Abstract
There are various electrical, mechanical and chemical methods used to achieve haemostasis in spine surgery. Chemical haemostatic agents are often preferable to bipolar cautery in intraspinal procedures, because these products control bleeding without occluding the vessel lumen and cause no thermal injuries to adjacent structures. A topical haemostat is the often the technique of choice to control bleeding from bone and to diffuse capillary and epidural venous oozing. This paper focuses on technical aspects of the application of absorbable porcine gelatine and regenerated, oxidised cellulose. These haemostats have been used in neurosurgical intraspinal procedures for more than 30 years; however, new application forms like Surgicel fibrillar and Surgifoam powder imply different handling options, which are discussed in this paper.
Keywords: Haemostats, Spine, Absorbable porcine gelatine, Regenerated oxidised cellulose, Intraspinal surgery
Introduction
Achieving haemostasis during surgical procedures within the spinal canal is of paramount importance. Whereas bleeding of up to one litre may be tolerated within structures such as the abdominal cavity, bleeding of only a few millilitres within the spinal canal may cause devastating neurological damage. In addition, microsurgical approaches to intraspinal structures depend on clear visualisation of the most delicate structures: continuous bleeding may impede identification of eloquent and/or pathological structures. Mechanical methods of haemostasis such as direct pressure and ligature are not applicable in intraspinal surgery because of the depth at which the surgery is performed and the indispensability of structures. For most of this century, the mainstay of controlling intraspinal bleeding has been bipolar cautery, allowing precise coagulation of small vessels, and, compared to monopolar cautery, minimizing the dangerous spread of current to adjacent tissue. Intraspinal, intradural and intramedullary bipolar cautery, however, has severe drawbacks. The complete occlusion of the vessel lumen may compromise the perfusion of the neural tissue supplied by the cauterized vessel. In addition, dissipation of heat from the tips of the bipolar forceps may induce thermal injury to adjacent vascular and neural structures. Though bipolar cautery is most effectively used to occlude identifiable vessels, it has minimal efficacy in controlling the diffuse capillary bleeding that characterises most intraspinal pathologies. For these reasons chemical haemostatic agents are often preferable to bipolar cautery in intraspinal procedures. These products can control bleeding without occluding the vessel lumen and cause no thermal injuries to adjacent structures. When applied topically, these agents can effectively control diffuse capillary oozing.
