Abstract
The volume of blood sampled for blood culture determines its sensitivity. We measured low mean blood volumes in submitted aerobic (8.38 ± 3.88 ml) and anaerobic (7.16 ± 3.83 ml) blood culture bottles. Educational seminars were held for phlebotomy teams, and renewed measurements thereafter revealed significantly higher blood volumes in submitted aerobic (9.77 ± 4.42 ml) and anaerobic (8.30 ± 3.64 ml) bottles. Education of phlebotomy teams improves the blood volume in blood culture bottles and should be part of quality control procedures.
TEXT
The volume of blood sampled is the key determinant of the sensitivity of blood cultures (1, 2). At least two sets of blood cultures should be obtained per septic episode (1, 2); for each set, the optimum lies at 20 ml, i.e., 2 bottles of 10 ml of blood; each milliliter missed decreases the sensitivity by 3% (3). Monitoring of blood volume submitted for blood culture is thus an important quality control measure (2). Within this study, we measured blood volumes in submitted culture bottles and measured the effect of an educational seminar for the phlebotomy teams on blood volumes in culture bottles.
We used the Bactec 9000 system and its supplies (BD Biosciences, Erembodegem, Belgium). Newly submitted sets of bottles (1 Plus aerobic/F bottle and 1 Plus anaerobic/F bottle) as well as sets flagged negative after 5 days of incubation were weighed. We used one Mettler Toledo (model PB 1502-L) balance for all measurements. Unused blood culture bottles were weighted to obtain mean weights and standard deviations. Six uncapped unused aerobic blood culture bottles had a mean weight of 142.6 ± 0.5 g; six uncapped unused anaerobic blood culture bottles had a mean weight of 138.1 ± 0.7 g. We tested the vacuum of one uncapped set; the vacuum of the aerobic bottle drew in 25.6 ml of water, and that of the anaerobic bottle drew in 18.7 ml.
To measure the volume of blood in bottles, we subtracted the mean unused bottle weight from the full bottle weight. The weight difference in grams was divided by the density of blood (1.060 g/ml [4]) to measure the volume of blood in the bottle. We used a volume of 8 ml (i.e., 2 ml below the recommended volume) as the minimal norm, as previously proposed (5). All data were stored and analyzed using SPSS version 18.0 (IBM).
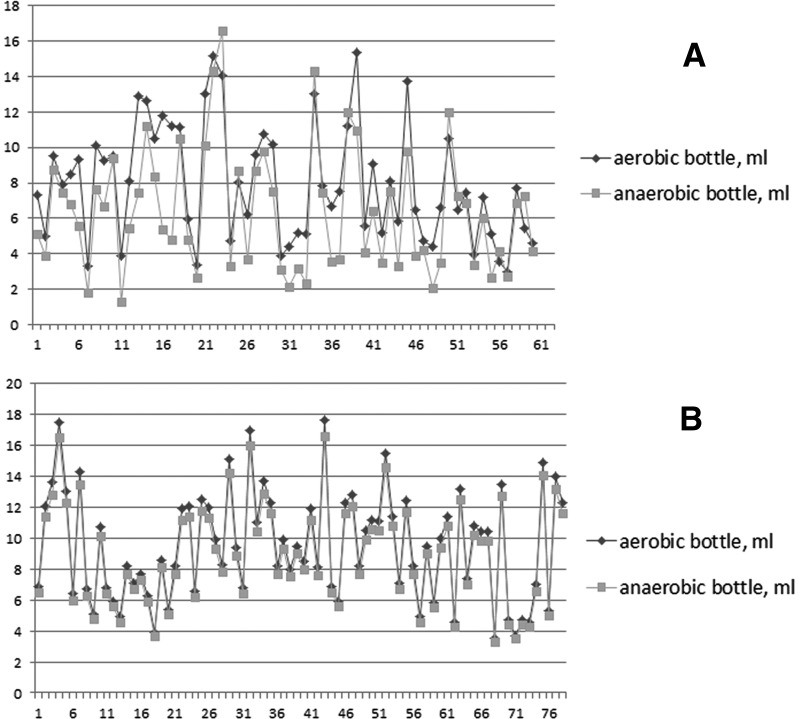
In experiment 1, we weighed a total of 150 sets of two bottles: 90 sets labeled negative and 60 sets of newly submitted bottles; the results are given in Table 1. Forty-nine percent (74/150) of the aerobic and 61% (92/150) of the anaerobic bottles had a low volume of blood (<8 ml). Within sets, volumes in aerobic and anaerobic bottles were related, i.e., if the blood volume in the aerobic bottle was low, the volume in the anaerobic bottle was also low (Fig. 1A). This internal consistency of volumes within sets implies an important role of the phlebotomist in the volume of blood inserted into the bottles.
Table 1.
