Abstract
We conducted serological surveys for Coxiella burnetii in archived sera from patients that visited a rural clinic in western Kenya from 2007 to 2008 and in cattle, sheep, and goats from the same area in 2009. We also conducted serological and polymerase chain reaction-based surveillance for the pathogen in 2009–2010, in human patients with acute lower respiratory illness, in ruminants following parturition, and in ticks collected from ruminants and domestic dogs. Antibodies against C. burnetii were detected in 30.9% (N = 246) of archived patient sera and in 28.3% (N = 463) of cattle, 32.0% (N = 378) of goats, and 18.2% (N = 159) of sheep surveyed. Four of 135 (3%) patients with acute lower respiratory illness showed seroconversion to C. burnetii. The pathogen was detected by polymerase chain reaction in specimens collected from three of six small ruminants that gave birth within the preceding 24 hours, and in five of 10 pools (50%) of Haemaphysalis leachi ticks collected from domestic dogs.
Introduction
Q fever is a disease of humans caused by infection with the obligate intracellular bacterial pathogen, Coxiella burnetii. It is a zoonotic infection, typically transmitted from animal hosts to humans through inhalation of contaminated aerosols or ingestion of infected animal products such as milk or cheese.1 Ticks have also been implicated as vectors, and over 40 species of ticks have been found naturally infected with the agent.1 Coxiella burnetii has a wide host range, including wild and domestic mammals, birds, reptiles, and arthropods.2 Domestic ruminants (primarily goats, cattle, and sheep) represent the most frequent source of human infection,3 although transmission from dogs and cats is also documented.4,5 The uterus and mammary glands of female animals are sites of chronic C. burnetii infection, and infected females may shed large amounts of bacteria into the environment during parturition or spontaneous abortion.2 Once shed, the organisms may remain infective in the environment for several months.1
Infection in humans, usually by inhalation, may be asymptomatic (up to 60% of infected individuals) or may manifest clinically after an incubation period ranging between 1 and 3 weeks.1,6 Clinical signs of acute Q fever include fever of 2–14 days' duration, atypical pneumonia, and/or hepatitis.1 Although the disease is typically self-limiting, severe debilitating illness requiring hospitalization can occur in a small proportion (2–5%) of acutely infected cases.6 Chronic disease may develop following infection, particularly in patients with predisposing conditions such as preexisting cardiac valvulopathy, pregnancy, or immunosuppression.1 Common manifestations of chronic disease include endocarditis and vascular infection.1 Coxiella burnetii displays antigenic (phase) variation associated with loss of virulence and mutational variation in the lipopolysaccharide.1 High levels of antibodies to phase I antigens are detected during chronic Q fever, whereas antibodies to phase II antigens are produced in acute disease.6
Coxiella burnetii is found worldwide, with the exception of New Zealand.7 A recent large outbreak in the Netherlands involved at least 3,523 human cases from 2007 through 2009,8 and was characterized by a high rate of hospitalization, with 20% of notified cases admitted to hospital in 2008–2009.9 Pneumonia was the predominant clinical presentation.8 The Netherlands outbreak has been linked to the increase in the country's dairy goat population, which more than doubled in size between 2000 and 2009, and highlights the public health risks of Q fever epidemics posed by domestic ruminants.
Despite the high-profile nature of some Q fever outbreaks, and the attention that C. burnetii has received as a potential bioterrorism agent,10 information on the prevalence of infection in sub-Saharan Africa is scant.11,12 In Kenya, serological evidence of Q fever in patients with acute febrile and respiratory illness was shown in the 1950s.13 Other studies showed the prevalence of antibodies to C. burnetii among Kenyans to range between 10% and 20%.14,15 A more recent investigation found that four people (8%) of a group of 50 travelers to Kenya contracted Q fever,16 and in another recent study investigators diagnosed acute Q fever in 5% of febrile patients admitted to two hospitals from September 2007 to August 2008, in neighboring northern Tanzania.17 Among domestic ruminants in Kenya, the prevalence of antibodies was reported as 7–57% in cattle and 33–34% in goats.14,15,18,19 There are no other recent reports of investigations into disease prevalence in resident human or livestock populations, or any information on the relationship between prevalence in human and animal populations.
