Abstract
Patterns of correlates, comorbidity and impairment associated with attention-deficit hyperactivity disorder (ADHD) in children and youth were examined in representative samples from the community and from treatment facilities serving medically indigent youth in Puerto Rico. Information from caretakers and youths was obtained using the Diagnostic Interview Schedule for Children, (version IV), measures of global impairment, and a battery of potential correlates. In the community (N=1,896) and the treated samples (N=763), 7.5 and 26.2% of the children, respectively, met criteria for DSM-IVADHD in the previous year. Although the prevalence rates and degree of impairment differed, the general patterns of correlates, comorbidity and impairment were similar in both populations. The exceptions were associated with conduct disorder, anxiety, impairment in the ADHD comorbid group, and age factors that appeared to be related to selection into treatment.
Keywords: ADHD, Correlates, Prevalence, Comorbidity, Hispanic/Latino
The clinical research literature has consistently shown that Attention-Deficit/Hyperactivity Disorder (ADHD) (American Psychiatric Association 1994) is a disabling disorder that affects individuals across the lifespan (Barkley et al. 1990; 2002). However, it is not clear whether the patterns of correlates, comorbidity, and impairment of the disorder in treated samples are the same for persons identified with ADHD in probability community samples. Studying the differences in patterns is important because findings from treatment samples can be biased due to selection effects that Cohen and Cohen (1984) called, “the clinician’s illusion.” They argued that bias can arise because clinical studies tend to focus on persons with more chronic and severe manifestations of the disorder. Insofar as these selection effects are ignored when looking at patterns of correlates, comorbidity, and impairment, the estimates of the associations related to these patterns can be affected by statistical bias known as Berkson’s bias (Angold et al. 1999; Berkson 1950). To estimate the extent of the bias, it is necessary to compare findings in treated samples and epidemiological samples, using similar study designs and measures.
Treatment-referred samples are appropriate for studies that aim to generalize findings to children who receive services in clinics, and also for studies that provide initial descriptions of rare disorders when the concern is identification of potential risk factors, or when very little developmental epidemiological research has been done (Angold et al. 1999). However, when evaluating results from treated cases, researchers must keep in mind the likelihood that these cases have more symptomatology, are more impaired, and usually constitute a higher burden to caregivers than children not receiving services. Also, minority/ethnic groups and prepubertal girls may be underrepresented in clinical samples (Goodman et al. 1997). Epidemiological studies that obtain representative community samples are designed to provide results that can be generalized to children with the disorder in the general population (Angold et al. 1999), but these studies are expensive and often use methods that make their results difficult to compare to clinical studies.
The ADHD research literature is illustrative of the tradeoff between the clinical and epidemiological traditions. There are hosts of studies that use treated samples and samples of convenience (e.g., Barkley 2003; Tannock 1998), but studies with probability community samples are comparatively few in number (Buitelaar 2002). The literature on treated samples has tended to focus on correlates related to clinical features, while the epidemiological literature has placed more emphasis on the prevalence and comorbidity of the disorder. We briefly review findings on risk factors, comorbidity, and impairment that have been reported in the two literatures.
Gender, child prematurity, age (particularly the 6–11 age-range), and speech-language problems have been found to be associated with ADHD both in treatment (Tannock and Schachar 1996) and community samples (Bird et al. 1988; Breslau et al. 1996; Canino et al. 2004; Scahill et al. 1999; Szatmari et al. 1989). Among family variables, negative parent–child relationship, parental negative discipline, and low levels of social support have also been identified as correlates of ADHD in treatment (Barkley et al. 1991; Fischer 1990) and community samples (Keown and Woodward 2002; Woodward et al. 1998).
In treated samples, a significant association has been reported between family burden / stress and ADHD (Barkley et al. 1991; Fischer 1990). Studies with treatment samples also indicate that having a relative with ADHD, major depression or antisocial behaviors increases the risk of ADHD in the offspring (Barkley et al. 1990; Biederman et al. 1992). However, these associations between family burden/stress and family history of psychiatric problems and ADHD have not been studied in community samples. Finally, school variables such as special education/counseling, grade failure and school suspension or expulsion have been found to be associated with ADHD in treatment samples (Barkley et al. 1990). Of these school variables, only grade failure has been studied and found to be significantly associated with ADHD in community samples (Bird et al. 1989).
Results have also been reported from treatment samples associating parental perception of a child’s sleep problems (Corkum et al. 1998) to ADHD, but this relationship has not been examined in community samples. In contrast, parental reports of childhood chronic health problems have been identified as correlates of ADHD in community samples (Bird et al. 1989; Szatmari et al. 1989), but to our knowledge this variable has not been studied in treatment samples.
Our review also suggests that the relation of demographic variables to ADHD has not been much studied in treatment samples. Even though it has been examined in community studies, the pattern of association is mixed. Our group recently reported that urban residence and perception of poverty—rather than actual income—was a correlate of the disorder, when measured using DSM-IV criteria (Canino et al. 2004). Several community studies using earlier diagnostic criteria in children or adolescent samples found an association for socioeconomic status (Bird et al. 1988), family on welfare and urban residence (Szatmari et al. 1989), and income (Scahill et al. 1999).
Comorbidity of ADHD with other psychiatric disorders, particularly conduct disorder, has been documented in community and treated samples but not systematically compared (Biederman et al. 1991; Jensen et al. 1997). Also, recent findings from community studies suggest that the significant association between two disorders may be explained by the presence of other disorders. For example, the comorbidity of ADHD with a depressive disorder may be specific to that disorder or due to an indirect association between these two with anxiety disorders (Costello et al. 2003; Ford et al. 2003). It is important to determine if ADHD comorbidity is specific to a given disorder or due to a pattern of associations across disorders in community and in clinical samples. Finally, the impairment associated with ADHD has been documented mostly in treatment samples. In such instances it is not clear whether the impairment attributed to ADHD is associated or inflated by the disorders that are comorbid with it (Biederman et al. 1991; Hinshaw 2002).
This review suggests that for the variables examined in both types of samples there has been reassuring consistency in the correlates of ADHD, but many correlates identified in one kind of sample have not been studied or reported in the other kind. Moreover, the studies are not always easy to compare because they have used different diagnostic ascertainment methods, different assessment instruments when examining the same construct, and different analytic strategies.
The design of our epidemiological study in Puerto Rico (Canino et al. 2004) provided a unique opportunity to shed light on this issue. This study included both a random sample of children age 4–17 and a probability sample of children referred to treatment, also in the 4–17 age range from the island of Puerto Rico. Identical case ascertainment, assessment, and analytical methods were used. In addition, analyses can be adjusted for the presence of other disorders in order to control for the contribution of comorbidity to the pattern of associations.
Canino et al. (2004) reported the rates of DSM-IV disorders in the community sample. Eight percent of the children qualified for the 12-month diagnosis of ADHD on the basis of information combined across parent and child interviews. The rates varied significantly with age, gender, perception of poverty, zone of residence, global impairment, and service use. In this article, we examine the association of a wide range of potential correlates, indicators of impairment, and comorbidity, and we contrast the findings in the community sample to those in the sample of children who had been referred to treatment.
Unlike the previous report, in this article we focus on diagnoses of ADHD that are based on reports of the parent only. Restricting the informant to the parent allows us to control for informant source in the comparisons of prevalence rate across age-groups. We expect to find similar findings in the two samples for variables related to risk of ADHD, but we do not necessarily expect to find the same findings for variables that are influenced by severity or course of illness. Examples of the former variables include sociodemographic characteristics and caregiver characteristics, while examples of the latter include child variables such as school failure, and parent–child relationship variables. For the second set of variables, the selection factors associated with treatment are likely to influence patterns of association.
Materials and Methods
Participants
The community sample was an island-wide probability household sample of children aged 4–17 years. This sample and the methods of the study have been described in detail elsewhere (Canino et al. 2004). Briefly, the sample was stratified by Puerto Rico’s (P.R.) health reform regions, urban and rural areas, child’s age and gender, using U.S. 1990 Census block groups as primary sampling units. A household was selected for inclusion in the study if it had children between the ages of 4–17. One child was selected at random from each household using Kish Tables (1965) adjusted for age and gender. Out of 2,102 eligible households, 1,886 parent-child dyads were interviewed for a total completion rate of 90.1% for parent-child dyads.
The target population for the clinical sample was the total number of medically indigent children in P.R. ages 4–17 who received mental health and substance abuse services through the public health system and through the private sector by Managed Behavioral Health Organizations (MBHOs) from January 1, 1998 to May 31, 1998. At that time the government of P.R. was undergoing a health reform and had initiated the contracting out with private health insurance companies of all health services previously provided by public health centers across the island to the medically indigent. In this reform, services were provided through MBHOs subcontracted by private health insurance companies using a managed care model. Data for the selection of children in the public mental health and substance abuse sectors were obtained from the rosters of children who received services during the specified time period from 11 community mental health centers and six outpatient substance abuse clinics. For the private sector, claims data from the four MBHOs were used. The selected medically indigent children and adolescents (8,568) received services within the specified period distributed as follows: public outpatient mental health clinics (N=3,489), outpatient substance abuse clinics (N=710), and MBHOs (N=4,368). A systematic sample with a random starting point was selected for both the public and private sectors. The sample was stratified by type of service (public mental health, substance, and MBHO). The selected sample consisted of 1,175 medically indigent children; 400 from the public mental health sector, 150 from public drug and alcohol services, and 625 from the MBHOs. Of the 1,175 selected children, 114 were deemed ineligible. Only one child was selected from each family. The total number of eligible children was 1, 061 and 751 parent-child dyads were successfully interviewed for a response rate of 71.0% for parent–child dyads.
