Abstract
Current research literature on toilet training for children with autism or developmental delays focuses on smaller case studies, typically with concentrated clinical support. Limited research exists to support an effective school-based program to teach toileting skills implemented by public school staff. We describe an intervention program to toilet train 5 children with autism or developmental delays who demonstrated no prior success in the home or school setting. Intervention focused on (a) removal of diapers during school hours, (b) scheduled time intervals for bathroom visits, (c) a maximum of 3 min sitting on the toilet, (d) reinforcers delivered immediately contingent on urination in the toilet, and (e) gradually increased time intervals between bathroom visits as each participant met mastery during the preceding, shorter time interval. The program was effective across all 5 cases in a community-based elementary school. Paraprofessional staff implemented the program with minimal clinical oversight.
Keywords: autism, paraprofessional staff, school setting, toilet training

Skill deficits in the areas of self-help may be a significant hurdle for people diagnosed with autism and other developmental disabilities. Indeed, toilet training for children with developmental disabilities was (Konarski & Diorio, 1985) and continues to be one of the most frequently researched self-help skills. Blum, Taubman, and Nemeth (2004) defined effective daytime toilet training as when a child has less than four wetting accidents per week. For the vast majority of typically developing children in the United States, 98%, meet this criterion by their third birthday (Blum, Taubman, & Nemeth, 2003).
The field of applied behavior analysis provides an ample body of literature that spans over four decades and describes effective toilet training programs in applied settings. Early models (e.g., Azrin & Foxx, 1974; Van Wagenen, Meyerson, Kerr, & Mahoney, 1969) relied on intense yet short periods of intervention coupled with direct clinical support to maximize learning. A seminal article written by Azrin and Foxx remains a staple in current practice for toilet training; more recent literature follows the underpinnings of their findings though points toward less focus on the concept of rapid training and instead concentrates on a durable life skill readily implemented in nonclinical settings (Cicero & Pfadt, 2002; Kroeger & Sorensen-Burnworth, 2009; Kroeger & Sorensen, 2010; LeBlanc, Carr, Crossett, Bennett, & Detweiler, 2005; Stadtler, Gorsky, & Brazelton, 1999).
Since the inception of The Individuals with Disabilities Education Act, 2004 (IDEA; U.S. Department of Education, 2004), school districts are required to teach skills that are beyond the scope of straightforward academic goals; a focus on and accountability for functional life skills is a requirement as well. Education of children who require specialized services needs to address broad issues of learning including adaptive skills that support inclusion (Bryson, Rogers, & Fambonne, 2003).
Even with the vast body of information available regarding toilet training, there are few studies that deal directly with the issue of toilet training in school settings (see Luiselli, 1997) and even fewer that remove direct, ongoing clinical support during training. This study evaluated a public school-based toilet training procedure implemented by paraprofessional staff with minimal clinical support. The goal of the study was to explore the effectiveness of a formal toileting procedure to increase continent voids as well as bladder control for expanded periods of time in a public school program with minimal clinical oversight. The procedure included multiple components, including the following: removal of diapers during school hours, a scheduled time interval for bathroom visits, a maximum of 3 min sitting on the toilet at each visit, positive reinforcement of urination in the toilet, and gradually increasing time intervals for bathroom visits as each student progressed through training.