The establishment of a population-based infectious disease surveillance program in western Kenya20 provided a valuable opportunity for generating domestic animal prevalence data that could be linked with human health outcomes. To assess the current status of Q fever among humans and infection prevalence in domestic ruminants, we conducted surveys for C. burnetii in cattle, goats, sheep, and ticks in this rural agro-pastoral community, and tested specimens from human patients presenting to a clinic in the same area for Q fever.
Materials and Methods
Study site.
All data were collected in Asembo within Rarieda (formerly Bondo) District in western Kenya in 2007–2010. This rural site on the eastern shore of Lake Victoria falls within a health and demographic surveillance system (HDSS) that has been run by the Kenya Medical Research Institute (KEMRI) and U.S. Centers for Disease Prevention and Control (CDC) since 2001. The HDSS collects household demographic and socioeconomic data three times per year, and includes information on the number of livestock owned.21 Households are clustered into compounds composed of related family units, with most compounds having between one and five family units.22 The primary economic activity is subsistence smallholder agro-pastoralism and fishing. In this area, 44% of households own cattle (mean number owned: 1.84) and 43% own at least one sheep or goat (mean number owned: 2.12; HDSS data for 2008, unpublished).
The Kenyan International Emerging Infections Program of KEMRI/CDC has conducted population-based infectious disease surveillance (PBIDS) of people in Asembo since late 2005, with between 23,500 and 25,000 people under surveillance in 33 villages.20 Participants enrolled in PBIDS have household visits to determine health status every 2 weeks, and receive free medical care for all acute illnesses at a centrally located clinic, St. Elizabeth Lwak Mission Hospital (henceforth Lwak Hospital). Specimen collection and diagnostic testing are focused on determining etiologies for four infectious disease syndromes, namely acute respiratory infection, diarrhea, jaundice, and febrile illness. Sera are collected from patients participating in PBIDS presenting to Lwak Hospital and meeting case definitions for acute respiratory illness, jaundice or acute febrile illness,20 or who are hospitalized for any non-traumatic illness. Between January 2007 and January 2010, 3,948 serum specimens were collected and archived at −80°C at the KEMRI/CDC laboratory in Kisumu.
Ethical review.
The collection of specimens from humans was approved by the KEMRI Ethical Review Committee (protocol no. 932) and CDC Institutional Review Board (protocol no. 4566), and from animals by the KEMRI and CDC Animal Care and Use Committees (protocol no. 1191 and 1562BRETBDX, respectively). Written informed consent was obtained from all patients or animal owners before specimen collection.
Human serosurvey.
To assess previous exposure to C. burnetii in humans, we retrospectively examined a subset of archived sera. Sera collected from January 2007 through February 2008 were identified and 248 specimens randomly selected from this period (sufficient to attain a 95% confidence interval with an absolute precision of 5% at an expected prevalence of 20%).23 Sera were tested at the KEMRI/CDC laboratory in Kisumu for IgG antibodies against phase I and phase II C. burnetii antigens derived from the Nine Mile strain, using an indirect fluorescence antibody (IFA) assay (Fuller Laboratories, Fullerton, CA). Serum specimens were screened at a dilution of 1:32. A positive and a negative control were included for each assay run, and all slides were read by a single operator. A sample was considered positive if bright, sharply defined apple-green fluorescent elementary bodies were observed against a background of red counterstained material at this serum dilution.
Human respiratory patients.
Under the PBIDS clinic surveillance protocol, blood specimens are collected from patients who meet the case definition for acute lower respiratory infection (ALRI). This is defined in persons 5 years of age or older as cough, difficulty breathing or chest pain and either documented axillary temperature ≥ 38.0°C or oxygen saturation < 90%, and in children under 5 years of age as cough or difficulty breathing with one of the following: elevated respiratory rate for age (non-severe pneumonia),20 or lower chest wall indrawing, stridor, oxygen saturation < 90%, maternal report of convulsions, inability to drink or breastfeed, or vomiting everything, or on exam lethargy or unconsciousness (severe and very severe pneumonia).20 All patients who meet the case definition have acute-phase sera collected and archived at the time of presentation, and patients are requested to return to the clinic after 4–6 weeks for the collection of convalescent-phase serum specimens. Paired sera are tested serologically for a range of respiratory pathogens.
