Abstract
Background
The study objectives were to determine (a) the effects of group-mediated cognitive–behavioral interventions on change in performance self-efficacy, satisfaction with function, and with appearance among older, overweight/obese adults in poor cardiovascular health and (b) whether self-efficacy mediated change in 400-m walk time.
Methods
This translational, randomized controlled trial of physical activity and weight loss was conducted within community Cooperative Extension Centers. Participants were randomized to three intervention arms: Physical Activity, Weight Loss+ Physical Activity, or a Successful Aging education control.
Results
Across 18 months, the Weight Loss+Physical Activity intervention demonstrated greater improvements in self-efficacy, satisfaction with function, and appearance versus other trial arms. Physical Activity intervention participants also experienced significant improvements in self-efficacy and satisfaction with function versus those in Successful Aging. Self-efficacy mediated 400-m walk time at 18 months.
Conclusions
Both group-mediated cognitive–behavioral interventions yielded desirable improvements in social cognitions and preserved mobility improvements post-intervention.
Keywords: Group-mediated interventions, Older adults, Obesity, Physical activity, Mobility
Introduction
It is well recognized that older adults aged 65–75 years have a higher incidence of both cardiovascular disease [1] and the metabolic syndrome [2]. The burden of these health conditions limits mobility [3, 4], a consequence that compromises subsequent health status [5], reduces quality of life [6], and increases the future risk of institutionalization [7]. Recently, we conducted a theoretically based, translational, randomized controlled clinical trial of lifestyle interventions for older adults who were obese and had cardiometabolic dysfunction—the Cooperative Lifestyle Intervention Program [8]. The primary aim of the trial was to compare the effects of three treatments—Physical Activity, Weight Loss +Physical Activity, and Successful Aging education—on an 18-month change in a measure of mobility—400-m walk time—that is known to be related to important health outcomes [5, 9, 10]. The results of this trial were positive and revealed that Weight Loss+Physical Activity produced significantly better improvements in mobility than either Physical Activity or Successful Aging. The objective of the current investigation was to examine changes in social cognitive constructs targeted by the Physical Activity and Weight Loss+Physical Activity interventions and the role of self-efficacy as a mediator of the observed treatment differences in 400-m walk time.
Previous research with pre-frail and community-dwelling older adults suggests that participation in physical activity improves self-efficacy [11–13] and satisfaction with physical function [13]. However, to our knowledge, no existing research has examined changes in such process-related outcomes when considering intervening on multiple health behaviors simultaneously. Both a scientific statement by the American Heart Association [14] and one in cardiac rehabilitation [15] have identified the need to address such relationships in populations at risk for cardiovascular disease. In fact, Painter et al. [16] have emphasized that relatively few of the published investigations of health behavior interventions in the past decade actually operationalized and tested central theoretical processes of behavior change.
Our recently completed randomized control trial employed Physical Activity and Weight Loss+Physical Activity interventions that were evidence-based [17, 18] and guided by principles drawn from Bandura’s social cognitive theory and the group dynamics literature. Because our target population was physically compromised and the primary outcome was the 400-m walk time, two key motivational constructs from the social cognitive theory targeted for change within the interventions were self-efficacy for walking and outcome expectancies related to satisfaction with physical function and appearance.
Bandura [19] explains that the sources of information that determine self-efficacy are multiple and provides extensive evidence to support his position. For example, direct experience with either success or failure, modeling by watching others, being socially reinforced for progress by receiving praise from individuals or groups, imaginal experiences, and positive or negative physiological reactions can determine the strength of self-efficacy. Direct experience is considered to be the strongest source of efficacy information that contributes toward those beliefs. During an intervention that occurs over time, participants may be exposed to all of these determinants because of both systematically planned aspects of the intervention and nonsystematic experiences that may be a part of intervention exposure. Planned construction of the social environment of an intervention or treatment program can systematically focus the exposure of participants to a variety of self-efficacy determinants [20, 21]. Self-efficacy belief change is a marker for participants’ exposure to the totality of these experiences. When targeting change in self-efficacy, the foundation for hypotheses made on the basis of theory and past evidence is that the systematically planned experiences are the main contributors to any change.
Whereas an emphasis has been placed on the importance of developing self-efficacy in physical activity interventions among older adults [22], there is some evidence that both with and without the maintenance of activity self-efficacy will decay over time (see [23]). Elsewhere, we have argued that a different approach to intervention needs to be taken to avoid such decay. Specifically, participants need to be armed with the skills that allow them to continue to self-manage physical activity during maintenance and sustain their self-efficacy for long-term function [24–26]. The present trial aimed to accomplish this end.
In the older adult and physical activity literature, an agency component of social cognitive theory that has received less attention is outcome expectancies generally and satisfaction with function specifically [26]. A review of this construct in multiple theories in the health behavior change literature by Williams et al. [27] suggests that outcome expectancies deserve more attention. Whereas the focus of attention of physical activity research on outcome expectancies in the context of social cognitive theory has been on the distal physical and mental health benefits of physical activity [27], there has been less focus on the class of outcomes associated with self-reflection and self-evaluation. Bandura [19] clearly identifies the extent of anticipated self-satisfaction with progress in attainments as an important incentive in this class of outcomes. For the present trial, the outcome expectancies described by Bandura [19] as being self-evaluative reactions to personal behavior change were targeted as outcomes flowing from intervention experiences across the duration of the trial. Behavioral attainments themselves are not self-evaluative outcome expectancies. Self-evaluative reactions to these attainments, such as satisfaction with improved function, are the outcome expectancies. Inasmuch as the treatments in this trial were Physical Activity and Weight Loss+Physical Activity, these self-evaluative outcome expectancies follow from achieving goals that were targets of the respective intervention arms.
Thus, the purpose of the present investigation was twofold. The first purpose was to examine the effects of the different treatments on self-efficacy for walking and the outcome expectancies of satisfaction with this function and with appearance. Specifically, we tested the hypotheses that improvement in walking self-efficacy, satisfaction with function, and satisfaction with appearance would be greater in the Physical Activity and Weight Loss+Physical Activity treatments than in Successful Aging. In addition, we expected the effects of walking self-efficacy and satisfaction with function for Weight Loss+Physical Activity to be stronger than in Physical Activity and for satisfaction with appearance to change only in Weight Loss+Physical Activity. Our reasoning for these hypotheses was based on both theory and the published results of the primary outcome of the trial. As mentioned previously, a number of social determinants contribute to the development of self-efficacy beliefs [19], and many of these were part of the treatment during the trial. Specifically, however, the agency component of the social cognitive theory [19] identifies direct experience as the strongest of the influential determinants. Thus, the direct experience of improved mobility and losing weight should be reflected in improvements in older adults’ walking self-efficacy and in their outcome expectancies of satisfaction with physical function and appearance, respectively. In analyses of the primary outcome of this trial [8], we found that both Weight Loss+Physical Activity and Physical Activity treatments resulted in greater improvement in 400-m walk time than the Successful Aging treatment and that the Weight Loss+Physical Activity group lost considerable weight—7.7 % at 18 months—compared to either the Successful Aging or the Physical Activity group.
