Abstract
Purpose
The goal of this study was to evaluate the treatment and recovery of patients treated for Gartland type III supracondylar humerus fractures in order to determine if postponing treatment leads to a higher rate of open surgical treatment or complications.
Methods
A retrospective study was conducted examining the medical records of children with Gartland type III supracondylar humerus fractures at our institution for a two-year period. The patients included in the study were treated with closed reduction and percutaneous pinning (CRPP) or open reduction and internal fixation (ORIF).
Results
After exclusions, 134 patients were included in the study, with an average age of 5.6 years. The patients were grouped according to whether their treatment was postponed (39.6 %) or immediate (60.4 %). The majority of all patients were treated using CRPP: 46 (86.8 %) of the postponed patients and 75 (92.6 %) of the immediate patients. Very few postsurgical complications occurred in the patients; there was only one (1.6 %) case of iatrogenic nerve injury in a postponed patient as well as four (3.8 %) cases of loss of carrying angle: one (2.3 %) in postponed patients and three (4.8 %) in immediate patients.
Conclusions
Postponing treatment of type III supracondylar humerus fractures in children did not lead to an increase in open surgical treatment; nor did it lead to an increase in complications.
Keywords: Supracondylar humerus fracture, Delayed fracture treatment, Closed reduction percutaneous pinning, Pediatric
Introduction
Supracondylar humerus fractures are some of the most common fractures experienced by the pediatric population [1–4]. In the past, pediatric supracondylar humerus fractures were treated urgently, and therefore taken for surgical treatment without delay. This practice was instituted to avoid potential complications including nerve injury, compartment syndrome, and a need to perform open surgery, all of which were thought to result from delaying treatment [5]. More recently, it has been proposed that delaying treatment is acceptable, with no adverse outcomes resulting from delayed treatment [2]. Recent investigations evaluating children with supracondylar humerus fractures found no difference between patients with early or delayed treatment for the following parameters: functional status including carrying angle or Baumann’s angle, grip strength, and range of motion; rates of complications including pin-track infection, nerve injury, and occurrence of compartment syndrome; as well as the need for open surgery [6–8]. In contrast, there are studies which support the case for early treatment, demonstrating that reduction becomes more difficult for patients with delayed treatment, and the occurrence of compartment syndrome in patients whose treatment is delayed [9–11]. As noted, there is still some debate as to whether these fractures should be treated as urgent cases with early intervention, or if patients with delayed treatment also experience satisfactory outcomes [1–5, 12–15]. The goal of this study was to evaluate the treatments and outcomes of patients with Gartland type III supracondylar humerus fractures in order to determine if postponing treatment leads to a higher rate of open surgical treatment or complications. To our knowledge, this is the only investigation in which the presence of preoperative risk factors is evaluated and a potential correlation with the need for open reduction or the decision to postpone surgery is examined. These preoperative risk factors include radial pulse presence, severe swelling, ecchymosis, and nerve injury. The results of this investigation will help guide treatment decisions at our institution for patients with supracondylar humerus fractures.
Methods
After approval by the Academic Medical Center Institutional Review Board, we conducted a retrospective study consisting of a chart review. Patients (aged 0–18) who underwent closed reduction and percutaneous pinning (CRPP) or open reduction and internal fixation (ORIF) treatment for a Gartland type III supracondylar humerus fracture at our institution during a two-year period between January 1, 2008 and December 31, 2009 were eligible for inclusion in the study. Four senior orthopedic surgeons performed all of the procedures included in this study. The decision to treat immediately or postpone treatment was made at the discretion of the attending surgeon. Treatment in the emergency department (ED) consisted of splinting in place, with gentle, minimal flexion at the elbow. Surgical management of these patients was determined by the attending orthopedic surgeon, and included closed reduction and percutaneous pinning or open reduction and pinning. When an open reduction was performed, a lateral approach was used. Radiographs were taken preoperatively, during the procedure, one week after injury, and as needed during the follow-up period. The time of immobilization ranged from three to six weeks and was decided at the discretion of the attending orthopedic surgeon. Patients were expected to follow-up for six weeks or until normal range of motion and carrying angle were achieved, up to four months postoperatively. Excluded from the study were patients who were 18 years and older, had sustained an open fracture, were treated through a procedure other than CRPP or ORIF, or had metabolic bone disease. During this time period, 136 patients underwent treatment for Gartland type III supracondylar humerus fractures. Two patients were excluded due to inadequate documentation. After exclusions, 134 patients qualified for inclusion in the study. A flowchart of patient enrollment is depicted in Fig. 1.