To determine the prevalence of C. burnetii infection in these patients with respiratory illness, we retrospectively identified paired serum specimens collected from ALRI cases occurring from July 2009 through January 2010. Convalescent-phase serum specimens were screened for IgG antibodies against C. burnetii phase II antigen by indirect enzyme-linked immunosorbent assay (ELISA) (Panbio, Brisbane, Australia) using the manufacturer's recommended cutoff. End-point titers of IgG antibodies in acute and convalescent sera were determined by IFA assay for all pairs in which the convalescent-phase tested positive or equivocal on ELISA, with serial dilutions starting from 1:16. The operator who performed the IFA was blind to the status (acute or convalescent) of the specimen. A ≥ 4-fold increase in IFA titer to C. burnetii phase II antigen defined acute Q fever, and a titer ≥ 1:1,024 to C. burnetii phase I antigen in either acute- or convalescent-phase sera defined possible chronic Q fever.
Domestic ruminants cross-sectional study.
Data were collected from January through May 2009. The study population comprised all domestic ruminants (cattle, goats, and sheep) living within compounds in the 33 villages of the PBIDS. The sampling frame was compiled from data on the number of each species of domestic animal within the compounds, as reported at the most recent HDSS visit for which data were available. Three hundred livestock-owning compounds (LOCs) were randomly selected from the sampling frame of 4,528 LOCs, with a LOC defined by ownership of one or more animals of any of the following species: cattle, sheep, goats, chickens. The heads of the selected compounds were approached and offered enrollment. If livestock were no longer owned, replacement LOCs was then randomly selected from the same village.
Specimens were collected from a maximum of three randomly selected animals of any age from each of the species of domestic ruminants present at enrolled compounds. Blood was collected by venipuncture of the jugular vein into plain vacutainers (BD, Franklin Lakes, NJ). Vaginal swabs were collected from adult females only, using nylon flocked swabs (eSwabs, Copan Innovation, Brescia, Italy) and placed in universal transport medium (Copan Innovation). Blood collection tubes were kept at ambient temperature for 15–30 minutes, and then transported to the field laboratory on ice with the vaginal swabs. At the field laboratory, blood tubes were centrifuged at 2,000–3,000 revolutions per minute for 7–10 minutes, and serum pipetted into cryovials. Sera and swabs were then transported on ice to the KEMRI-CDC laboratory and stored at −80°C until testing. Ruminant serum samples were tested for the presence of IgG antibodies to C. burnetii by indirect ELISA (Chekit Q fever ELISA, IDEXX), following the manufacturer's instructions. DNA was extracted from vaginal swab specimens using QIAamp DNA Mini Kit (Qiagen, Valencia, CA) in a biosafety level 3 laboratory, and tested by quantitative real-time polymerase chain reaction (qPCR) assay using the IS1111 gene target for C. burnetii, as previously described.24
Domestic ruminant births/abortions.
To further investigate shedding of C. burnetii by domestic ruminants, we conducted surveillance for births and abortions in the ruminant population in the PBIDS area during 1 week in August 2009, as part of a pilot study for a larger surveillance program on animal disease syndromes. A network of animal health reporters (AHRs) was established in the 33 villages in the PBIDS (1–2 AHRs per village), through which all livestock owners could report births or abortions in their ruminant herds. The AHRs then contacted the study field veterinary team by mobile phone, who responded to the case as soon as possible. Available samples were collected by the veterinary team, including blood and vaginal swabs from dams, placenta, and liver, lungs, spleen, and brain of aborted fetuses or stillborn animals. DNA was extracted and tested as described previously.
Collection of arthropods.
All domestic ruminants from which blood was collected were also inspected for ticks. In addition and when present, up to three domestic dogs in each enrolled compound were also inspected. In each animal, we examined specific body sites (ruminants: ear, dewlap, shoulder, belly, groin, udder, and perineum; dogs: ear, neck, nape, belly, and groin) and collected 1–2 non-engorged adult ticks of different genera per site (although only Amblyomma ticks were tested from ruminants). Ticks were preserved in 70% ethanol at room temperature until delivery to the laboratory, and then stored in ethanol at −80°C. Ticks were pooled by individual host animal and tick species (1–6 ticks per pool). Ticks of the genus Amblyomma collected from ruminants and all ticks collected from dogs were identified using published entomological keys25; after identification, ticks were washed in molecular-grade water and mechanically disrupted using a bead mill (Qiagen TissueLyser LT). Genomic DNA was extracted using QIAamp blood and tissue kits (Qiagen) according to the manufacturer's instructions, using a final elution volume of 100 μL, and tested by IS1111 qPCR.24
Results
Human serosurvey.