Method
Participants and Settings
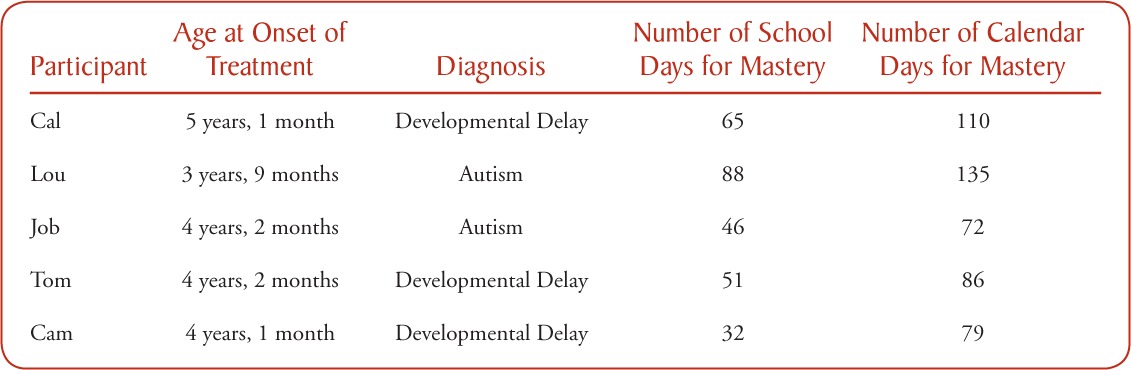
Participants were 5 boys ranging in age from 3 to 5 years old and were diagnosed with either autism or a developmental delay (see Table). None of the participants demonstrated urinary continence, even though parents reported at least one attempt to teach toileting skills at home, and the school also attempted to toilet train the participants. All 5 participants were assigned to the same preschool classroom, intended to deliver services to children identified with autism or developmental delays.
Table.
Age, Diagnosis, and Length of Treatment for Each Participant
All participants were enrolled in a preschool setting in Connecticut and had active individualized educational plans (IEPs) in place. Their school day consisted of direct instruction as well as inclusionary time with peers, based on each participant's ability and individual needs. The classroom had an assigned special education teacher, and each participant had 1:1 support throughout the day. The 1:1 staff held at least an associate's degree and received ongoing training and oversight from a Board Certified Behavior Analyst (BCBA). The participants attended school 5 days per week, 6 hours per day.
The toilet training program occurred in the same preschool classroom for each child. The classroom provided a small area for discrete trial instruction, a play area, an area for morning circle, and a snack area. A bathroom adjoining the classroom had a small toilet designed for preschool-aged children, allowing for a smooth transition from the classroom into the bathroom throughout the day.
Response Definition and Measurement
The dependent variable (DV) was the percentage of correct urinations in the toilet. Correct urination for the purpose of this study was defined as the release of urine while seated on the toilet. The independent variable was the school-based toilet training program. Assigned 1:1 staff were responsible for all data collection. Data were generated by recording each child's urinary status throughout the day. A monthly scatter plot was provided, which was separated into 30-min increments each day (go to http://www.abainternational.org/Journals/bap_supplements.asp for a copy of the data sheet). Staff documented the occurrence of urination immediately in the cell corresponding with the time of day. The coded format on the scatter plot included C for correct, A for accident, and I for incomplete. Correct was defined as the release of urine while seated on the toilet. Accident was defined as release of urine at any other location. Incomplete was defined as when the child neither urinated in the toilet nor had an accident during a 30-min interval. At the end of each day, the percentage correct was determined by a simple C/A+C equation (number correct over the number correct plus accidents). This allowed for a simple conversion to a percentage correct per day.
The data collected also allowed for detection of reliable times each participant was more likely to produce urine throughout the day. These data were readily available by plotting the times of the day over a more extended period of time (e.g., 1 week or longer) and determining a pattern of urination.
Interobserver Agreement and Program Fidelity
A second observer collected data for the purpose of assessing interobserver agreement (IOA) and participated in an average of 37% of all bathroom visits (range, 31% to 45%) across all 5 participants during baseline and intervention phases. IOA was 100% across all subjects during baseline, intervention, and post-treatment data collection.
Training for paraprofessionals began with a 1-hr in-service training before the start of the program. This training consisted of a PowerPoint presentation to explain procedures, a review of data collection systems, and role playing of the procedure. A BCBA provided didactic training and oversight of the staff for the first day of program implementation. Following this initial training, the consulting BCBA or special education teacher intermittently completed direct observation of program implementation, at least weekly. Any steps performed incorrectly were reviewed with the direct care staff and corrected at the time of the observation. The density of clinical support provided was based on the success of each participant. If the child was successful, weekly review of data occurred and the time between bathroom visits was increased. If the child demonstrated limited success, clinical staff more carefully monitored and assessed the effectiveness of reinforcer, accuracy of the bathroom visit schedule, the clarity of staff prompts, and suggested changes as warranted.
