Abstract
Purpose
Non-displaced distal radius fractures in children are traditionally treated in a forearm cast. However, a traditional cast does not tolerate getting wet, with skin lesions and bad smell as result. A Swim cast, which has the ability to dry quickly, is an airy cast that is applied using the MOKcast technique. We hypothesize that Swim casts contribute to higher patient satisfaction scores than traditional casts, without any adverse effects on fracture healing or skin condition.
Methods
A prospective, randomized, single-center, blinded study was conducted to compare traditional and Swim cast treatment in children aged 5–15 years with greenstick or torus fractures of the distal radius. Primary endpoint was the patient and parent satisfaction, as determined by a questionnaire. Secondary endpoints were radiographic and clinical bone healing and cast-related skin conditions.
Results
A total of 68 patients, divided into two treatment groups (traditional case and Swim cast;n = 34 per group). Baseline characteristics were similar between the groups. The overall satisfaction score (0–10) reported by the patients was 8.6 in the Swim cast group versus 7.5 in the traditional cast group (p < 0.002); the overall satisfaction score reported by the parents was 8.3 and 7.7, respectively (p < 0.02). There was no difference in radiographic or clinical healing between groups, and skin conditions also did not differ significantly between groups.
Conclusion
In our patient group, treatment of non-displaced, pediatric, distal radius fractures by Swim cast yielded better patient satisfaction results compared to treatment with the traditional, cotton-lined cast, without adverse effects on fracture healing or skin condition.
Keywords: Distal radius fractures, Patient satisfaction, MOK cast, Swim cast, Traditional cast
Introduction
A non-displaced greenstick or torus fracture of the distal radius in children is traditionally treated by cast immobilization. The major disadvantage of traditional casts is the fact that the cast has to be kept dry, otherwise skin maceration may occur, possibly resulting in (yeast) infections and concomitant dermal conditions.
A alternative to the traditional cotton-lined cast is a ‘Swim’ cast which was developed by making a number of critical adjustments according to the MOKcast principle during the preparation of the traditional cast [1]. A ‘Swim’ cast prevents prolonged moistening of the skin, which results in maceration and consequent skin irritation, bad smell, and infection. It is an air-ventilating cast manufactured without the use of a synthetic wool liner. In the MOKcast technique, which was developed by Axel Wierzimok, a semi-flexible Polyester cast made of the same polyurethane material as used in the traditional cast is applied directly over the protective stocking without using a liner. An airy cast is made by first placing a piece of adhesive felt padding at the base of the thumb prior to applying the case and then removing this padding after the cast has been applied and has dried. To create a lightweight cast and to improve fast drying, only a single layer of synthetic cast is applied after a reinforcing longuette of the same cast material is used on the ulnar side. The MOKcast technique is closely related to focused rigidity casting [1]. The technique uses elastic synthetic tape and has been reported to be more comfortable for patients than a traditional cast for a number of reasons, among which is its reduced weight [2].
The aim of the study was to compare the Swim cast to the traditional cast in terms of patient comfort, bone healing, and skin lesions.
Materials and methods
This was a prospective, randomized, controlled, single-blinded trial performed over a 1-year period in which traditional casts (cotton-lined) were compared to Swim casts (MOKcast technique). Children aged 5–15 years who had sustained an isolated greenstick or torus fracture of the distal radius were eligible for entry. Exclusion criteria were: polytrauma patients; patients suffering from osteogenesis imperfecta or other bone diseases; pre-existent fractures or deformity of the injured forearm (congenital or acquired); concurrent participation in another study.
At initial admission in the Emergency Department (ED) parents received an information letter describing the study. During the first week, all children included in the study were treated in a forearm mineral plaster splint (plaster of Paris), in accordance to hospital protocol. One week later at the outpatient clinic, with informed consent by the parents or caretakers, the patients were randomized into two treatment groups: those receiving a traditional forearm cast or those receiving a Swim cast (Fig. 1). Randomization was by the drawing of an envelope in the presence of employees of the plaster room who guided this process and occurred in blocks of ten patients. Both types of casts were worn for 2–3 weeks following the initial week of treatment in a plaster of Paris splint. Children younger than 8 years were immobilized for a total of 3 weeks and children 8 years and older were immobilized for a total of 4 weeks, in accordance with hospital protocol.
Fig. 1.
