Abstract
Since the first case of strongyloidiasis reported in China in 1973, there have been 330 confirmed cases as of 2011. The present study conducted a meta-analysis on 106 cases for which detailed information on clinical symptoms, diagnosis, and outcome was available. Most (63%) cases were from the past decade. Immunocompromised patients and those given cortical hormones accounted for 68% of the cases, and case-fatality rate was 38%. General clinical symptoms included abdominal pain (53%), diarrhea (46%), fever (40%), and vomiting (39%). The parasite positivity rate in feces, sputum, and urine by microscopic diagnosis was 75%, 24%, and 8%, respectively, and gastrointestinal endoscopy or other biopsy detection rates were 17%. A lack of specific clinical manifestations makes early diagnosis and correct treatment difficult. Strongyloidiasis is an emerging disease in China, and public and clinical awareness needs to be raised to improve prevention and control.
Introduction
Strongyloides stercoralis (Bavay, 1876) was first described in Vietnam from a fecal sample of a French soldier with diarrhea. It is a facultative pathogen, alternating opportunistically between a free-living and parasitic life cycle. Adult worms reside in the intestine during the parasitic cycle, and larvae may invade the lungs, brain, liver, kidney, and other organs, resulting in strongyloidiasis.1 The incidence of strongyloidiasis is increasing in many developing countries and is facilitated by international travel and immigration,2,3 and increasing numbers of immunosuppressed or immunocompromised patients. Misdiagnosis and missed diagnosis resulting from the lack of disease-specific manifestations contribute to it being a neglected tropical disease.4
We reviewed and analyzed strongyloidiasis cases reported in China.5–98 The first documented patient was from Guangxi Province in 1973. Since that time, 330 cases have been reported. We focus on 106 cases for which detailed information, including analysis of clinical symptoms, diagnosis, treatment, and epidemic distribution, is available. We expect that this analysis will highlight the importance of strongyloidiasis in China, enhance clinical diagnostic ability, and arouse public attention to prevention.
Methods
Strongyloides stercoralis was used as key word to search all relevant articles in the China National Knowledge Infrastructure database, the VIP Database for Chinese Technical Periodicals, the Wanfang database, as well as PubMed, ScienceDirect, and Springerlink. Publications related to strongyloidiasis reports in China were reviewed and characterized for parasitology, epidemiology, symptom and signs, diagnosis, treatment, and prevention.
Results and Discussion
Parasitology.
Free-living, infective S. stercoralis filariform larvae can penetrate the skin and initiate the parasitic life cycle, a mode of transmission similar to hookworm.1 The larvae migrate to the digestive system via the circulatory system and invade and colonize the small intestinal (mostly duodenal and jejunal) mucosa, where they develop into adult worms. Adult female worms usually reside under the intestinal mucosa where they shed eggs. Fertilized eggs produce rhabditiform larvae that exit the mucosa into the intestinal cavity from which they are excreted in the feces. The parasitic life cycle likely includes autoinfection, especially in immunosuppressed or immunocompromised hosts. Three routes are possible: direct endo-autoinfection during which rhabditiform larvae hatch and continue to develop in the mucosa and circulate to other organs and tissues via the circulatory system; indirect endo-autoinfection characterized by rhabditiform larvae escaping the mucosa and developing into filariform larvae in the intestinal cavity and invading the circulatory system from the colonic mucosa or lower intestine; and exo-autoinfection whereby filariform larvae excreted from the feces re-infect the host from perianal skin.
Epidemiology.
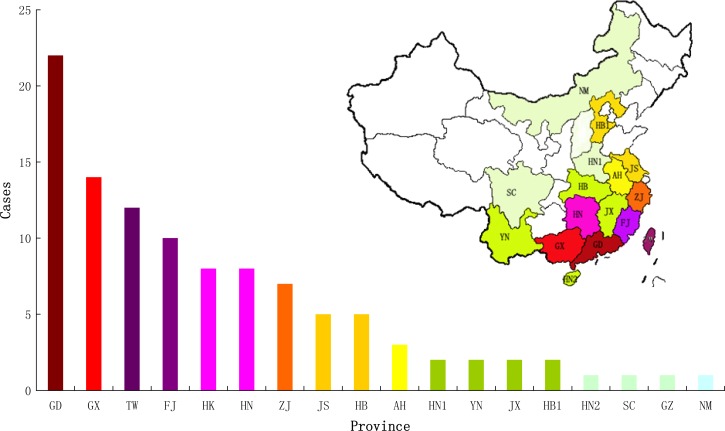
Thirty to 100 million persons worldwide are infected with S. stercoralis, and most cases are in tropical, subtropical, and temperate regions.4 The National Human Parasite Distribution survey has reported strongyloidiasis in 26 Provinces (cities and districts) in China, mainly in the southern regions of this country (Figure 1). Prevalence countrywide averages 0.12%, and some regions have rates as high as 11.0–14.0%.1 The farming areas of Tianyang and Baise Counties (Guangxi Province) had an average infection rate of 3.69%.99 Residents of Qiaozhuang, Boxing County (Shandong Province), had an S. stercoralis infection rate of 1.29% (11 of 854), with no obvious differences in sex and age distribution.100 A survey in Menghai County (Yunnan Province) reported an infection rate of 11.6% (29 of 250).101
Figure 1.
Cumulative cases and distribution of strongyloidiasis in China, 1973–2011. GD, Guangdong Province; GX, Guangxi Province; TW, Taiwan Province; FJ, Fujian Province; HK, Hong Kong; HN, Hainan Province; ZJ, Zhejiang Province; JS, Jiangsu Province; HB, Hebei Province; AH, Anhui Province; HN1, Hainan Province; YN, Yunnan Province; JX, Jiangxi Province; HB1, Hubei Province; HN2, Henan Province; SC, Sichuan Province; NM, Neimeng Province.