A total of 248 and 246 archived sera were tested by IFA for IgG antibodies against C. burnetii phase I and phase II antigen, respectively. The IgG antibodies against C. burnetii phase I antigen were detected in 58 specimens (23.4%, exact binomial 95% confidence intervals [CI]: 18.3–29.2%), and IgG antibodies against phase II antigen were detected in 76 specimens (30.9%, 95% CI: 25.2–37.1%). All the specimens that reacted with phase I antigen also reacted with phase II antigen.
Human respiratory patients.
Of 2,246 patients who met the case definition for ALRI from July 2009 through January 2010, 493 (22%) returned for collection of convalescent sera. Of these, 135 pairs were available for testing. Convalescent-phase sera were screened for IgG antibodies against C. burnetii phase II antigen by indirect ELISA. Nineteen patients (14.1% of ALRI patients, 95% CI: 8.7–21.1%) had positive titers on ELISA. Of these, 4 (3% of ALRI patients, 95% CI: 0.8–7.4%) were diagnosed serologically with acute Q fever by IFA as determined by a ≥ 4-fold rise between acute and convalescent sera. All four patients were males, 7–31 years of age, who presented with fever (documented axillary temperatures of 38.2–39.5°C), chills, cough, and headache (Table 1). The reported duration of illness ranged from 2 to 10 days. All four patients were from households that owned one or more domestic ruminants around the time of illness. One of the patients (#2 in Table 1) also showed seroconversion to influenza B virus. No patients were diagnosed with possible chronic Q fever.
Table 1.
Clinical features of four patients from rural western Kenya with acute lower respiratory illness, diagnosed serologically with acute Q fever
| Patient no. | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Sex | Male | Male | Male | Male |
| Age (years) | 31 | 22 | 10 | 7 |
| Fever? | Y | Y | Y | Y |
| Axillary temperature | 38.3°C | 38.7°C | 38.2°C | 39.5°C |
| Chills? | Y | Y | Y | Y |
| Cough? | Y | Y | Y | Y |
| Headache? | Y | Y | Y | Y |
| Difficulty breathing? | N | N | N | N |
| Sneezing? | N | N | N | Y |
| Sore throat? | Y | N | N | N |
| Ear problems? | N | N | N | N |
| Diarrhea? | N | N | N | N |
| Abdominal pain? | N | N | N | N |
| Vomiting? | N | N | Y | Y |
Domestic ruminants cross-sectional study.
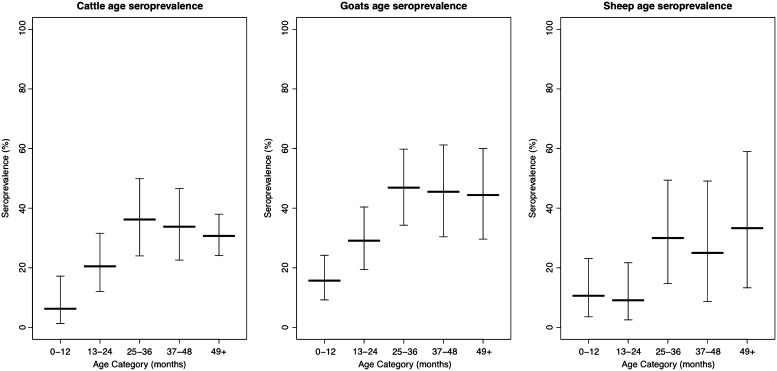
Of the 300 LOCs identified, 236 owned one or more species of domestic ruminant. ELISA results were obtained for sera from 463 cattle, 378 goats, and 159 sheep in these compounds. The seroprevalence of antibodies to C. burnetii, was 28.3% (95% CI: 24.2–32.6%) in cattle, 32% (95% CI: 27.3–37%) in goats, and 18.2% (95% CI: 12.6–25.1%) in sheep. The age-stratified seroprevalence results for the three species are given in Figure 1. Coxiella burnetii DNA was detected by IS1111 PCR in vaginal swabs from 5 of 233 (2.1%) cattle, 5 of 222 (2.3%) goats, and 4 of 85 (4.7%) sheep.
