Abstract
A species-specific molecular beacon real-time PCR assay was developed for rapid diagnosis of Exserohilum rostratum infection. As low as 100 fg of E. rostratum DNA can be reliably detected in the presence of 50 ng of human DNA, with a dynamic linear quantification range from 20 ng to 200 fg.
TEXT
Adeadly outbreak of fungal meningitis associated with injections of contaminated methylprednisolone is ongoing in the United States (1). The major cause of this iatrogenic meningitis is Exserohilum rostratum, a plant pathogen that rarely causes human disease. This fungus has been identified from patient tissue and cerebrospinal fluid (CSF) samples, as well as unopened vials of the implicated lots of methylprednisolone, by culture or DNA sequencing, followed by a PCR assay (1–4). However, cultures from clinical samples, especially CSF, often appear negative due to the paucity of free-floating organisms. There is a need to develop a highly sensitive rapid nucleic acid-based test that can be used to reliably and quantitatively identify Exserohilum rostratum from a variety of patient specimens. Moreover, there is no reliable quantitative biomarker in CSF by which one can measure a reduction of tissue burden of E. rostratum in response to antifungal therapy. Here, we describe a specific, sensitive, and quantitative real-time PCR assay using molecular beacon (MB) technology to detect and quantify E. rostratum that facilitates primary diagnosis in the ongoing outbreak investigation, that may be used for monitoring of therapeutic response in infected patients, and that can aid in in-depth animal model studies of this poorly studied fungal pathogen.
Seven clinical isolates of E. rostratum (Table 1) were grown on potato dextrose agar (PDA) slants and incubated at 37°C for 5 days. A small piece (≈1 cm2) of mycelium mat was scraped off the slant and subjected to DNA extraction using the MasterPure yeast DNA purification kit (Epicentre Biotechnologies, Madison, WI) with modifications of adding an extra mechanical lysis as well as a proteinase K lysing step to the cell lysis solution treatment. Briefly, the mycelium was dispersed in 500 μl of yeast cell lysis solution and processed on a FastPrep instrument (MP Biomedicals Inc., Solon, OH) in lysing matrix tubes (MP Biomedicals Inc.), after which proteinase K (500 μg/ml) was added and cell lysates were incubated at 65°C for 45 min, followed by a 10-min centrifugation at 16,000 × g. The supernatant was then processed until the final elution according to the manual of the extraction kit. The final elution volume was 50 μl.
Table 1.
Exserohilum rostratum clinical isolates used in this study
| UTHSC accession no. | Institution | Source |
|---|---|---|
| 12-2725 | John Hopkins Hospital | Tissue |
| 12-2786 | John Hopkins Hospital | CSF |
| 12-2809 | St. Thomas Hospital | CSF |
| 12-2810 | St. Thomas Hospital | CSF |
| 12-2838 | St. Thomas Hospital | Anterior brain |
| 12-2839 | St. Thomas Hospital | CSF |
| 12-2840 | St. Thomas Hospital | CSF |
For the design of a species-specific real-time PCR assay, available internal transcribed spacer (ITS) region sequences for E. rostratum and closely related species (Exserohilum longirostratum, Exserohilum mcginnisii, and Exserohilum gedarefense) and genera (Bipolaris and Drechslera) were searched for in GenBank, and alignments were created using ClustalW2 (http://www.ebi.ac.uk/Tools/msa/clustalw2/). A molecular beacon probe targeting the ITS1 region was designed according to guidelines described at http://www.molecular-beacons.org and obtained from Biosearch Technologies (Novato, CA). The MB probe (5′-CGTCGACAGCGTCCGCCCCAAGTATTTTCGACG-3′; the underlined nucleotides comprise the target sequence, which forms the molecular beacon's loop, and the sequences at both ends without underlining are artificial and form the molecular beacon's stem) was labeled with fluorescein (FAM) fluorophore at the 5′ end and 4-(4′-dimethylaminophenylazo) benzoic acid (DABCYL) quencher at the 3′ end. Oligonucleotide primers (ITS1-F, 5′-CGTAGGTGAACCTGCGGAGGGATC-3′; ITS1-R, 5′-ATTATTATACTGACGCTGATTGC-3′) were designed using the online software Primer3 (http://frodo.wi.mit.edu/) and obtained from Integrated DNA Technologies (Coralville, IA). A BLAST search (http://www.ncbi.nlm.nih.gov/BLAST/) was performed to check the specificity of the DNA sequences of the primers and probe.
An internal amplification control (IAC) was incorporated into this assay to determine the presence of PCR inhibitors. The IAC template was a 200-nucleotide (nt) single-stranded DNA (ssDNA) fragment of potato leafroll virus coat protein gene (GenBank accession no. FJ859026) synthesized by IDT (Coralville, IA). The amplicon was detected with a forward primer (5′-CTTATGAGTTGGACCCCCATT-3′), a reverse primer (5′-CATTCTACCCCGTTTATCATCC-3′), and an MB probe (5′-CGACGTCCCTCCAGTCCTACGTCAACACGTCG-3′) labeled with CAL Fluor Red 610 fluorophore and black hole quencher 2 (BHQ2) (Biosearch).