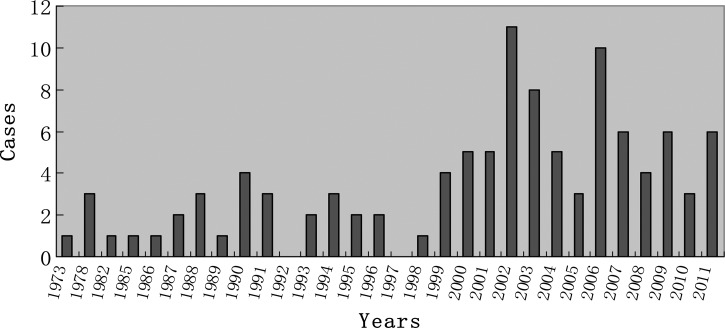
Ninety-four reports of strongyloidiasis were reported during 1973–2012, and 106 cases in these reports are accompanied by detailed information. After the described case in 1973, an additional four cases were documented in the subsequent decade (1973–1982). Case reports have increased every year since 1985, except in 1992 and 1997, and 58% of the 106 cases occurred during the past 10 years (2002–2011) (Figure 2). Case reports were from provinces and autonomous regions, most of which are south of the Yangtze River. A total of 21% (22 of 106), 13% (14 of 106), and 11% (12 of 81) of the cases originated in Guangdong, Guangxi and Taiwan, respectively (Figure 1). Small geographic clusters of cases were evident in Lufeng, Guangdong (four cases);11,64 Nanping, Fujian (three cases);30,35,43 and Yunxiao County, Fujian (two cases).65,67 Clustering also was evident in families in rural areas.64
Figure 2.
Annual number of strongyloidiasis cases in China, 1973–2011.
One-hundred and three of the 106 cases reported sexes of the patients (71 male patients and 32 female patients) (male:female ratio = 2.19:1). A total of 54 reports documented occupation; 64% described as peasants, workers (15%), or students (9%) (Figure 3). Some patients in the worker groups worked on farms,33,65,67 and most of the student patients lived or came from villages.64,86 This distribution and sex ratio bias (males are the principal field workers) support the conclusion that rural populations have the highest risk for strongyloidiasis. This risk probably results the agrarian living and working environment and frequent exposure to soil. The age distribution of the 91 patients for which records are available are consistent with increased exposure with age. Although the youngest and oldest patients were 5 and 88 years of age, respectively,17,55 69% of the patients were > 41 years of age, and persons 41–50 years of age accounted for the largest number of cases (25) (Figure 4).
Figure 3.
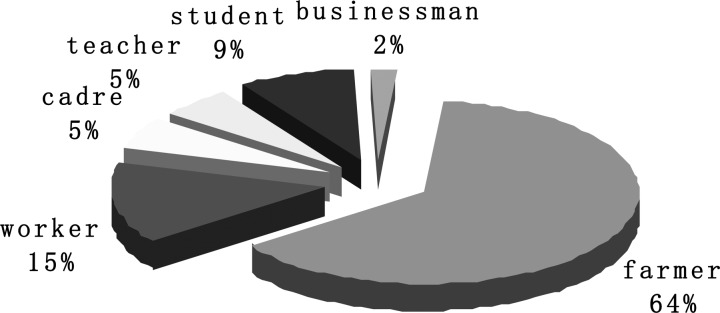
Occupation distribution of patients with strongyloidiasis in China, 1973–2011.
Figure 4.
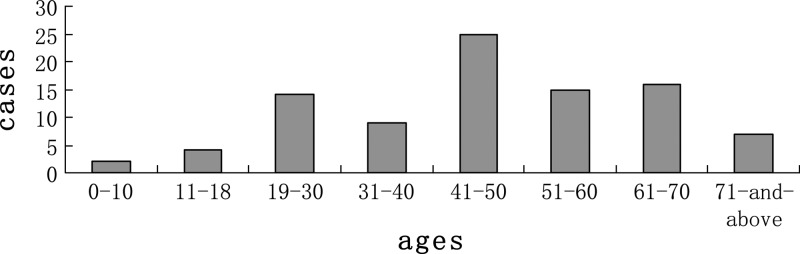
Age distribution of patients with strongyloidiasis in China, 1973–2011.
Clinical features.
Larval and adult S. stercoralis are pathogenic, and severity of diseases is correlated closely with worm burden (intensity of infection) and immunologic status of the host. People with normal immune system function generally will not have clinical symptoms if infected mildly (low worm burden). A chronic autoinfection may persist for several years with occasional gastrointestinal symptoms. In contrast, immunecompromised patients may have disseminated hyperinfection characterized by mass migration of the larvae inside the body. Invasion of the brain, liver, lung, and kidney results in severe damage that can progress to organ failure and death.