The second purpose was to empirically test whether changes in walking self-efficacy that participants experienced as a function of the group-mediated cognitive–behavioral counseling-related interventions mediated change in 400-m walk time. While a test of this hypothesis is theoretically meaningful, it also addresses two calls for such evidence. The first is the call of Painter et al. [16] for an increase in the conduct of such tests of health behavior change programs. The second is the 2010 American Heart Association’s [14] call for more evidence of the theory-based links between the target social cognitive constructs of interventions and the physical behaviors and outcomes changed.
Methods
Overview
The trial had an overall translational goal to deliver lifestyle interventions within existing community infrastructures. We were interested in whether the environment and staff of community Cooperative Extension Centers could be utilized to conduct lifestyle interventions in order to achieve important health outcomes for older adults aged 60–79 years with cardiometabolic dysfunction. From a translational perspective, the ability of centers and staff to deliver such interventions would expand the capacity for program delivery and the reach of potentially successful interventions.
The study recruited 288 participants aged 60–79 years from three counties (Forsyth, Davidson, and Guilford) in North Carolina. The urban area in Forsyth County is Winston-Salem, NC. It constitutes 60–65 % of the population (see www.aboutus.org/quickfacts.census.gov). The data for Guilford County mirror these data, with Greensboro being the urban area in this County. The Cooperative Extension Agencies in both counties are located on the borders of both cities and serve the rural populations. All of Davidson county is considered rural.
After baseline assessments were conducted by blinded personnel and the project manager had randomized participants to treatment, they returned for assessments at 6, 12, and 18 months. Participants were treated in eight waves, with all sessions being conducted indoors at the North Carolina County Extension Centers. Each wave within counties consisted of ~39 participants with ~13 in each treatment arm. A Data Safety and Monitoring Board routinely evaluated the execution of the study protocol and adverse events. Electronic copies of the intervention manuals and the study protocol are available upon request from the corresponding author.
All interventionists had degrees in the health sciences and were trained by the study investigators. A registered dietician provided oversight for the dietary intervention arm. The Successful Aging arm and portions of the Weight Loss+ Physical Activity arm were delivered by Cooperative Extension agents—also known as Family and Consumer Sciences educators—who are field faculty from North Carolina State University. These educators have degrees in Home Economics and/or Nutrition Education. Cooperative extension centers are located in all counties and on the Cherokee Reservation in North Carolina and in most counties nationwide. Cooperative extension specialists are trained to provide unbiased, research-based information to the public in such areas as agriculture, human nutrition, diet and health, food safety, gerontology, and human development.
Eligibility
The eligibility criteria identified ambulatory, overweight or obese, community-dwelling older adults who either had cardiovascular disease or cardiometabolic dysfunction, and evidence of self-reported limitations in mobility. The following were the inclusion criteria: (1) 60–79 years old; (2) <60 min/ week of moderate, structured physical activity; (3) body mass index (BMI)>28 kg/m2; (4) evidence of a myocardial infarction, percutaneous transluminal angioplasty, chronic stable angina, or cardiovascular surgery in the past 6 months or an Adult Treatment Panel III diagnosis of the metabolic syndrome [28]; (5) a self-reported mobility limitation; and (6) willingness to sign an informed consent and a Health Insurance Portability and Accountability Act HIPAA authorization form.
Exclusion criteria included: (1) baseline BMI≥40 kg/ m2; (2) bipolar depression or schizophrenia; (3) unstable angina, symptomatic congestive heart failure, or exercise-induced complex ventricular arrhythmias; (4) resting blood pressure >160/100 mmHg; (5) diagnosis of systemic diseases that precluded participants from safely participating in the interventions; (6) a fasting blood glucose>140 mg/dl, type 1 diabetes, or type 2 diabetes with insulin therapy; (7) active treatment for cancer; (8) significant visual or hearing impairment; (9) dementia, delirium, or impaired cognitive function; (10) participating in another medical intervention study; (11)>21 alcoholic drinks per week; (12) unable to walk unassisted; and (13) unable to speak or read English.
Recruitment, Enrollment, and Randomization
Recruitment occurred in a parallel schedule to the delivery of intervention waves over 2.5 years. The first person was enrolled on 17th January 2005 and the last person was closed out on 6th April 2010. Recruitment strategies included newspaper ads and direct mailings. Each participant was randomized to treatment by a project manager using a permuted block randomization scheme with stratification by wave.
Measures
Demographics/Chronic Disease Status
Demographics, medical history, and comorbidities were collected by self-report.
Self-Efficacy
The measure of self-efficacy for walking (i.e., task/performance efficacy) consisted of eight hierarchical items and was developed in a manner consistent with recommendations by Bandura [19, 29]. The stems for each item asked participants how confident they were that they could walk at a moderate pace without stopping for 5, 10, 15, 20, 25, 30, 35, or 40 min. For each question, a ten-point confidence scale was employed that ranged from 0 to 10. Walking self-efficacy scores were calculated by summing the participant’s confidence ratings across the eight questions and rescaling them to a score that ranged from 0 to 100. The construct validity and sensitivity to change for this method of assessing walking self-efficacy in older adults is supported by existing publications in aging [30–32].
Outcome Expectancies: Satisfaction with Function and Appearance
A nine-item satisfaction measure from a measure originally developed by Ray et al. [33] was used to assess the outcome expectancies of satisfaction with physical function and appearance; six items are related to physical function and three are related to appearance. Each item was rated on a seven-point scale that was scored from −3 to +3, with each value labeled by the following phrases: very dissatisfied (−3), somewhat dissatisfied (−2), a little dissatisfied (−1), neither (0), a little satisfied (+1), somewhat satisfied (+2), and very satisfied (+3). The measure has demonstrated good convergent validity and other psychometric properties [34] and has been used in several randomized controlled trials involving physical activity which found it sensitive to change in older adult populations [32, 34, 35].
Mobility
The 400-m walk time was used to assess mobility [36]. In this test, participants walk in a corridor on a course that is 20 m long (one loop is 40 m). The course has cones positioned on either end of the corridor, and participants must complete ten loops in performing the test. The test is performed individually, in an indoor facility, and under controlled conditions (see [8] for more details). In a study of middle- to older-aged women, the 400-m walk time had excellent stability (ICC=0.95) and was significantly related to the measured peak work capacity (VO2peak), physical activity, body composition, and balance [37]. Moreover, prospective analyses on healthy older adults have shown that performance on the 400-m walk time is predictive of mortality, incident cardiovascular disease, and disability [10].