Preference Assessment
Before the start of intervention, clinical staff interviewed each participant's parents and direct care staff to identify highly preferred items for use in the toilet training program. Once the team compiled a list of high preference items for each participant, direct preference assessments were conducted (Paclawskyj & Vollmer, 1995). The participants had no access to the nominated items outside of the toilet training program. Four of the 5 participants selected edible rewards (e.g., M&Ms, crackers, etc.), and one participant selected a handheld, battery-operated spin toy. Access to the toy was limited to 15 s directly following correct urination.
Procedures
A concurrent multiple baseline across participants design was used to detect the effect of the training program on correct urinations. The baseline consisted of keeping the child in their regular diapers throughout the day, checking the diaper to determine if it was wet or dry every 30 to 60 min, and scheduled visits to the bathroom every 60 to 120 min. The teacher based this schedule on typical bathroom reminders that occurred in the inclusionary preschool program. Positive verbal and social interaction were delivered contingent on the presence of a dry diaper as well as for urination in the toilet.
A multicomponent toilet training procedure was then implemented by paraprofessional staff.
A countdown timer, a soft child-sized potty seat, a footstool for leg support, three clean sets of clothes, and individualized reinforcers were used while implementing the following program.
Diaper removal.
At the beginning of the school day, the participant's diaper was removed, and he wore regular underpants and sweatpants for the remainder of the day.
Fluid offering.
At the beginning of the day, students were given 8 oz of water or high preference beverage, preferably ingested within the first 90 min of the day. Additional fluids were offered if limited urinary output occurred. After participants successfully urinated in the toilet at least every 90–120 min, fluid offering was discontinued and typical fluid intake (e.g., snack time, lunch time) remained in place for the remainder of the intervention.
Bathroom visits.
Upon entering the classroom, participants were immediately taken to the bathroom. Participants sat on the toilet for a maximum of 3 min. Staff reset the timer for another 30 min interval, immediately after each trip to the bathroom. At the end of every 30 min, the timer sounded, the staff delivered the instruction “Time for Potty” and directed the participant to the bathroom with graduated guidance and social praise for cooperation.
Bathroom task analysis.
Once in the bathroom, staff delivered verbal cues to move through the program procedures. The cues included: Go to bathroom, lights on, close door, pants down, sit on toilet, stay on toilet [as needed], all done [upon sound of timer or upon urination], pants up, wash hands, lights off. Cues were succinct, upbeat, and were posted on the bathroom wall for staff to reference. Social praise followed all attempts to comply with each step. Once seated on the toilet, the staff set the timer for 3 min. At the start of the interval, staff held the reinforcer in the participant's field of vision. In an upbeat manner, staff stated, “First pee, then X” (X = reward). This statement occurred at least 2 to 3 times during the 3-min interval. Positive social interaction occurred when the participant remained seated. Staff gently redirected the participant back onto the toilet if needed.
Consequences for voiding in the toilet.
Staff carefully observed for any urinary output. If the participant urinated even a drop when on the toilet, staff delivered the reward, enthusiastic social praise within 0.5 s (e.g., “You peed on the potty! Time for X!”), and allowed the child to get off of the toilet. Clinical judgment was used to gradually increase the amount of urinary output required for reinforcement, after substantial improvements in urination on the toilet were initially established. If the participant excreted no urine at the end of 3 min, the timer sounded and the staff member guided the participant to pull his pants up, wash his hands, and exit the bathroom.
Consequence for urinary accidents.
Staff responded to wetting episodes with a neutral notification to the participant that he was wet (e.g., “You wet your pants. You need to change”). Staff immediately guided the child to the bathroom and assisted him in changing his clothes in a neutral manner. Upon exiting the bathroom, the staff reset the timer for 30 min.