Instruments and Measures
Diagnostic Interview Schedule for Children
Presence of DSM-IV psychiatric disorders in children during the last year was assessed using the latest translation into Spanish of the computerized Diagnostic Interview Schedule for Children, version IV (DISC-IV; Bravo et al. 2001) with parallel youth and parent interview versions. The DISC-IV is a structured instrument designed to be administered by lay interviewers for the assessment of psychiatric and substance use disorders in children and adolescents. Children younger than 11 years were not interviewed because there is evidence that their reports are not reliable (Schwab-Stone et al. 1994). Oppositional defiant disorder (ODD) was excluded from the child protocol due to its poor reliability in child reports (Jensen et al. 1999). In the present research the following diagnoses were ascertained: ADHD, social phobia, panic disorder, separation anxiety disorder, post-traumatic stress disorder, generalized anxiety disorder, major depressive disorder, dysthimic disorder, ODD, and conduct disorder. The translation and adaptation of the DISC-IV into Spanish, as well as its test retest reliability have been reported elsewhere (Bravo et al. 2001). The DISC-IV also measures the level of impairment and distress associated with each diagnosis. The test–retest reliability (kappa statistic) of parent reports of ADHD over one to two weeks including the impairment criterion was 0.49, which represents fair agreement (Bravo et al. 2001).
Brief Impairment Scale (BIS)
The Spanish BIS provides a measure of the caretaker’s report of a child’s global impairment along interpersonal, school/work, and self-fulfillment dimensions of functioning during the last year (Bird et al. 2005). The BIS has high internal consistency (0.81–0.88) and test–retest reliability (0.70) as measured by the intraclass correlation coefficient (ICC). The scale has also shown good concurrent and convergent validity (Bird et al. 2005).
Parent Interviewer Children’s Global Assessment Scale (PICGAS)
The latter yields a global measure of the child’s impairment on adaptive functioning at home, community, school, and with friends as scored by lay interviewers (Bird et al. 1996). The Spanish translation of the PICGAS has been shown to be moderately reliable (test–retest ICC= 0.69). The concurrent, discriminant, and construct validity of the instrument have also been reported (Bird et al. 1996) using combined data from four communities (including Puerto Rico). The PICGAS and BIS are moderately correlated (r=−0.53).
Demographic Factors
We obtained information on child’s gender and age, and caretaker’s education, civil status (not married), household income, zone of residence, and perception of poverty (live well, live from paycheck to paycheck, and live poorly) was obtained from caretaker’s response to a structured interview.
Perinatal and Developmental History
We developed six parent-reported measures: intensive treatment for prematurity during the first month of the child’s life; child’s physical health and limitations to child’s activities due to physical conditions or health; speech or language problems identified by a health professional; grade failure; school expulsion or suspension; and problems sleeping at night during the last year.
Parent–Child Attachment Scale
This scale (ten items) is adapted from Hudson’s Index of Parental Attitudes and the Child’s Attitude Towards Mother/Father Scale (Hudson 1982), and assesses the primary caretaker’s perception about the quality of the parent–child relationship. Estimates of the scale’s reliability range from 0.76 for Hispanic participants (mostly Puerto Ricans) to 0.81 and 0.82 for African-American and Caucasian subjects, respectively (Smith and Krohn 1995). The internal consistency of the scale for Puerto Rican caretakers in our community sample is 0.76. We examined the reliability of this scale and the other instruments used in the present study in a clinical sample of Puerto Rican children described elsewhere (Bravo et al. 2001). The test–retest reliability (ICC) obtained is 0.72.
Family Psychiatric History Screen for Epidemiologic Studies
We used a shortened and revised version of the Lish et al. (1995) scale. It measures history of psychiatric illness in primary caretakers and mental health service utilization. We examined three measures: more inattention or hyperactivity-impulsivity than others during childhood; depression (ever depressed for 2 weeks or more or suicide attempt); and school/job expulsion/arrested (suspended or expulsed from school, fired from job due to attitudinal and performance factors, or arrested, jailed or convicted for a crime).
Family Care Burden Scale
This is a short 7-item scale based on a family burden scale developed by Messer et al. (1996). It measures the impact that the child’s physical health and emotions, behavior, or learning capacity have on the caretaker’s feelings of personal well being, family relationships, activities, and responsibilities. The internal consistency of this scale in our reliability study is 0.72 and the ICC is 0.50.
Parental Discipline Scale
This is an 8-item scale, which inquires about positive and negative parental disciplinary practices (Goodman et al. 1998). We used the scale related to negative disciplinary practices which include physical punishment, yelling, and emotional detachment. For the community sample, the internal consistency of this scale is 0.62 (caretakers) and 0.61 (youths). The ICC in our reliability study is 0.67 (caretakers) and 0.66 (youths).
Social Support Scale
It measures overall satisfaction, help and understanding from others using a single item. In our reliability study the ICC is 0.51.
Parent–Child Involvement Scale
It measures children’s (age 9–17 years) perception of primary caretaker’s involvement and support with school and friends, as well as quantity and quality of time spent together. Scale internal consistencies are 0.70 for Caucasian subjects, and 0.78 for Hispanics (Smith and Krohn 1995). For Puerto Rican youths, the internal consistency obtained in the reliability study is 0.80; the ICC is 0.73.
Procedures
The procedures of the study have been described in detail elsewhere (Canino et al. 2004). The survey was carried out from January 1999 through December 2000. The confidentiality of the participants was protected as required by the University of Puerto Rico Institutional Review Board (IRB). All participants received thorough written and verbal explanations of the study and gave written consent/assent under procedures approved by the IRB. Interviewers were trained to provide a list of resources to parents and children in the event they identified a child they considered in need of specialized services or in case a parent or child asked for a referral. If a respondent reported physical or sexual abuse, interviewers first informed a designated clinician (two child psychiatrists and three clinical psychologists were on call) who was part of the research team before reporting the case to the authorities. The clinician would review the case with the interviewer to determine if immediate protection was needed, in which case the authorities would be informed within a two-h period. In order to ensure that referred cases would not end up in a long waiting list at the Youth and Family Services in Puerto Rico, we established personal contact with a social worker from this agency to whom all cases were sent. Prior to participating in the interview, parents and children were informed that reports of physical or sexual abuse could result in disclosure to appropriate authorities. The consent form also informed parents and children of our responsibility to report these types of events.
Interviews took place in the child’s home and were conducted by different interviewers for the parent and child (they were blind to the results of the other’s interview). Interviews were audiotaped and 15% of these were spot-checked at random for quality control purposes.
Analytic Strategy
The samples were weighted to represent the population of children ages 4–17 in P.R. (community sample) and the Puerto Rican population of medically indigent children of the same age range who received mental health services from January 1, 1998 to May 31, 1998 (treatment sample). Sampling weights reflect differences in selection probability due to the complex sample design. For the treatment sample, sampling weights include an additional adjustment for non-response. All statistical analyses were conducted using SUDAAN software (release 8.0) (Research Triangle Institute 2001). All parameters were estimated with Taylor series linearization methods (Binder 1983).
We defined caseness as presence of DISC-IV criteria based on parental reports including at least one moderate level of impairment or distress linked to each of the psychiatric disorders ascertained. Although in our previous report (Canino et al. 2004) we combined parent and child reports for children aged 11–17 years, in the present study we used parental reports only when estimating prevalence. Unlike children 11–17, younger participants were not interviewed with the DISC-IV and we wanted to compare prevalence rates across age-groups maintaining informant source constant. Also, data have suggested that parents (vs. youths) are more reliable informants for ascertaining the presence of ADHD (Barkley et al. 1991; Bravo et al. 2001; Schwab-Stone et al. 1994; Jensen et al. 1999). Logistic regression was used to estimate both crude and adjusted odds ratios when examining the correlates and patterns of comorbidity of ADHD. Although some of the correlates studied can be conceptualized as antecedents or consequences of ADHD, we organize our presentation in the domains of demographic, child, school, and family characteristics. This analytical approach was consistent with the cross sectional design of the study, which did not allow for analyses of the direction of the association between correlates of ADHD. SUDAAN’s multiple regression procedure was used to contrast the mean response of functional impairment across the different categories of ADHD and other diagnoses. If the main effect for group membership was significant, pairwise contrast were conducted between the five groups.
Because the two samples relate to different populations, and because the sampling designs were different, we carried out analyses in each sample separately rather than combining the data into a single analysis. To compare estimates from the two analyses, we computed a test statistic composed of the difference in the two regression estimates, divided by an estimate of the standard error of that difference.1 Under the null hypothesis of no difference and with the sample sizes available for these analyses, this statistic will be distributed as a standard normal variable (Freeman 1962).