General remarks
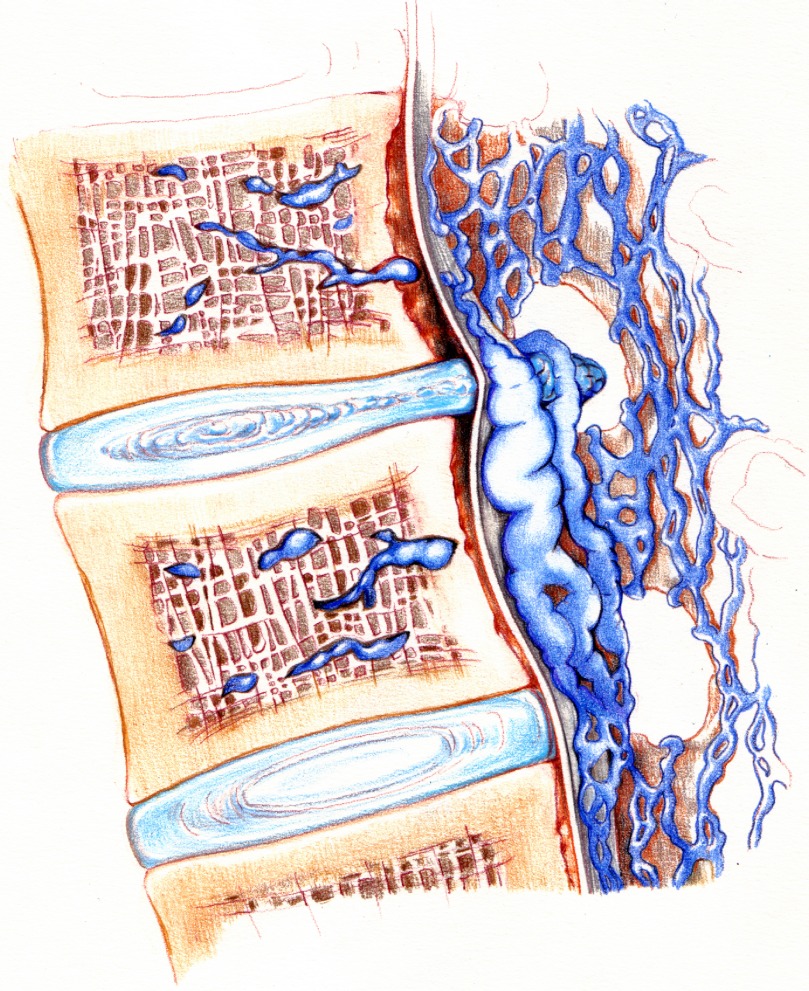
In the majority of intraspinal, extradural procedures, bleeding is caused by venous vessels. This low-pressure bleeding will eventually stop when the patient is repositioned in the supine position and the intraspinal counter-pressure exceeds the intravenous pressure. However, due to venous compression, dilated varicose intraspinal veins may be a source of continuous bleeding, thereby impeding visualisation of eloquent structures and causing severe blood loss (Fig. 1). A topical haemostat is the technique of choice as an adjunct to diathermy, to bone wax placed on bleeding bone and to the conventional clamping and tying of bleeders. Arterial bleeding, which is usually not manageable with application of haemostats, is only rarely encountered during most intraspinal extradural procedures.
Fig. 1.
Artist’s rendition of the most common cause for troublesome bleeding during microsurgical intraspinal procedures. Mass effect of disc protrusion causes venous compression, which leads to dilated varicose intraspinal veins. These veins are the source of continuous bleeding, impeding visualisation of eloquent structures and can even cause severe blood loss
This paper will focus on the application of absorbable porcine gelatine and regenerated oxidised cellulose. The favourable chemical properties of these haemostats have been reviewed elsewhere [2].
Given the plethora of a complicated intraoperative situation, we will discuss the most commonly encountered indications for haemostats during a standard intraspinal procedure: bleeding from bone and epidural venous oozing.
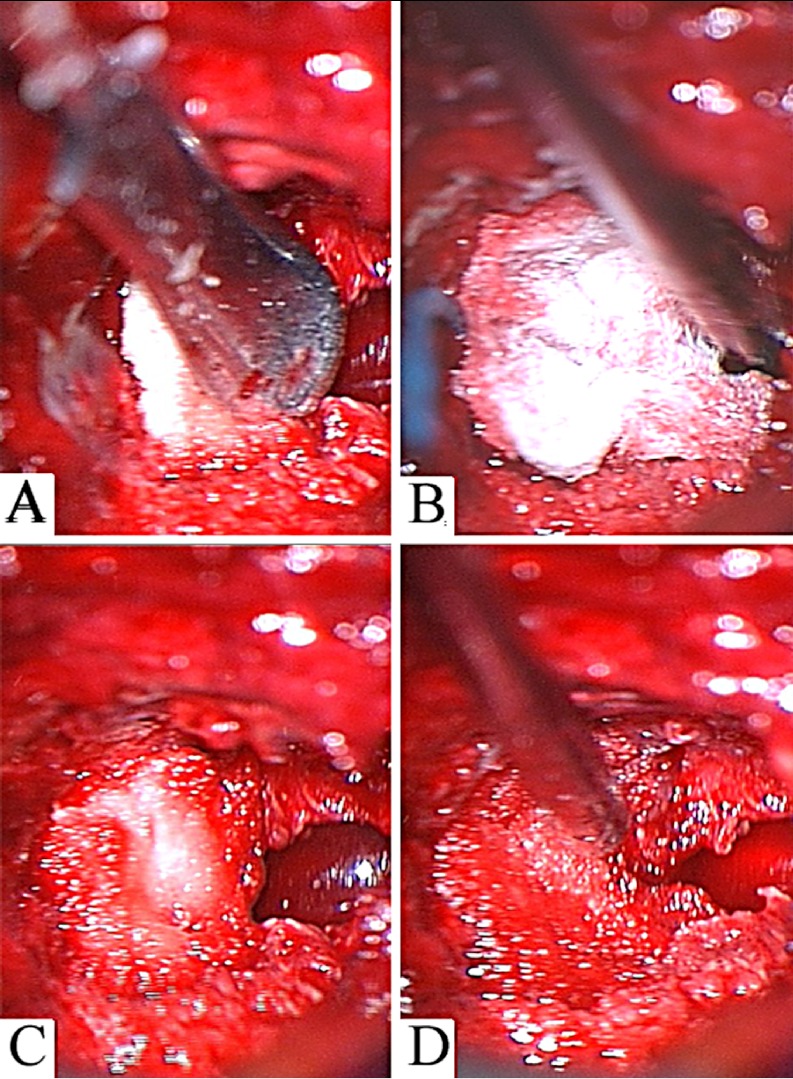
Bone
Most intraspinal procedures involve a more or less extensive removal of bone. As bone is chipped away, the remaining bone and tissue tends to ooze. Bone wax is commonly used to stop bleeding from oozing bone. Though widely used, bone wax has some disadvantages. Because of its consistency it is often difficult to mold wax to the contours of the bleeding areas using a dissector. Recently, Surgifoam powder (absorbable porcine gelatine, also: Spongostan powder) has been introduced into the European market. This haemostat forms a paste that can be spread or shaped to conform to irregular surfaces to stop bleeding fast. In contrast to bone wax, Surgifoam powder is easily moulded on the irregular surfaces of chipped bone. We prefer to apply a pea-sized portion of Surgifoam powder on the oozing surface and mould it into the bone after covering it with wet cottonoid patties (Fig. 2). Bleeding will stop almost immediately. Residual Surgifoam powder may be removed by topical suction or irrigation.