The real-time PCR was performed in a 25-μl reaction mixture consisting of 12.5 μl of Premix Ex Taq (2×) (Perfect Real Time; TaKaRa Bio Inc., Mountain View, CA), 0.2 μM each E. rostratum primer, 0.1 μM E. rostratum MB, 0.15 μM each IAC primer, 75 nM IAC MB, 4,000 copies of the IAC template, 2 μl of DNA, and 0.5 μl of ROX dye II on an Mx3005P real-time instrument (Stratagene, La Jolla, CA). Optimal thermal cycling conditions included an initial denaturation step at 95°C for 5 min, followed by 45 cycles of 95°C for 20 s (denaturation), 53°C for 30 s (annealing), and 72°C for 30 s (extension). The analytical specificity was first checked in silico by BLAST, as described above, and then evaluated by testing DNAs from all 7 E. rostratum clinical isolates and other fungal pathogens (Aspergillus fumigatus, Fusarium spp., Candida albicans), as well as human genomic DNA. The analytical sensitivity was evaluated by testing triplicates of serially diluted genomic DNA from the E. rostratum isolate UTHSC 12-2725, ranging from 20 ng to 50 fg per PCR. The above-described assays were repeated twice on two separate days to assess the reproducibility and interday assay variation. To determine the impact of human DNA background in clinical samples on the assay's performance, 50 ng of human genomic DNA was spiked in each E. rostratum DNA dilution to proceed with real-time PCR.
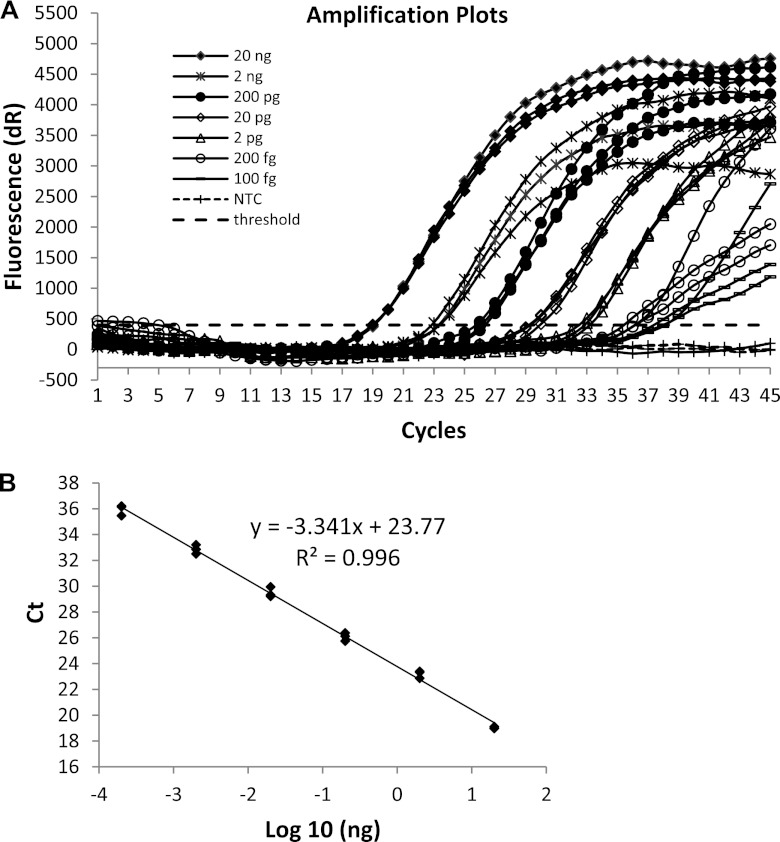
BLAST results showed that this novel probe is highly specific for E. rostratum, although it also has a perfect match with ITS1 sequences from three closely related species, E. longirostratum, E. mcginnisii, and E. gedarefense, as well as two Alternaria strains which are most likely misidentified by the depositors (5). As E. gedarefense is not a human pathogen and previous taxonomic and molecular studies suggested that E. rostratum, E. longirostratum, and E. mcginnisii are probable conspecific species (6–8), such potential cross-reactions do not diminish the specificity of this assay. In fact, all 7 clinical isolates were successfully detected by this assay with robust signals, while tests against the same amount of DNA from human and other fungal species included in this study remained negative. The assay reliably detected as little as 100 fg of genomic DNA of E. rostratum in all 6 replicates tested, and 50 fg of DNA was detected in 3 of 6 replicates. The best linear quantification range was over 6 logs from 200 fg to 20 ng per PCR, with an R2 (goodness-of-fit) value of 0.996 (Fig. 1). The amplification efficiency was 99.2%. The IAC was consistently positive from the no-template control to reaction mixtures containing 20 ng of E. rostratum DNA, with a mean threshold cycle (CT) value of 37.03 ± 0.84. The linear dynamic range was not changed by spiking 50 ng of human DNA in the PCR, as the CT values were almost identical to those achieved from pure E. rostratum DNA at each comparable level within the range. Although the large amount of human DNA slightly shifted the lowest detectable level from 50 fg to 100 fg (100% detection rate) and resulted in a delayed IAC CT value of 39.18 ± 1.17, it did not compromise linear quantification of the assay under such circumstances. These results demonstrated that very small quantities of E. rostratum DNA can be detected in a background of large amounts of human DNA (5 × 105-fold excess DNA by mass) using this assay, indicating great potential of using this assay on clinical samples, especially human tissues or biopsy specimens, for rapid diagnosis. The ability to detect a wide dynamic quantitative range of E. rostratum genomic DNA in the presence of human DNA would also enable this assay to be utilized for therapeutic monitoring in serial CSF samples of patients receiving antifungal therapy.