Results
Prevalence of ADHD
The 12-month prevalence rate and corresponding 95% confidence intervals of DISC-IV ADHD for children in the community was 7.5% (6.1–9.3) and 26.2% (23.5–29.2) for those attending mental health and substance abuse clinics. The former estimate of the prevalence rate is slightly lower than the one previously reported by our group (8.0%) (Canino et al. 2004); the difference is due to the fact that the latter was based on both parent and child informants for children aged 11–17. ADHD was more prevalent in boys for both populations. In the community, the prevalence rate for males was 10.3% (8.0–13.1) and for females 4.7% (3.1–7.2). In the clinics, the rate for males was 29.3% (25.9–33.0) and for females 18.7% (14.3–24.1).
Demographic Characteristics of the Two Samples
Tables 1 and 2 show information on the distributions of demographic variables (Table 1), and of the child, school, and family variables (Table 2) for each sample, broken down by ADHD diagnostic status, as well as for the combined sample. The pattern of associations appears quite consistent between the two samples across most of the variables. We analyze these associations in Table 3, which shows both crude odds ratios (OR) as well as adjusted OR that take into account demographic and other correlates. The crude OR and 95% confidence intervals are shown in columns 1 and 3. They are calculated using logistic regression with ADHD as the outcome and each potential correlate treated as the sole explanatory variable. The adjusted OR values shown in columns 2 and 4 are also computed using logistic regression. For the demographic variables, number of non-ADHD diagnoses was entered as a covariate. For the regression analysis of child, school, and family variables, perception of poverty, caretaker’s education, parental marital status, and number of diagnoses other than ADHD were entered as covariates. The analyses reported in Table 3 include perception of poverty rather than family income because the latter variable was not related to risk of ADHD in either sample (see Table 1), and adjusting for family income did not change the pattern of results shown in Table 3. See Canino et al. (2004) for an explicit discussion of this issue. For the child’s number of non ADHD diagnoses variable, the previously mentioned demographic variables were entered as covariates. Zone of residence was excluded from these analyses, since this variable was available only for the community. In Table 3, we note with footnotes the variables for which the adjusted association with ADHD varies across clinical and community samples.
Table 1.
Demographic characteristics for community and treatment populations in Puerto Rico ages 4–17 years by ADHD diagnosis of child
| Community | Treatment | |||||
|---|---|---|---|---|---|---|
| ADHD | Non-ADHD | Total | ADHD | Non-ADHD | Total | |
| Sample size | 143 | 1,754 | 1,897 | 201 | 562 | 763 |
| Gender of child (% male) | 69.5 | 49.5 | 51.0 | 79.5 | 68.2 | 71.2 |
| Mean age of child (years) | 9.2 | 10.6 | 10.5 | 11.2 | 12.7 | 12.3 |
| Gender of caretaker (% female) | 96.5 | 98.0 | 97.9 | 96.8 | 93.2 | 94.2 |
| Mean age of caretaker (years) | 34.8 | 37.8 | 37.6 | 40.5 | 40.4 | 40.5 |
| Caretaker’s marital status (% not married) | 47.4 | 42.3 | 42.6 | 55.4 | 54.5 | 54.7 |
| Caretaker’s education | ||||||
| < High school (%) | 35.8 | 30.8 | 31.2 | 31.8 | 36.4 | 35.2 |
| High school (%) | 41.1 | 40.4 | 40.4 | 49.5 | 47.8 | 48.3 |
| > High school (%) | 23.2 | 28.9 | 28.4 | 18.7 | 15.8 | 16.5 |
| Household income ($) | ||||||
| < 12,000 (%) | 37.6 | 40.9 | 40.6 | 46.5 | 51.6 | 50.3 |
| 12,001–25,000 (%) | 42.6 | 32.8 | 33.5 | 40.0 | 38.1 | 38.6 |
| > 25,000 (%) | 19.8 | 26.4 | 25.9 | 13.4 | 10.4 | 11.2 |
| Poverty perception | ||||||
| Live well (%) | 42.1 | 52.1 | 51.4 | 30.8 | 39.2 | 37.0 |
| Live paycheck to paycheck (%) | 32.8 | 33.8 | 33.7 | 40.5 | 35.4 | 36.7 |
| Live poorly (%) | 25.1 | 14.1 | 14.9 | 28.7 | 25.4 | 26.2 |
All data except sample size are reported as weighted estimates of population percentages or means. ADHD attention-deficit hyperactivity disorder
Table 2.
Child, school, and family variables for community and treatment populations in Puerto Rico ages 4–17 years by ADHD diagnosis of child
| Community (N=1,897) | Treatment (N=763) | |||||
|---|---|---|---|---|---|---|
| ADHD | Non-ADHD | Total | ADHD | Non-ADHD | Total | |
| Child (caretaker’s report) | ||||||
| Treatment prematurity | 15.1 | 6.4 | 7.1 | 13.2 | 8.7 | 9.8 |
| Speech/language problems | 17.9 | 7.2 | 8.0 | 33.0 | 15.4 | 20.0 |
| Child’s health problems | 31.7 | 20.6 | 21.4 | 35.7 | 26.0 | 28.5 |
| Sleep problems (last year) | 29.9 | 8.4 | 10.1 | 43.8 | 21.8 | 27.5 |
| Number of disordersa | 0.9b | 0.1 | 0.2 | 1.5b | 0.4 | 0.7 |
| School (caretaker’s report) | ||||||
| Special education/counseling | 37.7 | 10.9 | 12.9 | 75.7 | 47.0 | 54.5 |
| Grade failure | 21.2 | 16.2 | 16.5 | 39.0 | 43.1 | 42.0 |
| School suspension/expulsion | 15.7 | 7.1 | 7.7 | 35.1 | 25.8 | 28.2 |
| Family (caretaker’s report) | ||||||
| Caretaker’s childhood I or HI | 35.9 | 10.3 | 12.2 | 35.5 | 18.7 | 23.1 |
| Caretaker depression | 59.5 | 26.5 | 29.0 | 58.4 | 47.7 | 50.5 |
| Caretaker expulsion/arrested | 22.3 | 9.6 | 10.6 | 29.6 | 16.1 | 19.7 |
| Family Burden Scalea | 11.3 | 8.4 | 8.7 | 12.5 | 10.2 | 10.8 |
| Parent-Child Attachment Scalea | 30.8 | 35.5 | 35.2 | 29.1 | 32.5 | 31.6 |
| Negative Discipline Scalea | 7.2 | 5.6 | 5.7 | 7.1 | 6.0 | 6.3 |
| Social Support Scalea | 7.6 | 8.1 | 8.0 | 7.3 | 7.7 | 7.6 |
| Family (youth’s age 9–17 report) | ||||||
| Negative Discipline Scalea | 5.2 | 4.0 | 4.0 | 4.7 | 4.4 | 4.4 |
| Parent-Child Involvement Scalea | 24.8 | 26.7 | 26.6 | 25.7 | 25.3 | 25.4 |
All data except sample size are reported as weighted estimates of population percentages or means. ADHD attention-deficit hyperactivity disorder, I inattention, HI hyperactivity–impulsivity
Continuous variable (means); unfootnoted variables are binary (percentages).
For the ADHD group, the mean is for comorbid disorders
Table 3.