Fig. 1.
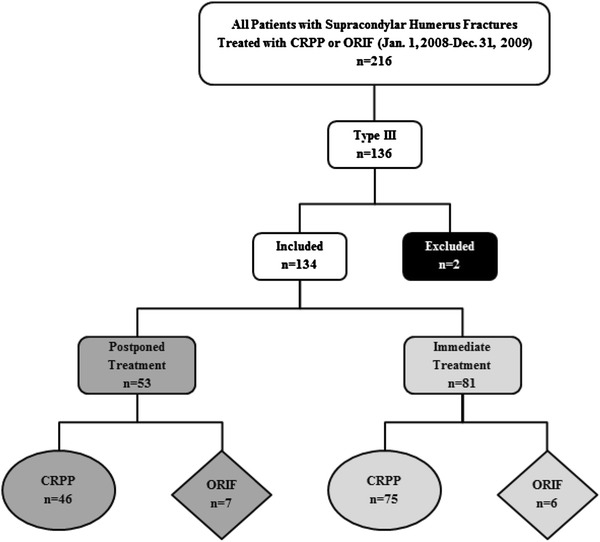
Flowchart of patient enrollment. All patients with a Gartland type III supracondylar humerus fracture were considered for inclusion in the study. The patients were divided into two groups: those who underwent immediate treatment, defined as treatment less than or equal to 12 h from presentation to the emergency department (shown on the right in light gray), and those who underwent postponed treatment, defined as treatment greater than 12 h from presentation to the emergency department (shown on the left in dark gray)
The remaining patients were divided into two groups according to the length of time between presentation to our emergency department (ED) and treatment. The immediate group included patients who underwent treatment less than or equal to 12 h after presentation to our ED. The postponed group included patients who underwent treatment greater than 12 h after presentation to our ED. The postponed group generally included patients who arrived at our ED after 6 pm. The patients’ medical records were examined to abstract information regarding the treatment, recovery, and complications of the study subjects.
Patient demographic information, in addition to information regarding the time between the injury and presentation to our emergency department and the time to treatment, as well as data on the time of day that the injury occurred, were gathered. Additional data abstracted included information about the injury at presentation to the emergency department, such as mechanism of injury, fracture type, radial pulse presence, severe swelling, ecchymosis, nerve injury, associated injuries, treatment method, and length of hospital stay. Patients were recorded as having an absent radial pulse, severe swelling, ecchymosis, or nerve injury if these were explicitly stated in the emergency department, consultation, or clinical notes. Complications and functional status after treatment were analyzed, including length of time in cast and length of time until removal of pins, complications (including incidence of pin-track infection, iatrogenic nerve injury, compartment syndrome, loss of carrying angle, malunion), and range of motion (full/near-full or limited) at the final follow-up visit.
SPSS v.17.0 was utilized to perform all statistical procedures. Statistically significant differences were considered to be achieved at ap value of ≤0.05, two-tailed.
Results
Of the 134 children included in the study, 68 (50.7 %) were females, and the average age was 5.6 years (SD, 2.6; range, 1–13). Race was evenly distributed in the study population, with 51/134 (38.1 %) of the patients African American and 54/134 (40.3 %) Caucasian. When demographics were compared for the two groups, they were found to be similar (Table 1). When grouped according to time elapsed between presentation to our ED and treatment, 81 patients (60.4 %) were assigned to the immediate treatment group, defined as treatment less than or equal to 12 h after presentation to ED, and 53 (39.6 %) patients underwent postponed treatment, defined as treatment greater than 12 h from presentation to ED.
Table 1.