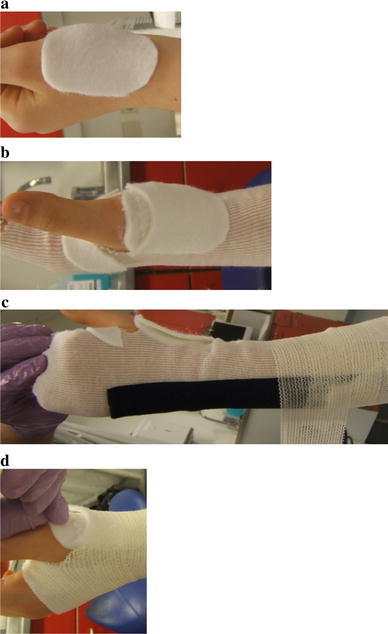
MOKcast technique. a A small piece of adhesive felt padding is placed at the base of the first metacarpal up to 1 cm proximal of the tabatière anatomique (anatomical snuff box). b A synthetic stocking is applied between the first and second digit and around the tabatière anatomique; another piece of felt padding is placed on the stocking. c A longuette is placed proximal from the ulnar styloid process down to the proximal joint facet of the ulna, and the polyester cast is applied circumferentially in order to allow ventilation. d The felt padding placed on the skin is removed
Patients in the Swim cast group were instructed not to shower or swim just before going to bed so as not to get the bed wet because it takes some time for the cast to dry. No additional instructions were given regarding avoiding swimming or going to the beach. Patients receiving the traditional cast were advised to use a protective plastic bag when taking a shower or going for a swim.
After the treatment period the cast was removed by employees of the plaster room, and control radiographs (anterior-posterior and lateral) were made. A radiologist assessed bone healing (assessment of periosteal callus formation) and the presence of a secondary dislocation of the distal radius on control radiographs. In standard clinical practice control radiographs are not performed for such fractures; however, with the aim to assess the new treatment (Swim cast), we deemed it necessary to ascertain healing.
Clinical bone healing was assessed by one of three trained surgery residents (painless axial compression and local palpation of the distal radius). The surgery resident also assessed the skin for lesions (urticaria, redness, desquamation, maceration, pressure sores, and inflammation). Both the radiologist and the surgery resident were blinded to the type of cast that was administered.
Parents and patients were asked to complete a short questionnaire (Fig. 2) with questions on whether the patient took a shower and/or went for a swim, assessment of the cast treatment, and the degree of patient satisfaction with regards to the treatment. All patients received the same questionnaire (grading scale 0–10). The study was conducted in accordance with the Declaration of Helsinki, and the Institutional Review Board approved the study.
Fig. 2.
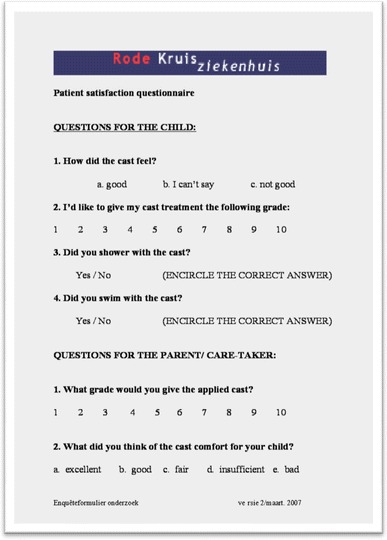
Translated patient and parent satisfaction questionnaire
The primary outcome measure used to determine the needed sample size was patient satisfaction. A 15 % difference in patient satisfaction was considered to indicate a clinically important difference. Since patient satisfaction could be either worse or better in the Swim cast group, sample size was calculated two-sided, withα = 0.05 and a power of 80 %. As no standard deviation (SD) of patient satisfaction concerning traditional forearm cast in children has been reported in the literature, we applied the second best method to obtain the SD, which was to use the statistical rule of thumb that the SD can be estimated by dividing the spreading of answers by 4. In our study, we expected patient satisfaction results to range from 3 to 10, thus providing a range of 8. The estimated SD would be 2.0. The resulting sample size was consequently calculated to be 28 patients per group. Taking into account a 15 % loss to follow-up, a minimum of 32 patients should be included in each group.
Patient and parent satisfaction, skin lesions, bone healing, and positional changes were all compared by an independent samples t test (continuous variables) or χ2 statistics (proportions) (SPSS ver. 19; SPSS Inc, Chicago, IL).
Results
In total, 68 patients were randomized into the two treatment groups. Patients in both groups [traditional cast (n = 34) and Swim cast (n = 34)] were similar in terms of sex, age and side of the fracture (Table 1). In both groups the average immobilization period was 3.9 weeks (p = 0.75). The majority of patients were enrolled in the study during the spring and summer (Fig. 3).