Logistic regressions of ADHD diagnosis with crude and adjusted odds ratios for demographic, child, school, and family variables for community and treatment populations in Puerto Rico
| Community (N=1,897) | Treatment (N=763) | |||
|---|---|---|---|---|
| Crude OR | Adjusted OR | Crude OR | Adjusted OR | |
| Demographics (caretaker’s report) | ||||
| Careteaker’s education | ||||
| < High School | 1.14 (0.63–2.07) | 1.11 (0.55–2.25) | 0.84 (0.59–1.20) | 0.72 (0.47–1.09) |
| High School | – | – | – | – |
| > High School | 0.79 (0.46–1.36) | 0.94 (0.46–1.91) | 1.15 (0.76–1.73) | 1.20 (0.77–1.87) |
| Not married | 1.23 (0.79–1.91) | 1.07 (0.65–1.77) | 1.04 (0.76–1.42) | 0.96 (0.67–1.37) |
| Poverty perception | ||||
| Live well | – | – | – | – |
| Live paycheck-paycheck | 1.20 (0.72–2.00) | 0.92 (0.51–1.67) | 1.45** (1.01–2.09) | 1.26 (0.84–1.88) |
| Live poorly | 2.20*** (1.29–3.76) | 1.73 (0.87–3.46) | 1.44 (0.96–2.15) | 1.22 (0.77–1.94) |
| Child (caretaker’s report) | ||||
| Gender (male) | 2.32** (1.36–3.97) | 2.67*** (1.43–5.01) | 1.81** (1.24–2.62) | 2.32**** (1.43–3.76) |
| Agea | 0.91** (0.86–0.96) | 0.91***b (0.85–0.97) | 0.86** (0.82–0.90) | 0.81****b (0.77–0.86) |
| Treatment prematurity | 2.83** (1.30–6.16) | 2.46*** (1.12–5.42) | 1.66** (1.00–2.74) | 1.30 (0.69–2.45) |
| Speech/language problems | 2.82** (1.61–4.95) | 1.48 (0.71–3.09) | 2.71** (1.90–3.86) | 2.51**** (1.60–3.96) |
| Child’s health problems | 1.80** (1.13–2.85) | 1.23 (0.72–2.10) | 1.59** (1.12–2.24) | 0.88 (0.56–1.36) |
| Sleep problems (last year) | 4.64** (2.97–7.24) | 2.16** (1.15–4.03) | 2.80** (2.01–3.91) | 1.26 (0.83–1.92) |
| Number of non ADHD disordersa | 3.84**** (2.71–5.45) | 3.88**** (2.70–5.59) | 2.30**** (1.89–2.78) | 2.32**** (1.90–2.83) |
| School (caretaker’s report) | ||||
| Special education/counseling | 4.97** (3.04–8.13) | 5.04**** (2.85–8.90) | 3.52** (2.50–4.97) | 3.41**** (2.31–5.03) |
| Grade failure | 1.40 (0.85–2.29) | 0.63 (0.32–1.25) | 0.84 (0.62–1.15) | 0.67** (0.46–0.98) |
| School suspension/expulsion | 2.46** (1.31–4.63) | 1.13 (0.55–2.33) | 1.56** (1.11–2.17) | 0.87 (0.57–1.34) |
| Family (caretaker’s report) | ||||
| Caretaker childhood I or HI | 4.88** (3.01–7.91) | 1.83* (0.96–3.49) | 2.39** (1.70–3.36) | 1.11 (0.71–1.74) |
| Caretaker depression | 4.08** (2.59–6.41) | 1.20 (0.67–2.14) | 1.54** (1.14–2.09) | 0.76 (0.52–1.12) |
| Caretaker expulsion/arrested | 2.69** (1.52–4.76) | 1.42 (0.70–2.85) | 2.19** (1.51–3.18) | 1.87*** (1.19–2.94) |
| Family Burden Scalea | 1.41** (1.32–1.52) | 1.19*** (1.06–1.33) | 1.20** (1.15–1.26) | 1.08*** (1.02–1.14) |
| Parent–Child Attachment Scalea | 0.80** (0.76–0.83) | 0.90**** (0.85–0.95) | 0.88** (0.85–0.91) | 0.96* (0.91–1.00) |
| Negative Discipline Scalea | 1.54** (1.33–1.78) | 1.19*** (1.05–1.35) | 1.35** (1.24–1.47) | 1.18*** (1.06–1.31) |
| Social Support Scalea | 0.77** (0.68–0.88) | 1.07 (0.88–1.32) | 0.83** (0.75–0.91) | 0.90 (0.79–1.01) |
| Family (youth’s age 9–17 report) | ||||
| Negative Discipline Scale a | 1.39**** (1.20–1.61) | 1.36c (1.19–1.56) | 1.09 (1.00–1.19) | 1.03c (0.92–1.15) |
| Parent–Child Involvement Scale a | 0.96** (0.92–1.00) | 0.97 (0.92–1.03) | 1.01 (0.98–1.03) | 1.03 (1.00–1.05) |
Ninety-five percent confidence intervals in parentheses. For demographic variables, the adjusted odds ratio (OR) control for number of disorders other than ADHD. For child, school, and family variables, the adjusted OR control for caretaker’s education, marital status, perception of poverty, and number of comorbid diagnoses, as well as for the other variables in the model. For the number of disorders variables, adjustment was made only with the previously mentioned demographic variables. ADHD attention-deficit hyperactivity disorder, I inattention, HI hyperactivity–impulsivity.
Continuous variables; unfootnoted variables are binary.
p<0.01 for the difference of the adjusted regression coefficients between community and clinical samples.
p<0.001 for the difference of the adjusted regression coefficients between community and clinical samples.
p=0.06,
p<0.05,
p<0.01,
p<0.001
Overview of Differences Between Samples
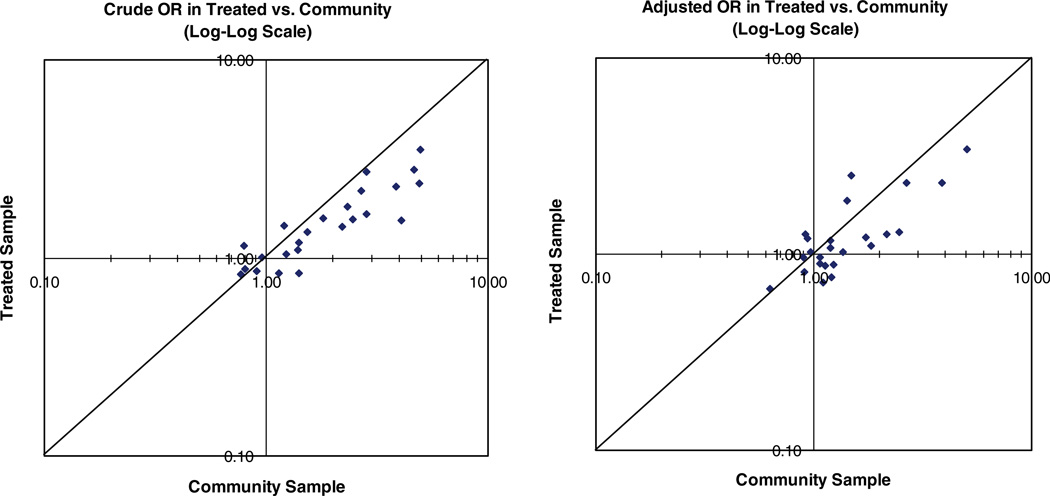
The pattern of associations with demographic, child, school, and family variables shows remarkable similarity across community and clinical samples, although the size of the associations tend to be larger in the community sample. The left panel of Fig. 1 is a plot of the crude OR for the two independent samples. The consistency of the relative magnitude of the findings is striking and is reflected in the strong association (r=0.87) of the OR estimates. Also apparent is that for nearly 80% of the crude OR estimate; the value is higher in the community sample than in the clinic sample. As we review the correlates below, we will emphasize the similarity of the findings, except for age and negative discipline as reported by youths that were statistically different across sample types.
Fig. 1.
Correspondence of sets of crude (left panel) and adjusted (right panel) odds ratios (OR) for treatment and community samples
Demographic Correlates and Adjustment Variables
As in our previous report (Canino et al. 2004), perception of poverty was related to ADHD in both the community and the clinical sample before adjusting for other variables. Those reporting that they lived well had fewer children with ADHD. However, when caretaker’s education, civil status, and number of non-ADHD diagnoses were adjusted, the association was reduced and was no longer statistically significant. Because perception of poverty was more strongly related to ADHD than reports of overall family income, we use this variable to control for social class in the adjusted analyses as previously indicated.
Child, School, and Family Correlates
In both the community and clinical samples all child, family and school unadjusted variables based on caretaker’s reports were significantly associated with ADHD with the exception of grade failure (Table 3). Across both samples, children with ADHD tended to be male, younger, have more intensive treatment for prematurity during the first month of life, to have more language, health and sleep problems, and to qualify for DSM-IV diagnoses other than ADHD. They also were referred more for special education/counseling and experienced more suspensions/expulsions from school. Interestingly, in both Puerto Rican samples, children with ADHD were not significantly more likely to experience grade failure than children without ADHD.2
In both samples, the family characteristics of children with ADHD were strikingly different from those without ADHD. The unadjusted results revealed that children with ADHD were more likely to come from families in which the caretaker reported her or his own ADHD symptoms in childhood. In addition, the caretaker was more likely to have a history of depression and of being expelled/arrested. Families with ADHD children were also more likely to report higher family burden, and higher negative discipline, but lower parent–child attachment, and levels of social support. Although the child’s reports of family processes were generally consistent with the parent’s reports in the community sample, the children with ADHD in the clinic appeared not to differ from children without that diagnosis in the family measures. Indeed, the difference between the samples in child-reported negative discipline was one of the few sample differences that was statistically reliable.
We have been emphasizing the common patterns of associations in the community and clinic samples, but we wondered whether these comparisons might have been confounded by important differences in the two samples. We know that the clinical sample experiences higher levels of general global disadvantage, and that this disadvantage is itself related to the prevalence of ADHD. To compare the two samples while taking into account these differences, we examined the full range of child, school and family associations while adjusting for measures of global disadvantage including perception of poverty, caretaker’s education, parental marital status, and number of diagnoses other than ADHD.
When we adjusted for these potential confounding effects (columns 2 and 4 in Table 3), the odds ratios tended to be reduced, especially in the community sample. This overall pattern is reflected in the right panel of Fig. 1, which shows the correspondence of the two sets of results after adjustment. The adjustment reduces the magnitude of the associations, especially in the community sample. This suggests that a portion of the associations previously discussed is due to general disadvantage. As in the left panel of the figure, the pattern of associations remains very similar in the two samples; the correlation of the points is .83.
As a result of the general reduction in the odds ratios due to adjustment, several of the associations in both samples were no longer statistically significant. The variables that lost significance were child’s health problems, child’s school suspension/expulsion, caretaker depression, caretaker’s childhood impulsivity/hyperactivity,3 social support and youth’s report of parent–child involvement. Five associations remained significant in both samples after adjusting for social class and global comorbidity. These were gender, age, special education, family burden, and caretaker-reported negative discipline. In addition, the adjusted OR for the parent–child attachment scale as reported by the caretaker was clearly significant in the community and it approached significance (p=0.06) in the clinic sample. Other associations lost significance in one sample but not the other. The fact that a variable has a significant association in one sample but not the other should not be interpreted as a genuine difference between the study results. Only two variables had associations with ADHD after adjustment that was statistically different in magnitude between the samples: age and youth-reported negative discipline.