Fig. 2.
A Application of Surgifoam powder to control bleeding from oozing bone after partial laminectomy; B Surgifoam powder is easily applied on the oozing surface using a dissector and molded into the bone after covering it with wet cottonoid patty; C bleeding will stop almost immediately; D residual Surgifoam powder may be removed by topical suction or irrigation
Epidural oozing
Dissection of the dura from the lamina causes epidural venous oozing (Fig. 1). This can be a particular nuisance since many of the intraspinal approaches are typically performed through small incisions or under a microscope and even a small amount of oozing can obstruct the surgeon’s view. The use of bipolar cautery is limited, since dissipation of heat from the tips of the bipolar forceps may induce thermal injury to adjacent nerve roots or neural structures. Though commonly used, the application of absorbable gelatine sponges in this setting has severe drawbacks. Blood-soaked gelatine tends to stick to surgical instruments. Furthermore, gelatine sponges don’t form a tight bond with the source of bleeding and are, therefore, very easily dislodged. The introduction of regenerated oxidised cellulose (Surgicel) offers superior handling characteristics as compared to gelatine sponges. It is supplied as a knitted strip that can be easily trimmed to any size. Cut into small pieces, Surgicel conforms well to shapes, is easily manipulated and does not stick to instruments. The best way to prevent dislodgement by the suction device is to place a cottonoid patty on the Surgicel strip, thus enabling the surgeon to manoeuvre the haemostat, with the tip of the suction device, into the final position (Fig. 3). Surgicel fibrillar is supplied as a layered, three-dimensional wafer with a consistency resembling cotton. Since the layers are peeled off in the desired amount, controlled placement of custom-sized pieces is facilitated. In contrast to gelatin sponges, Surgicel fibrillar remains pliable and can be reshaped within the wound. If necessary and safe, bipolar cautery can additionally be directly applied to the fibrillar surface to produce more effective haemostasis. Interestingly, Surgicel fibrillar allows for a direct application of suction, obviating the need for the overlying cottonoid patty (Fig. 4). This is most comfortable for microneurosurgical, intraspinal procedures in which the rather bulky cottonoid patty significantly obscures the surgeon’s view. Similar to the application of gelatine sponges, Surgicel can swell and should be removed from the site of application, when haemostasis is achieved.