Fig 1.
Analytical sensitivity test (A) and linear quantification of E. rostratum in a real-time PCR (B). NTC, no-template control.
This highly sensitive assay is robust and has the potential to be used on diverse clinical samples. An important challenge for any nucleic acid-based molecular assay is the sensitive detection of low fungal burdens in infected patients. In many cases, it is inefficient extraction of total nucleic acids and reduction of signal due to the relatively large amount of human DNA compared to target fungal DNA present in the extracts (9). To avoid such downstream problems, we have utilized a molecular diagnostic approach of extraction and detection that was previously employed to assess small amounts of fungal nucleic acid from various primary samples (lung tissue, bronchoalveolar lavage fluid, plasma, whole blood, etc) in experimental animals or patients infected with Aspergillus spp. (10, 11). Thus, the current assay holds promise for successful application on animal and/or clinical samples, such as CSF and brain tissues.
To our knowledge, this is the first reported real-time PCR assay for rapid detection and quantification of Exserohilum rostratum meningitis. We believe that this assay will be an important and timely contribution to meeting the challenges of this public health threat for detection and therapeutic monitoring of infected patients.
Being aware of the low positivity of culture isolation from clinical samples and the ongoing microbiological testing of unopened vials of the implicated glucocorticosteroids, as well as additional products from the same manufacturer or suppliers, this rapid, specific, and quantitative real-time PCR assay can facilitate clinical diagnosis, therapeutic monitoring, and parallel nonclinical laboratory investigations. Further evaluation of the assay's performance on CSF samples from the outbreak patients and animal models is urgently needed to fulfill this task.
Footnotes
Published ahead of print 9 January 2013
REFERENCES
- 1. Centers for Disease Control and Prevention 2012. Multistate outbreak of fungal infection associated with injection of methylprednisolone acetate solution from a single compounding pharmacy—United States, 2012. MMWR Morb. Mortal. Wkly. Rep. 61:839–842 [PubMed] [Google Scholar]
- 2. Kauffman CA, Pappas PG, Patterson TF. 2012. Fungal infections associated with contaminated methylprednisolone injections—preliminary report. N. Engl. J. Med. doi:10.1056/NEJMoa1213978 [DOI] [PubMed] [Google Scholar]
- 3. Levitz SM. 2012. Compounding drugs contaminated with fungi: a recipe for disaster. Emerg. Microbes Infect. 1:e41 doi:10.1038/emi.2012.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wilson LE, Blythe D, Sharfstein JM. 2012. Fungal meningitis from injection of contaminated steroids: a compounding problem. JAMA 308:2461–2462 [DOI] [PubMed] [Google Scholar]
- 5. Brunings AM, Datnoff LE, Palmateer AJ, Locke JC, Krause CR. 2009. Exserohilum leaf spot on tiger grass. Plant Health Prog. doi:10.1094/PHP-2009-1215-01-RS. http://www.ars.usda.gov/SP2UserFiles/Place/36071000/GPRG/2009PublicationsandSummaries/ExserohiliumLeafSpotOnTigerGrass[Article].pdf [Google Scholar]
- 6. da Cunha KC, Sutton DA, Gene J, Capilla J, Cano J, Guarro J. 2012. Molecular identification and in vitro response to antifungal drugs of clinical isolates of Exserohilum. Antimicrob. Agents Chemother. 56:4951–4954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Hoog GS, Cuarro GJ, Figueras MJ. (ed). 2000. Atlas of clinical fungi, 2nd ed ASM Press, Washington, DC [Google Scholar]
- 8. Lau A, Chen S, Sorrell T, Carter D, Malik R, Martin P, Halliday C. 2007. Development and clinical application of a panfungal PCR assay to detect and identify fungal DNA in tissue specimens. J. Clin. Microbiol. 45:380–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khot PD, Fredricks DN. 2009. PCR-based diagnosis of human fungal infections. Expert Rev. Anti Infect. Ther. 7:1201–1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Denning DW, Park S, Lass-Florl C, Fraczek MG, Kirwan M, Gore R, Smith J, Bueid A, Moore CB, Bowyer P, Perlin DS. 2011. High-frequency triazole resistance found in nonculturable Aspergillus fumigatus from lungs of patients with chronic fungal disease. Clin. Infect. Dis. 52:1123–1129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhao Y, Park S, Warn P, Shrief R, Harrison E, Perlin DS. 2010. Detection of Aspergillus fumigatus in a rat model of invasive pulmonary aspergillosis by real-time nucleic acid sequence-based amplification. J. Clin. Microbiol. 48:1378–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]