Table 1.
Patient characteristics per treatment group
| Group | Traditional cast (n = 34) | Swim cast (n = 34) | p value |
|---|---|---|---|
| Patient characteristics | |||
| Age | 9.7 year | 9.9 year | 0.81 |
| Male/female ratio | 38/62 % | 41/59 % | 0.80 |
| Fracture side (right/left proportion) | 41/59 % | 41/59 % | 1.00 |
| Torus fracture | 79 % | 85 % | 0.21 |
| Immobilization duration | 3.9 weeks | 3.9 weeks | 0.75 |
Age and immobilization duration are means
Continuous variables (age, immobilization duration) are compared using the independent samples t test, and proportions (male/female ratio, fracture sidedness, and fracture type) are compared with χ2 statistics
Fig. 3.
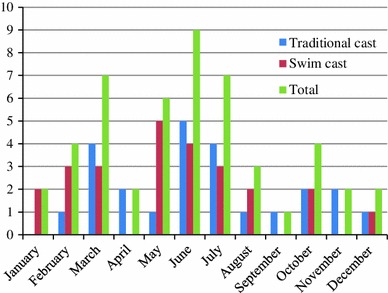
Number of patients included during the year per treatment group
Parents and children scaled their overall satisfaction of the treatment with the traditional cast as (7.5 ± 0.9) and (7.7 ± 0.9), respectively, versus 8.6 ± 1.6 and 8.3 ± 1.0 in the Swim cast group (Table 2). Both differences were found to be statistically significant between groups.
Table 2.
Overall satisfaction assessment of parents and children in both groups (independent samples t test)
| Assessment | Traditional cast | Swim cast | p value |
|---|---|---|---|
| Assessment patients | 7.5 ± 0.9 | 8.6 ± 1.6 | 0.002 |
| Assessment parents | 7.7 ± 0.9 | 8.3 ± 1.0 | 0.02 |
Data are presented as the mean ± standard deviation (SD)
All patients in the Swim cast group took a shower, and 55 % went for a swim while wearing the cast (p ≤ 0.001); in the traditional cast group, 44 % took a shower (with protection of the cast) and 12 % went for a swim (while wearing a plastic protective bag (p ≤ 0.001) (Table 3).
Table 3.
Percentage of patients that took a shower and went for a swim
| Shower/swim | Traditional cast (%) | Swim cast (%) | p value |
|---|---|---|---|
| Took a shower | 44 | 100 | <0.001 |
| Went for a swim | 12 | 55 | <0.001 |
Proportion of subjects per treatment group that showered and swam are compared with χ2 statistics
Clinical bone healing occurred in all of the patients in the traditional cast group (100 %) and in 97 % of those in the Swim cast group (exception: 1 patient), which was a statistically significant difference (p = 0.32) (Table 4). The one exception, a 14-year old boy with a greenstick fracture of the distal radius, had a clinically unhealed distal radius after 4 weeks of immobilization and subsequently received an additional 2 weeks of immobilization. Otherwise, no differences were found concerning radiological and clinical consolidation of the fractures. No secondary dislocation was found in both groups, and there were no significant differences between the groups in terms of skin lesions (Table 5). However, since sample size was calculated on the primary outcome being patient satisfaction and not on skin complications, it is possible that the study was underpowered to show a significant difference in skin complications.
Table 4.
Percentage of clinical and radiological bone healing and secondary dislocation in each group
| Bone healing | Traditional cast (%) | Swim cast (%) | p value |
|---|---|---|---|
| Clinical bone healing | 100 | 97 | 0.32 |
| Radiological bone healing | 100 | 100 | 1.0 |
| Secondary dislocation | 0 | 0 | 1.0 |
Proportions per treatment groups are compared with χ2 statistics
Table 5.
Skin lesion percentage in each group
| Skin lesions | Traditional cast (%) | Swim cast (%) | p value |
|---|---|---|---|
| Urticaria | 6 | 6 | 1.0 |
| Redness | 9 | 18 | 0.28 |
| Desquamation | 12 | 9 | 0.69 |
| Pressure sores | 15 | 6 | 0.23 |
| Maceration | 0 | 0 | 1.0 |
| Inflammation | 0 | 3 | 0.31 |
Proportions per treatment groups are compared with χ2 statistics
Discussion
The findings in this trial show that children aged 5–15 years who sustained a distal radius fracture treated with a Swim cast were significantly more satisfied than those children treated with a traditional cast, without any decrease in clinical and radiological bone healing or worsened skin condition. Despite the use of an unvalidated satisfaction questionnaire (no validated questionnaire is as yet available for this purpose), we did not expect any bias due to the straight forward questions asked in the questionnaire that simply recorded if and how often patients showered and/or went for a swim as well as how satisfied both the parents and patient were with the treatment. Selection bias is also unlikely since patients were randomized, and patient characteristics did not differ significantly in both groups.
