Abstract
Lumbar spinal stenosis is a common condition in elderly patients and also one of the most common reasons to perform spinal surgery at an advanced age. Disc degeneration, facet degeneration and hypertrophy, and ligamentum flavum hypertrophy and calcification usually participate in the genesis of a stenotic condition in the elderly. These changes can lead to symptoms by themselves or decompensate a preexisting narrow canal. Although some lesions are more central or more lateral, this classic dichotomy is less present in the elderly patient, in whom the degenerative process usually encroaches both central and lateral pathways. Some less common causes of lumbar spinal stenosis are found in the aging subject, such as Paget's disease. However, it must be stressed that so-called stenotic images (sometimes severe) are present on imaging studies in a great number of symptom-free individuals, and that the relationship between degenerative lesions, importance of abnormal images, and complaints is still unclear. Lumbar stenosis is a very common reason for decompressive surgery and/or fusion. Various conditions can lead to a narrowing of the neural pathways and differential diagnosis with vascular troubles, also common in the elderly, can be challenging. The investigation of stenotic symptoms should be extremely careful and thorough and include a choice of technical examinations including vascular investigations. This is of utmost importance, especially if a surgical sanction is considered to avoid disappointing results.
Keywords: Lumbar spinal stenosis, Elderly, Paget's disease
Introduction
Although stenosis and claudication were described as early as 1883 [14], the modern description of this pathology was performed by Verbiest [32] in the 1950s. Lumbar spinal stenosis is a common condition in elderly patients and also one of the most common reasons to perform spinal surgery at an advanced age [31]. Spinal stenosis leading to radiculopathy or neurogenic claudication can be caused by various factors, of which a number are related to degenerative processes. The real participation of so-called congenital stenosis is still subject of debate. Global degenerative changes in the osteoarticular system associated with aging causes similar lesions throughout the body. However, degeneration in the spine has some very specific characteristics. The three-joint nature of the functional unit and the intimate contact with neural structures as well as the existence of a large avascular structure (the intervertebral disc) account for this specificity. Degenerative disc disease is by far the most common cause of lumbar spinal stenosis. A bulging degenerated intervertebral disc anteriorly, combined with thickened infolding of ligamenta flava and hypertrophy of the facet joints posteriorly result in narrowing of the spinal canal. The site of compression may be central, lateral, or a combination of the two [36].
Also specific to spinal degeneration is the fact that although all elderly subjects do not present with osteoarthritis of peripheral joints such as hips or knees, nearly all exhibit radiological images of degeneration on spine imaging, as well in symptomatic than in symptom-free patients [3]. The latter observation is interesting, as most patients with severe osteoarthritis of knee or hip present complaints, but many with severe images of degeneration are symptom free [3]. Furthermore, abnormal images on magnetic resonance imaging (MRI) do not predict in any way the occurrence of spine-related complaints 7 years later [4]. Autopsy studies on large number of subjects have found disc degeneration, facet joints osteoarthritis, or osteophytes in 90–100% of subjects aged over 64 years [19, 34]. Identification of stenotic images in the middle and exit zones of the foramen have been made possible by MRI studies, and stenosis has been found in up to 80% of subjects aged over 70 years [25]. Furthermore, a poor correlation between radiological stenosis and symptoms has been reported [10]. This means that in many cases spinal degeneration cannot really be considered as a disease, and that the relationship between complaints and radiological changes must be very cautious.
As for many continuous characteristics, both canal size and dural sac size present a Gaussian distribution. When a canal size is too narrow for the dural sac size that it contains, stenosis occurs. An identical canal size can therefore be stenotic for one person but not for another who happens to have a smaller dural sac size. Lumbar spinal stenosis is therefore a clinical condition and not a radiological finding or diagnosis. In addition, a poor correlation between radiological stenosis and symptoms has been reported [11]. It must be stressed that stenosis is not a pathological entity per se as up to 21% of nonsymptomatic subjects over the age of 60 years demonstrate stenotic images on MRI [3]. This means that the size of the canal is only one component in the pathogenesis of symptomatic stenosis. Lumbar spinal stenosis refers to a pathological condition causing a compression of the contents of the canal, particularly the neural and vascular structures. If compression does not occur, the canal should be described as narrow but not stenotic [24]. The functional status of the spine has also been studied in relation to stenosis and the worsening of symptoms in extended position. It has been shown that subjects with degenerative changes inducing a borderline canal diameter but without complaints have abnormal patterns of motion in sagittal extension recalling those in stenotic patients [30]. This suggests a sort of proprioceptive protective behavior in the case of potentially stenotic movements.