Adjusting the schedule of bathroom visits.
Once the participant reached 100% correct urination for at least 3 consecutive days, the duration of time between trips to the bathroom increased by 15 min increments. In some instances, the child went well beyond the 3 consecutive day criterion. This occurred for two reasons. First, if criterion was met on a Friday, we preferred to extend criterion to ensure that the skill remained intact after a weekend recess from program. Second, staff were instructed to maintain the bathroom visit schedule until data were reviewed by the clinical team. At times, data reviews were limited to several days beyond meeting criterion due to the availability of the clinician on site. Schedule changes continued until the participant was able to remain dry all day and urinate on the toilet with 100% accuracy when visits to the bathroom were scheduled every 120 min.
Thinning the reward schedule.
Social praise continued to occur for every checked instance of dry pants and for correct urinations on the toilet; however, a gradual thinning of the edible rewards with 4 participants and the tangible reward with 1 participant occurred throughout the process. Once the participant urinated appropriately in the toilet on a 60 min schedule, the reward was provided for every second or third correct urination.
The formal program ceased once the participant demonstrated the ability to correctly urinate in the toilet with 100% accuracy on a 120-min schedule of bathroom visits. At this point, the participant was cued with a more natural schedule (e.g., typical bathroom breaks with preschool-aged children). Social praise for correct urinations remained in place in the school setting. Daily data collection continued at least 5 days after mastery and occurred at 2-hr intervals to assess maintenance of the skill.
Results and Discussion
Figure 1 depicts data for Cal, Lou, Job, Tom, and Cam. Baseline for Cal revealed 38% correct urination in the toilet over 16 days in baseline. Cal required 65 days of training to reach the mastery criterion (100% continent voids in the toilet during bathroom visits scheduled at 120 min intervals). Baseline for Lou revealed 8% correct over 24 days. Lou required 88 days of training to reach the mastery criterion. Baseline for Job revealed 34% correct over 40 school days. Fluctuation in the data appeared to be related to spring recess and a short summer break (1-week each), causing short-term regression, though Lou's performance quickly recovered. Job rapidly moved through the sequence of increased time intervals and had no accidents throughout the treatment, requiring a total of 46 days to reach the mastery criterion. Baseline for Tom revealed 14% correct in the toilet over 12 days of baseline. Like Job, Tom moved quickly through the training requiring 51 days to meet the mastery criterion. Baseline for Cam revealed 9% voiding in the toilet over 15 school days. In the beginning of treatment, Cam had multiple accidents from 11:30 am to 12:30 pm. Based on these data, Cam was brought to the bathroom every 15 min from 11:15 am to 12:30 pm. The remainder of the day continued with a 30 min schedule for bathroom visits. Cam reached the mastery criterion after 32 school days. Table 1 summarizes the number of school days as well as calendar days required for each student to move from diaper dependency to 100% mastery criterion with a 2-hr bathroom visit schedule in place.
Figure 1.