Mean blood volume in bottles submitted for blood culture
| Bottle type | Before seminars |
After seminars |
Significance level (P)a | ||
|---|---|---|---|---|---|
| Mean blood vol (ml) | % of bottles with blood vol of <8 ml | Mean blood vol (ml) | % of bottles with blood vol of <8 ml | ||
| Aerobic | 8.38 ± 3.88 | 49 | 9.77 ± 4.42 | 36 | 0.004 |
| Anaerobic | 7.16 ± 3.83 | 61 | 8.30 ± 3.64 | 54 | 0.008 |
Calculated using Student's t test, comparing mean blood volumes before and after seminars. Equal variance of the measurements could be assumed based on P values of >0.05 in Levene's test.
Fig 1.
Blood volumes in newly submitted blood culture bottles, experiments 1 (A) and 2 (B). The x axes show the bottle numbers; the y axes show the blood volume in milliliters.
An educational seminar was set up for all phlebotomy team members involved in blood sampling for blood culture in our hospital, which summarized the studies on the associations between blood volume sampled and sensitivity of blood culture (reviewed in references 1 to 3), as well as the results of experiment 1. Three educational sessions were held at the two hospital locations within a 1-week time frame, to ensure that all staff would be able to attend. In experiment 2, 1 week after the educational seminars, another 157 sets (78 newly submitted sets and 79 sets labeled negative after 5 days of incubation) were weighed using the same methodology. In these sets, the percentage of bottles with low blood volume decreased to 36% (57/157 aerobic bottles) and 54% (84/157 anaerobic bottles) (Table 1), respectively. The mean blood volume in the bottles was significantly increased (Table 1). We observed similar internal consistency in volumes of aerobic and anaerobic bottles in the 78 newly submitted sets of experiment 2 (Fig. 1B).
Education of the phlebotomy team improved the blood volume in bottles submitted for blood culture, which reconfirms the importance of monitoring these volumes as part of laboratory quality control programs. The 49 to 61% of bottles with low blood volume observed in experiment 1 are higher than figures from previous studies, where rates of 20% (3), 26 to 36% (5), and 40% (6) have been reported. The educational seminars restored this rate to within these previously published ranges, at least for the aerobic bottles (Table 1).
The higher frequency of low volumes in the anaerobic bottles than in the aerobic bottles remains unexplained. As aerobic bottles are usually filled first, this may represent an effect of occlusion of the punctured vein, after prolonged exposure to the negative pressure induced by the vacuum of the aerobic and later anaerobic bottle. Alternatively, it could be a result of the milder vacuum in anaerobic bottles than in aerobic bottles, although we have not tested this in large series of bottles. This is an issue that warrants specific attention by phlebotomists and may even warrant two separate phlebotomies in selected patients.
The decreased sensitivity associated with inadequate sample volumes is not the only reason to routinely measure sample volumes and continuously instruct phlebotomy teams. In previous studies, samples with inadequate blood volume were also more prone to yield growth of contaminants, although the cause of this phenomenon could not be established. It has been hypothesized that the ratio of contaminating bacterial load to blood volume provided sufficient contaminant concentrations to grow and yield a positive result within the routine incubation period (6, 7).
The effect of a single series of educational seminars was positive, but the long-term effects were not measured in the current study. This effect is likely to diminish over time. Hence, such educational activities, as well as the monitoring of their effect on sample volume, should have a recurrent rather than incidental character (2).
In conclusion, education of phlebotomy teams can help to improve the volume of blood in blood culture bottles and thus aid to optimize the sensitivity of blood culture. These educational activities should be a continuous part of laboratory quality control procedures.
Footnotes
Published ahead of print 26 December 2012
REFERENCES
- 1. Reimer LG, Wilson ML, Weinstein MP. 1997. Update on detection of bacteremia and fungemia. Clin. Microbiol. Rev. 10:444–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baron EJ, Weinstein MP, Dunne WM, Jr, Yagupsky P, Welch DF, Wilson DM. 2005. Cumitech 1C, blood cultures IV, p 1–16, 23–25 Coordinating ed, Baron EJ. ASM Press, Washington, DC [Google Scholar]
- 3. Mermel LA, Maki DG. 1993. Detection of bacteremia in adults: consequences of culturing an inadequate volume of blood. Ann. Intern. Med. 119:270–272 [DOI] [PubMed] [Google Scholar]
- 4. Cutnell J, Johnson K. 1998. Physics, 4th ed, p 308 Wiley Interscience, Hoboken, NJ [Google Scholar]
- 5. Willems E, Smismans A, Cartuyvels R, Coppens G, Van Vaerenbergh K, Van den Abeele AM, Frans J, Bilulu Study Group 2012. The preanalytical optimization of blood cultures: a review and the clinical importance of benchmarking in 5 Belgian hospitals. Diagn. Microbiol. Infect. Dis. 73:1–8 [DOI] [PubMed] [Google Scholar]
- 6. Gonsalves WI, Cornish N, Moore M, Chen A, Varman M. 2009. Effects of volume and site of blood draw on blood culture results. J. Clin. Microbiol. 47:3482–3485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bekeris L, Tworek J, Walsh M, Valenstein P. 2005. Trends in blood culture contamination: a College of American Pathologists Q-Tracks study of 356 institutions. Arch. Pathol. Lab. Med. 129:1222–1225 [DOI] [PubMed] [Google Scholar]