Some definitions need to be clarified. The classic symptom characterizing spinal stenosis is neurogenic claudication. The pathophysiology of this phenomenon is not entirely understood. However, Porter [22] and Porter and Ward [23] have proposed an elegant theory. In this explanation claudication is caused by the venous pooling induced by the stenotic impairment of venous drainage at root level and occurs only if stenosis (central and/or lateral) is present at two adjacent levels. This situation is, however, not the rule and most stenotic patients do not present with true neurogenic claudication. In this review we consider as stenotic as stenosis all situations in which radiculopathy and/or claudication is present and compression of the dural sac and/or roots is found on imaging studies (with the exclusions of herniated discs, soft arthrosynovial cysts and tumors).
The participation of "congenital" stenosis to the later development of symptoms is controversial. It seems that, excluding the true severe achondroplasia and some other rare congenital conditions, the so-called congenital narrow canals are merely the extreme of the Gaussian distribution of normal subjects as described above. This is further stressed by the fact that these subjects rarely have any troubles unless they develop degenerative changes. The concomitant presence of degenerative changes appears to be a prerequisite to the development of symptomatic spinal stenosis [16]. Classically, central stenosis and lateral stenosis have been described as distinct entities. However, it appears that in the elderly with marked degenerative changes central and lateral lesions are linked in the genesis of complaints. These complaints linked to stenosis are sciatic pain due to the direct compression of neural structures and neurogenic claudication. The exact etiopathogenesis of the latter is still under debate, but the theory presented by Porter and Ward [22, 23] appears to explain (almost) the nature of this symptom. In elderly patients the differential diagnosis with claudication of vascular origin is of the utmost importance to find the adequate treatment and avoid useless surgical procedures.
Differential diagnosis
In elderly persons many concurrent pathologies are often present. Among these, vascular disorders can be a challenge in the differential diagnosis in both acute and chronic presentations of spinal stenosis. Among the acute conditions able to mimic a cauda equina syndrome are ruptured abdominal aortic or iliac aneurysms, acute aortic dissection, acute leg ischemia, and deep venous thrombosis. In the more frequent case of chronic conditions it is arterial insufficiency causing intermittent ischemia that most resembles neurogenic troubles. Presentation of intermittent leg pain and discomfort, usually during walking, shows, sometimes subtle, differences between the two pathologies. In both claudications walking becomes impossible but only in neurogenic is stooping or sitting necessary to alleviate the symptoms. Likewise, claudication appears in both cases during a walking test whereas cycling is interfered only by arterial problems. With advanced neurogenic claudication descending stairs becomes impossible obliging patients to walk downstairs backwards to adopt a forward flexed position, going upstairs is usually without problems, in contrast to arterial pathologies which all stair walking difficult.
Arterial claudication involves the posterior leg muscles only, sometimes the buttocks, perhaps the thighs, always the calf, but never the anterior muscles and the groin. Intermittent numbness (hypesthesia) in the sole of the foot may occur after exercise. This should not be confused with paresthesia (pins and needles). It is most likely to be confused with S1 root suffering [9]. In neurogenic claudication elements other than the leg pain are often present: sensory-motor disturbances and low back pain. The diagnosis is to be oriented by history (smoking, previous arterial disease, cold feet, previous lumbar problems, postural and occupation pain factors, walking stairs) and by a complete examination including appropriate orthopedic, neurological, and vascular tests. Given the age group involved, both pathologies may be present in the same patient. In these cases the differential diagnosis, especially if surgery is foreseen, may be a headache. Vascular and stenotic problems are maybe more frequently intercorrelated than generally assumed, and we advocate a basic vascular investigation prior to spinal stenosis surgery [8]. In diabetic patients it may be difficult to differentiate between lumbar stenosis and diabetic polyneuropathy as the latter is also common in older individuals. Electrophysiological investigations help to distinguish between these two pathologies although they are appear to be of more limited utility in the investigation of neurogenic claudication [1].