Physical Activity Intervention
The Physical Activity intervention (48 total sessions) was developed based upon an evidence-based program for older adults [17, 18] and was conceptually driven by principles from Bandura’s social cognitive theory [19] and the group dynamics literature [20]. A major reason we used these two perspectives to guide intervention development is because both have been linked to the facilitation of treatment adherence (e.g., [19, 20, 38]) and offer protocols/skills in that regard. This group-mediated cognitive–behavioral intervention focused on developing a group-focused learning environment to foster (a) instruction and encourage participants’ practice of home-based activity and (b) their development of self-regulatory skills to carry out this activity. We used the group with which member participants identified to systematically focus and socially reinforce those planned experiences that contribute to the development of stronger self-efficacy beliefs. A brief synopsis of the use of the group is instructive.
The initial stages of the intervention consciously dwell on group formation and identity such that participants view themselves as being in a unique group and engage in setting normative group goals as well as individual goals. The group is consciously used as an agent of change and support [18, 20] through its motivation of group-focused learning. This group formation creates a normative environment in which ongoing practice of the self-regulatory skills taught and group discussion of weekly progress of walking as physical activity occur throughout the intensive portion of the intervention. The motivational advantages of group-focused counseling are well documented [20, 21, 24].
A primary goal was to gradually increase or shape physical activity in a home-based environment to 30+min of moderate to vigorous physical activity on most days of the week for a total of 150+min/week. Participants walked at a moderate intensity of “somewhat hard—13,” as assessed by the Borg Rating of Perceived Exertion Scale [39]. Weekly trackers (written self-monitoring logs) were used to document walking behavior.
The Physical Activity intervention involved two phases: intensive and maintenance. The 6-month intensive phase involved counseling sessions in a mix of three group sessions and one individual session per month. Group sessions lasted 90 min and individual sessions lasted 30 min. Each group session started with a 30- to 45-min period of walking followed by an interactive, group-motivated, behaviorally focused session. The behavior change skills learned over the course of the intensive phase served to promote self-regulated walking during the maintenance phase. The walking practiced during the group sessions in the intensive phase as well as the home-based activity serve as the direct experience that promotes individuals’ performance efficacy, a primary target of social cognitive change in the interventions (i.e., Physical Activity and Weight Loss+Physical Activity). The behavior change skills learned and practiced during the intensive phase encourage individuals to self-regulate and maintain their walking by virtue of increasing their goal-setting and planning skills and their ability to adapt and resume walking if they lapse. Below, the months of the intensive phase are described emphasizing the primary skills learned that would aid self-regulation during maintenance.
Intensive Phase
During the first 2 months of the intensive phase, participants were asked, as a group, to identify their primary motivations for becoming more active, and group leaders emphasized the risk of disability with aging. In addition, the group was introduced to the concepts of goal setting and self-monitoring; documenting minutes of walking in activity logs and learning how to adjust goals when warranted.
During months 3 and 4, group discussions focused on creating a physical activity program that had the flexibility to accommodate the multiple barriers that inevitably occur. During this period, strategies focused on the development of self-regulatory skills and a network of social support.
During months 5 and 6, group discussions focused on the concept of the group and its participants perceiving themselves as physically active, independent older adults. They were taught how to use environmental cues to facilitate activity goals and how to avoid or deal with relapses when they occurred. To avoid ongoing group dependency, in months 3 through 6, the intervention progressively focused on weaning participants from dependency on the interventionist and group toward self-managed physical activity.
Maintenance Phase
Months 7–18 constituted the maintenance phase with a reduction in the frequency of staff contact to two per month. One contact was a group session with the group and its members discussing progress and the second was a telephone contact that lasted ~10–20 min. For both contacts, discussion mirrored the weekly check-in during the intensive phase in that physical activity goals were discussed, specific plans of action implemented, and self-regulatory skills reinforced.
Weight Loss and Physical Activity Intervention
The combined treatment arm (48 total sessions) involved the physical activity program described above in conjunction with dietary weight loss using the same conceptual model as Physical Activity for group-mediated, cognitive–behavioral counseling [17, 18]. Thus, the same group-focused learning environment fostered (a) instruction and encouraged participant practice of both home-based activity and dietary weight loss and (b) the development of self-regulatory skills to carry out the relevant actions related to activity and diet behavior. The weight loss goal for the intensive phase was to reduce caloric intake to produce a weight loss of ~0.3 kg/ week for the first 6 months, for a total loss in mass of 7–10 %. During the maintenance phase, participants were encouraged to continue weight loss as long as BMI was ≥20 kg/m2; however, the primary focus was on weight maintenance.
At program inception, participants were assigned a daily energy intake goal based on their baseline weight. A 1,200-to 1,500-kcal goal was used for those weighing<250 lbs and a 1,500- to 1,800-kcal goal for those weighing ≥250 lbs. Recommendations for choices of foods were based on the MyPyramid Food Guidance System. Participants were given food tracking booklets, and at the end of each week, an average was calculated for their calorie and fat consumption. The intervention was co-delivered by a trained interventionist and Family and Consumer Sciences educators in the North Carolina County Extension Centers.
As with Physical Activity treatment, the intensive phase sessions lasted 90 min for a given session; the first segment reviewed participants’ progress from the previous session. After a private weigh-in, participants provided a confidential progress update and identified the problems encountered. Progress was highlighted with strong positive feedback. Reported difficulties were dealt with through advice as well as group support for common difficulties in the second segment of the session. The second segment involved group-mediated counseling that focused on skill training related to cognitive–behavioral self-management skills, nutritional training, and topics in exercise science. Each month, there was a cooking demonstration or food tasting that illustrated the preparation of palatable, low-fat, low-calorie foods. The final component of the second segment consisted of setting individual goals for the coming week and encouragement for the group members to try the food-related activity learned.
The interventionists placed a major focus on increasing group members’ abilities to self-regulate eating behavior. This involved (a) promoting awareness of how different internal and external factors promote eating [40]; (b) having members track and discuss personal triggers to eating; (c) teaching them to stop and think before eating; (d) using a five-stage problem-solving model to develop specific action plans for difficult situations [41]; (e) normalizing slips and relapses; and (f) using the individual sessions (i.e., first segment of each 90-min session) to provide feedback and reinforcement to participants. As in the Physical Activity arm, the maintenance phase involved two contacts each month: one contact with the group and its members and one individual telephone counseling call.