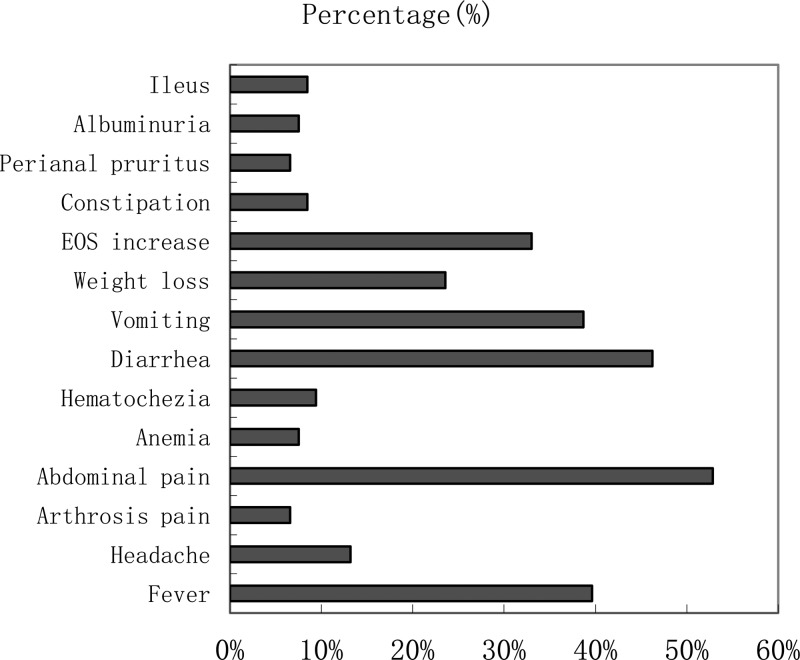
Strongyloidiasis patients have mainly non-specific gastrointestinal symptoms, including nausea, vomiting, abdominal pain, diarrhea accompanied by fever, anemia, and malaise. General clinical symptoms in the 106 detailed reports included abdominal pain (53%), diarrhea (46%), fever (40%), vomiting (39%), and lack of appetite (24%) (Figure 5). Severe infection can be complicated with gastrointestinal bleeding, leading to hemorrhagic anemia, kidney failure, and death.20 Patients with massive gastrointestinal infection may have intestinal obstruction.6,10,32,64
Figure 5.
Symptoms and other diseases among patients with strongyloidiasis in China, 1972–2011. EOS = eosinophils.
Strongyloidiasis patients may also have stiff necks and severe headaches as a result of infection of the brain. One case diagnosed as intracranial strongyloidiasis was confirmed by magnetic resonance imaging.28 The patient ceased therapy and returned home for economic reasons. The patient's condition worsened and resulted ultimately in systemic failure and death. Filariform larvae were detected in the cerebrospinal fluid of another patient but this person recovered fully after a course of treatment.44 Other reported cases of strongyloidiasis involve the urinary system; one patient had frequent, urgent, and painful urination but no diarrhea history, and a six-year-old patient infected in the spine had dyskinesia of both lower limbs.14,36
Eosinophil data were available for 55 of the 106 cases; 35 increased (63%), 8 were normal (15%), and 12 decreased (22%). The highest eosinophil value reported was 38.4% (absolute value of 4.81 × 109 cells/L), and the lowest value was 0%.7,46,47,67,81,88 Helminth infections are accompanied by elevated levels of eosinophis. However, this finding may occur with S. stercoralis infections. More research is needed to determine whether the relationship of eosinophils with these infections.
Strongyloides stercoralis infection may lead to elevated IgE levels in patients. There were only 12 documented immunity test reports among our samples, and these include 5 reports with IgE levels three-fold higher than the reference range (< 200 IU/mL or < 0.009 g/L).1–5 Among the five case-patients, one patient with an IgE level of 638.53 IU/mL had a severe infection and eventually died.47 There were two case-patients with pulmonary disseminate infections and IgE levels of 736 IU/mL and 739 IU/mL.13,17 Two other patients had mild infections and IgE levels of 2,560 IU/mL and 2.09 g/L.23,83 The IgE values increased in all five patients, and changes in range were generally inversely proportional to the degree of infection. Patients with mild infections had the most significant increase in IgE levels. Patients with severe or disseminated infections had relatively lower levels of IgE.
Seventy-two (68%) of the 106 strongyloidiasis patients had other diseases, including rheumatoid arthritis, systemic lupus erythematosus, diabetes, nephrotic syndrome, chronic obstructive pulmonary disease, and carcinoma, or used immunosuppressive drugs (Table 1). All of these patients were expected to have suppressed immunity that exacerbates a disseminated infection and results in severe symptoms and death. The mortality rate of the 72 patients was 37.5% (27 of 72). Disseminated strongyloidiasis occurs usually among immunosuppressed patients, such as those with malignant tumors or those using immunosuppressive agents (especially steroids). However, patients with acquired immunodeficiency syndrome did not show many disseminated infections and the reasons for this are unclear. One possible explanation is that the level of CD4+ cells had not decreased much when patients with acquired immunodeficient syndrome died.102 Patients with diabetes and nephrotic syndrome have higher disseminated strongyloidiasis infection rates. Diabetes patients may prevent severe strongyloidiasis infection through immunologic screening.102,103
Table 1.
Underlying characteristics associated with human strongyloidiasis in China, 1973–2011
| Characteristic | No. cases |
|---|---|
| Carcinoma | 7 |
| Rheumatoid arthritis | 7 |
| Systemic lupus erythematosus | 5 |
| Chronic obstructive pulmonary disease | 6 |
| Nephrotic syndrome | 7 |
| Diabetes | 5 |
| Allergic purpura | 3 |
| Chronic bronchitis | 2 |
| Rheumatic heart disease | 2 |
| Fisher syndrome | 1 |
| Sjogren's syndrome | 1 |
| Scleroderma | 1 |
| Endobronchial tuberculosis | 1 |
| Meningitis | 1 |
| Duodenal ulcer | 1 |
| Induction of labor | 1 |
| Parasitosis | 9 |
| Drug abuse | 1 |
| Steroid therapy for other diseases | 10 |
Diagnosis and treatment.