To our knowledge, this is the first report of the MOKcast technique and its advantages over traditional plaster cast since the original report by Wierzimok [1].
The higher satisfaction score of patients and parents is assumed to be due to the fact that patients could shower and swim with their cast, which is an especially important advantage for children. Another explanation for the increased comfort could be the weight; Swim casts contain fewer layers than the traditional casts and are therefore lighter and more comfortable to wear. The weight of a Swim cast is approximately 45 % of that of the traditional cast.
Since the results of this study were analyzed, children admitted to the Red Cross Hospital with greenstick or torus fractures are treated with a Swim cast. No adverse effects of the treatment have been reported since its routine implementation.
Of the 32 patients in the Swim cast group, 55 % went for a swim. One possible explanation for this low percentage is the 1-year inclusion period; during the autumn, winter, and beginning of the spring the average temperatures in the Netherlands are between 4 °C and 14 °C. Nevertheless, this percentage is very large compared to the percentage of patients with a traditional case who went for a swim, i.e., 12 %. In this respect, no additional information on swimming was obtained (frequency, kind of water, the temperature of the water, etc.).
There have been some reports describing other waterproof cast techniques, such as the Gore-tex technique. Gore-tex, a semipermeable membrane, allows perspiration vapor to escape but prevents water from passing through the membrane [3]. A randomized controlled trial comparing waterproof (Gore-tex) cast liners with traditional cast liners showed a significantly improved comfort on all of the scores (irritation, itch, discomfort) in the waterproof liner group [4]. Dubowitz et al. [5] described a case in which a patient had a distal fracture of the left scaphoid. After 1 week, the patient received a Gore-tex cast lining instead of a traditional lining of cotton or felt, which allowed the patient to dive. After 3 weeks, the routine radiographic and computed tomography follow-up showed excellent bone healing [5].
The outcome of all described waterproof cast techniques are adequate. Nevertheless, the price of some techniques is quite high [6]. A Swim cast is about 50 % cheaper than a traditional cast because less of the same material is needed in this technique.
Conclusion
In the treatment of greenstick or torus fracture of the distal radius in children, our findings indicate that Swim casts receive a better overall satisfaction score compared to traditional casts. Furthermore, among our patient cohort, treatment with a Swim cast (MOKcast technique) did not result in a higher complication rate in terms of bone healing and skin lesions.
Conflict of interest
None of the authors received financial or grant support for this study.
Contributor Information
Robert Jan Derksen, Phone: +31-6-81605166, Email: Rderksen@rkz.nl.
Joris P. Commandeur, Email: jp.commandeur@vumc.nl
Ronald Deij, Email: rdeij@rkz.nl.
Roelf S. Breederveld, Email: rbreederveld@rkz.nl
References
- 1.Wierzimok AA. Innovative patientenfreundliche Ruhigstellung mit Cast. Die Schwester/Der Pfleger. 2000;39:1018–1021. [Google Scholar]
- 2.Cohen AP, Shaw DL. Focused rigidity casting: a prospective randomised study. J R Coll Surg Edinb. 2001;46:265–270. [PubMed] [Google Scholar]
- 3.Kruse RW, Fracchia M, Boos M, Guille JT, Bowen JR. Goretex fabric as a cast underliner in children. J Pediatr Orthop. 1991;11:786–787. doi: 10.1097/01241398-199111000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Haley CA, DeJong ES, Ward JA, Kragh JF., Jr Waterproof versus cotton cast liners: a randomized, prospective comparison. Am J Orthop (Belle Mead NJ) 2006;35:137–140. [PubMed] [Google Scholar]
- 5.Dubowitz G, Miller DM. Cast adrift: Gortex cast liners allow greater patient activity. Wilderness Environ Med. 2003;14:167–168. doi: 10.1580/1080-6032(2003)14[167:CAGCLA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Shannon EG, DiFazio R, Kasser J, Karlin L, Gerbino P. Waterproof casts for immobilization of children’s fractures and sprains. J Pediatr Orthop. 2005;25:56–59. doi: 10.1097/00004694-200501000-00013. [DOI] [PubMed] [Google Scholar]