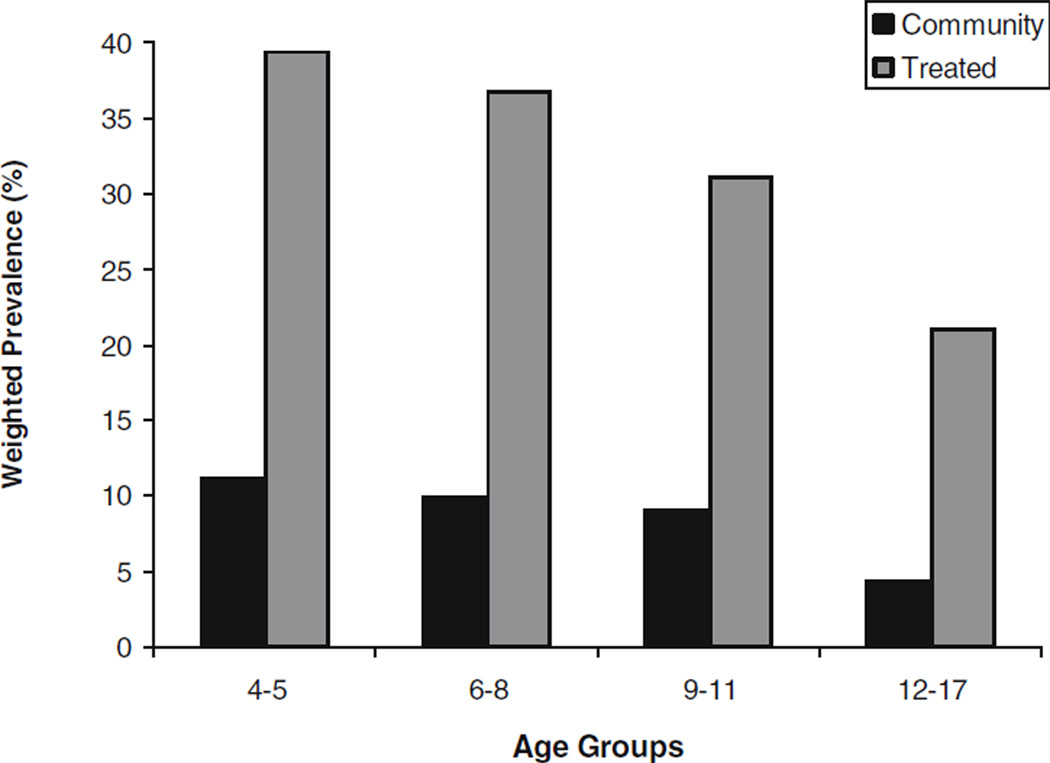
In contrast to the general pattern of stronger associations in the community sample than the clinical sample, the association of age with ADHD after adjustment was stronger in the clinic sample. Although ADHD becomes less prevalent with older ages in both samples, the decline in prevalence is steeper in the clinic sample. We explored this relationship further by plotting the age specific prevalence rates in Fig. 2 for the two samples. In the community sample, the prevalence of ADHD was highest in the 4–5 age groups (11.2%) and decreased in the 6–8, 9–11, and 12–17 age groups to a rate of 4.4%. When computing the comparable rates in the clinical sample we first noted that there were too few children in the 4–5 age groups to obtain a stable estimate. However, from the rate of 36.8% in the 6–8 age groups, the rate declined sharply to 21.1% in the 12–17 age groups. The figure makes it clear that the proportion of the younger children with ADHD in the clinic is much higher than the community, but that the difference in the rates is reduced when older children are considered.
Fig. 2.
Weighted 12-month prevalence (%) of DISC-IV ADHD for children in the community and for those attending mental health and substance abuse clinics in Puerto Rico by age groups
The other association that differs systematically in the community and clinic samples after adjusting for global disadvantage is the youth’s report on the Negative Discipline scale. In contrast to the findings for age, the association with this scale and ADHD is stronger in the community sample than in the clinic sample. In fact, the association is significant in the community, but completely missing in the clinic.
ADHD Patterns of Comorbidity
In general, comorbidity of ADHD with other disorders was more common in the clinic sample. In the community the percentage of children positive for ADHD with zero, one, or two or more additional DISC-IV diagnoses was 46, 30, and 24%, whereas in the clinic the percentages were 27, 34, and 39%. Table 4 shows the rates of conduct disorder (CD), ODD, any anxiety and any depression among those diagnosed with ADHD in the past year, as well as the rates of ADHD among those diagnosed with each of the four classes of disorder. With the exception of CD, the rates of the disorders among children with ADHD were higher in the clinic, consistent with the treatment selection effects (Angold et al. 1999). This pattern was also reflected in the rates of ADHD among children with ODD, anxiety, and depression.
Table 4.
Patterns of comorbidity for ADHD in community and treatment samples, with and without adjustment for other disorders (weighted data)
| Comorbid category (CC) | % ADHD With CC | % CC with ADHD | Unadjusted OR | Adjusted OR for other disorders |
|---|---|---|---|---|
| Community Sample (N=1,897) | ||||
| CD | 13.18 | 72.43 | 37.79*** (13.72–104.05)a | 5.88* (1.09–31.88) |
| ODD | 38.89 | 53.07 | 22.17*** (13.01–37.77) | 13.29***(6.37–27.71) |
| Any Anx | 24.43 | 37.40 | 9.41*** (5.03–17.62)b | 5.35***(2.13–13.47) |
| Any Dep | 9.27 | 35.25 | 7.39*** (3.20–17.07) | 0.66 (0.16–2.71) |
| Treatment Sample (N=763) | ||||
| CD | 10.22 | 44.89 | 2.42** (1.35–4.34)a | 0.60 (0.26–1.37) |
| ODD | 61.19 | 66.76 | 12.94***(8.83–18.96) | 13.30***(8.40–21.05) |
| Any Anx | 33.51 | 51.89 | 4.04***(2.75–5.94)b | 2.93***(1.82–24.73) |
| Any Dep | 22.73 | 51.01 | 3.50*** (2.25–5.46) | 0.84 (0.48–1.47) |
Ninety five percent confidence intervals in parentheses, ADHD attention deficit hyperactivity disorder, CD conduct disorder, ODD oppositional defiant disorder, Any Anx any anxiety disorder, Any Dep any depressive disorder, OR Odds Ratio. Adjusted ORs for column 4 were derived from a logistic regression model that included all disorders as predictors.
Unadjusted odds ratio in community is different from unadjusted OR in clinic, p<0.01.
Unadjusted odds ratio in community is different from unadjusted OR in clinic, p<0.05
p<0.05,
p<0.01,
p<0.001
Table 4 (column 4) also shows the OR reflecting the association of ADHD with each of the disorders after taking into account prevalence rates. Although the proportion of cases with comorbid disorders is higher in the clinical sample for three of the four disorders, the strength of the comorbidity association is generally stronger in the community sample. For two disorders, CD and any anxiety, the difference in the odds ratios between the samples is statistically significant.4 Despite the differences in the samples, the OR are all significantly different from unity, indicating a consistent pattern of comorbidity of ADHD with all four disorders in both samples.
The last column of Table 4 shows the association of each disorder with ADHD after adjusting for comorbidity with the other disorders. In these logistic regression models, the odds of having ADHD was examined as a function of having CD, ODD, any anxiety, and any depressive diagnosis.5 This analysis allowed us to determine if the comorbidity was specific to a given disorder or due to a more general pattern across disorders. After adjustment there was no longer a significant association between ADHD and any depressive disorder in either sample. In the clinics, ADHD was no longer significantly associated with CD after adjustment. In both samples, ODD and any anxiety remained associated with ADHD after adjustment. The effect of the adjustment was generally larger in the community sample, and the difference between the magnitudes of the association for any anxiety that was previously noted was no longer evident after adjustment. For CD the difference in magnitude was maintained.
ADHD and Global Impairment
We next assessed the impairment profile across groups by dividing participants into those with ADHD alone and ADHD comorbid, and those with other diagnoses alone and other diagnoses comorbid. These four groups were compared with a group of children with no diagnosis, controlling for demographic variables. All groups with a diagnosis were significantly different from the no diagnosis group. Furthermore, for each sample and both impairment measures, the comorbid groups were the most impaired (Table 5).
Table 5.