Figure 1.
Age-stratified seroprevalence of IgG antibodies to Coxiella burnetii in sera collected from cattle, goats, and sheep in western Kenya from January through May 2009. The three panels show the age seroprevalence in cattle, goats, and sheep, respectively. Within each panel, bold horizontal bars indicate the mean seroprevalence in each age class and the vertical bars show the 95% confidence intervals for these estimates.
Domestic ruminant births/abortions.
Six births (five in goats and one in a sheep) and one abortion in a cow were detected during the week-long surveillance. In all cases, specimens were collected within 24 hours of the event. Three births in goats resulted in one stillborn kid in each, along with one to two live offspring. Samples from the placenta of one of these cases, and vaginal swabs from a sheep and a goat in the same compound that gave birth on consecutive days, were positive for C. burnetii on the qPCR assay for the IS1111 gene target.
Arthropods.
A total of 258 adult Amblyomma variegatum ticks were collected from 162 cattle in the study area, and pooled by individual host. Coxiella burnetii DNA was detected by IS1111 PCR in 4 of 162 (2.5%) pools. In dogs, 102 ticks were collected from 36 animals, resulting in pools of the following species: Rhipicephalus sanguineus (15 pools), Rhipicephalus appendiculatus (9 pools), unspeciated Rhipicephalus (10 pools), A. variegatum (10 pools), Haemaphysalis leachi (10 pools), and Rhipicephalus (Boophilus) decoloratus (5 pools). The number (and percent) of pools positive using the IS1111 PCR assays were: Rh. sanguineus 2 (20%), Rh. appendiculatus 1 (11.1%), unspeciated Rhipicephalus 2 (20%), A. variegatum 2 (20%), H. leachi 5 (50%), and Rh. (Boophilus) decoloratus 1 (20%).
Discussion
We identified Q fever as a possible cause of acute lower respiratory illness among rural residents in western Kenya. In addition, we found a high prevalence of antibodies to C. burnetii in domestic ruminants in the same area, with high rates of shedding of the organism shortly after parturition in a small sample of animals.
The prevalence of antibodies to C. burnetii in patients attending Lwak Hospital is similar to that reported in several population-based studies elsewhere in sub-Saharan Africa (17–37%),12,26,27 indicating high levels of exposure to the pathogen. In addition to the recent study in northern Tanzania in which acute Q fever was diagnosed in 5.0% of febrile inpatients,17 another study reported recent infection with C. burnetii in 9.5% of febrile patients > 5 years of age in two urban areas in Mali.28 A literature review did not identify any recent investigations of Q fever as a cause of respiratory illness in Africa, although in the report of Q fever in travelers returning from Kenya,16 the two symptomatic patients both had respiratory involvement.
In addition to ALRI, it is likely that Q fever also contributes to the burden of acute febrile illness in patients in our study area. Both ALRI and febrile illness are managed empirically in this setting, due largely to a lack of reliable rapid diagnostic tests for diseases other than malaria. Although malaria may be responsible for > 50% of febrile illness episodes in this holoendemic area,29 knowledge of the full range of prevalent etiologies is important to improve the empiric treatment of this syndrome. Doxycycline is considered the preferred antibiotic for the treatment of acute Q fever,1 and there is evidence that newer macrolides and fluoroquinilones are also effective.30 Notably, C. burnetii is resistant in vitro to those antimicrobial agents that are typically used for the empirical treatment of ALRI in Kenya (penicillin and its derivatives, and aminoglycosides).1 A diagnosis of Q fever pneumonia should therefore be considered in patients not responding to first-line antimicrobial therapy, particularly in those with exposure to known risk factors.
Inhalation of fomites contaminated by the parturient fluids of infected animals is the main mode of human infection with C. burnetii.3 Despite a very small sample, a high proportion of small ruminants in our study were found to shed the pathogen at parturition (2 of 5 goats and 1 of 1 sheep sampled).The stratified age-seroprevalence curves in ruminants show an increase in prevalence with age until around 2–3 years, followed by a plateau. This pattern has been observed elsewhere31 and is consistent with cumulative exposure to the pathogen from a young age, with the highest prevalence of antibody in reproductively mature animals.