Central stenosis
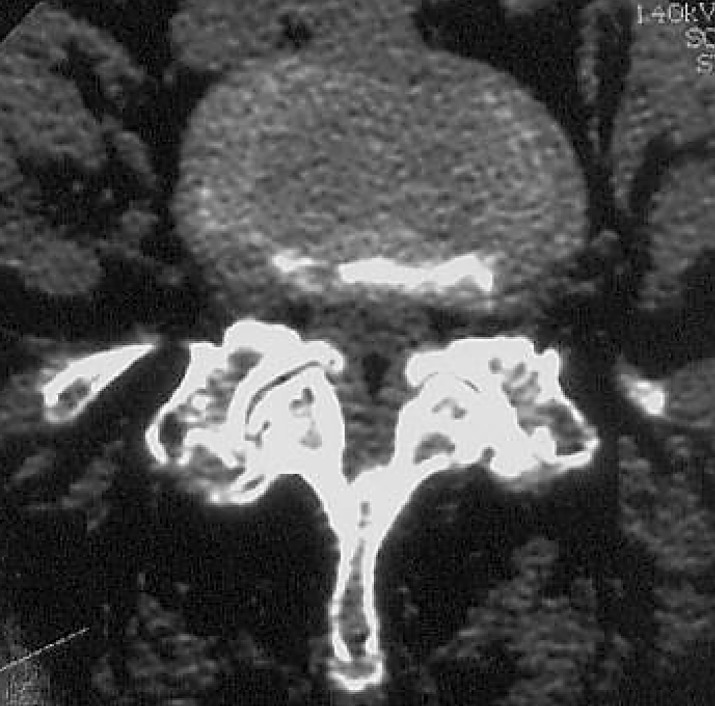
Central stenosis in the elderly is the result of a combination of factors. Disc degeneration and collapse of the disc results in a uniform bulging of the posterior annulus, which encroaches the neural canal surface. In some cases symptoms are present only in sagittal extension as a borderline stenosis may appear only in this position [30]. Dynamic assessment techniques are welcome in those cases (Fig. 1). Also as a result of disc collapse a secondary zygapophyseal arthrosis with facet hypertrophy occurs, further diminishing the central canal at the intervertebral level. Degenerated facet joint, when showing medial hypertrophic changes, may also participate in the canal stenosis (Fig. 2).
Fig. 1.

Myelogram showing multilevel central degenerative stenosis. Myelography remains the only widely available examination enabling dynamic and upright assessment
Fig. 2.
Degenerative hypertrophy of joints narrowing central canal
Due to this disc collapse and decrease in intervertebral height the often thickened ligamentum flavum [27] may buckle [24], thus further decreasing canal space at the disc level. Furthermore, fibrotic chondrometaplasic changes and even ossification of the ligamentum flavum may also occur [20, 24, 28, 29]. This reduces the elasticity of the ligamentum, which may then bulge in the canal even if it keeps a normal thickness [24]. Several studies have shown a higher frequency of calcification of ligamentum flavum in stenotic than nonstenotic subjects [28]. The extent of these histological changes appears to be correlated with age [28]. It must, however, be stressed that in the elderly central and lateral lesions very often both participate in the stenostic pathology (Fig. 3).
Fig. 3.
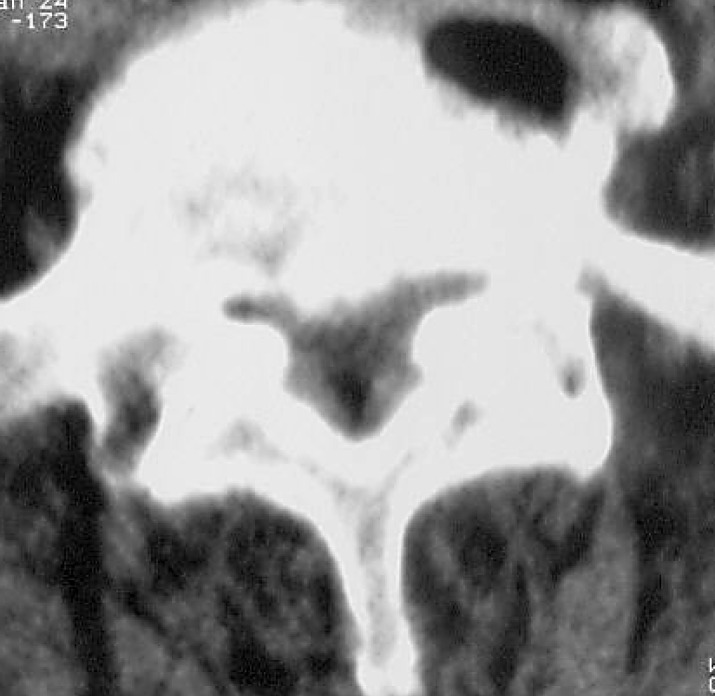
Trefoil-shaped canal typical of combined central and lateral stenotic conditions
Lateral or root canal stenosis
Lateral stenosis is defined as an entity in which a nerve root, dorsal root ganglion, or spinal nerve is entrapped in its pathway. In the case of degenerative changes the nerve root can be subject to compression secondary to the disc collapse by approximation of the pedicles due to the decrease in disc height. Furthermore, hypertrophy of the facet joint or other osteophytic changes can compress the root at its entrance in the foramen or in the foramen itself (Fig. 4). Whereas anteriorly McNab spurs (traction osteophytes at the insertion level of Sharpey fibers) are the rule in spondylosis, they seldom occur posteriorly. However, when present they participate in the narrowing the both the central and the lateral canal. Other osteophytes can be found such as those resulting from the calcification of an arthrosynovial cyst (Fig. 5). It appears that degenerative lesions are also often present in the middle zone or exit zone of the L4–L5 and L5–S1 foraminal pathways [25].