The lack of specific clinical features resulting from S. stercoralis infection results in a high percentage of misdiagnosed cases. Twenty-three of the 106 cases were diagnosed initially as ancylostomiasis (6 cases), carcinoma (2 cases), gastritis (3 cases), enteritis (3 cases), bronchitis (1 case), and dysentery (1 case) before follow-up examinations confirmed strongyloidiasis. Therefore, strongyloidiasis should be considered and ruled out for all immunocompromised patients from high-risk regions (rural) who have gastrointestinal and respiratory symptoms. Patients with bloody, purulent, or watery feces should be tested to differentiate strongyloidiasis from shigellosis or amebic dysentery.54,69 Similarly, patients with abdominal pain should be examined to differentiate strongyloidiasis from gastritis and duodenitis.26,33,37
Diagnosis of strongyloidiasis is based mainly on detection of rhabditiform or filariform larvae in samples of feces, sputum, gastric juices, and cerebrospinal fluid. Immunologic techniques, such as enzyme-linked immunosorbent assay and immunoblots, and molecular methods based on gene amplification can also be useful in diagnosis.104 Seventy-five percent of the 106 patients tested positive in stool specimens, while 24, 8, 4 and 2% were positive in sputum, urine, vomit and duodenal drainage specimens, respectively. Approximately 1% of the patients had positive results for strongyloidiasis in gastric juices, hydrocele, cerebrospinal fluid, scrotal hydrocele fluid, and pericardial effusions. Gastrointestinal endoscopic biopsy and other pathologic examination detected 17% of the cases, and fiber optic bronchoscopy accounted for an additional 1%. Twenty-nine percent of the patients tested were pathogen positive for more than one specimen.
Strongyloides stercoralis of every developmental stage were detected among the 106 cases (Table 2). Rhabditiform and filariform larvae were reported in 48% and 20% of the cases, respectively, and 14% had eggs. Male and female adult worms were detected simultaneously in stool specimens in two cases. Male worms are seldom seen in human host,71,82 and there is debate as to whether they are part of the parasitic life cycle. However, there are a number of early reports of males in diseased patients.105
Table 2.
Diagnosis of human strongyloidiasis in China, 1972–2011*
| Sample | No. cases | Developmental stage | ||||
|---|---|---|---|---|---|---|
| RL | FL | Egg | Adult (female) | Adult (male) | ||
| Feces | 70 | 44 | 11 | 9 | 3 | 2 |
| Sputum | 18 | 11 | 4 | 1 | 1 | 0 |
| Urine | 9 | 8 | 1 | 2 | 0 | 0 |
| Vomit | 4 | 3 | 1 | 2 | 0 | 0 |
| Gastric juices | 1 | 0 | 0 | 1 | 1 | 0 |
| Cerebrospinal fluid | 1 | 0 | 1 | 0 | 0 | 0 |
| Hydrocele | 1 | 0 | 1 | 0 | 0 | 0 |
| Duodenal drainage | 1 | 0 | 0 | 1 | 0 | 0 |
| Gastric/duodenal biopsy | 18 | 2 | 1 | 5 | 2 | 0 |
| Fiber optic bronchoscopy | 1 | 0 | 0 | 1 | 0 | 0 |
From 106 cases described in the text. RL = rhabditiform larvae; FL = filariform larvae.
Treatment.
Treatment of strongyloidiasis should begin after diagnosis and apply the principles of early treatment with sufficient dosage and duration to cause complete worm elimination. Traditionally, tiabendazole is the drug of first choice with other options including mebendazole, albendazole, and levamisole. Seventy-nine of the 106 case reports contained detailed information on drug treatments and albendazole was the choice for 62% (49 of 79) of the patients with dosage provided based on the patient's condition. Regimens of 400–800 mg, twice a day for 3–10 days, resulted in a cure rate of 61%. Patients with obstinate strongyloidiasis or albendazole resistance can be treated with ivermectin54 and 3 of 106 patients receiving this drug recovered fully.17,31 Traditional Chinese medicine also was effective; three cases of strongyloidiasis accompanied by allergic purpura were cured after oral administration of 10 g of guan zhong, three times a day for seven days, then a 7–10 days break, followed by another course for one week.41 Gentian violet was recommended for three patients with renal failure. One case of strongyloidiasis accompanied by hemorrhagic enteritis was treated with 90 mg/day of gentian violet for 14 days and the patient recovered and was discharged.78
Prevention.
The incidence of strongyloidiasis in China has been increasing in recent years, especially in the southern region, and rural and immunocompromised populations at highest risk. Because the disease has nonspecific clinical features, it is easily to misdiagnosis. Medical professionals, especially doctors and diagnosticians, should improve their diagnostic and differential diagnostic capabilities. High-risk population should be made aware of the infection threat and instructed in preventative measures. Patients receiving immunosuppressive therapy who have gastrointestinal symptoms should be tested to exclude strongyloidiasis.
Recommendations for prevention of strongyloidiasis in China include not being barefoot while working or traveling in fields in strongyloidiasis-epidemic regions. Raw vegetables and fruits should be washed multiple times with clean fresh water to avoid possible S. stercoralis contamination. Patients with immunocompromised or immunosuppressed conditions or those initiating immunosuppressive therapy should be screened for S. stercoralis infection. Persons with positive test results should be treated before onset of symptoms or with the other proposed therapies. Patients receiving steroid hormones (dexamethasone) for long periods should take preventative medications (albendazole) for strongyloidiasis every three months.
Footnotes
Financial support: This study was supported by grants from the National Natural Science Foundation of China (U0832004) and Guangdong University of Foreign Studies GDUPS (2009) to Xiaoguang Chen.
Authors' addresses: Chunmei Wang, Jiabao Xu, and Xiaohong Zhou, Department of Parasitology, Southern Medical University, Guangzhou, China, E-mails: wangcmq@163.com, xujiabao007@gmail.com, and daizhouxh@163.com. Juan Li, Nanfang Hospital, Southern Medical University, Gaungzhou, China, E-mail: lj40038@126.com. Guiyun Yan, Program in Public Health, University of California, Irvine, CA, E-mail: guiyuny@uci.edu. Anthony A. James, Department of Molecular Biology and Biochemistry, University of California, Irvine, CA, E-mail: aajames@uci.edu. Xiaoguang Chen, No 1023 Shatai South Road, Guangzhou, China, E-mail: xgchen2001@hotmail.com.