Successful Aging Education Intervention
The Successful Aging education treatment was developed by faculty at the North Carolina State University who serve as Extension Specialists for North Carolina County Extension Centers. Each scripted lesson was taught by a Family and Consumer Sciences agent in each county and was tailored for older adults. The purpose and structure of the Successful Aging group was to (1) control for general levels of staff and participant interactions; (2) optimize recruitment and to ensure participants’ ongoing cooperation and retention; (3) select a control intervention that would have minimal effects on the primary outcome; and (4) utilize an intervention that had tangible benefit. Participants in the Successful Aging arm met weekly for the first 2 months, monthly through the sixth month, and then bimonthly until the end of the study—a total of 18 sessions.
In the Successful Aging education treatment, participants were taught how to actively “take charge” of their health as individuals. Examples of the topics covered included: how the body changes with aging, preventing or delaying disease, eating for good health, positive attitudes toward aging, family relationships and caregiving, and talking to health-care providers. The Successful Aging intervention differed from the other two arms of the study in that participants did not receive a progressive, supervised program of physical activity or diet for weight loss; however, both physical activity and nutrition for aging were addressed as separate and distinct topics. Also, there was no attempt to systematically use unique group identity, motivation, and support as in the other study arms. Education was delivered in a class-like setting with standard opportunity for some question-and-answer interaction interspersed with the delivery of educational information.
As described in the overview, after baseline assessments and randomization to treatment, participants in each wave returned for assessments at 6, 12, and 18 months.
Statistical Analyses
The primary analyses used linear mixed models with covariates including the baseline outcome assessment, county, wave within county, visit (6, 12, and 18 months), and gender. Participant was included as a random effect to account for the within-participant correlation. Adjusted means were used to account for the variables in the primary model. The effects of treatment on self-efficacy, satisfaction with function, and satisfaction with appearance were estimated using two separate contrasts that compared the treatments of Successful Aging education and Physical Activity to the Weight Loss+Physical Activity treatment. Tests of mediation used the approach of MacKinnon et al. [42]; these analyses also included baseline weight, county, wave within county, and gender as covariates.
Results
Inclusion, Retention/Adherence, and Descriptive Characteristics
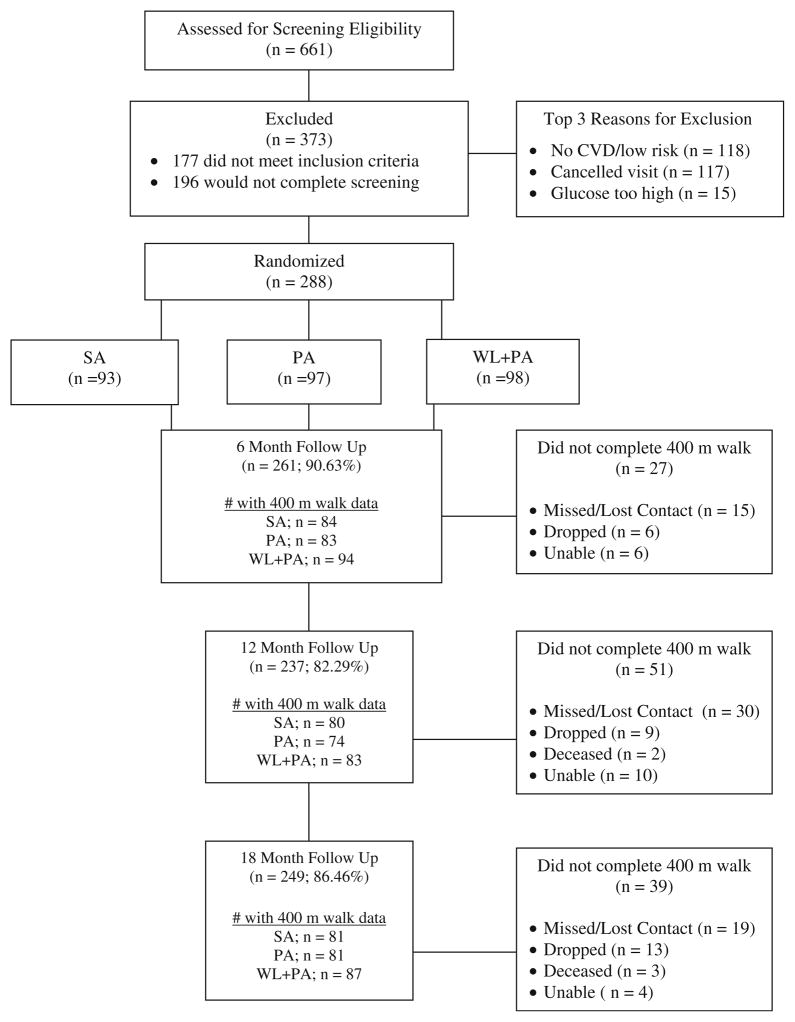
The CONSORT diagram (Fig. 1) shows that 86.5 % of the participants completed the 18-month follow-up; using a mixed model, we were able to conduct analyses for mobility (400-m walk time) on 93.4 % of those randomized. Participants in the Successful Aging treatment attended a mean (SD) of 70.9 % (±26.5) of the scheduled sessions, whereas for the Physical Activity treatment it was 79.8 % (±24.6) and for the Weight Loss+Physical Activity treatment was 88.2 % (±25.2). Women made up 67.0 % of this cohort, and 81.9 % were white. As shown in Table 1, the participants were socioeconomically diverse, had multiple comorbidities, and all were either overweight or obese.
Fig 1.
CONSORT Diagram. SA successful aging education control, PA physical activity, WL+PA weight loss+physical activity, CVD cardiovascular disease; dropped, no longer wanted to be contacted; missed/ lost contact, unable to attend screening visit or unable to locate the participant
Table 1.