Fig. 4.
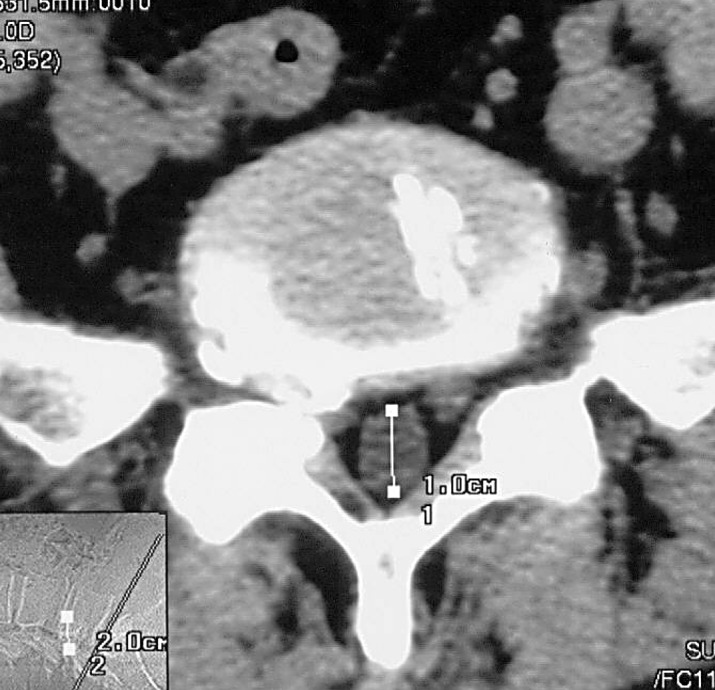
Lateral stenosis with intraforaminal osteophyte causing nerve entrapment
Fig. 5.

Calcified arthrosynovial cyst causing root entrapment
Degenerative spondylolisthesis
Degenerative spondylolisthesis, described by McNab [18] as "spondylolisthesis with an intact neural arch," are most frequent at the L4–L5 level and may result in a stenotic condition. The term degenerative spondylolisthesis was coined by Newman [21]. The displacement due to facet hypertrophy can critically narrow the canal. In contrast to isthmic spondylolisthesis, degenerative spondylolisthesis is self-contained and rarely reaches grade II. Claudication, or much more often sciatic pain, are the encountered symptoms in stenosis secondary to degenerative spondylolisthesis. This is related to the fact that degenerative spondylolisthesis is usually at one level, and the two level pathogenesis described by Porter is not reached. Central stenosis is rare in lytic spondylolisthesis but in some cases of L5–S1 displacement the posterior element can be pulled forward against the body of S1, thus compressing the corda [35]. More often the loss of height of the disc induces a posterior bulging, which can trap the nerve root ion the foramen resulting in lateral stenosis. The osteofibrous callus present at the isthmic fracture level can exceptionally become hypertrophic (Gill's nodules) [7] and compress the neural canal. Although those conditions are usually discovered in younger patients, they are occasionally be a problem in the elderly.