References
- 1.Chen XG, Zheng XL. Medical parasitology [in Chinese] Mil Med Press: 2008:58–62. [Google Scholar]
- 2.Lim S, Katz K, Krajden S, Fuksa M, Keystone JS, Kain KC. Complicated and fatal Strongyloides stercoralis infection in Canadians: risk factors, diagnosis and management. CMAJ. 2004;171:479–484. doi: 10.1503/cmaj.1031698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paula FM, Costa-Cruz JM. Epidemiological aspects of strongyloidiasis in Brazil. Parasitology. 2011;138:1331–1340. doi: 10.1017/S003118201100120X. [DOI] [PubMed] [Google Scholar]
- 4.Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, Stothard R, Thybo S, Verweij JJ, Magnussen P. Strongyloidiasis: the most neglected of the neglected tropical diseases? Trans R Soc Trop Med Hyg. 2009;103:967–972. doi: 10.1016/j.trstmh.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Shen SJ, Li J, Wang CM, Zhou B, Mai RJ, Jiang RL, Zhou XH. A case of rheumatoid arthritis complicated with Strongyloides stercoralis [in Chinese] Int J Med Parasit Dis. 2011;38:119–122. [Google Scholar]
- 6.Wang XL, Li JD, Xu PR, Deng WP. Digestive tract strongyloidasis presented with small intestine obstruction. A case report [in Chinese] Chin J Integr Med. 2011;50:257–258. [Google Scholar]
- 7.Xiang Y, Lu ZJ, Yan YH, Lin Y. Scleroderma complicated with strongyloidiasis [in Chinese] Int Med Health Guidance News. 2011;17:569–570. [Google Scholar]
- 8.Chen YX, Xie JZ, Shen HX, Zhou CD. Patient with Sjogren's syndrome infected with strongyloidiasis. A case report and literature review [in Chinese] J Trop Med. 2011;11:1222–1223. [Google Scholar]
- 9.Zhu XY, He L, Zhang HG, Yang SJ, Zhang XL, Zhou YR. Etiological detection and treatment of a hyperinfection Strongyloides stercoralis case [in Chinese] J Med Pest Control. 2011;27:170–171. [Google Scholar]
- 10.Tsai MJ, Wu TS, Tsai KB, Chen HC, Hwang JJ, Huang MS. Acute respiratory distress syndrome complicating Strongyloides stercoralis. Int J Gerontol. 2011;5:53–55. [Google Scholar]
- 11.Huang JT, Wei JZ. A case report of Strongyloidiasis infection. Nat Med. 2010;41:50. (In Chinese) [Google Scholar]
- 12.Lu F, Ye LP, Zhu ZH, Zhang JN. A case report of Hodgkin lymphoma complicated with Strongyloides stercoralis. Chin J Parasite Parasitol Dis. 2010;28:1. [PubMed] [Google Scholar]
- 13.Chen JH, Chao TY, Peng WC. Strongyloides stercoralis infection of skin and lung. Q J Med. 2010;103:199–200. doi: 10.1093/qjmed/hcp106. [DOI] [PubMed] [Google Scholar]
- 14.Fu LM, Zhang M, Yang DM, Feng X, Yan J. A case of iIntraspinal Strongyloides stercoralis infection [in Chinese] Chin J Diffic and Compl Cas. 2009;8:57. [Google Scholar]
- 15.Lu YJ, Zou JM. A case report of lymphocytic leukemia complicated with Strongyloides stercoralis infection [in Chinese] Chin J Parasitol Parasit Dis. 2009;27:139. [PubMed] [Google Scholar]
- 16.Jiang WS, Xie SY, Lan WM. A case report of severe Strongyloides stercoralis infection [in Chinese] Chin J Parasite Parasitol Dis. 2009;27:1. [Google Scholar]
- 17.Hsu WH, Yang SF, Su YC. Strongyloides stercoralis ileitis detected by double-balloon endoscopy. Endoscopy. 2009;41:E292–E293. doi: 10.1055/s-0029-1215073. [DOI] [PubMed] [Google Scholar]
- 18.Liu HC, Hsu JY, Chang KM. Strongyloides stercoralis hyperinfection presenting with symptoms mimicking acute exacerbation of chronic obstructive pulmonary disease. J Chin Med Assoc. 2009;72:442–445. doi: 10.1016/S1726-4901(09)70403-4. [DOI] [PubMed] [Google Scholar]
- 19.Huang ZR. A case of nephrotic syndrome with Strongyloides stercoralis infection [in Chinese] China Practical Medicine. 2008;3:145. [Google Scholar]
- 20.Zhang KR, Duan JH. A case report of severe strongyloidiasis complicated with gastrointestinal hemorrhage. J Trop Med. 2008;8:1198. [Google Scholar]
- 21.Shen HW, Wang LJ. A case report of Strongyloidiasis infection [in Chinese] Chin J Lab Med. 2008;31:1190–1191. [Google Scholar]
- 22.He ZT. Misdiagnosis analysis of Strongyloides stercoralis [in Chinese] Hainan Medical J. 2008;19:89–122. [Google Scholar]
- 23.Zhuang H, Yan HY, Li WJ. A case report of Strongyloides stercoralis infection [in Chinese] J Pract Med Tech. 2007;14:27. [Google Scholar]
- 24.Wang WW, Dai SZ, Yang LP. A case report of praziquantel treating Strongyloides stercoralis complicated with Clonorchis sinensis infection [in Chinese] Chin J Zoonoses. 2007;23:1164. [Google Scholar]
- 25.Wang JX, Wang MZ. A case of frugster infected with Strongyloides stercoralis [in Chinese] J Pathogen Biol. 2007;2:182–188. [Google Scholar]
- 26.Cui Y, Chen XY, Lu H, Shi Y. A case of duodenum Strongyloides stercoralis infection [in Chinese] Chin J Gastroenterol. 2007;12:383. [Google Scholar]