Characteristics of participants
| Characteristic | Treatment group, mean±SD or N (%)
|
||
|---|---|---|---|
| SA (N=93) | PA (N=97) | WL+PA (N=98) | |
| Age (years) | 67.2±4.8 | 67.2±5.1 | 66.8±4.6 |
| Sex | |||
| Male | 31 (33.3 %) | 33 (34.0 %) | 31 (31.6 %) |
| Female | 62 (66.7 %) | 64 (66.0 %) | 67 (68.4 %) |
| Race | |||
| White | 76 (81.7 %) | 76 (78.4 %) | 84 (85.7 %) |
| Black | 15 (16.1 %) | 19 (19.6 %) | 14 (14.3 %) |
| Other | 2 (2.2 %) | 2 (2.1 %) | 0 (0.00 %) |
| Education | |||
| Less than high school | 3 (3.2 %) | 2 (2.1 %) | 1 (1.0 %) |
| High school/high school and some college | 43 (46.2 %) | 47 (48.5 %) | 47 (48.0 %) |
| At least associate’s degree | 47 (50.5 %) | 48 (49.5 %) | 50 (51.0 %) |
| BMI | 32.6±3.5 | 32.8±3.9 | 33.1±4.1 |
| Comorbidities | |||
| Myocardial infarction | 10 (10.8 %) | 4 (4.1 %) | 7 (7.1 %) |
| Angina | 11 (11.8 %) | 17 (17.5 %) | 13 (13.3 %) |
| Hypertension | 60 (64.5 %) | 65 (67.0 %) | 73 (74.5 %) |
| Diabetes | 18 (19.4 %) | 15 (15.5 %) | 16 (16.3 %) |
| Arthritis | 61 (65.6 %) | 49 (50.5 %) | 61 (62.2 %) |
| Cancer | 17 (18.3 %) | 21 (21.6 %) | 19 (19.4 %) |
| Metabolic syndrome | 49 (52.7 %) | 54 (55.7 %) | 58 (59.2 %) |
SA successful aging education control, PA physical activity, WL+PA weight loss+physical activity, BMI body mass index
Back Ground: Weight Loss, Levels of Physical Activity, and Mobility
We briefly summarize the values for weight loss and physical activity here given their relation to our research questions concerning walking self-efficacy and the outcome expectancies of satisfaction with function and appearance. More detail is available in the main outcomes paper [8].
Participants in Successful Aging and Physical Activity treatments experienced very small decreases in weight, approximately 1.0 % after randomization, whereas the Weight Loss+Physical Activity group had lost 8.5 % at 6 months and essentially retained this loss at 18 months, 7.7 % (p<0.0001). In addition, there were significant group differences (p<0.01) for minutes of moderate physical activity, with the Physical Activity and the Weight Loss+ Physical Activity treatments increasing their minutes of moderate physical activity over time as compared to the Successful Aging group (p<0.02); the average adjusted means at the months of follow-up assessments were 120.4 min/week for Successful Aging, 156.4 min/week for Physical Activity, and 189.4 min/week for Weight Loss+Physical Activity.
There were also significant treatment effects for mobility performance such that the Weight Loss+Physical Activity group significantly improved their 400-m walk time compared to Successful Aging (p<0.001) and Physical Activity (p<0.02). The greatest decrease in walk time was observed at 6 months following the intensive phase of the intervention. At 18 months, the Weight Loss+Physical Activity group sustained its improvement in comparison to the other two conditions where performance improvements decayed.
With these behavioral effects as backdrop, we now present the results for our social cognitive variables. Both treatment and mediation hypotheses are examined.
Effects of the Treatments on Walking Efficacy and Outcome Expectancies
Mixed model analyses of covariance controlling for the baseline measure of interest, age, and gender resulted in significant main effects for walking self-efficacy (F2,492= 25.93, p<0.0001) and the outcome expectancies of satisfaction with function (F2,492 =14.73, p <0.0001) and satisfaction with appearance (F2,492 =27.37, p < 0.0001). As illustrated in Tables 2, 3, and 4, across the 18 months of the study, the Weight Loss+Physical Activity group experienced greater improvements in self-efficacy, satisfaction with function, and satisfaction with appearance as compared to either Successful Aging or Physical Activity. Physical Activity experienced significant improvements in self-efficacy and satisfaction with function as compared to Successful Aging, but did not differ on the measure of satisfaction with appearance.
Table 2.
Walking self-efficacy: raw data for each time point and average adjusted values from the linear model
| Time of assessment | Treatment group
|
||
|---|---|---|---|
| SA | PA | WL+PA | |
| Baseline, M (±SD) | 65.1 (28.2) | 60.8 (27.6) | 60.3 (28.8) |
| 6 months, M (±SD) | 67.8 (30.3) | 79.8 (25.8) | 86.3 (20.4) |
| 12 months, M (±SD) | 67.7 (28.1) | 80.1 (26.7) | 87.2 (21.3) |
| 18 months, M (±SD) | 65.2 (30.3) | 78.6 (25.6) | 85.1 (25.2) |
| Average-adjusted M (±SE) | 64.9 (2.2) | 79.2 (2.2) | 86.6 (2.1) |
| 95 % CIs for adjusted M | 60.5–69.2 | 74.9–83.5 | 82.5–90.7 |
SA successful aging education control, PA physical activity, WL+PA weight loss+physical activity, CIs confidence intervals
Table 3.
Satisfaction with function: raw data for each time point and average adjusted values from the linear model
| Time of assessment | Treatment group
|
||
|---|---|---|---|
| SA | PA | WL+PA | |
| Baseline, M (±SD) | −1.0 (1.4) | −1.2 (1.4) | −1.2 (1.4) |
| 6 months, M (±SD) | −0.3 (1.6) | 0.3 (1.7) | 0.7 (1.4) |
| 12 months, M (±SD) | −0.0 (1.5) | 0.5 (1.7) | 0.6 (1.7) |
| 18 months, M (±SD) | −0.2 (1.6) | 0.3 (1.5) | 0.7 (1.7) |
| Average-adjusted M (±SE) | −0.3 (0.1) | 0.3 (0.1) | 0.7 (0.1) |
| 95 % CIs for adjusted M | −0.5, −0.3 | 0.1–0.6 | 0.5–0.9 |
The satisfaction seven-point scale was scored from −3 to +3 using the following phrases as anchors: very dissatisfied (−3), somewhat dissatisfied (−2), a little dissatisfied (−1), neither (0), a little satisfied (+1), somewhat satisfied (+2), and very satisfied (+3). Thus, for example, note at baseline that the SA group (M=−1.0) was a little dissatisfied with their physical function
SA successful aging education control, PA physical activity, WL+PA weight loss+physical activity, CIs confidence intervals
Table 4.