Coxiella burnetii was detected by PCR in all species of ticks studied. Ticks become infected during the transient bacteremia that occurs in the vertebrate host early after infection. In our study, the highest prevalence of infection with C. burnetii was found in H. leachi (the yellow dog tick), one of two ticks adapted to feeding on domestic dogs in tropical and sub-tropical areas. Detection of C. burnetii in this species has been reported in Kenya previously32; these findings suggest that domestic dogs may play a role as reservoir hosts and sources of human infection with C. burnetii in Kenya, as has been reported elsewhere.5
Our findings show that Q fever is a significant yet under-diagnosed cause of human respiratory illness in Kenya. Domestic ruminants are sources of human infection, through direct contact or contamination of the environment during parturition or abortion. Although not assessed in this study, consumption of dairy products from infected ruminants is also likely to pose a risk. Although risk factor studies would be helpful to identify the principal modes of transmission to humans in this setting, our results support the likely efficacy of recognized public health and hygiene measures for mitigating the risk of transmission from domestic ruminants, such as confinement of domestic animals during parturition, avoidance of contaminated pastures and contact with placental material, and boiling or pasteurization of milk before consumption. This study also suggests that investigation of the role of domestic dogs and tick-borne transmission is warranted to identify potential sources of infection and risk factors that are currently not well recognized.
ACKNOWLEDGMENTS
We thank the IEIP-Z field team (Samuel Asembo, Michael Otieno, James Oyigo, and Pauline Otieno) for the collection of ticks and specimens from domestic animals, and Immaculate Amadi and Catherine Sonye for assistance with laboratory testing.
Disclaimer: The findings and conclusions are those of the authors. They do not necessarily represent the official policy or position of the Centers for Disease Control and Prevention, the Department of the Navy, Department of Defense, or the U.S. Government.
Footnotes
Financial support: This research was supported by the Wellcome Trust, UK (grant no. 081828/B/06/Z) and U.S. Centers of Disease Control and Prevention and Global Emerging Infections Surveillance and Response System Program (work unit no. 188M.0931.001.A0074).
Authors' addresses: Darryn L. Knobel, Department of Veterinary Tropical Diseases, Faculty of Veterinary Science, University of Pretoria, Onderstepoort, South Africa, E-mail: darryn.knobel@up.ac.za. Alice N. Maina and Allen L. Richards, Viral and Rickettsial Diseases Department, Naval Medical Research Center, Silver Spring, MD, E-mails: alicemaina727@gmail.com and allen.richards@med.navy.mil. Sally J. Cutler, School of Health, Sports and Bioscience, University of East London, United Kingdom, E-mail: S.Cutler@uel.ac.uk. Eric Ogola and Muthoni Junghae, Kenya Medical Research Institute, Centers for Disease Control and Prevention-Kenya, International Emerging Infections Program, Kenya, E-mails: EOgola@kemricdc.org and mjunghae@ke.cdc.gov. Daniel R. Feikin, Johns Hopkins Bloomberg School of Public Health and Centers for Disease Control and Prevention, Baltimore, MD, E-mail: dfeikin@jhsph.edu. Jo E. B. Halliday and Sarah Cleaveland, Institute of Biodiversity, Animal Health and Comparative Medicine, College of Medical, Veterinary and Life Sciences, University of Glasgow, United Kingdom, E-mails: jo.halliday@glasgow.ac.uk and sarah.cleaveland@glasgow.ac.uk. Robert F. Breiman, International Emerging Infections Program, Global Disease Detection Division, Centers for Disease Control and Prevention, Kenya, E-mail: rbreiman@ke.cdc.gov. M. Kariuki Njenga, Integrated Human-Animal Health Program, Global Disease Detection Division, Centers for Disease Control and Prevention, Kenya, E-mail: knjenga@ke.cdc.gov.