Other conditions
Other conditions in the elderly can cause spinal stenosis. Neurological complications are common in Paget's disease as the spine is one of the most common sites affected by the disease. The lumbar spine is involved in 50% of cases [12]. Enlargement of the vertebral body is common (Fig. 6), and this flattened body can compromise the integrity of the intervertebral foramina, interfere with the blood supply to the dura and nerve roots, or lead to spinal stenosis [26]. A single vertebra is usually involved; however, the frequency of neurological complications are rare compared with the high frequency of lumbar spine involvement in Paget's disease of bone. The vast majority of patients suffering of spinal Paget have no symptoms, yet when symptomatic, it is not necessarily at the level of Pagetic involvement. The Pagetic vertebra may favor disc prolapse, which in itself can cause nerve root entrapment. The increased vascularity of the Pagetic vertebrae may diminish the spinal cord or the nerve root blood supply, ultimately leading to a spinal artery steal syndrome [5]. The Pagetic process can involve the neural arches further reducing the diameter of the central or lateral canal.
Fig. 6. a.
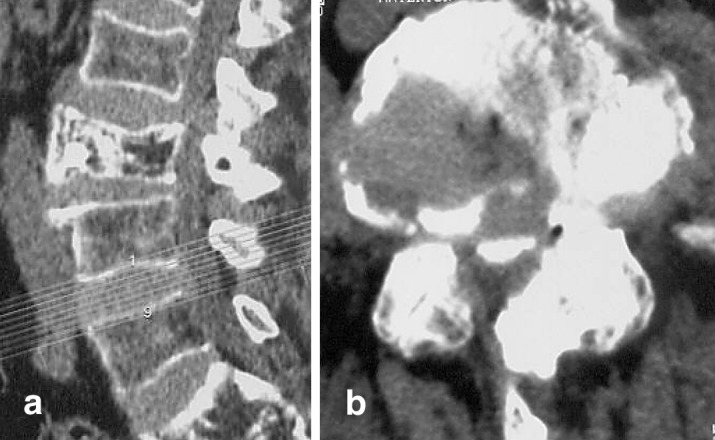
Lateral view of an enlarged Pagetic vertebra causing global stenosis. b Axial view
Some cases of amyloidosis, associated with prolonged hemodialysis or amyloid tumors, and causing spinal stenosis or even cauda equina syndrome have been reported [15]. However, amyloid deposit in the ligamentum flavum have been reported in series of patients with spinal stenosis who did not present the amyloidosis conditions described higher. The presence and the abundance of those deposits are closely correlated to age [6]. The meaning of these deposits in the context of stenosis is, however, unclear. Rare cases of epidural gas leaks originating from the degenerative intradiscal space may cause compressive phenomena [13].
Iatrogenic stenosis
Iatrogenic stenoses are of course not specific to the elderly. They can happen after spinal surgery at any age (Fig. 7). However, some spinal disorders specific to the elderly are often treated in very aggressive way, and the generous use of instrumentation (or even abuse of it) may cause stenotic situations. One of these conditions is degenerative deformity, usually scoliosis.
Fig. 7.
Central stenosis above a fusion site. Fusion was performed with pedicular screws
Relationship of stenosis and heavy manual work
The relationship in elderly persons between back troubles and occupation is the subject of much discussion. Some authors have suggested a relationship between long-term heavy manual work and spinal stenosis [2]. Using ultrasound measurements McDonald et al. [17] showed that a narrower spinal canal is associated with increased back-related complaints in coal miners. There are conflicting reports about the relationship of long-term heavy physical labor and/or exposure to vibration and the appearance of spinal degeneration (disc degeneration and osteophytes). In very complete review Videman and Battié [33] found only a modest relation of occupational risk factors and spinal degeneration.
Conclusion
Lumbar spinal stenosis is a very common condition in the elderly. In most cases it is due to degenerative changes, the changes can lead to symptoms by themselves or decompensate a preexisting narrow canal. However, it must be stressed that so-called stenotic images (sometimes severe) are present on imaging studies in a great number of symptom-free individuals, and that the relationship between degenerative lesions, importance of abnormal images, and complaints is still unclear. Lumbar stenosis is also a very common reason for decompressive surgery and/or fusion. Various conditions can lead to a narrowing of the neural pathways and differential diagnosis with vascular troubles, also common in the elderly, can be challenging. The investigation of stenotic symptoms should be extremely careful and thorough and include a choice of technical examinations including vascular investigations. This is of utmost importance, especially if a surgical sanction is considered to avoid disappointing results.
