1 to 1,534 days. The most expensive billed charge was $7.8 million.
Overall, government insurance was billed an average of $52,357 per patient (Md $20,104), private insurance was billed an average of $43,763 per patient (Md $17,615), other insurance was billed an average of $40,929 per patient (Md $16,244), and those with no insurance listed were billed an average of $42,998 per patient (Md $17,510).
For the top ten most common injuries, the total billed charges and the average charges for those injuries are found in Table 3, Table 4 and Table 5, respectively. Motor vehicle collisions and crashes, falls, and assaults/abuses not only account for over half of the injuries, but also account for half of the billed charges over the five-year period. Motor vehicle crashes account for $406.3 million in billed charges over the five-year period, with falls accounting for $244.3 million, and assault/abuse accounting for another $219.5 million in billed charges. Combined, these three areas account for almost $1 billion in billed charges over the five-year period. The top ten most expensive injuries by billed charges are found in Table 4, and the top ten most expensive injuries by average cost per injury are found in Table 5.
Table 3: Top 10 Most Common Head Injury Causes between 2006 and 2010.
| Rank | Cause | ICU Admits | Non-ICU Admits | Total |
|---|---|---|---|---|
| 1 | Fall | 2,229 (20%) | 9,303 (33%) | 11,535 (29%) |
| 2 | MVA | 2,305 (21%) | 4,205 (15%) | 6,510 (16%) |
| 3 | Assault/Abuse | 1,277 (11%) | 2,022 (7%) | 3,299 (8%) |
| 4 | Struck by or Against an Object | 503 (4%) | 1,465 (5%) | 1,968 (5%) |
| 5 | Unspecified Accident | 424 (4%) | 1,393 (5%) | 1,817 (5%) |
| 6 | MPC | 632 (6%) | 1,109 (4%) | 1,741 (4%) |
| 7 | Pedal Cycle Accident | 345 (3%) | 1,128 (4%) | 1,473 (4%) |
| 8 | Sports | 234 (2%) | 873 (3%) | 1,107 (3%) |
| 9 | ATV/Snowmobile Accident | 272 (2%) | 696 (2%) | 968 (2%) |
| 10 | Animal Injury | 139 (1%) | 337 (1%) | 476 (1%) |
Data collected from 39,384 cases nationwide
Table 4: Top 10 Most Expensive Head Injury Causes Between 2006 and 2010 (gross).
| Rank | Cause | Total Injuries | Total Billed Charges | National Projection* |
|---|---|---|---|---|
| 1 | MVA | 6,510 | $377,735,908 | $1,888,679,540 |
| 2 | Fall | 11,535 | $229,080,110 | $1,145,400,550 |
| 3 | Assault/Abuse | 3,299 | $206,039,197 | $1,030,195,985 |
| 4 | MPC | 1,741 | $111,031,461 | $555,157,305 |
| 5 | Unspecified Accident | 1,817 | $63,574,970 | $317,874,850 |
| 6 | Struck By or Against Object | 1,968 | $59,405,074 | $297,025,370 |
| 7 | ATV/Snowmobile | 968 | $36,749,239 | $183,746,195 |
| 8 | Pedal Cycle Accident | 1,473 | $29,710,149 | $148,550,745 |
| 9 | Sports Injury | 1,107 | $19,589,211 | $97,946,055 |
| 10 | Animal Injury | 476 | $18,165,366 | $90,826,830 |
Data collected from 39,384 cases nationwide
*PHIS capture rate is 18%, and National Projection was calculated by multiplying Total Billed Charges by 5.
Table 5: Top 10 Most Expensive Head Injury Causes Between 2006 and 2010 (average).
| Rank | Cause | Total Injuries | Average Billed Charge | National Projection* |
|---|---|---|---|---|
| 1 | Aircraft Accident | 6 | $191,437 | $957,185 |
| 2 | Other Asphyxiation | 7 | $181,685 | $908,425 |
| 3 | Firearms/Explosives | 135 | $100,062 | $500,310 |
| 4 | Overexertion | 11 | $81,106 | $405,530 |
| 5 | Stab/Slice/Piercing | 54 | $79,333 | $396,665 |
| 6 | MPC | 1741 | $67,373 | $336,865 |
| 7 | Assault/Abuse | 3299 | $65,119 | $325,595 |
| 8 | Neglect | 26 | $62,545 | $312,725 |
| 9 | MVA | 6510 | $61,711 | $308,555 |
| 10 | Watercraft Accident | 27 | $56,303 | $281,515 |
Data collected from 39,384 cases nationwide
It should be reiterated that almost twenty percent (n = 7,549) of the study sample had no E-codes listed. These patients account for $461.4 million of the total sum, and an average billed charge of $61,124 per patient. These totals rank first, and tenth in the total billed charges and average billed charge, respectively.