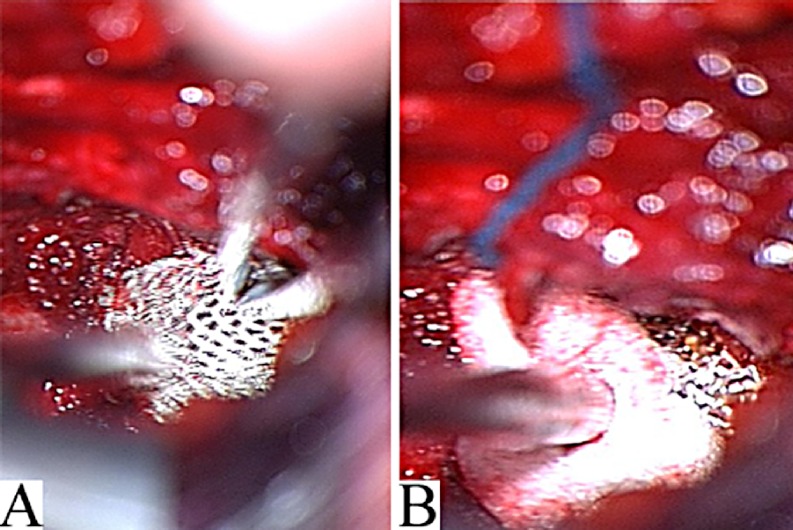
Fig. 3 A.
A small piece of Surgicel is shaped on the bleeding surface by bipolar forceps and suction device; B dislodgement by the suction device is best prevented by placing a cottonoid patty on the Surgicelstrip and manoeuvring the haemostat into the desired position
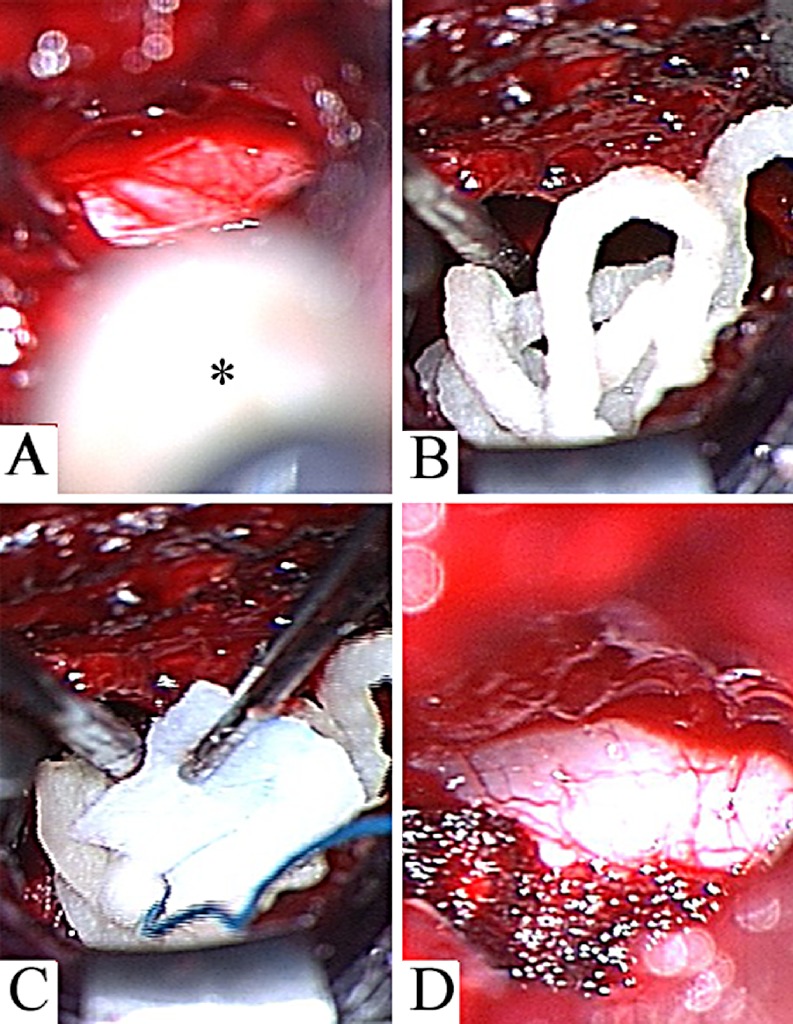
Fig. 4 A.
During microsurgical nerve-root decompression, severe venous oozing may be encountered; B a custom-sized piece of Surgicel fibrillar is placed on the nerve root; C after irrigation Surgicel fibrillar remains pliable and can be reshaped within the wound, allowing a direct application of suction; D this obviates the need for the overlying cottonoid patty
The consistency of Surgifoam powder enables the surgeon to spread this haemostat into the contours of the bleeding surface, even using a syringe (Fig. 5). To achieve quick and effective haemostasis, the bleeding surface is covered with Surgifoam powder. A cottonoid patty is used to mold the powder gently into the bleeding surface. An outstanding feature of Surgifoam powder is that the paste which covers the target structures can be easily removed using the suction device, enabling the surgeon to proceed, while leaving the residual haemostat in position (Fig. 5).
