Abstract
Epidural abscess of the spinal column is a rare condition that can be fatal if left untreated. It promptly progresses and can cause neurologic paralysis, urinary retention or cauda equina syndrome. Compromised immune system that occurs in patients with diabetes mellitus, AIDS, chronic renal failure, alcoholism, or cancer is a predisposing factor. It mostly occurs in adults. Here we would like to report a case of spontaneous pyogenic lumbar epidural abscess with neurological deficit diagnosed in a 15 year old boy. We treated this case successfully with surgical microscopic decompression and drainage.
Keywords: Spinal infection, Spinal epidural abscess, Antibiotics, Spinal surgery
Introduction
Spinal epidural abscess (SEA) is a very rare disease and occurs at an incidence rate of 0.2 to 2.8 cases per 10000 hospital admissions (1–3). The most important factors involved are spinal surgery, recent trauma, immunosuppression, a distal site of infection, intravenous drug use, diabetes mellitus and alcoholism (4–6). However, 20% of patients will have no clear predisposing factor (7). Back pain and fever are two common complaints in the emergency department that are always missed (7). SEA represents a spinal emergency condition and a potentially life-threatening disease that can cause severe neurological deficits due to the compressive effect of abscess on the spinal co rd or nerve roots or ischemia (7). The neurological deficit can be as severe as paralysis. In this report we will present a case of 15 year old boy with spontaneous pyogenic epidural abscess.
Case report
A 15 year old boy presented to orthopedic clinic with a 2 week history of urinary retention, back pain, bilateral leg numbness and weakness, lumbar pain exacerbated by movement, sweat and fever. He had received conservative medical treatment with a diagnosis of low back pain but there was no response to analgesic and medical treatment. He had also referred to urologist due to his urinary retention. Ultra-sonograohy of bladder and kidneys detected no abnormal finding. He was then discharged after urinary catheterization with an unexplained diagnosis of urinary retention. His lower back pain was exacerbated and severe neurological deficit was also added to his clinical picture. He also developed difficulty in weight bearing and walking. His past medical history was not significant. He denied any previous trauma, spinal surgery, or immunodeficiency. He was not taking any medication. In physical examination, he presented with blood pressure of 100/80 mmHg, pulse rate of 100 pulse/minute and a body temperature of 38.5º C. Hematologic examination revealed a white blood cell count of 18600 /µl (neutrophil 70%), an erythrocyte sedimentation rate (ESR) of 68 mm/hr and a C reactive protein 3-plus positive.
On physical examination, there was a tenderness over the left side of lumbar vertebrae and on the left and right sides of para-lumbar region. Neurological examination showed hyperactive deep tendon reflexes, muscle weakness (3/5), and decreased pin prick sensation in the right leg. Rectal tone and sensation were normal but there was a perineal numbness.
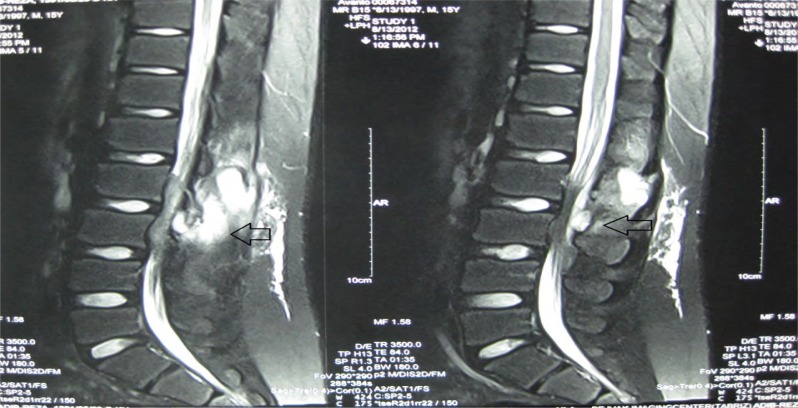
Radiologic imaging showed no significant evidence (Fig. 1). On magnetic resonance imaging (MRI) scan that were taken at the time of admission there were abnormal signal intensity at right paraspinal muscles of L2 and L3 level. The lesion was extended to the posterior aspect of thecal sac and its extra-dural mass effect caused canal stenosis and cauda equina compression to anterior wall of the canal. Radiologist recommended emergent laminectomy and debulking of the canal (Figs. 2, 3).