Discussion
Head and brain injuries are a significant contributor to morbidity and mortality in the pediatric and young adult populations. Moreover, they are complex injuries that can be sustained through a number of different mechanisms and causal factors. While many articles discuss the incidence rates of brain injuries as a whole, very little has been published looking at the different causal factors and the costs associated with them.13
This results of this study are similar to another study that identifies motor vehicle collisions and falls as the highest contributors to head injury in the pediatric population.13 Previous research documented the top five causes of head injuries as motor vehicle crashes, falls, assaults, other transports accidents, and being struck by or against an object.13 However, motor vehicle crashes were lower in this study (16.4% vs. 38.9%), and falls were higher (29.1% vs. 21.2%).13 The difference in motor vehicle crashes may be due to the age constraints in this study, and inability for most pediatric hospital patients to drive.
This study shows a marked difference in the total cost of healthcare from previous studies. Where Bowman et al (2008) estimated $1 billion annually in hospital costs for injured children, this study reports annual charges approximately one-third lower. The biggest contributing factor to this difference is the selective use of only 41 pediatric hospitals instead of data incorporating nationwide totals. While missing charges can also account for smaller charge numbers, billing information was documented in ninety-four percent of the patients included in this dataset. However, a more significant factor is the use of billed charges in this study and not the overall healthcare costs to these patients. While the overall costs represent a better global picture of the economic burden of treating these injuries, this study is able to show more direct-care costs to insurance companies, taxpayers, and hospitals.
This study reports approximately $1.7 billion in billed charges over a five-year period, again markedly lower than another study focusing on hospital utilization in children with traumatic brain injury that reports almost $1 billion in total charges for the year 2000 alone.12
However, the database utilized in this study has a capture rate of eighteen percent versus previous studies utilizing nationwide totals. With an eighteen percent capture rate, we can project a national total for billed charges at $9.4 billion over a five-year period. This then converts to $1.8 billion in annual estimated billed charges nationwide in 2010 dollars. While higher than previous studies, this may be due to specialized trauma centers and higher level of care that may be associated with treating head injuries at these centers. Where Schneier et al (2006) reports an average billed charge of $20,325 (Md $8,056), our study reports average billed charges more than twice as high for the total sample. However, non-ICU admissions had an average billed charge of $24,444 (Md $13,224) in this study.
The payor source is also different from previous research. Schier et al (2006) reports sixty percent of the sample size having private insurance and only twenty-five percent covered under Medicaid. The number of patients with government insurance in our study is almost twice as high (41%) and the number of patients with private insurance is exactly half (30%).
Additionally, this study attempted to identify the mechanism of injury related to traumatic brain injury. However, this dataset may have captured both brain and facial injuries, not the injuries related specific to the brain. Clearer and more specific inclusion criteria focusing on intracranial injuries would be more beneficial in the future, but this is one of the limitations of conducting studies using large databases. This study also made no distinction between the severity of the brain injury, and captured all patients listed in the database fitting the inclusion criteria. Data in this study identified patients who were admitted to an ICU, which implies more severe injuries. However, without GCS scores we cannot accurately distinguish or quantify the severity of the injuries in this dataset.
We were also unable to determine whether injuries were localized only to the head, or included multi-system/multi-organ injuries. Multi-organ and mult-system injuries would result in longer hospital stays, higher billed charges, and worse outcomes.
E-code data has the potential to be a great tool for global causal factors, but the vast number of diagnoses a patient may have in a single encounter coupled with missing E-codes make research in this area very difficult. This study alone identified almost forty-thousand patients with ICD-9 codes designating head injuries, but almost twenty percent of the sample did not have an identifiable E-code listed. Missing E-codes can have a significant impact on the outcome of any research conducted using these codes. It is further suggested that any research utilizing E-codes should be more narrowly-focused so that the factors involved in the E-code are analyzed, not the E-code itself.