Demographic characteristics of supracondylar humerus fracture surgery patients
| Postponed group (n = 53) | Immediate group (n = 81) | p | |
|---|---|---|---|
| Value | Value | ||
| Age, mean (SD), y | 5.3 (2.4) | 5.9 (2.7) | 0.226* |
| Female gender, n (%) | 25 (47.2 %) | 43 (53.1 %) | 0.597† |
| Racen (%) | |||
| African American | 24 (45.3 %) | 27 (33.3 %) | n/a |
| Caucasian | 22 (41.5 %) | 32 (39.5 %) | |
| Hispanic | 3 (5.6 %) | 10 (12.3 %) | |
| Other | 2 (3.8 %) | 10 (12.3 %) | |
| Unknown | 2 (3.8 %) | 2 (2.6 %) | |
* Student’st test
†Pearson’s χ2 test
The most common mechanism of injury was a fall, with 120 (91.0 %) patients sustaining their injuries in this manner. We collected data on the preoperative assessment for all of the patients, including associated injuries such as other fractures, head injuries, or nerve injuries. We also collected information regarding preoperative risk factors, including the presence of a radial pulse, severe swelling, ecchymosis, and nerve injury, to determine if there was a correlation between these factors and postponing treatment or the need for open surgery. The immediate group had a higher incidence (16.0 %) of associated injuries than the postponed group (7.5 %). When we assessed the overall occurrence of preoperative risk factors, this was higher for the immediate group, with 43.2 % of the patients in this group presenting with at least one of the listed preoperative risk factors, compared to 28.3 % for the postponed group, although this was not a significant difference (Fig. 2, p = 0.101). When we examined specific risk factors, we found that the patients with postponed treatment had a higher incidence of ecchymosis and nerve injury detected during the preoperative assessment done at the emergency department, with 13.2 and 3.8 % of the patients suffering from these risk factors, respectively (Fig. 2). In contrast, patients with immediate treatment had a higher incidence of severe swelling, 30.9 %, compared to 17 % for the postponed group, as well as higher incidence of lack of a palpable radial pulse (2.5 %), while the postponed group had no patients without a palpable radial pulse (pulseless white hand). However, these differences were not statistically significant.
Fig. 2.
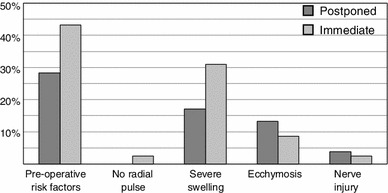
Graph representing preoperative complications of patients assessed upon admission to our institution. Patients in the immediate group are represented by thelight gray bars, and the postponed group is shown as the dark gray bars
The primary goal of this study was to evaluate the treatment of patients with Gartland type III supracondylar humerus fractures in order to determine if postponing treatment leads to a higher rate of open surgical treatment. When we evaluated the patients who required open surgery, we found that 46 (86.8 %) of the postponed patients were treated with CRPP and 7 (13.2 %) were treated with ORIF (Table 2). This is statistically similar to the immediate group, in which 75 (92.6 %) of the postponed patients were treated with CRPP and 6 (7.4 %) were treated with ORIF (p = 0.371). The average operative time for the two groups was also similar: 49.4 min for the delayed group and 46.5 min for the postponed group (p = 0.418). We next examined information regarding the time between presentation at our ED and surgical treatment of the patients. As expected, this was significantly different for the two groups: an average of 16 h (SD, 2.7) for the postponed group and 7.4 h (SD, 3.4) for the immediate group (p < 0.001).
Table 2.
Surgical treatment of supracondylar humerus fracture surgery patients
| Postponed group (n = 53) | Immediate group (n = 81) | p | |
|---|---|---|---|
| Value | Value | ||
| Type of surgery,n (%) | |||
| CRPP | 46 (86.8 %) | 75 (92.6 %) | 0.371† |
| ORIF | 7 (13.2 %) | 6 (7.4 %) | |
| Operative time, mean (SD) in minutes | 49.4 (24.2) | 46.5 (20.5) | 0.418* |
| Time from ED to treatment, mean (SD) in hours | 16.0 (2.7) | 7.4 (3.4) | <0.001* |
* Student’st test
†Pearson’s χ2 test
We next collected information on follow-up and postoperative complications for these patients. Of the 134 patients included in the study, 106 returned for an average follow-up of 2.1 months, ranging from 0.5 to 25 months. The two groups had similar lengths of follow-up (data not shown). The average times in cast and until pin removal were also similar for the two groups, with an average of 3.6 weeks and 3.5 weeks, respectively, for all patients. There were similar, low rates of postoperative complications for both groups (Table 3). There were no cases of malunion, compartment syndrome, vascular injury, or pin-track infection. There was one (1.6 %) case of iatrogenic ulnar nerve injury from a medial pin and three patients who experienced loss of carrying angle (4.8 %) in the immediate group. There were no cases of iatrogenic nerve injury and one case of loss of carrying angle in the postponed group (2.3 %). For patients who experienced a postoperative complication, the time between presentation at our ED and surgery was 9.5 h, similar to the average of 11 h for all patients.