- 27.Luo GH, Huang L, Zhao BQ. A case report of central neural system infected with cryptococcosis complicated with strongyloidiasis [in Chinese] Chin J Infectious Dis. 2007;25:694. [Google Scholar]
- 28.Zhao SH. A case of severe disseminated strongyloidiasis [in Chinese] J Dali Univ. 2007;2:32. [Google Scholar]
- 29.Guan XY. A case report of incidental detection of Strongyloides stercoralis [in Chinese] Guangxi Med J. 2006;28:1682. [Google Scholar]
- 30.Li JW. A case report of diabetes complicated with severe Strongyloides stercoralis infection [in Chinese] Applied J Gen Prac. 2006;4:701–702. [Google Scholar]
- 31.Hsieh YP, Wen YK, Chen ML. Minimal change nephrotic syndrome in association with strongyloidiasis. Clin Nephrol. 2006;66:459–463. doi: 10.5414/cnp66459. [DOI] [PubMed] [Google Scholar]
- 32.Lam CS, Tong MK, Chan KM, Siu YP. Disseminated strongyloidiasis: a retrospective study of clinical course and outcome. Eur J Clin Microbiol Infect Dis. 2006;25:14–18. doi: 10.1007/s10096-005-0070-2. [DOI] [PubMed] [Google Scholar]
- 33.Lv G, Tan X, Wu CP, Lin QL. A case report of severe Strongyloides stercoralis infection caused death in Hainan Province [in Chinese] China Trop Med. 2005;5:277. [Google Scholar]
- 34.Su SL, Chen GF, Zhang RQ. A case of severe Strongyloides stercoralis infection complicated with meningoma and cholelithiasis [in Chinese] Chin J Parasitol Parasit Dis. 2005;23:9. [PubMed] [Google Scholar]
- 35.Gao SH, Chi XD. A case report of Strongyloides stercoralis infection caused death [in Chinese] Chin J Infect Control. 2005;4:278. [Google Scholar]
- 36.Li SL, Wu QH. A case report of Strongyloides stercoralis infection in unitary system [in Chinese] Chin J Schisto Control. 2004;16:310. [Google Scholar]
- 37.Wang AL, Liu SD, Zang YL, Wang KR. A case report of severe Strongyloides stercoralis infection in small intestine [in Chinese] Modern Digestion Intervention. 2004;9:100. [Google Scholar]
- 38.Li YW, Zhao BQ. A case report of lupus nephritis complicated with disseminated Strongyloides stercoralis infection [in Chinese] Chin J Parasitic Dis Control. 2004;17:122. [Google Scholar]
- 39.Zhao JQ, Liu ZJ, Li XP. A case report of sputum detection of Strongyloides stercoralis [in Chinese] Chin J Lab Diagn. 2004;8:27. [Google Scholar]
- 40.Ma TY, Zhang AJ, Lei ZH. A case report of systemic lupus erythematosus complicated with Strongyloides stercoralis infestation [in Chinese] Hebei Med J. 2004;26:126. [Google Scholar]
- 41.Meng ZX. Treating anaphylactoid purpura caused by Strongyloides stercoralis by traditional medicine: report of 3 cases [in Chinese] CJMC. 2003;3:1725. [Google Scholar]
- 42.Lei SY, Yang YJ, Bai L. Mixed infection of Strongyloides stercoralis and Clonorchis sinensis: report of one case [in Chinese] J First Mil Med Univ. 2003;23:636. [PubMed] [Google Scholar]
- 43.Li YS, Zhang ZP, Xu LS, Lin CX, Den YQ, Chen BJ, Cai CH, Zhang RY, Xie KJ, Liu B, Lin JX. Checking of eggs and worms in a patient severely infected with Strongyloides stercoralis [in Chinese] J Trop Med. 2003;3:312. [Google Scholar]
- 44.Li YS, Lin JX, Chen BJ, Xu LS. Diagnosis and treatment of infestation with Strongyloides stercoralis in brain [in Chinese] J Trop Med. 2003;3:188–189. 214. [Google Scholar]
- 45.Ouyang LM, He HH. A severe case of strongyloidiasis autoinfection [in Chinese] Chin J Parasitol Parasit Dis. 2003;21:288. [Google Scholar]
- 46.Hu JY, Tang ZM. A case report of Strongyloides stercoralis infection [in Chinese] Chin J Parasitic Dis Contr. 2003;16:228. [Google Scholar]
- 47.Lu XD, Shan XY, Xu RL, JY T. Report on a case of death caused by severe Strongyloidiasis stercoralis [in Chinese] Zhejiang Clin Med J. 2002;4:887. [Google Scholar]
- 48.Shen Q. Fisher symptom complicated with Strongyloides stercoralis infection and nurse case [in Chinese] Mo Nurse. 2002;8:482. [Google Scholar]
- 49.Huang WQ. Strongyloides stercoralis infection caused pancreatitis, case report [in Chinese] Guangxi Prev Med. 2002;8:110. [Google Scholar]
- 50.Xu YL, Hu RS, Li QZ. A case report of Strongyloides stercoralis infection [in Chinese] Chin J Clin Lab Sci. 2002;20:150. [Google Scholar]
- 51.Sheng YP, Deng YJ. A case report of lupus nephritis complicated with Strongyloides stercoralis infection [in Chinese] Chin J Parasitol Parasit Dis. 2002;20:367. [Google Scholar]
- 52.Wei YY. Lesson learned from strongyloidiasis misdiagnosis [in Chinese] Clin Misdiagnosis Mistherapy. 2002;15:31. [Google Scholar]
- 53.Zhang XM, Chang ZS, Chen SH, Zhang YN, Shi RZ. Morphological identification of filariform larvae and adult larvae in sputum from severe Strongyloides stercoralis infection patients [in Chinese] Chin J Parasitol Parasit Dis. 2002;20:253. [PubMed] [Google Scholar]