Fig. 1.
Lateral lumbosacral radiography of the 15 year old boy presented.
Fig. 2.
Magnetic Resonance Imaging (MRI) of lumbar vertebra detected an intensity in paralumbar of L2 and L3 (arrow).
Fig. 3.
Canal stenosis and compressed cauda equina in MRI due to spinal epidural abscess.
Immediately the patient underwent surgical operation. Abscess drainage and L2 and L3 laminectomy were done under microscopic surgery. Surgical finding was a yellow colored abscess-like fluid under yellow ligament. Culture testwas positive for Staphylococcus aurous. Following the operation, all the symptoms disappeared and neurological deficit were resolved.
Intravenous antibiotic (cefazolin 1gr) was administered for two postoperative weeks then oral antibiotic (cephalexin 500 mg every 6 hours) were continued for 4 weeks. After 6 weeks from the time of operation, white blood cell (WBC) counts, ESR and CRP were all found to be normal. On a three month follow-up period there was no recurrence and the patient was returned to his normal life.
Discussion
Epidural Abscess is a significant diagnostic challenge. Its diagnosis must be made promptly because delay in treatment can result in irreversible neurologic damage or even death (3). Paralysis and death occur in 16% and 15% of patients respectively (8). Progression of neurological deficit can vary from few hours to several months (3, 8). Clinical feature of the problem might be nonspecific. Back pain in initial stages can lead to a missed diagnosis in spontaneous cases (9). Radiological modalities are most common diagnostic devices used for detection of abscess within spinal vertebra, but radiographic imaging is not much helpful. Magnetic resonance imaging with a sensitivity of 91% is now considered the diagnostic gold standard (9).We found Staphylococcus aureus on culture, similar to previous reports (8). Early recognition and high clinical suspicion before development of symptoms will yield to excellent results. Surgical decompression remains the mainstay of treatment for spinal epidural abscess (2). Endoscopy-assisted surgery and percutaneous drainage are also reported to be successful treatment modalities (2).
Conclusion
According to our report, spinal epidural abscess is one of the most important differential diagnosis of acute back pain in patients without a positive history. Careful physical examination and attention to the neurological symptoms can help in diagnosis. Early surgical treatment can prevent development of neurological deficit.
References
- 1.Martin RJ, Yuan HA. Neurosurgical care of spinal epidural, subdural, and intramedullary abscesses and arachnoiditis. Orthop Clin North Am. 1996;27:125–36. [PubMed] [Google Scholar]
- 2.Mackenzie AR, Laing RB, Smith CC, Kaar GF, Smith FW. Spinal epidural abscess: the importance of early diagnosis and treatment. J Neurol Neurosurg Psychiatry. 1998;65:209–12. doi: 10.1136/jnnp.65.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chao D, Nanda A. Spinal epidural abscess: a diagnostic challenge. Am Fam Physician. 2002;65(7):1341–6. [PubMed] [Google Scholar]
- 4.Soehle M, Wallenfang T. Spinal epidural abscess: clinical manifestations, prognostic factors, and outcomes. Neurosurgery. 2002;51(1):79–87. doi: 10.1097/00006123-200207000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Vilke GM, Honingford EA. Cervical spine epidural abscess in a patient with no predisposing risk factors. Ann Emerg Med. 1996;27(6):777–80. doi: 10.1016/s0196-0644(96)70201-9. [DOI] [PubMed] [Google Scholar]
- 6.Rabih O. Darouiche. Spinal Epidural Abscess. review article. N Engl J Med. 2006;355:2012–20. doi: 10.1056/NEJMra055111. [DOI] [PubMed] [Google Scholar]
- 7.Louis Amy, Fernandes Christopher. Spinal epidural abscess. Can J Emerg Med. 2005;7(5):351–4. doi: 10.1017/s1481803500014603. [DOI] [PubMed] [Google Scholar]
- 8.Kim MC, Jung HT. Pediatric Lumbar Epidural Abscess Combined with Cauda Equina Syndrome: Case Report. ASJ. 2011;5(2):133–137. doi: 10.4184/asj.2011.5.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000;23(2):175–204. doi: 10.1007/pl00011954. [DOI] [PubMed] [Google Scholar]