References
- 1.Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12:518–553. doi: 10.1128/cmr.12.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babudieri B. Q fever: a zoonosis. Adv Vet Sci. 1959;5:81–182. [Google Scholar]
- 3.Marrie TJ. Epidemiology of Q fever. In: Marrie TJ, editor. Q Fever: The Disease. Vol. 1. Boca Raton, FL; CRC Press, Inc.: 1990. pp. 49–70. [Google Scholar]
- 4.Langley JM, Marrie TJ, Covert A, Waag DM, Williams JC. Poker players' pneumonia. An urban outbreak of Q fever following exposure to a parturient cat. N Engl J Med. 1988;319:354–356. doi: 10.1056/NEJM198808113190607. [DOI] [PubMed] [Google Scholar]
- 5.Buhariwalla F, Cann B, Marrie TJ. A dog-related outbreak of Q fever. Clin Infect Dis. 1996;23:753–755. doi: 10.1093/clinids/23.4.753. [DOI] [PubMed] [Google Scholar]
- 6.Raoult D, Marrie T, Mege J. Natural history and pathophysiology of Q fever. Lancet Infect Dis. 2005;5:219–226. doi: 10.1016/S1473-3099(05)70052-9. [DOI] [PubMed] [Google Scholar]
- 7.Hilbink F, Penrose M, Kovacova E, Kazar J. Q fever is absent from New Zealand. Int J Epidemiol. 1993;22:945–949. doi: 10.1093/ije/22.5.945. [DOI] [PubMed] [Google Scholar]
- 8.Roest HI, Tilburg JJ, van der Hoek W, Vellema P, van Zijderveld FG, Klaassen CH, Raoult D. The Q fever epidemic in the Netherlands: history, onset, response and reflection. Epidemiol Infect. 2011;139:1–12. doi: 10.1017/S0950268810002268. [DOI] [PubMed] [Google Scholar]
- 9.van der Hoek W, Dijkstra F, Schimmer B, Schneeberger PM, Vellema P, Wijkmans C, ter Schegget R, Hackert V, van Duynhoven Y. Q fever in the Netherlands: an update on the epidemiology and control measures. Euro Surveill. 2010;15:19520. [PubMed] [Google Scholar]
- 10.Madariaga MG, Rezai K, Trenholme GM, Weinstein RA. Q fever: a biological weapon in your backyard. Lancet Infect Dis. 2003;3:709–721. doi: 10.1016/s1473-3099(03)00804-1. [DOI] [PubMed] [Google Scholar]
- 11.Tissot-Dupont H, Brouqui P, Faugere B, Raoult D. Prevalence of antibodies to Coxiella burnetii, Rickettsia conorii, and Rickettsia typhi in 7 African countries. Clin Infect Dis. 1995;21:1126–1133. doi: 10.1093/clinids/21.5.1126. [DOI] [PubMed] [Google Scholar]
- 12.Mediannikov O, Fenollar F, Socolovschi C, Diatta G, Bassene H, Molez JF, Sokhna C, Trape JF, Raoult D. Coxiella burnetii in humans and ticks in rural Senegal. PLoS Negl Trop Dis. 2010;4:e654. doi: 10.1371/journal.pntd.0000654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Craddock AL, Gear J. Q fever in Nakuru, Kenya. Lancet. 1955;269:1167–1169. doi: 10.1016/s0140-6736(55)92898-1. [DOI] [PubMed] [Google Scholar]
- 14.Brotherson JC, Cooke ER. Q fever in Kenya. East Afr Med J. 1956;33:125–130. [PubMed] [Google Scholar]
- 15.Vanek E, Thimm B. Q fever in Kenya. Serological investigations in man and domestic animals. East Afr Med J. 1976;53:678–684. [PubMed] [Google Scholar]
- 16.Potasman I, Rzotkiewicz S, Pick N, Keysary A. Outbreak of Q fever following a safari trip. Clin Infect Dis. 2000;30:214–215. doi: 10.1086/313613. [DOI] [PubMed] [Google Scholar]
- 17.Prabhu M, Nicholson WL, Roche AJ, Kersh GJ, Fitzpatrick KA, Oliver LD, Massung RF, Morrissey AB, Bartlett JA, Onyango JJ, Maro VP, Kinabo GD, Saganda W, Crump JA. Q fever, spotted fever group, and typhus group rickettsioses among hospitalized febrile patients in northern Tanzania. Clin Infect Dis. 2011;53:e8–e15. doi: 10.1093/cid/cir411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown RD. Q fever-veterinary aspects. East Afr Med J. 1956;33:441–445. [PubMed] [Google Scholar]