- 54.Zhang RY, Chen BJ, Lin JX. Ivermectin in intractable Strongyloides stercoralis infection [in Chinese] Strait J Preventive Med. 2002;8:79. [Google Scholar]
- 55.Zhao QL. A case report of Strongyloides stercoralis infection caused high fever [in Chinese] J Pract Paras Dis. 2002;10:92. [Google Scholar]
- 56.Lin FQ, Huang BP. A case report of Strongyloides stercoralis infection [in Chinese] J Clin Internal Med. 2002;19:201. [Google Scholar]
- 57.Lai C-P, Hsu Y-H, Wang J-H, Lin C-M. Strongyloides Stercoralis infection with bloody pericardial effusion in a non-immunosuppressed patient. Circ J. 2002;66:613–614. doi: 10.1253/circj.66.613. [DOI] [PubMed] [Google Scholar]
- 58.Zhao ZY, Liu JM. Strongyloides stercoralis infection: two cases and literature review [in Chinese] Guangxi Med J. 2001;23:645–647. [Google Scholar]
- 59.Sun YF, Li BL, Liu Y, Lu JL. A case of pulmonary strongyloidiasis [in Chinese] J Chin Antituberculosis Assoc. 2001;23:127. [Google Scholar]
- 60.Wu XX, Zheng ZX. Two cases of strongyloidiasis-related nephrotic syndrome [in Chinese] Chin J Nephrol. 2001;17:187. [Google Scholar]
- 61.Wei HX, Cai SX, Lu YD. Two cases of pulmonary strongyloidiasis [in Chinese] Med J Chin PLA. 2000;25:322. [Google Scholar]
- 62.Lin JX, Chen BJ, Zhang RY, Li YS, Lin CX. A case report of albendazole-resistant Strongyloides stercoralis infection [in Chinese] Chin J Parasitol Parasit Dis. 2000;18:188. [PubMed] [Google Scholar]
- 63.Ting YM. Pulmonary strongyloidiasis: case report of 2 cases. Kaohsiung J Med Sci. 2000;16:269–274. [PubMed] [Google Scholar]
- 64.Zhang MH. Three cases of Strongyloides stercoralis infection caused chronic intestinal obstruction death [in Chinese] Nat Med. 1999;30:158. [Google Scholar]
- 65.Zheng SL, Fang YP. A case report of fecal detection of Strongyloides stercoralis [in Chinese] Nei Mongol Med J. 1999;31:78. [Google Scholar]
- 66.Wong TY, Szeto CC, Lai FF, Mak CK, Li PK. Nephrotic syndrome in strongyloidiasis: remission after eradication with antihelmintic agents. Nephron. 1998;79:333–336. doi: 10.1159/000045058. [DOI] [PubMed] [Google Scholar]
- 67.Zhang RY, Chen BJ, Chen FL, Deng XX, Lin JX. A case report of severe Strongyloides stercoralis infection [in Chinese] Strait J Preventive Med. 1996;2:54. [Google Scholar]
- 68.Huang MS, Hwang KP, Chiang PC, Hwang JJ. Pulmonary hyperinfection with Strongyloides stercoralis. J Formos Med Assoc. 1996;95:551–554. [PubMed] [Google Scholar]
- 69.Liu XR. A case report of Strongyloides stercoralis infection in north China [in Chinese] Modern J Integrated TCM Western Med. 1995;4:19. [Google Scholar]
- 70.Li JL, Li XQ. A case report of duodenal drainage detection of Strongyloides stercoralis [in Chinese] Chin J Clin Lab Science. 1995;13:280. [Google Scholar]
- 71.Gao LS, Chen SL, You SY, Wang YW. A case report of fecal detection of male adult Strongyloides stercoralis [in Chinese] Chin J Schisto Control. 1994;6:115. [Google Scholar]
- 72.Lei CQ, Yu KG. A case report of parasitic Strongyloides stercoralis in intestinal and urinary system [in Chinese] Chin J Parasitol Parasit Dis (Special Issue) 1994;S1:251. [Google Scholar]
- 73.Chen JJ, Lee CM, Changchan CS. Duodenal Strongyloides stercoralis infection [in Chinese] Endoscopy. 1994;26:272. doi: 10.1055/s-2007-1008965. [DOI] [PubMed] [Google Scholar]
- 74.Dai SZ, Zhong ZY, Lin ZB, Zhu JY, Chen YH. Two cases of Strongyloides stercoralis infection [in Chinese] J Zhanjiang Med College. 1993;11:71–74. [Google Scholar]
- 75.Shi YZ, Weng XH, Xu ZY, Chang ZS. A case report of Strongyloides stercoralis infection [in Chinese] Shanghai Med J. 1991;14:59. [Google Scholar]
- 76.Guo RH. A case report of Strongyloides stercoralis infection caused chronic diarrhea over 20 years [in Chinese] Wuhan Med J. 1991;1:110. [Google Scholar]
- 77.Jiang SX, Jin CS, Qiu JB. A case report of Strongyloides stercoralis infection [in Chinese] J Zhenjiang Med College. 1991;1:68–69. [Google Scholar]
- 78.Liu GH, Peng J. Death report of a cortical hormone–induced severe Strongyloides stercoralis infection case [in Chinese] Chin J Parasitol Parasit Dis. 1990;8:143. [Google Scholar]
- 79.Li YX. Three cases of human Strongyloides stercoralis infection [in Chinese] Zhejiang Prac Med. 1990;6:15–16. [Google Scholar]
- 80.Xu XR. A case report of Strongyloides stercoralis infection [in Chinese] Chin J Parasitol Parasit Dis. 1989;7:75–76. [Google Scholar]
- 81.Cai GD, Song XS. A case report of severe Strongyloides stercoralis infection and Strongyloides stercoralis observation. Chin J Parasitol Parasit Dis. 1988;6:47. [Google Scholar]