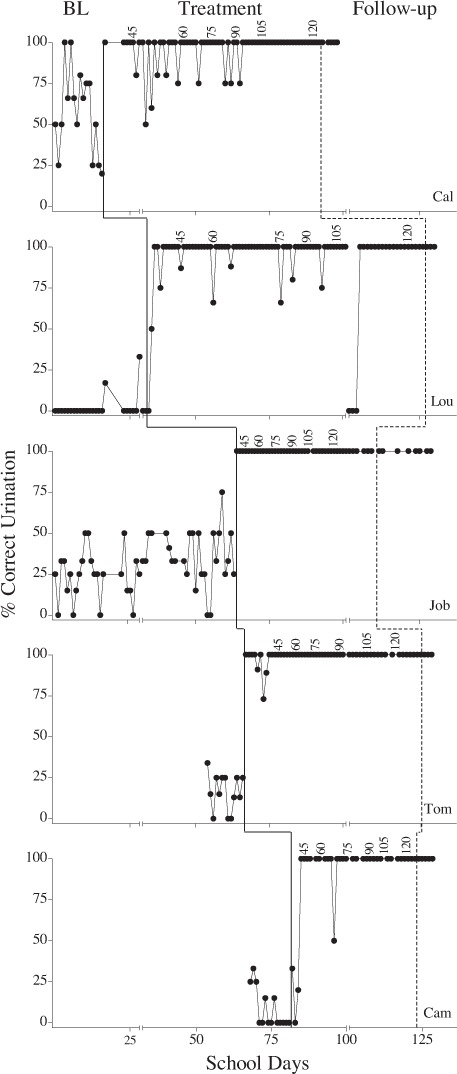
The percentage of correct urinations per school day is represented for 5 participants. Breaks in the x-axis refer to seasonal vacations and data labels denote time between bathroom visits.
The purpose of this study was to investigate the efficacy of a toilet training program for children with autism and developmental delays in a public school setting with minimal clinical oversight and with the intervention implemented by paraprofessional direct care staff. Results from this study demonstrated that all 5 participants were able to retain urine in their bladder for periods of 2 hrs or more and urinate in the toilet after implementation of this program in school.
This study differs from prior research as it describes a method that can be implemented in a school setting by paraprofessional staff. It implements toilet training in a nonclinical setting with minimal clinical support, and good effects were observed without the use of procedures like restitution or overcorrection for incontinence. All 5 participants succeeded, though each took varying time periods to meet criterion, ranging from 32 to 88 school days with an overall mean of 56 school days. The number of calendar days (to include weekends, holidays, and breaks) across all 5 participants ranged from 72 days to 135 days with an overall mean of 96 days, or just over 3 months.
Toilet training can be a developmental obstacle for participants diagnosed with autism or developmental delays, yet toileting skills are an important part of a person's development that allows for greater independence and enhances dignity in the social domain (McManus, Derby, & McLaughlin, 2003). Paraprofessional staff, who are often available in school districts serving children with autism and developmental delays, were capable in the current study to implement an effective outcome with minimal support from supervising clinicians. These results are encouraging because they suggest that this procedure may be practical enough for educational staff to implement in classroom settings.
Nevertheless, the amount of time dedicated to the process of toilet training does have an inherent cost in terms of time lost to teaching other important skills. Before implementing the program, the school-based team met with the parents and clearly described the amount of time that toilet training would take. In the beginning, an average of 5 to 10 min per ½ hr was used to transition to the bathroom, sit on the toilet, and return to work. As the interval between bathroom visits expanded, the impact of other programming was less of a concern. Parents were informed of this issue and understood and agreed to the impact on academics before enrolling their child in this study. Future research should attempt to determine the impact that allocating time to toilet training has on academic learning rate.
There are several limitations of this analysis that should be considered. First, although the procedures were applied across multiple children and paraprofessionals, additional applications of these procedures should be researched in other schools to determine the generality of the program. In addition, the generality of the program would also be better understood by measuring the effects of the school-based program on in-home continence. Once mastery was attained in the school setting in the current study, the special education teacher met with the parents to review procedural guidelines and encouraged the parents to monitor program implementation in the school. Parents of the participants reported successful toileting in the home environment following the successful training at school. Nevertheless, objective measurement of these sorts of outcomes are necessary to predict the likely generality of school-based toilet training programs.
A second limitation of this study was the omission explicit procedures to train and detect self-initiations to use the bathroom during the toilet training treatment program. The skill of self-initiating toileting is important and future research should replicate this toilet training program and add procedures for teaching self-requesting of bathroom visits.
Despite the limitations presented here, the data across participants provide strong evidence that paraprofessionals readily available in an inclusionary school system can effectively implement a data-based toilet training program with lasting effects.