Table 3.
Postoperative complications of supracondylar humerus fracture surgery patients
| Postponed group (n = 44) | Immediate group (n = 62) | p | |
|---|---|---|---|
| Value | Value | ||
| Post-op complications,n (% yes) | 1 (2.3 %) | 4 (6.5 %) | 0.284† |
| Iatrogenic nerve injury,n (% yes) | 0 (0.0 %) | 1 (1.6 %) | 0.571† |
| Loss of carrying angle,n (% yes) | 1 (2.3 %) | 3 (4.8 %) | 0.424† |
†Pearson’sχ2 test
We next evaluated the postoperative complications for patients who did not have any preoperative risk factors on initial examination. Of the 76 patients in this group, a total of 4 patients had a postoperative complication, all of which were loss of carrying angle. The loss of carrying angle was observed in 1 patient (2.7 %) from the postponed group and 3 patients (7.7 %) from the immediate group, which was not a significant difference (Table 4).
Table 4.
Postoperative complications of supracondylar humerus fracture surgery patients without preoperative risk factors
| Postponed group (n = 37) | Immediate group (n = 39) | p | |
|---|---|---|---|
| Value | Value | ||
| Post-op complications,n (% yes) | 1 (2.7 %) | 3 (7.7 %) | 0.615† |
| Iatrogenic nerve injury,n (% yes) | 0 (0.0 %) | 0 (0.0 %) | n/a |
| Loss of carrying angle,n (% yes) | 1 (2.7 %) | 3 (7.7 %) | 0.615† |
†Pearson’sχ2 test
When we examined range of motion, we found 55 patients in the study with documented range of motion assessments. These examinations were conducted an average of 8.7 (SD, 5.6) weeks after surgery. The majority of the postponed group had full or near-full range of motion, with 12 patients (57.1 %), whereas 9 patients (42.9 %) had limited range of motion. The number of immediate patients with full or near-full range of motion was statistically similar, 22 (64.7 %), whereas 12 (35.3 %) had limited range of motion (Table 5).
Table 5.
Range of motion of supracondylar humerus fracture surgery patients
| Postponed group (n = 21) | Immediate group (n = 34) | p | |
|---|---|---|---|
| Value | Value | ||
| Range of motion,n (%) | |||
| Full/near-full | 12 (57.1 %) | 22 (64.7 %) | 0.337† |
| Limited | 9 (42.9 %) | 12 (35.3 %) | |
†Pearson’sχ2 test
Discussion
The decision to treat type III supracondylar humerus fractures immediately is still a matter of debate among pediatric orthopedic surgeons, with several groups positing that delayed treatment does not lead to an increased need for open surgery [1–8, 10, 14–19]. Other investigations show that delaying treatment leads to an increase in open surgery or complications [9–11]. In order to answer these questions for patients seen at our institution, we conducted a retrospective investigation, examining preoperative risk factors, treatment, postoperative complications, and functional status for patients treated for these fractures.
There are many risk factors that can prompt the decision to treat the patient immediately or can predict the need to perform open surgery, including severe swelling, vascular compromise, nerve injury, or ecchymosis [2, 20]. In our study, three (8.8 %) patients who had severe swelling had open surgical treatment, and all were in the immediate group. We speculate that severe swelling may have been a significant factor in the decision to perform immediate surgery as well as a factor in the need to perform open surgery. In addition, there was only one case of vascular compromise which was treated immediately, consistent with studies noting that vascular compromise is an emergent condition and treatment should not be delayed [20]. Notably, patients from the immediate group experienced preoperative risk factors more frequently than the postponed group, with 15 % more of these patients found to have preoperative risk factors. The likely reason for this difference is that a patient with preoperative risk factors will almost certainly be treated as an urgent case to avoid the occurrence of postoperative complications. However, when we examined the rate of postoperative complications for patients with no preoperative risk factors, we found no difference between the two groups (Table 4).