Satisfaction with appearance: raw data for each time point and average adjusted values from the linear model
| Time of assessment | Treatment group
|
||
|---|---|---|---|
| SA | PA | WL+PA | |
| Baseline, M (±SD) | −2.1 (1.0) | −2.0 (1.1) | −2.1 (1.1) |
| 6 months, M (±SD) | −1.5 (1.4) | −1.2 (1.4) | −0.0 (1.8) |
| 12 months, M (±SD) | −1.1 (1.5) | −1.0 (1.5) | 0.1 (1.9) |
| 18 months, M (±SD) | −1.3 (1.6) | −1.1 (1.5) | −0.2 (1.9) |
| Average-adjusted M (±SE) | −1.3 (0.1) | −1.2 (0.1) | −0.1 (0.1) |
| 95 % CIs for adjusted M | −1.6, −1.0 | −1.5, −0.9 | −0.3, 0.2 |
The satisfaction seven-point scale was scored from −3 to +3 using the following phrases as anchors: very dissatisfied (−3), somewhat dissatisfied (−2), a little dissatisfied (−1), neither (0), a little satisfied (+1), somewhat satisfied (+2), and very satisfied (+3). Thus, for example, note at baseline that the PA group (M=−2.0) was somewhat dissatisfied with their appearance
SA successful aging education control, PA physical activity, WL+PA weight loss+physical activity, CIs confidence intervals
Test of Mediation
Table 5 provides the results for the direct effects in the mediation analysis. In this table, α represents the effect of the two different treatment contrasts—Weight Loss+ Physical Activity versus Physical Activity and Successful Aging—on walking self-efficacy scores, β the effect of walking self-efficacy scores at 6 months on 18-month 400-m walk time, and τ′ the effect of the treatment contrast on 400-m walk time. We used the approach of MacKinnon et al. [42] to estimate the αβ=τ−τ′ effect, a recognized test for mediation. The αβ effect for the Successful Aging versus Weight Loss+Physical Activity contrast was estimated to be 15.04 (95% CI=9.04–21.84), whereas for the Successful Aging versus Physical Activity contrast it was 9.54 (95% CI=3.84–15.86). The effects of the two treatment contrasts on 400-m walk time became non-significant with walking self-efficacy in the model (p<0.0001 for walking self-efficacy), indicating that this social cognition completely mediated the impact of the intervention effects on 400-m walk time.
Table 5.
Direct effects in mediational analysis
| Effect tested | Estimate | Standard error | t value |
|---|---|---|---|
| SA versus WL+PA | |||
| α | −18.86 | 3.49 | −5.41** |
| β | −0.79 | 0.09 | −8.76** |
| τ′ | 18.67 | 5.46 | 3.42** |
| PA versus WL+PA | |||
| α | −6.90 | 1.97 | −1.97* |
| β | −0.79 | 0.09 | −8.76** |
| τ′ | 8.60 | 5.48 | 1.58 |
α represents the effect of the two different treatment contrasts—WL+ PA versus PA and SA—on walking self-efficacy scores, β is the effect of walking self-efficacy scores at 6 months on 18-month 400-m walk time, and τ′ is the effect of the treatment contrast on 400-m walk time
SA successful aging education control, PA physical activity, WL+PA weight loss+physical activity
p<0.05,
p<0.001
Discussion
Our results are consistent with the theoretical basis and the cognitive–behavioral training of this randomized control trial. They indicate that older adults in the Weight Loss+ Physical Activity intervention significantly improved their walking self-efficacy and outcome expectancies of satisfaction with physical function and appearance at levels greater than either Physical Activity or Successful Aging treatments. Relative to declines in the social cognitive variables (i.e., self-efficacy) reported by McAuley et al. [23] in the older adult physical activity literature, our intervention provides a positive contrast. Based on their examination of the decay in self-efficacy over time, McAuley et al. [23] recommended that future interventions should plan to deal with the difficulty of transitioning to maintenance by using strategies to bolster and maintain efficacy while participants are still in the intensive phase (p. 82). The present trial used such strategies (focal strategies: months 3–6 for both the Physical Activity and the Weight Loss+Physical Activity intervention arms). Their success in promoting maintenance has been previously reported for other group-mediated cognitive–behavioral counseling interventions with older adults (e.g., [17, 18]).
The group-mediated cognitive–behavioral counseling-type intervention used in this study promoted maintenance as follows. The Weight Loss+Physical Activity version of the intervention reflected improvements in walking self-efficacy at 6 months and then maintenance of improved efficacy through the remaining 12 months of the trial. This pattern followed for the outcome expectancies related to satisfaction with function and appearance. It is also noteworthy that the Physical Activity group-mediated cognitive–behavioral counseling intervention led to significant improvements in self-efficacy and satisfaction with function as compared to the Successful Aging treatment, a point we will address later. The improvements in self-efficacy across the 18 months of the study paralleled improvements observed for the 400-m walk time [8]. Also, the improvement in the outcome expectancies of satisfaction with function and appearance follow two other improvements in the Weight Loss+Physical Activity group; that is, the attainments of increased physical activity and weight loss.
A social cognitive theory interpretation would suggest that the treatment arm experiences that led to these benefits constituted the direct experience that (a) fostered increased walking self-efficacy, (b) confirmed progress with mobility, (c) enhanced satisfaction surrounding this functional improvement, and (d) enhanced evaluation of and satisfaction with appearance. These changes are theorized to operate in concert and serve to facilitate persistent and adherent behavior. Participants’ self-evaluative reactions to their own improvements across the course of the trial are postulated to contribute to the observed changes in social cognitions [19]. Moreover, an additional facet of this theorizing suggests that self-efficacy functions as a possible mechanism thought to stimulate improvement in functional outcomes. Hence, we tested the hypothesis that changes in walking self-efficacy would mediate the effects of treatment on changes in mobility—400-m walk time. We found that walking self-efficacy assessed at 6 months clearly mediated the impact of the intervention on improved 400-m walk time a full year later, lending credence to the argument that the development of efficacy is one of the potential mechanisms underlying the increase in physical activity and improved mobility. The finding also supports the call by Painter et al. [16] for testing of the theoretical tenets of health behavior change interventions as well as addressing a similar recommendation for future research by the American Heart Association [14].
Although the identification of mediators of interventions is needed, careful interpretation about their cause is important. During any systematically delivered intervention, more than a single factor may operate to change a targeted marker of motivational process. The marker we assessed in the present investigation was self-efficacy beliefs. Given that the intervention protocols concentrated on planned, weekly counseling to influence several determinants of efficacy beliefs, we would be remiss not to draw attention to the planned group influence which provided socially reinforced feedback and supported progress of each group member. We therefore caution readers not to interpret the changes in efficacy solely to individual direct experience based upon the above mediational analysis. As noted in our introduction, Bandura [19] clearly stipulates that there are multiple factors that can collectively contribute to self-efficacy beliefs, such as direct experience with the behavior in question, social support, vicarious experience, and social influence factors that stem from being part of a group. Neither the purpose nor the design of our study was to isolate determinants of change in self-efficacy. While change in self-efficacy beliefs mediated the effect that the intervention had on improvement in mobility, this change is a product of a number of determinants for which self-efficacy is a marker.