Mean impairment for ADHD alone, ADHD comorbid, other diagnoses alone, other diagnoses comorbid, and no diagnoses group in community and treatment samples (weighted data)
| Groups | ||||||
|---|---|---|---|---|---|---|
| Measures | ADHD-A | ADHD-C | Other Dx-A | Other Dx-C | No Dx | Comparisons |
| Community Sample | ||||||
| N | 67 | 75 | 73 | 32 | 1,635 | |
| BIS | 11.18 (1.01) | 19.03 (1.41) | 13.06 (0.90) | 16.95 (1.81) | 7.25 (0.21) | C=OC>A=OA>No |
| PICGAS | 68.24 (3.20) | 55.42 (3.07) | 69.24 (2.24) | 58.71 (3.11) | 86.27 (0.65) | C=OC<A=OA<No |
| Treatment Sample | ||||||
| N | 55 | 144 | 70 | 55 | 428 | |
| BIS | 18.10 (1.14) | 24.34 (0.74) | 18.78 (1.19) | 22.50 (1.48) | 12.08 (0.34) | C=OC>A=OA>No |
| PICGAS | 59.53 (2.39) | 49.80 (1.66) | 54.79 (2.12) | 45.90 (2.32) | 71.59 (0.87) | C=OC<A=OA<No |
The five groups were compared controlling for demographic variables. Mean impairment scores are adjusted for demographic variables. Standard errors in parentheses. Means are based on cases with valid values. ADHD attention-deficit hyperactivity disorder, A alone, C comorbid, OA other diagnoses alone, OC other diagnoses comorbid, No no diagnoses, BIS Brief Impairment Scale, PICGAS Parent Interviewer Children’s Global Assessment Scale. Higher BIS and lower PICGAS scores indicate more global impairment. For both samples, the null hypothesis of equal mean BIS and PICGAS impairment across groups was rejected (WALD F range: 27.81 to 38.17; p<0.001). Pairwise comparisons were significant at least at the 0.05 alpha levels, except for the PICGAS C vs. OA comparison which was 0.06
The mean difference between each of the diagnosis groups and the no diagnosis group on the BIS and PICGAS was contrasted across the community and clinical populations. The only contrast that was found to be significant was the mean difference on the PICGAS between the ADHD comorbid and the no diagnosis group. The mean difference was significantly larger in the community sample (p<0.01). This difference is mainly due to the fact that the no diagnosis group in the clinical sample is more impaired than the same group in the community sample. The level of impairment of the ADHD comorbid groups is similar across samples.
Discussion
Over a wide range of possible correlates, as well as variables representing comorbidity and impairment, we found the pattern of associations with the diagnosis of ADHD to be similar in representative samples of children from the community and from treatment service settings. With only a few exceptions, the magnitude of the associations was larger in the community sample than in the clinical sample. This increased magnitude is likely to be influenced to the fact that the overall rate of ADHD in the community was 1/3 the size of the rate in the treated sample. Although ADHD is rare among community members in general, those who are in risk categories defined by comorbid CD or any anxiety disorder have comparable ADHD risk in both samples. The contrast between the risk group and the baseline is more striking in the community sample, and hence estimates of associations are larger.
Community-based epidemiological studies provide the best evidence for the relation of both risk factors and consequences of mental disorders (e.g. Cohen and Cohen 1984; Angold et al. 1999), but we found that results obtained from our sample of treated patients generally approximated the results from the community. Although there was evidence of bias in the magnitude of the associations obtained in clinical samples, the direction of the bias tended to be toward more conservative findings. An important exception is age, which we discuss in detail later.
Common Findings in Two Samples
Based on caretaker reports, children in both samples with the DISC-IV diagnosis of ADHD were more likely to be male, younger rather than older, and to have had a history of medical, behavioral and educational problems, including treatment for premature birth, general health problems, speech and language problems, sleep problems, and other DSM-IV disorders. In school, children with ADHD were more likely to be receiving counseling or special education, and to have had a history of suspension or expulsion. According to reports by the caretaker, the children with ADHD in both samples are more likely to have come from families in which the caretaker suffered childhood impulsivity or hyperactivity symptoms, had a history of depression, had a history of school/job expulsion/arrested, and felt relatively bereft of social support. These caretakers reported more burden due to the care of the child with ADHD, lower quality of relationship with the child, and a tendency to use more negative discipline than caretakers of children without ADHD.
In both samples, the list of associations just reviewed could have been shared with other disorders besides ADHD. Moreover, we found that ADHD was more common in children with conduct disorder, oppositional defiant disorder, as well as anxiety and affective disorders. It is likely that comorbidity is itself related to the correlates we have considered. For this reason, we revisited the associations after adjusting for generalized disadvantage and comorbidity.
When these adjustments were taken into account in our analysis of correlates of ADHD, only a subset of variables remained significantly associated in both samples. These correlates appear to be more specific to ADHD than the others: gender, age, perceived family burden, poorer parent–child relationships and parental report of negative discipline. In addition, children with ADHD appeared to be more likely to receive school based services than children without ADHD, even after adjustment for other disorders and social disadvantage.
We considered similar adjustments in our analyses of comorbidity. In both samples, ODD and any anxiety remained strongly associated with ADHD after adjustment, for the presence of other diagnoses, but depression was no longer associated after the adjustment. This finding is consistent with other recent reports (Costello et al. 2003; Ford et al. 2003). It also indicates the need for further research on the extent to which comorbidity between disorders may be explained by the presence of other disorders (Ford et al. 2003).
With regard to impairment, the rank order of differences in global impairment levels found between groups across populations was similar. These results indicate that the ADHD comorbid group is more globally impaired than the other non-comorbid groups after adjusting for demographic variables, independently of whether children are sampled from clinics or the community. The fact that the ADHD alone group was significantly more impaired than the group without DISC-IV diagnoses support the view that the impairment associated with the disorder is due to the disorder itself and cannot be accounted by psychiatric comorbidity or treatment status. These results are very robust since they were replicated with different impairment measures (BIS and PICGAS) and informants (caretaker and lay interviewer).
The cross-sectional nature of the analyses of both samples prevents a strict causal interpretation of these associations, although it seems likely that school services are, in part, a response to the difficulties associated with ADHD. Perceived family burden and poorer parent–child relationships could be outcomes as well as risk factors for ADHD. It is interesting that the association of gender with ADHD was very similar in both samples after adjusting for disadvantage and other disorder with an odds ratio of approximately 2.5, but the etiologic meaning of this association is a topic of ongoing debate (e.g., Heptinstall and Taylor 2002).
Contrasting Findings in Two Samples
The most important difference between the findings based on the community sample and the clinical sample had to do with the nature and magnitude of the age effect. We found that children under the age of 6 were virtually never referred to treatment, even though our community sample documented that ADHD is evident in children as young as 4 years old. It is likely that children are not referred at younger ages because the impairment associated with ADHD only becomes prominent at the time the child enters school. However, studies that rely on clinic samples will be unable to document the full developmental progression of ADHD.
While children under the age of 6 with ADHD are underrepresented in our clinical sample, children with ADHD are overrepresented in the age range 6–8. More than a third of the children in that age range qualify for a diagnosis of ADHD on the basis of the caretaker’s report. Like in the community sample, the prevalence of ADHD decreases in older age groups, but the rate of decrease is steeper in the clinical sample than the community sample. This is one of the rare instances in our comparisons where an association between ADHD and a correlate is stronger in the clinical sample than the community sample. We believe the explanation for this difference rests with the processes that identify children of different ages for treatment, as well as the processes that retain the children in the treatment setting. By the time children are 12–17 years old, they are likely to be referred to treatment because of symptoms of internalizing disorders as well as externalizing behaviors that are unrelated to ADHD. Because of the possibility of selection processes competing with developmental processes, we believe that age effects in clinical samples should be studied with longitudinal rather than cross-sectional designs.
The decrease of ADHD rates with age is consistent with previous reports (e.g., Costello et al. 2003). However, it is important to note that this decline may be affected by the fact that the types of symptoms and the diagnostic thresholds set in the DSM-IV for inattention and hyperactivity–impulsivity are not necessarily in correspondence with the different developmental periods underlying the age groups analyzed (Barkley et al. 2002). Also, the fact that parents were the sole informants used to ascertain the diagnosis of ADHD (see below) might have contributed to an under detection of symptoms in the 12–17 age range. This point is particularly relevant to inattention symptoms which are more evident in the school setting and tend to persist with age (Hart et al. 1995).
In addition to age, the only other variable that seemed to relate to ADHD differently in the clinical and community samples was youth report of negative discipline. Consistent with the general tendency for stronger associations in the community sample, youth report of negative disciplinary practice was associated with higher rates of ADHD in the community but not in the clinics. The absence of any association based on youth reports in the clinic flies in the face of consistent associations between ADHD and the parent reports of negative discipline. Both in the community and clinic populations, parents who report more negative discipline are more likely to have children with ADHD. The children in the clinic with ADHD do not seem to notice the greater negative discipline that the parents report. Whether this is a systematic effect of their disorder on the reporting process, or a chance sampling fluctuation, is difficult to ascertain. We simply note that youth reports of this variable in clinical samples should be viewed cautiously.
Another important difference in findings between the community sample and clinic sample had to do with the strength of the comorbid association between ADHD and both CD and any anxiety. Consistent with the other correlates, the associations were higher in the community than in the clinical sample. The pattern of this bias is precisely the one discussed by Angold et al. (1999) as an example of selection effects. They show with a concrete example (pp. 60–61) how the scarcity of cases with no diagnosis in clinical samples can diminish estimates of the association of two disorders.