We also analyzed whether postponing treatment would lead to more postoperative complications as well compromised functional status, defined by the occurrence of a limited range of motion. When we examined all of the postoperative complications together, both groups of patients had a similar, low rate of complications, with a total of five patients (4.7 %) in the study experiencing any postoperative complication. When we assessed range of motion, we found that the majority of all patients had full or near-full range of motion. This conclusion is similar to those given in previous studies [6, 21, 22].
In addition to reducing postoperative complications, other reasons to postpone treatment until the following morning include patients’ lack of sufficient NPO (“nil per os,” Latin for nothing by mouth) status for safe anesthesia practice, as well as waiting until the morning, when dedicated orthopedic operating room staff are available. In a study done by Cashman et al. [21], the investigators examined whether performing surgery after midnight would increase postoperative complications compared to deferring treatment until the morning. They concluded that there is no difference in complication rates when treatment of supracondylar fractures is postponed. Furthermore, other studies have shown that patients with supracondylar humerus fractures whose surgery is postponed by 2–12 days experience satisfactory outcomes [23, 24]. We found that patients with postponed treatment did not require open surgical treatment more than patients who were treated immediately; nor did they experience more postoperative complications or reduced function. We found that patients experienced similar complications and recovery, regardless of whether they were treated immediately or their treatment was postponed. Representative radiographs of patients from both the immediate and postponed groups are shown in Fig. 3. As depicted in the postoperative images, the patients from both groups show well-healed fractures at the final follow-up examination.
Fig. 3a–d.

Radiographs showing representative patients with Gartland type III supracondylar humerus fractures before and after treatment for both immediate and postponed patients. Radiograph taken a preoperatively and c at final follow-up of a patient from the immediate group. Radiograph taken b preoperatively and d at final follow-up of a patient from the postponed group
Some limitations of this study include those inherent in retrospective studies. These include uncontrolled variables such as the time from injury to arrival at the emergency room, as well as the time to final surgical treatment. In addition, the time to follow-up was an average of 2.1 months, and postoperative complications may occur well after this time period. Finally, follow-up and range-of-motion information were not available for all of the patients included in the study.
The results of our investigation support the notion that postponing treatment of type III supracondylar humerus fractures neither increases the likelihood of open surgery nor increases the rate of complications following treatment. In our institution, the treatment of uncomplicated supracondylar humerus fractures may be postponed or treated immediately.
Conflict of interest
None of the authors received financial or grant support for this study.
References
- 1.Murnaghan ML, Slobogean BL, Byrne A, Tredwell SJ, Mulpuri K. The effect of surgical timing on operative duration and quality of reduction in type III supracondylar humeral fractures in children. J Child Orthop. 2010;4:153–158. doi: 10.1007/s11832-010-0240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pretell Mazzini J, Rodriguez Martin J, Andres Esteban EM. Surgical approaches for open reduction and pinning in severely displaced supracondylar humerus fractures in children: a systematic review. J Child Orthop. 2010;4:143–152. doi: 10.1007/s11832-010-0242-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dua A, Eachempati KK, Malhotra R, Sharma L, Gidaganti M. Closed reduction and percutaneous pinning of displaced supracondylar fractures of humerus in children with delayed presentation. Chin J Traumatol. 2011;14:14–19. [PubMed] [Google Scholar]
- 4.Leet AI, Frisancho J, Ebramzadeh E. Delayed treatment of type 3 supracondylar humerus fractures in children. J Pediatr Orthop. 2002;22:203–207. [PubMed] [Google Scholar]
- 5.Sibinski M, Sharma H, Bennet GC. Early versus delayed treatment of extension type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg Br. 2006;88:380–381. doi: 10.1302/0301-620X.88B3.17181. [DOI] [PubMed] [Google Scholar]