- 82.Sun CX. A case report of fecal detection of male adult Strongyloides stercoralis in a rheumatic heart disease patient [in Chinese] Chin J Parasitol Parasit Dis. 1988;S1:121. [Google Scholar]
- 83.Zheng XH, Wang QL. A case of Strongyloides stercoralis infection attack [in Chinese] Bull Hunan Med College. 1988;13:149. [Google Scholar]
- 84.Liu GH. A case report of Strongyloides stercoralis–induced hemorrhagic enteritis and intestinal perforation. Chin J Parasitol Parasit Dis. 1987;5:237. [Google Scholar]
- 85.Liu G, Zhang RH. A case report of mixed infection of Hookworm, Hymenolepis nana and Strongyloides stercoralis [in Chinese] J Guangxi Med Univ. 1987;4:90. [Google Scholar]
- 86.Ran JB, Wan QH. Human Strongyloides stercoralis infection in China attached with a case report [in Chinese] Acta Acad Med Zunyi. 1986;9:47. [Google Scholar]
- 87.Han F, Xu S, Lin SW, Ding WG. A case report of severe Strongyloides stercoralis infection [in Chinese] Acta Universitatis Medicinalis Nanjing. 1985;5:289. [Google Scholar]
- 88.Chen ZC, Tian DL. A case report of Strongyloides stercoralis infection in urinary system [in Chinese] Nat Med J China. 1982;62:184. [Google Scholar]
- 89.Wu YJ. A case report of genitourinary tract infected with Strongyloides stercoralis [in Chinese] Hebei New Med. 1978;2:28–29. [Google Scholar]
- 90.Pathology Teaching and Research Group, Parasitology Teaching and Research Group, Internal Medicine Teaching and Research Group in Guangxi Medical University Two cases of severe Strongyloides stercoralis autoinfection [in Chinese] Chin J Intern Med. 1978;1:55–56. [Google Scholar]
- 91.Xie ZS. A case report of Strongyloides stercoralis caused chronic biliary tract infection. Nat Med. 1973;8((in Chinese)):400–401. [Google Scholar]
- 92.Wen JZ. Thirteen cases of strongyloidiasis. J Guangxi Normal Univ. 1979;2:70–74. 117. [Google Scholar]
- 93.Li SL. Twenty cases of Strongyloides stercoralis induced high fever [in Chinese] Chin J Schisto Control. 2001;13:241. [Google Scholar]
- 94.Tsai HC, Lee SS, Liu YC, Lin WR, Huang CK, Chen YS, Wann SR, Tsai TH, Lin HH, Yen MY, Yen CM, Chen ER. Clinical manifestations of strongyloidiasis in southern Taiwan. J Microbiol Immunol Infect. 2002;35:29–36. [PubMed] [Google Scholar]
- 95.Zhou L. Clinical nursing of 64 patients with Strongyloides stercoralis [in Chinese] J Trop Dis Parasitol. 2004;2:36. [Google Scholar]
- 96.Zhang CX. Report of 40 cases of Strongyloides stercoralis [in Chinese] Chin J Schisto Control. 2005;17:165. [Google Scholar]
- 97.Zhang RL, Liang Z, Cao AL, Zheng XY. Analysis of the examination results of 19 cases infected with Strongyloides stercoralis in Guangdong Province [in Chinese] J Trop Med. 2007;7:991. [Google Scholar]
- 98.Wu TC, Lei WY, Chen MC, Hu CT. Strongyloides stercoralis infection: a health issue regarding indigenous people in Taiwan. Trans R Soc Trop Med Hyg. 2012;106:468–472. doi: 10.1016/j.trstmh.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 99.Liu YF, Zhao BQ, Lu ZC. Prevalence of Strongyloides stercoralis at west mountain area in Guangxi Province [in Chinese] J Pract Paras Dis. 1997;5:48. [Google Scholar]
- 100.Guo JD, Zhao LL. Strongyloides stercoralis investigation among population at Yellow River flood area in the lower Yellow River [in Chinese] Chin J Parasitic Dis Contr. 2005;18:2–4. [Google Scholar]
- 101.Jiang JY, Du ZW, Wang XZ, Wang LB, Li LH. The investigation on the infection of Strongyloides stercoralis in Menghai County in Yunnan Province [in Chinese] J Pathogen Biol. 2008;3:202. [Google Scholar]
- 102.Olmos J, Gracia S, Villoria F, Salesa R, González-Macías J. Disseminated strongyloidiasis in a patient with acquired immunodeficiency syndrome. Eur J Intern Med. 2004;15:529–530. doi: 10.1016/j.ejim.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 103.Mendonça SC, Gonçalves-Pires Mdo R, Rodrigues RM, Ferreira A, Jr, Costa-Cruz JM. Is there an association between positive Strongyloides stercoralis serology and diabetes mellitus? Acta Trop. 2006;99:102–105. doi: 10.1016/j.actatropica.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 104.Kia EB, Rahimi HR, Mirhendi H, Nilforoushan MR, Talebi A, Zahabiun F, Kazemzadeh H, Meamar AR. A case of fatal strongyloidiasis in a patient with chronic lymphocytic leukemia and molecular characterization of the isolate. Korean J Parasitol. 2008;46:261–263. doi: 10.3347/kjp.2008.46.4.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhao WX. Beijing: People's Medical Publishing House; 1983. Human Parasitology [in Chinese] pp. 623–624. [Google Scholar]