Footnotes
Many thanks to the parents who willingly agreed to include their children in this study. They remain anonymous to ensure the confidentiality of the children, though their cooperation is deeply appreciated. Also, we are indeed grateful to the special education teachers, ABA therapists and the school district, all of who worked as dedicated staff to meet the needs of the children and provide empirical evidence to forward to the scientific and educational community at large.
Action Editor Jonathan Tarbox
References
- Azrin N., Foxx R. Toilet training in less than a day. New York: Simon and Schuster; 1974. [Google Scholar]
- Blum N. J., Taubman B., Nemeth N. Why is toilet training occurring at older ages? A study of factors associated with later training. Journal of Pediatrics. 2004;145:107–111. doi: 10.1016/j.jpeds.2004.02.022. [DOI] [PubMed] [Google Scholar]
- Blum N. J., Taubman B., Nemeth N. Relationship between age at initiation of toilet training and duration of training: A prospective study. Pediatrics. 2003;111:810–814. doi: 10.1542/peds.111.4.810. [DOI] [PubMed] [Google Scholar]
- Bryson S. E., Rogers S. J., Fombonne E. Autism spectrum disorders: Early detection, intervention, education, and psychopharmacological management. Canadian Journal of Psychiatry. 2003;48:506–515. doi: 10.1177/070674370304800802. [DOI] [PubMed] [Google Scholar]
- Cicero F. R., Pfadt A. Investigation of a reinforcement-based toilet training procedure for children with autism. Research in Developmental Disabilities. 2002;23:319–331. doi: 10.1016/s0891-4222(02)00136-1. [DOI] [PubMed] [Google Scholar]
- Konarski E. A., Diorio M. S. A quantitative review of self-help research with the severely and profoundly retarded. Applied Research in Mental Retardation. 1985;6:229–245. doi: 10.1016/s0270-3092(85)80072-2. [DOI] [PubMed] [Google Scholar]
- Kroeger K. A., Sorensen-Burnworth R. Toilet training individuals with autism and other developmental disabilities. Research in Autism Spectrum Disorders. 2009;3:607–618. [Google Scholar]
- Kroeger K. A., Sorensen R. A parent training model for toilet training children with autism. Journal of Intellectual Disability Research. 2010;54:556–567. doi: 10.1111/j.1365-2788.2010.01286.x. [DOI] [PubMed] [Google Scholar]
- LeBlanc L. A., Carr J. E., Crossett S. E., Bennett C. M., Detweiler D. D. Intensive outpatient behavioral treatment of primary urinary incontinence of children with autism. Focus on Autism and Other Developmental Disabilities. 2005;20:98–105. [Google Scholar]
- Luiseli J. Teaching toileting skills in a public school setting to a child with pervasive developmental disorder. Journal of Behavior Therapy and Experimental Psychiatry. 1997;28:163–168. doi: 10.1016/s0005-7916(97)00011-6. [DOI] [PubMed] [Google Scholar]
- McManus M., Derby K. M., Dewolf E., McLaughlin T. F. An evaluation of an ın-school and home based toilet training program for a child with fragile X syndrome. International Journal of Special Education. 2003;18:73–79. [Google Scholar]
- Paclawskyj T. R., Vollmer T. R. Reinforcer assessment for children with developmental disabilities and visual impairments. Journal of Applied Behavior Analysis. 1995;28:219–224. doi: 10.1901/jaba.1995.28-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadtler A., Gorsky P., Brazelton T. B. Toilet training methods: Clinical interventions and recommendations. Pediatrics. 1999;103:1359–1361. [PubMed] [Google Scholar]
- U.S. Department of Education. Building the legacy: IDEA 2004. 2004. Retrieved August 20 2009, from http://idea.ed.gov/archive.
- Van Wagenen R. K., Meyerson L., Kerr N. J., Mahoney K. Field trials of a new procedure in toilet training. Journal of Experimental Child Psychology. 1969;8:147–159. doi: 10.1016/0022-0965(69)90036-8. [DOI] [PubMed] [Google Scholar]