- 6.Iyengar SR, Hoffinger SA, Townsend DR. Early versus delayed reduction and pinning of type III displaced supracondylar fractures of the humerus in children: a comparative study. J Orthop Trauma. 1999;13:51–55. doi: 10.1097/00005131-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AH. The effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in children. J Bone Joint Surg Am. 2001;83-A:323–327. doi: 10.2106/00004623-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Carmichael KD, Joyner K. Quality of reduction versus timing of surgical intervention for pediatric supracondylar humerus fractures. Orthopedics. 2006;29:628–632. doi: 10.3928/01477447-20060701-13. [DOI] [PubMed] [Google Scholar]
- 9.Yildirim AO, Unal VS, Oken OF, Gulcek M, Ozsular M, Ucaner A. Timing of surgical treatment for type III supracondylar humerus fractures in pediatric patients. J Child Orthop. 2009;3:265–269. doi: 10.1007/s11832-009-0189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramachandran M, Skaggs DL, Crawford HA, Eastwood DM, Lalonde FD, Vitale MG, Do TT, Kay RM. Delaying treatment of supracondylar fractures in children: has the pendulum swung too far? J Bone Joint Surg. 2008;90-B:1228–1233. doi: 10.1302/0301-620X.90B9.20728. [DOI] [PubMed] [Google Scholar]
- 11.Donnelly M, Green C, Kelly IP. An inconvenient truth: treatment of displaced paediatric supracondylar humeral fractures. Surgeon. 2012;10:143–147. doi: 10.1016/j.surge.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Kim WY, Chandru R, Bonshahi A, Paton RW. Displaced supracondylar humeral fractures in children: results of a national survey of paediatric orthopaedic consultants. Injury. 2003;34:274–277. doi: 10.1016/S0020-1383(02)00321-2. [DOI] [PubMed] [Google Scholar]
- 13.Mulpuri K, Hosalkar H, Howard A. AAOS clinical practice guideline: the treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg. 2012;20(5):328–330. doi: 10.5435/JAAOS-20-05-328. [DOI] [PubMed] [Google Scholar]
- 14.Gupta N, Kay RM, Leitch K, Femino JD, Tolo VT, Skaggs DL. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop. 2004;24:245–248. doi: 10.1097/01241398-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Mallo G, Stanat SJ, Gaffney J. Use of the Gartland classification system for treatment of pediatric supracondylar humerus fractures. Orthopedics. 2010;33:124–128. doi: 10.3928/01477447-20091124-08. [DOI] [PubMed] [Google Scholar]
- 16.Ozkoc G, Gonc U, Kayaalp A, Teker K, Peker TT. Displaced supracondylar humeral fractures in children: open reduction versus closed reduction and pinning. Arch Orthop Trauma Surg. 2004;124:547–551. doi: 10.1007/s00402-004-0730-1. [DOI] [PubMed] [Google Scholar]
- 17.Loizou CL, Simillis C, Hutchinson JR. A systematic review of early versus delayed treatment for type III supracondylar humeral fractures in children. Injury. 2009;40:245–248. doi: 10.1016/j.injury.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 18.Allen SR, Hang JR, Hau RC. Review article: paediatric supracondylar humeral fractures: emergency assessment and management. Emerg Med Australas. 2010;22:418–426. doi: 10.1111/j.1742-6723.2010.01332.x. [DOI] [PubMed] [Google Scholar]
- 19.Bales JG, Spencer HT, Wong MA, Fong YJ, Zionts LE, Silva M. The effects of surgical delay on the outcome of pediatric supracondylar humeral fractures. J Pediatr Orthop. 2010;30:785–791. doi: 10.1097/BPO.0b013e3181f9fc03. [DOI] [PubMed] [Google Scholar]
- 20.Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1121–1132. doi: 10.2106/JBJS.G.01354. [DOI] [PubMed] [Google Scholar]
- 21.Cashman JP, Guerin SM, Hemsing M, McCormack D. Effect of deferred treatment of supracondylar humeral fractures. Surgeon. 2010;8:71–73. doi: 10.1016/j.surge.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Han QL, Wang YH, Liu F. Comparison of complications and results of early versus delayed surgery for Gartland type III supracondylar humeral fractures in pediatric patients. Orthop Surg. 2011;3:242–246. doi: 10.1111/j.1757-7861.2011.00153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silva M, Wong TC, Bernthal NM. Outcomes of reduction more than 7 days after injury in supracondylar humeral fractures in children. J Pediatr Orthop. 2011;31:751–756. doi: 10.1097/BPO.0b013e31822f16e5. [DOI] [PubMed] [Google Scholar]
- 24.Tiwari A, Kanojia RK, Kapoor SK. Surgical management for late presentation of supracondylar humeral fracture in children. J Orthop Surg (Hong Kong) 2007;15:177–182. doi: 10.1177/230949900701500211. [DOI] [PubMed] [Google Scholar]