Fig. 5 A.
Example of intraspinal application of Surgifoam powder using a syringe*; B and C a cottonoid patty is used to mold the paste gently into the bleeding surface; D Surgifoam powder is easily removed using the suction device, revealing the target structures while haemostasis is achieved
Discussion
For decades absorbable porcine gelatine and regenerated oxidised cellulose have been used in intraspinal surgery. The superior handling characteristics of both haemostats make them most effective for the control of bleeding during microsurgical procedures. In our opinion they should be used primarily when bipolar cautery is either ineffective or dangerous. There are, however, complications associated with the intraspinal application of haemostats.
There are several reports of paraplegia after thoracic surgery during which oxidised cellulose had been used during thoracotomy for haemorrhage control and was later found to have passed through the intervertebral foramen, causing spinal cord compression [3, 5]. It is therefore recommended, that in all intraspinal and perispinal procedures, over-liberal use of Surgicel should be avoided, and attempts should be made to remove all excess Surgicel once adequate haemostasis is obtained. Similar to the complications associated with the use of oxidised cellulose, there are several reports of severe neurological deficits due to the intraspinal application of absorbable gelatin sponges [1, 4, 6]. If gelatine sponges are not handled properly, they can engorge, thus causing a mass effect. Therefore, care must be taken to avoid placing a large mass of sponge in a closed space, such as the spinal canal. Though Surgifoam powder consists of absorbable gelatine, its technical properties make it unlikely to cause mass effects. However, residual Surgifoam powder should be removed by topical suction or irrigation.
Although topical haemostats are widely used, there are only a few reports on the postoperative CT or MR characteristics of these products. In fact, oxidised cellulose granulomata may mimic tumour recurrence [9] or postoperative abscess [7, 10] on both CT and sonography when a patient undergoes imaging early in the postoperative period [11]. Oto described the appearance of oxidised, regenerated cellulose on postoperative MR imaging with a short relaxation time on T2-weighted images, resulting in low signal intensity in the early postoperative period. The author concluded that MR imaging may be helpful in differentiating Surgicel from an abscess and, therefore, in preventing unnecessary attempts at re-operation [8].
Conclusions
Despite these complications, the use of absorbable porcine gelatine and regenerated, oxidised cellulose as haemostats in intraspinal surgery must be considered safe and beneficial. However, the appropriate use of haemostats requires a certain understanding of their advantages, limitations and the nature of complications associated with their application.
References
- 1.Alander Spine. 1995;20:970. doi: 10.1097/00007632-199504150-00016. [DOI] [PubMed] [Google Scholar]
- 2.Arand Neurosurgery. 1986;18:223. doi: 10.1227/00006123-198602000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Banerjee South Med J. 1998;91:481. doi: 10.1097/00007611-199805000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Bellen Acta Orthop Belg. 1992;58:236. [PubMed] [Google Scholar]
- 5.Brodbelt Ann R Coll Surg Engl. 2002;84:97. [PMC free article] [PubMed] [Google Scholar]
- 6.Friedman Spine. 2001;26:E485. doi: 10.1097/00007632-200110150-00029. [DOI] [PubMed] [Google Scholar]
- 7.Ibrahim Eur J Cardiothorac Surg. 2002;22:489. doi: 10.1016/S1010-7940(02)00328-7. [DOI] [PubMed] [Google Scholar]
- 8.Oto AJR Am J Roentgenol. 1999;172:1481. doi: 10.2214/ajr.172.6.10350276. [DOI] [PubMed] [Google Scholar]
- 9.Sandhu Br J Neurosurg. 1996;10:617. doi: 10.1080/02688699646989. [DOI] [PubMed] [Google Scholar]
- 10.Turley Abdom Imaging. 1994;19:345. doi: 10.1007/BF00198195. [DOI] [PubMed] [Google Scholar]
- 11.Young AJR Am J Roentgenol. 1993;160:275. doi: 10.2214/ajr.160.2.8424333. [DOI] [PubMed] [Google Scholar]