In comparing the results to those in the existing research literature, there are some similar patterns to previous studies and some that are unique. The common intervention model in the studies is the use of a group-mediated cognitive–behavioral intervention coupled with training in the behaviors targeted for change in the respective study treatments. The behavioral and social cognitive improvement observed in the Physical Activity and Weight Loss+Physical Activity arms of this trial are of a similar nature to those observed in other intervention studies of asymptomatic and symptomatic older adults which used the group-mediated cognitive–behavioral intervention model [17, 18, 35]. However, the findings of the current trial are unique in several respects. First, to the best of our knowledge, it is unique that mobility in older, functionally compromised obese adults with either cardiovascular disease or cardiometabolic dysfunction was improved by coupling together change in both weight and physical activity. Second, it is clear that both losing weight and increasing physical activity must be addressed to attain this improvement in 400-m walk time and sustain it over 18 months. As noted earlier, data from the main trial results [8] revealed that at 6 months, participants in the Physical Activity intervention had better mobility than Successful Aging participants, but by 18 months, this benefit was lost while the benefits achieved in the Weight Loss+Physical Activity treatment group were sustained. Overall, the Weight Loss+Physical Activity arm had greater improvements in self-efficacy and satisfaction with function than either the Successful Aging or Physical Activity arms.
Collectively, these findings suggest that while the group-mediated cognitive–behavioral interventions for Physical Activity and Weight Loss+Physical Activity yielded desirable improvements, there is added value in concurrently addressing change in both weight and physical activity when the focus is on mobility. We suggest that the walking self-efficacy and mobility improvements in this trial arm may have occurred for several reasons, all framed by social cognitive theory. Bandura [19, 29] points out that self-efficacy, outcome expectancies, and the self-reflection on improving outcomes likely operate in concert over time. These factors, along with social factors experienced during the intervention’s intensive phase (e.g., social reinforcement, group influences), help to guide the persistence necessary to generate the sustained outcomes of improved mobility, weight loss, and improved physical activity observed for the Weight Loss+Physical Activity participants at 18 months. Thus, reasons for the improvement of these individuals could be (a) greater motivation to be physically active given observable weight loss, (b) their objective and perceptual view of physical activity may be that it is less difficult after weight loss, and/or (c) successful change in dietary behaviors might affect self-efficacy for the walking performance of participants. Regarding this latter point, Bandura [19] argues that when the development of competencies is socially structured such that participants acquire skills from different domains together, some generality of perceived efficacy can occur. He calls this co-development, and conjoined interventions such as Weight Loss+Physical Activity may provide the direct experience for this to occur. For example, in cardiac rehabilitation, Ewart [43] suggests that co-development of different behaviors (e.g., resistance training, flexibility, and walking) is wise and occurs via direct experience and interpretive counseling by program staff.
We would be remiss if we did not draw attention to some limitations concerning the treatment manipulations. We stressed conscious use of the group as a motivational environment in which participants in the Physical Activity and the Weight Loss+Physical Activity treatments learned about and practiced change [20, 21]. However, we did not obtain a treatment check that verified group formation and identity. Such a check would have validated that the groups in the two treatment interventions were true groups unlike the collection of individuals in the Successful Aging arm of the trial. In previous work using the group-mediated cognitive–behavioral intervention model in a short physical activity intervention with postnatal mothers, a manipulation check confirmed group cohesion for the treatment group [44, 45]. In future trials using the group-mediated approach, we advocate measuring both cohesion and therapeutic alliance [20, 21, 38].
The promising translational nature of this trial should be noted. Community health infrastructures were used in its delivery illustrating that, with modest training, the existing health resource capacity in counties can be effective in delivering safe lifestyle-oriented interventions to enhance behavior and belief change of at-risk older adults. The trial is also unique in that the combined behavioral intervention involving both weight loss and physical activity was effective in improving mobility, a critical activity to preserve older adults’ independence and help sustain other changes observed in the intervention.
While the translational implications of this research are of note, it is important to emphasize other strengths of this randomized control trial in light of critiques of health behavior research [16]. The interventions were theory-driven and evidence-based and examined in a manner where hypotheses drawn from theory (i.e., mediation) were tested. The independent and dependent measures used in these tests were correspondent (i.e., walking efficacy and satisfaction with function corresponded to a known estimate of functional mobility, 400-m walk time) and had been used in published research with older adults. As noted by Painter et al. [16] in their review of health behavior investigations, such characteristics are in the minority when examining the research literature. Finally, by examining outcome expectancies in addition to self-efficacy, we addressed a call by Williams et al. [27] for further research on this concept.
Acknowledgments
Support for this study was provided by the National Heart, Lung, and Blood Institute grant (HL076441-01A1), the National Institutes for Aging grant (P30 AG021332), and the General Clinical Research Center grant (M01-RR007122).
Footnotes
Trial Registration: Clinicaltrials.gov Identifier: NCT00119795
Conflict of Interest Statement The authors have no conflicts of interest to disclose.
Contributor Information
Lawrence Brawley, College of Kinesiology, University of Saskatchewan, Saskatoon, SK, Canada.
W. Jack Rejeski, Email: rejeski@wfu.edu, Department of Health and Exercise Science, Wake Forest University, P.O. Box 7868, Winston-Salem, NC 27109, USA. Department of Geriatric Medicine, Wake Forest University, Winston-Salem, NC, USA.
Jill E. Gaukstern, Department of Health and Exercise Science, Wake Forest University, P.O. Box 7868, Winston-Salem, NC 27109, USA.
Walter T. Ambrosius, Department of Biostatistical Sciences, Wake Forest University School of Medicine, Winston-Salem, NC, USA.