The last important difference between populations involved the difference in impairment, as measured by the PICGAS, between the ADHD comorbid group and the no diagnosis group. This difference was larger in the community sample mainly due to different levels of impairment of the no diagnosis group across populations. In the clinical sample this group had a higher level of impairment resulting in a smaller difference when contrasted with the ADHD comorbid group. The level of impairment of the comorbid ADHD groups was similar across populations.
Relation of Findings to Other Studies
The prevalence rate of ADHD in our clinic sample (26.2%) is comparable to that reported by Garland et al. (2001) in youths across five sectors of care (24.4%). This does not guarantee the generalizability of our findings for our clinical sample, but it does reassure us that the general makeup of our Puerto Rican clinical sample is comparable to samples on the mainland.
The current findings with regard to age and ADHD are somewhat different from those reported by Bird et al. (1988) on the basis of a survey of DSM-III disorders. In our community sample we found that ADHD became less common as children aged, and that ADHD was found in more than 10% of the youngest group. Bird’s group, in contrast, did not find many cases of ADHD among the 4–5 year old age group according to DSM-III criteria. It is likely that DSM-IV ADHD allows the detection of the disorder in younger children that were not previously identified. One third of the children ages 4–5 with ADHD in our community sample presented the hyperactive–impulsive type of the disorder, a subtype that was introduced for the first time in the DSM-IV.
As in previous studies, having an ADHD diagnosis increased significantly the probability of having an additional diagnosis (Angold et al. 1999; Tannock 1998) independently of treatment-referral status. Although statistically significant, the ADHD-CD comorbidity rates obtained in both our samples (10–13%) are lower than the rates reported in community (Jensen et al. 1997; Ford, personal communication) and clinical studies (about 20–50%) (Barkley 2003; Biederman et al. 1991). It is conceivable that children aged 11–17 may be better informants of CD and internalizing disorders than parents. We checked to see if the comorbidity rates would differ from those obtained when combining information across parent and child interviews. Our analyses indicated a similar pattern of findings when youth reports were considered (data not shown).
The lower ADHD-CD comorbidity in the present study is probably due to the overall lower rates of CD that have been documented among island Puerto Rican children and adolescents (Bird et al. 2001; Canino et al. 2004). The possibility that the lower rates obtained in P.R. might relate to underreporting by parents is unlikely. A study carried out in P.R. from a different perspective (Nevares et al. 1990) supports these findings. The study also found markedly lower rates of juvenile delinquency in P.R. than in longitudinal cohort studies conducted in Philadelphia (Wolfgang et al. 1972; Tracy et al. 1990) whose methods the P.R. study replicated. The lower rates of CD in the island have been attributed to strong family relations and social support among island’s youths (Bird et al. 1988) as compared to youth’s from other U.S. communities. The presence of a lower comorbidity rate for these two disorders is theoretically important since it points out to how socio-cultural variables could serve as protective factors for the development of CD, and as a result, the comorbidity of ADHD with this disorder. Further research work is needed in this area using longitudinal designs given the importance of its theoretical and clinical implications.
Finally, the correlates of ADHD in these Latino/Hispanic populations are in general comparable to those reported in previous research (Bird et al. 1989; 1988; Fischer 1990; Scahill et al. 1999; Szatmari et al. 1989; Woodward et al. 1998). An intriguing exception is grade failure which was not positively associated with ADHD in either sample. In the treatment sample the diagnoses of ADHD is actually protective against grade failure after adjusting for covariates. These children might be receiving educational interventions that allow them to be promoted instead of failed.
Importantly, correlates such as gender, age, family burden, parent–child relationship, and negative discipline appear to be more specific to ADHD than other correlates. The impairment associated with ADHD appears to be due to the disorder itself and cannot be accounted for by comorbidity with the disorders ascertained or treatment status (Hinshaw 2002). To our knowledge this is the first study to support these relationships in probability community and treatment samples, using identical case ascertainment, assessment, age range, and analytic methods and controlling for the contribution of social disadvantage and other disorders to the pattern of association.
Limitations
Our findings are limited to comparisons of parent reports. Teachers’ reports were not obtained due to budgetary limitations. Although in the DISC-IV only symptoms that parents report as present at home and school or other settings are considered for the diagnosis, they may not be fully cognizant of their children’s behavior at school. There is evidence, however, that suggests that parent-based diagnosis of ADHD in clinical samples can predict a diagnosis based on teacher report (Biederman et al. 1990).
Correlates of the disorder were ascertained from information provided only by self report from the child or the parent. No independent measures were obtained for correlates and impairment indicators. Consequently, the relations obtained may have been affected by shared method variance. However, this source of bias would have affected both the results of the community sample and clinical sample equally.
Our findings are also limited by the cross sectional design of our study. It is not possible to determine whether the correlates associated with ADHD were antecedents or consequences of the disorder. However, relevant information was obtained that can serve to formulate hypotheses that could lead to longitudinal studies.
A third important limitation of the design of our study of the clinical sample is that the sample was identified in 1998, but not interviewed until 2000. Because of this delay, there were children in the clinical sample who were not in treatment at the time of the evaluation, or even a year before the evaluation. However, the clinical sample was still more impaired than the community sample. Also, approximately 80% of the children in the clinical sample were receiving psychosocial services during the one-year time frame of the study.
Implications of Findings
The most important implication of our findings is that studies of clinical samples can be viewed as generally informative, if conservative, reports of correlates of disorders such as ADHD. The important exception to that general rule is the study of age effects, which seem to be obscured in the clinic by age-specific referral patterns. Without direct comparisons of representative community and clinical samples, it is impossible to know the extent of the bias associated with selection effects (e.g., Berkson’s bias). Our study shows that the magnitude of the bias may be limited for ADHD after prudent adjustment is made for the most obvious variables related to selection.
Our findings have important implications for intervention. Children with ADHD are globally impaired, independently of their comorbidity and treatment-referred status, and this disorder is highly prevalent as early as the preschool years. Thus, the importance of a public health policy related to an early identification and treatment of children with ADHD. The pattern of correlates of the disorder clearly indicates the importance of psychosocial variables in the treatment of ADHD based on a comprehensive assessment of children and their families. Individual treatment of the child through medication or psychosocial interventions may not be sufficient. Treatment has to be tailored to the needs of the child and his family and take into consideration, among other factors, parent–child relationships, parenting practices, family burden associated with the disorder, child’s sleep and speech / language problems, and proper school placement.
Acknowledgement
Data for this study were obtained through NIMH funded grants: MH54827. Canino (PI) and P01-MH 59876-02 Alegría (PI), and from P20 MD000537-01 Canino (PI) from the National Center for Minority Health Disparities. We thank Lizbeth Fabregas, the project director of the study, Graciela Reina and Adrianne Anderson for their generous assistance, and Bill Sribney for his comments on an earlier version of the manuscript.
Footnotes
Let BM be the regression coefficient for the community sample, and SM be its standard error. Let BL be the comparable coefficient for the clinical sample, and SL be its standard error. The test statistic, which under the null hypothesis is asymptotically distributed as a standard normal deviate, is .
After adjusting for selection variables, it appears that children with ADHD in both samples might be even less likely to experience grade failure than other children.
Note, however, that caretaker’s childhood I or HI approached significance (p=0.06) in the community sample.
The strength of the association between CD and ADHD was so much stronger in the community that even the conditional rates of disorder shown in columns 2 and 3 were higher in the community. This was despite the fact that overall rates of both ADHD and CD were lower in the community.
In addition, the previous models were augmented adjusting for demographic variables. However, since the latter did not alter significantly the patterns of associations, the results presented in last column in Table 4 are adjusted only for other comorbid conditions.
Contributor Information
José J. Bauermeister, Email: jjbauer@prtc.net, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico; 177 Las Caobas St, San Juan, Puerto Rico 00927.
Patrick E. Shrout, Department of Psychology, New York University, New York, NY, USA
Rafael Ramírez, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico.
Milagros Bravo, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico; Graduate School of Education, UPR, San Juan, Puerto Rico.
Margarita Alegría, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico; Department of Psychiatry, Harvard University, Cambridge, MA, USA; Cambridge Health Alliance, Cambridge, MA, USA.
Alfonso Martínez-Taboas, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico; Carlos Albizu University, San Juan, Puerto Rico.
Ligia Chávez, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico.
Maritza Rubio-Stipec, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico.
Pedro García, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico.
Julio C. Ribera, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico San Juan Veterans Administration Hospital, San Juan, Puerto Rico.