- 19.Gossler R, Leyk W, Hunermund G. Serological studies in cattle in the Kabete area (Kenya). 1. Occurrence of antibodies against parainfluenza 3, IBR-, BDD-virus, Chlamydia and Coxiella burnetii. Berl Munch Tierarztl Wochenschr. 1973;86:164–166. [PubMed] [Google Scholar]
- 20.Feikin DR, Olack B, Bigogo GM, Audi A, Cosmas L, Aura B, Burke H, Njenga MK, Williamson J, Breiman RF. The burden of common infectious disease syndromes at the clinic and household level from population-based surveillance in rural and urban Kenya. PLoS ONE. 2011;6:e16085. doi: 10.1371/journal.pone.0016085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adazu K, Lindblade KA, Rosen DH, Odhiambo F, Ofware P, Kwach J, Van Eijk AM, Decock KM, Amornkul P, Karanja D, Vulule JM, Slutsker L. Health and demographic surveillance in rural western Kenya: a platform for evaluating interventions to reduce morbidity and mortality from infectious diseases. Am J Trop Med Hyg. 2005;73:1151–1158. [PubMed] [Google Scholar]
- 22.Bigogo G, Audi A, Aura B, Aol G, Breimazn RF, Feikin DR. Health-seeking patterns among participants of population-based morbidity surveillance in rural western Kenya: Implications for calculating disease rates. Int J Infect Dis. 2010;14:e967–e973. doi: 10.1016/j.ijid.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 23.Thrusfield M. Veterinary Epidemiology. Oxford: Blackwell Science, Ltd.; 1995. p. 182. [Google Scholar]
- 24.Klee SR, Tyczka J, Ellerbrok H, Franz T, Linke S, Baljer G, Appel B. Highly sensitive real-time PCR for specific detection and quantification of Coxiella burnetii. BMC Microbiol. 2006;6:2. doi: 10.1186/1471-2180-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walker AR, Bouattar A, Camicas JL, Estrada-Pena A, Horak IG, Latif AA, Pegram RG, Preston PM. Ticks of Domestic Animals in Africa: A Guide to Identification of Species. Edinburgh; Bioscience Reports: 2003. [Google Scholar]
- 26.Kelly PJ, Matthewman LA, Mason PR, Raoult D. Q fever in Zimbabwe. A review of the disease and the results of a serosurvey of humans, cattle, goats and dogs. S Afr Med J. 1993;83:21–25. [PubMed] [Google Scholar]
- 27.Kobbe R, Kramme S, Kreuels B, Adjei S, Kreuzberg C, Panning M, Adjei O, Fleischer B, May J. Q fever in young children, Ghana. Emerg Infect Dis. 2008;14:344–346. doi: 10.3201/eid1402.070971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steinmann P, Bonfoh B, Peter O, Schelling E, Traore M, Zinsstag J. Seroprevalence of Q fever in febrile individuals in Mali. Trop Med Int Health. 2005;10:612–617. doi: 10.1111/j.1365-3156.2005.01420.x. [DOI] [PubMed] [Google Scholar]
- 29.Phillips-Howard PA, Nahlen BL, Alaii JA, ter Kuile FO, Gimnig JE, Terlouw DJ, Kachur SP, Hightower AW, Lal AA, Schoute E, Oloo AJ, Hawley WA. The efficacy of permethrin-treated bed nets on child mortality and morbidity in western Kenya I. Development of infrastructure and description of study site. Am J Trop Med Hyg. 2003;68:3–9. [PubMed] [Google Scholar]
- 30.Morovic M. Q fever pneumonia: are clarithromycin and moxifloxacin alternative treatments only? Am J Trop Med Hyg. 2005;73:947–948. [PubMed] [Google Scholar]
- 31.McCaughey C, Murray LJ, McKenna JP, Menzies FD, McCullough SJ, O'Neill HJ, Wyatt DE, Cardwell CR, Coyle PV. Coxiella burnetii (Q fever) seroprevalence in cattle. Epidemiol Infect. 2010;138:21–27. doi: 10.1017/S0950268809002854. [DOI] [PubMed] [Google Scholar]
- 32.Heisch RB, Grainger WE, Harvey AE, Lister G. Feral aspects of rickettsial infections in Kenya. Trans R Soc Trop Med Hyg. 1962;56:272–286. doi: 10.1016/0035-9203(62)90048-2. [DOI] [PubMed] [Google Scholar]