References
- 1.Adamova Eur Spine J. 2003;12:190. doi: 10.1007/s00586-002-0503-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berney Neurochirurgie. 1994;40:174. [Google Scholar]
- 3.Boden J Bone Joint Surg Am. 1990;72:403. [PubMed] [Google Scholar]
- 4.Borenstein J Bone Joint Surg Am. 2001;83:1306. doi: 10.2106/00004623-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Douglas J Bone Joint Surg Br. 1981;63:495. doi: 10.1302/0301-620X.63B4.6457839. [DOI] [PubMed] [Google Scholar]
- 6.Gagne Can J Neurol Sci. 1995;22:164. doi: 10.1017/s0317167100040257. [DOI] [PubMed] [Google Scholar]
- 7.Gill J Bone Joint Surg Am. 1955;37:493. [PubMed] [Google Scholar]
- 8.Gunzburg Eur Spine J. 2003;12:197. doi: 10.1007/s00586-002-0479-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gutwirth P (2000) Distinguishing vascular disease from lumbar spinal stenosis. In: Gunzburg R, Szpalski M (eds) Lumbar spinal stenosis. Lippicott Williams & Wilkins, Philadelphia, pp 115–124
- 10.Herno Spine. 1994;19:1975. [PubMed] [Google Scholar]
- 11.Herno Spine. 1999;24:1010. doi: 10.1097/00007632-199905150-00015. [DOI] [PubMed] [Google Scholar]
- 12.Kanis JA (1991) Pathophysiology and treatment of Paget disease of bone. Dunnitz, London
- 13.Kloc Neurol Neurochir Pol. 1998;32:699. [PubMed] [Google Scholar]
- 14.Lane Lancet. 1893;I:991. [Google Scholar]
- 15.Marcelli Spine. 1996;21:381. [Google Scholar]
- 16.Martinelli Instr Course Lect. 1992;41:179. [PubMed] [Google Scholar]
- 17.McDonald J Occup Med. 1984;26:23. [Google Scholar]
- 18.McNab J Bone Joint Surg Br. 1950;32:325. doi: 10.1302/0301-620X.32B3.325. [DOI] [PubMed] [Google Scholar]
- 19.Miller Spine. 1988;13:173. [PubMed] [Google Scholar]
- 20.Miyamoto J Bone Joint Surg Br. 1992;74:279. doi: 10.1302/0301-620X.74B2.1544970. [DOI] [PubMed] [Google Scholar]
- 21.Newman J Bone Joint Surg Br. 1963;45:39. [Google Scholar]
- 22.Porter RW (2000) Vascular compression theory. In: Gunzburg R, Szpalski M (eds) Lumbar spinal stenosis. Lippincott Williams & Wilkins, Philadelphia, pp 159–162
- 23.Porter Spine. 1992;17:9. doi: 10.1097/00007632-199209000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Postacchini Spine. 1994;19:917. doi: 10.1097/00007632-199404150-00009. [DOI] [PubMed] [Google Scholar]
- 25.Sasaki Eur Spine J. 1995;4:71. [Google Scholar]
- 26.Schmidek Clin Orthop. 1977;127:70. [PubMed] [Google Scholar]
- 27.Schonstron Clin Biomech. 1991;6:19. [Google Scholar]
- 28.Schrader Orthopade. 1993;22:223. [Google Scholar]
- 29.Schrader Eur Spine J. 1999;8:323. [Google Scholar]
- 30.Szpalski Eur Spine J. 1996;5:332. doi: 10.1007/BF00304349. [DOI] [PubMed] [Google Scholar]
- 31.Szpalski Baillieres Clin Rheumatol. 1998;12:141. doi: 10.1016/s0950-3579(98)80009-5. [DOI] [PubMed] [Google Scholar]
- 32.Verbiest J Bone Joint Surg Br. 1954;36:230. doi: 10.1302/0301-620X.36B2.230. [DOI] [PubMed] [Google Scholar]
- 33.Videman Spine. 1999;24:1164. doi: 10.1097/00007632-199906010-00020. [DOI] [PubMed] [Google Scholar]
- 34.Videman Spine. 1990;15:728. [Google Scholar]
- 35.Wiltse LL, Rothman SLG (1996) Lumbar and lumbosacral spondylolisthesis. In: Wiesel SW, Weinstein JN, Herkowitz et al (eds) The lumbar spin. Saunders, Philadelphia, pp 621–654
- 36.Wong J Westn Pac Orthopaedic Assoc. 1992;29:37. [Google Scholar]