Another problem with conducting retrospective research on databases is relying on coders to correctly code data. Previous research on the accuracy of E-codes in falls found that forty-six percent of the charts listing an E-code for unspecified falls could be assigned a more specific E-code based on the information documented in the patients’ charts.26 As ICD-9 codes are diagnostic codes used for primarily for billing purposes instead of the clinical management of patients, the validity of database information is questionable, and its application is limited. Additionally, assigning accurate E-codes may be difficult, particularly in determining accidental and non-accidental injuries, based on medical records. Without the ability to review specific charts, we are unable to verify the accuracy of the E-code data.
Another limitation of this study is the inability to capture zip codes of where injuries actually occur. This type of data can generally only be extracted through prospective studies, hospital-specific studies, or other database studies where this information is documented. Residential information may be useful, but research focusing on injuries should focus on the location of the injury whenever possible.
This dataset may also lend itself to selection bias. While many pediatric institutions focus on and treat childhood injuries, not all children under the age of 18 will be seen at pediatric medical centers as older children may be treated at adult hospitals. Although this dataset included and captured patients under the age of 18, those who were treated at adult facilities would not be captured in this dataset. This then points to an overall younger population, smaller catchment, and lower estimate of the projected billed charges for the pediatric population.
Despite the limitations, this study lends a significant contribution to the public health literature, namely in identifying an expanded listing of the top mechanisms of injury to the largest cause of morbidity and mortality in the pediatric population. Instead of focusing on and exploring a specific mechanism, we are able to examine the causes of brain injury as a whole, and the billed charges associated with them. While the billed charges do not represent a complete picture of the cost burden for treating these injuries, it captures some semblance of the magnitude of hospital costs based on the mechanism of injury, which contributes to understanding the breadth and scope of these injuries. Being able to understand brain and head injuries, particularly in terms of the specific mechanism of injury and the greatest contributing factors leading to the causes of head injuries, better prepares public health practitioners and injury prevention professionals to identify the most significant contributors to brain and head injuries. Only with this understanding will we be truly effective at reducing the incidence or prevalence of head injuries in children.
Acknowledgements
The authors thank Matt Hall at CHCA for data extraction and identifying RUCA 2 codes, and Erum S. Khalid for her hard work in the preparation and development of this manuscript.
Footnotes
Funding: This study was completed without financial support.
Competing interests: The authors report no financial conflict of interest in this manuscript.
Ethical approval: This study was approved by the Institutional Review Board at UT Southwestern Medical Center.
References
- 1.Peek-Asa C, Zwerling C, Stallones L. Acute traumatic injuries in rural populations. Am J Public Health. 2004 Oct;94(10):1689–93. doi: 10.2105/ajph.94.10.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kraus JF, McArthur DL. Epidemiologic aspects of brain injury. Neurol Clin. 1996 May;14(2):435–50. doi: 10.1016/s0733-8619(05)70266-8. [DOI] [PubMed] [Google Scholar]
- 3.Bowman SM, Bird TM, Aitken ME, Tilford JM. Trends in hospitalizations associated with pediatric traumatic brain injuries. Pediatrics. 2008 Nov;122(5):988–93. doi: 10.1542/peds.2007-3511. [DOI] [PubMed] [Google Scholar]
- 4. Robertson BD. Differences in service delivery and patient outcome between rural and urban areas: The case of traumatic brain injury at a level I pediatric trauma center in North Texas. Ann Arbor: UMI, ProQest, 2009. [Google Scholar]
- 5.Thurman D, Guerrero J. Trends in hospitalization associated with traumatic brain injury. JAMA. 1999 Sep 8;282(10):954–7. doi: 10.1001/jama.282.10.954. [DOI] [PubMed] [Google Scholar]