Glorisa Canino, Behavioral Sciences Research Institute (BSRI), University of Puerto Rico (UPR), San Juan, Puerto Rico.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Barkley R. Attention deficit hyperactivity disorder. In: Mash EJ, Barkley RA, editors. Child psychopathology. 2nd. ed. New York: Guilford; 2003. pp. 75–143. [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I An 8–9 year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Edelbrock C, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria-III. Mother–child interactions, family conflicts and maternal psychopathology. Journal of Child Psychology and Psychiatry. 1991;32:233–255. doi: 10.1111/j.1469-7610.1991.tb00304.x. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology. 2002;111:279–289. [PubMed] [Google Scholar]
- Berkson J. Are there two regressions? Journal of the American Statistical Association. 1950;45:164–180. [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, et al. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder. Patterns of comorbidity in probands and relatives psychiatrically and pediatrically referred samples. Archives of General Psychiatry. 1992;49:728–738. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- Biederman J, Keenan K, Faraone SV. Parent-based diagnosis of attention deficit disorder predicts a diagnosis based on teacher report. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:698–701. doi: 10.1097/00004583-199009000-00004. [DOI] [PubMed] [Google Scholar]
- Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. American Journal of Psychiatry. 1991;148:564–577. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- Binder DA. On the variances of asymptotically normal estimators from complex surveys. International Statistics Review. 1983;51:279–292. [Google Scholar]
- Bird HR, Andrew H, Shwab-Stone M, Goodman SH, Dulcan M, Richters J, et al. Global measures of impairment for epidemiologic and clinical use with children and adolescents. International Journal of Methods in Psychiatric Research. 1996;6:295–307. [Google Scholar]
- Bird HR, Canino GJ, Davies M, Ramirez R, Chavez L, Duarte C, et al. The Brief Impairment Scale (BIS): A multidimensional scale of functional impairment for children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:699–707. doi: 10.1097/01.chi.0000163281.41383.94. [DOI] [PubMed] [Google Scholar]
- Bird HR, Canino GJ, Davies M, Zhang H, Ramirez R, Lahey BB. Prevalence and correlates of antisocial behaviors among three ethnic groups. Journal of Abnormal Child Psychology. 2001;29:465–478. doi: 10.1023/a:1012279707372. [DOI] [PubMed] [Google Scholar]
- Bird HR, Canino G, Rubio-Stipec M, Gould MS, Ribera J, Sesman M, et al. Estimates of the prevalence of childhood maladjustment in a community survey in Puerto Rico: The use of combined measures. Archives of General Psychiatry. 1988;45:1120–1126. doi: 10.1001/archpsyc.1988.01800360068010. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Yager T, Stahezza B, Canino G. Risk factors for maladjustment in Puerto Rican children. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:847–850. doi: 10.1097/00004583-198911000-00006. [DOI] [PubMed] [Google Scholar]
- Bravo M, Ribera J, Rubio-Stipec M, Canino G, Shrout P, Ramirez R, et al. Test–retest reliability of the Spanish version of the Diagnostic Interview Schedule for Children (DISC-IV) Journal of Abnormal Child Psychology. 2001;29:433–444. doi: 10.1023/a:1010499520090. [DOI] [PubMed] [Google Scholar]
- Breslau N, Brown GG, DelDotto JE, Kumar S, Ezhuthachan S, Andreski P, et al. Psychiatric sequelae of low birth weight at 6 years of age. Journal of the Abnormal Child Psychology. 1996;24:385–400. doi: 10.1007/BF01441637. [DOI] [PubMed] [Google Scholar]
- Buitelaar JK. Epidemiological aspects: What have we learned over the last decade? In: Sandberg S, editor. Hyperactivity and attention disorders of childhood. New York: Cambridge University Press; 2002. pp. 30–63. [Google Scholar]
- Canino G, Shrout PE, Rubio-Stipec M, Bird HR, Bravo M, Ramirez R, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico: Prevalence, correlates, service use, the effects of impairment. Archives of General Psychiatry. 2004;61:85–93. doi: 10.1001/archpsyc.61.1.85. [DOI] [PubMed] [Google Scholar]
- Cohen P, Cohen J. The clinician’s illusion. Archives of General Psychiatry. 1984;41:1178–1182. doi: 10.1001/archpsyc.1984.01790230064010. [DOI] [PubMed] [Google Scholar]
- Corkum P, Tannock R, Moldofsky H. Sleep disturbances in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:637–646. doi: 10.1097/00004583-199806000-00014. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Fischer M. Parenting stress and the child with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology. 1990;19:337–346. [Google Scholar]
- Ford T, Goodman R, Meltzer H. The British child and adolescent mental health survey 1999: The prevalence of DSM-IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- Freeman H. Introduction to statistical inference. Reading, MA: Addison-Wesley; 1962. [Google Scholar]
- Garland AF, Hough RL, McCabe KM, Yeh M, Wood PA, Aarons GA. Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:409–418. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Hoven CW, Narrow WE, Cohen P, Fielding B, Alegría M, et al. Measurement of risk for mental disorders and competence in a psychiatric epidemiologic community survey: The National Institute of Mental Health Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study. Social Psychiatry and Psychiatric Epidemiology. 1998;33:162–173. doi: 10.1007/s001270050039. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Lahey BB, Fielding B, Dulcan M, Narrow W, Regier D. Representativeness of clinical samples of youths with mental disorders: A preliminary population-based study. Journal of Abnormal Psychology. 1997;106:3–14. doi: 10.1037//0021-843x.106.1.3. [DOI] [PubMed] [Google Scholar]
- Hart HE, Lahey BB, Loeber R, Applegate B, Frick PJ. Developmental changes in attention-deficit hyperactivity disorder in boys: A four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23:729–750. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- Heptinstall E, Taylor E. Sex differences and their significance. In: Sandberg S, editor. Hyperactivity and attention disorders of childhood. New York: Cambridge University Press; 2002. pp. 99–125. [Google Scholar]
- Hinshaw SP. Is ADHD an impairing condition in childhood and adolescence? In: Jensen PS, Cooper JR, editors. Attention deficit hyperactivity disorder. Kingston, New Jersey: Civil Research Institute; 2002. pp. 5–21. [Google Scholar]
- Hudson WW. Methodological observations on applied behavioral science. A measurement package for clinical workers. Journal of Applied Behavioral Science. 1982;18:229–238. doi: 10.1177/002188638201800210. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: Implications for research, practice, and DSM-V. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1065–1079. doi: 10.1097/00004583-199708000-00014. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird H, Dulcan MK, Schwab-Stone ME, et al. Parent and child contributions to diagnosis of mental disorder are both informants always necessary? Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- Keown LJ, Woodward LJ. Early parent–child relations and family functioning of preschool boys with pervasive hyperactivity. Journal of Abnormal Child Psychology. 2002;30:541–553. doi: 10.1023/a:1020803412247. [DOI] [PubMed] [Google Scholar]
- Kish L. Survey sampling. New York: Wiley; 1965. [Google Scholar]
- Lish JD, Weissman MM, Adams PB, Hoven CW, Bird H. Family psychiatric screening instruments for epidemiologic studies: Pilot testing and validation. Psychiatry Research. 1995;57:169–180. doi: 10.1016/0165-1781(95)02632-7. [DOI] [PubMed] [Google Scholar]
- Messer SC, Angold A, Costello EJ, Burns BJ. The Child and Adolescent Burden Assessment (CABA): Measuring the family impact of emotional and behavioral problems. International Journal of Methods in Psychiatric Research. 1996;6:261–284. [Google Scholar]
- Nevares D, Wolfgang ME, Tracy PT. Delinquency in Puerto Rico: The 1970 birth cohorts study. Westport, CT: Greenwood; 1990. [Google Scholar]
- Research Triangle Institute. SUDAAN user’s manual, Release 8.0. Research Triangle Park, NC: Research Triangle Institute; 2001. [Google Scholar]
- Scahill L, Schwab-Stone M, Merikangas KR, Leckman JF, Zhang H, Kasl S. Psychosocial and clinical correlates of ADHD in a community sample of school-age children. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:976–984. doi: 10.1097/00004583-199908000-00013. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone M, Fallon T, Briggs M, Crowther B. Reliability of diagnostic reporting for children aged 6–11 years: A test–retest study of the Diagnostic Interview Schedule for Children-Revised. American Journal of Psychiatry. 1994;151:1048–1054. doi: 10.1176/ajp.151.7.1048. [DOI] [PubMed] [Google Scholar]
- Smith C, Krohn MD. Delinquency and family life among male adolescents: The role of ethnicity. Journal of Youth and Adolescent. 1995;24:69–93. [Google Scholar]
- Szatmari P, Offord DR, Boyle MH. Correlates, associated impairments and patterns of service utilization of children with attention deficit disorder: Findings from the Ontario Child Health Study. Journal of Child Psychology and Psychiatry. 1989;30:205–217. doi: 10.1111/j.1469-7610.1989.tb00235.x. [DOI] [PubMed] [Google Scholar]
- Tannock R. Attention deficit hyperactivity disorder: Advances in cognitive, neurobiological, and genetic research. Journal of Child Psychology and Psychiatry. 1998;39:65–99. [PubMed] [Google Scholar]
- Tannock R, Schachar R. Executive dysfunction as an underlying mechanism of behavior and language problems in attention deficit hyperactivity disorder. In: Beitchman JH, Cohen N, Konstantareas M, Tannock R, editors. Language, learning, and behavior disorders: Developmental, biological, and clinical perspectives. New York: Cambridge University Press; 1996. pp. 128–155. [Google Scholar]
- Tracy PE, Wolfgang ME, Figlio RM. Delinquency careers in two birth cohorts. New York, New York: Plenum; 1990. [Google Scholar]
- Wolfgang ME, Figlio R, Sellin T. Delinquency in a birth cohort. Chicago: University of Chicago Press; 1972. [Google Scholar]
- Woodward L, Taylor E, Dowdney L. The parenting and family functioning of children with hyperactivity. Journal of Child Psychology and Psychiatry. 1998;39:161–169. [PubMed] [Google Scholar]