- 6.Calvert S, Miller HE, Curran A, Hameed B, McCarter R, Edwards RJ, et al. The King’s Outcome Scale for Childhood Head Injury and injury severity and outcome measures in children with traumatic brain injury. Dev Med Child Neurol. 2008 Jun;50(6):426–31. doi: 10.1111/j.1469-8749.2008.02061.x. [DOI] [PubMed] [Google Scholar]
- 7.Halldorsson JG, Flekkoy KM, Gudmundsson KR, Arnkelsson GB. Arnarson EO.Urban-rural differences in pediatric traumatic head injuries: A prospective nationwide study. Neuropsychiatr Dis Treat. 2007 Dec;3(6):935–41. doi: 10.2147/ndt.s2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen CY, Wu HP. Caring for traumatic brain injury in children can be a challenge! J Emerg Trauma Shock. 2011 Apr;4(2):161–2. doi: 10.4103/0974-2700.82198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atabaki SM. Pediatric head injury. Pediatr Rev. 2007 Jun;28(6):215–24. doi: 10.1542/pir.28-6-215. [DOI] [PubMed] [Google Scholar]
- 10.Ducrocq SC, Meyer PG, Orliaguet GA, Blanot S, Laurent-Vannier A, Renier D, et al. Epidemiology and early predictive factors of mortality and outcome in children with traumatic severe brain injury: experience of a French pediatric trauma center. Pediatr Crit Care Med. 2006 Sep;7(5):461–7. doi: 10.1097/01.PCC.0000235245.49129.27. [DOI] [PubMed] [Google Scholar]
- 11.Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE. Traumatic brain injury in the United States: A public health perspective. J Head Trauma Rehabil. 1999 Dec;14(6):602–15. doi: 10.1097/00001199-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006 Aug;118(2):483–92. doi: 10.1542/peds.2005-2588. [DOI] [PubMed] [Google Scholar]
- 13.Shi J, Xiang H, Wheeler K, Smith GA, Stallones L, Groner J, et al. Costs, mortality likelihood and outcomes of hospitalized US children with traumatic injuries. Brain Inj. 2009 Jul;23(7):602–11. doi: 10.1080/02699050903014907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil. 2005 Jun;20(3):229–38. doi: 10.1097/00001199-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 15. Guice KS, Cassidy LD, Oldham KT. Traumatic injury and children: a national assessment. J Trauma. 2007 Dec;63(6 Suppl):S68-80; discussion S81-6. [DOI] [PubMed] [Google Scholar]
- 16.Hawley CA, Ward AB, Long J, Owen DW, Magnay AR. Prevalence of traumatic brain injury amongst children admitted to hospital in one health district: a population-based study. Injury. 2003 May;34(4):256–60. doi: 10.1016/s0020-1383(02)00193-6. [DOI] [PubMed] [Google Scholar]
- 17.Javouhey E, Guérin AC, Chiron M. Incidence and risk factors of severe traumatic brain injury resulting from road accidents: a population-based study. Accid Anal Prev. 2006 May;38(2):225–33. doi: 10.1016/j.aap.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Mongelluzzo J, Mohamad Z, Ten Have TR, Shah SS. Corticosteroids and mortality in children with bacterial meningitis. JAMA. 2008 May 7;299(17):2048–55. doi: 10.1001/jama.299.17.2048. [DOI] [PubMed] [Google Scholar]
- 19.Shah SS, Hall M, Srivastava R, Subramony A, Levin JE. Intravenous immunoglobulin in children with streptococcal toxic shock syndrome. Clin Infect Dis. 2009 Nov;49(9):1369–76. doi: 10.1086/606048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report 46 (RR-14). Washington, DC: U.S. Department of Health and Human Services, 1997. [Google Scholar]
- 21.Ribbeck BM, Runge JW, Thomason MH, Baker JW. Injury surveillance: a method for recording E codes for injured emergency department patients. Anna Emerg Med. 1992 Jan;21(1):37–40. doi: 10.1016/s0196-0644(05)82234-6. [DOI] [PubMed] [Google Scholar]
- 22.Smith GS, Langley JD. Drowning surveillance: how well do E codes identify submersion fatalities. Inj Prev. 1998 Jun;4(2):135–9. doi: 10.1136/ip.4.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robertson BD, McConnel CE. Town-level comparisons may be an effective alternative in comparing rural and urban differences: a look at accidental traumatic brain injuries in North Texas Children. Rural Remote Health. 2011;11(1):1521. [PubMed] [Google Scholar]
- 24. WWAMI Rural Health Research Center. Rural-Urban Commuting Area Codes (version 2.0). 2009, http://depts.washington.edu/uwruca/, accessed 20 March 2011. [Google Scholar]
- 25. Council of Economic Advisors. Economic Report of the President. Washington, DC: United States Government Printing Office, February 2011.Table B-62. [Google Scholar]
- 26.Kaida AK, Marko J, Hagel B, Lightfoot P, Sevcik W, Rowe BH. Unspecified falls among youth: predictors of coding specificity in the emergency department. Inj Prev. 2006 Oct;12(5):302–7. doi: 10.1136/ip.2006.011924. [DOI] [PMC free article] [PubMed] [Google Scholar]