References
- 1.Yazdanyar A, Newman AB. The burden of cardiovascular disease in the elderly: Morbidity, mortality, and costs. Clin Geriatr Med. 2009;25:563–577. doi: 10.1016/j.cger.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNeill AM, Katz R, Girman CJ, et al. Metabolic syndrome and cardiovascular disease in older people: The Cardiovascular Health Study. J Am Geriatr Soc. 2006;54:1317–1324. doi: 10.1111/j.1532-5415.2006.00862.x. [DOI] [PubMed] [Google Scholar]
- 3.Ettinger WH, Jr, Fried LP, Harris T, Shemanski L, Schulz R, Robbins J. Self-reported causes of physical disability in older people: The Cardiovascular Health Study. CHS Collaborative Research Group [see comments] J Am Geriatr Soc. 1994;42:1035–1044. doi: 10.1111/j.1532-5415.1994.tb06206.x. [DOI] [PubMed] [Google Scholar]
- 4.Guralnik JM, LaCroix AZ, Abbott RD, et al. Maintaining mobility in late-life. 1. Demographic characteristics and chronic conditions. Am J Epi. 1993;137:845–857. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 5.Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc. 2000;48:493–498. doi: 10.1111/j.1532-5415.2000.tb04994.x. [DOI] [PubMed] [Google Scholar]
- 6.Ades PA, Savage PD, Tischler MD, Poehlman ET, Dee J, Niggel J. Determinants of disability in older coronary patients. Am Heart J. 2002;143:151–156. doi: 10.1067/mhj.2002.119379. [DOI] [PubMed] [Google Scholar]
- 7.Branch LG, Jette AM. A prospective study of long-term care institutionalization among the aged. Am J Public Health. 1982;72:1373–1379. doi: 10.2105/ajph.72.12.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rejeski WJ, Brubaker PH, Goff DC, Jr, et al. Translating weight loss and physical activity programs into the community to preserve mobility in older, obese adults in poor cardiovascular health. Arch Intern Med. 2011;171:47–67. doi: 10.1001/archinternmed.2010.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lampinen P, Heikkinen E. Reduced mobility and physical activity as predictors of depressive symptoms among community-dwelling older adults: An eight-year follow-up study. Aging Clin Exp Res. 2003;15:205–211. doi: 10.1007/BF03324501. [DOI] [PubMed] [Google Scholar]
- 10.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. J Am Med Assoc. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 11.McAuley E, Katula J. Physical activity interventions in the elderly: Influence on physical health and psychological function. In: Schulz R, Maddox G, Lawton MP, editors. Annual Review of Gerontology and Geriatrics. New York: Springer Publication Company; 1998. pp. 111–154. [Google Scholar]
- 12.Rejeski WJ, Miller ME, Foy CG, Messier SP, Rapp S. Self-efficacy and the progression of functional limitations and self-reported disability in older adults with knee pain. J Gerontol: Soc Sci. 2001;56:S261–S265. doi: 10.1093/geronb/56.5.s261. [DOI] [PubMed] [Google Scholar]
- 13.Rejeski WJ, King AC, Katula JA, et al. Physical activity in pre-frail older adults: Confidence and satisfaction related to physical function. J Gerontol: Psychol Sci. 2008;63:19–26. doi: 10.1093/geronb/63.1.p19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: A scientific statement from the American Heart Association. Circulation. 2010;122:406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berkhuysen MA, Nieuwland W, Buunk BP, Sanderman R, Rispens P. Change in self-efficacy during cardiac rehabilitation and the role of perceived overprotectiveness. Patient Educ Counsel. 1999;38:21–32. doi: 10.1016/s0738-3991(98)00115-3. [DOI] [PubMed] [Google Scholar]
- 16.Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: A systematic review. Ann Behav Med. 2008;35:358–362. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- 17.Brawley LR, Rejeski WJ, Lutes L. A group-mediated cognitive–behavioral intervention for increasing adherence to physical activity in older adults. J Appl Biobehav Res. 2000;5:47–67. [Google Scholar]
- 18.Rejeski WJ, Brawley LR, Ambrosius W, et al. Older adults with chronic disease: The benefits of group mediated counseling in the promotion of physically active lifestyles. Health Psychol. 2003;22:414–423. doi: 10.1037/0278-6133.22.4.414. [DOI] [PubMed] [Google Scholar]
- 19.Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- 20.Yalom ID. The Theory and Practice of Group Psychotherapy. 5. New York: Basic Books; 2005. [Google Scholar]
- 21.Newton-John TR, Geddes J. The non-specific effects of group-based cognitive–behavioural treatment of chronic pain. Chron Illness. 2008;4:199–208. doi: 10.1177/1742395308091868. [DOI] [PubMed] [Google Scholar]
- 22.McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exp Sport Sci Rev. 2000;28:85–88. [PubMed] [Google Scholar]
- 23.McAuley E, Mailey EL, Mullen SP, et al. Growth trajectories of exercise self-efficacy in older adults: Influence of measures and initial status. Health Psychol. 2011;30:75–83. doi: 10.1037/a0021567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rejeski WJ, Brawley LR. Functional health: Innovations in research on physical activity with older adults. Med Sci Sports Exerc. 2006;38:93–99. doi: 10.1249/01.mss.0000183191.65316.0a. [DOI] [PubMed] [Google Scholar]
- 25.Rejeski WJ, Brawley LR, Jung ME. Self-management in geriatric medicine. In: Halter J, editor. Hazzard’s Principles of Geriatric Medicine and Gerontology. 6. New York: McGraw-Hill; 2008. pp. 325–341. [Google Scholar]
- 26.Rejeski WJ, Tian L, Liao Y, McDermott MM. Social cognitive constructs and the promotion of physical activity in patients with peripheral artery disease. J Cardpulm Rehab Prev. 2008;28:65–72. doi: 10.1097/01.HCR.0000311512.61967.6e. [DOI] [PubMed] [Google Scholar]
- 27.Williams DM, Anderson ES, Winett RA. A review of the outcome expectancy construct in physical activity research. Ann Behav Med. 2005;29:70–79. doi: 10.1207/s15324796abm2901_10. [DOI] [PubMed] [Google Scholar]
- 28.Expert Panel on Detection EaToHBCiA. Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 29.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13:623–650. [Google Scholar]
- 30.McAuley E, Blissmer B, Katula J, Duncan T, Mihalko SL. Physical activity, self-esteem, and self-efficacy relationships in older adults: A randomized controlled trial. Ann Behav Med. 2000;22:131–139. doi: 10.1007/BF02895777. [DOI] [PubMed] [Google Scholar]
- 31.Rejeski WJ, Craven T, Ettinger WH, Jr, McFarlane M, Shumaker S. Self-efficacy and pain in disability with osteoarthritis of the knee. J Gerontol: Psychol Sci. 1996;51:24. doi: 10.1093/geronb/51b.1.p24. [DOI] [PubMed] [Google Scholar]
- 32.Rejeski WJ, Shelton B, Miller ME, Dunn AL, Sallis JF. Mediators of increased physical activity and change in subjective well-being: Results from the Activity Counseling Trial (ACT) J Health Psychol. 2001;6:159–168. doi: 10.1177/135910530100600206. [DOI] [PubMed] [Google Scholar]
- 33.Ray KM, Hector LL, Lynes LK, Stewart AL, Painter PL, Dibble SL. Assessment of satisfaction with physical fitness in kidney transplant recipients. Med Sci Sports Exerc. 1996;28(Supplement):S7–S8. [Google Scholar]
- 34.Reboussin BA, Rejeski WJ, Martin KA, et al. Correlates of satisfaction with body function and body appearance in middle- and older aged adults: The Activity Counseling Trial (ACT) Psychol Health. 2000;15:239–254. [Google Scholar]
- 35.Rejeski WJ, Focht BC. Aging and physical disability: On integrating group and individual counseling with the promotion of physical activity. Exerc Sport Sci Rev. 2002;30:166–170. doi: 10.1097/00003677-200210000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Simonsick EM, Montgomery PS, Newman AB, Bauer DC, Harris T. Measuring fitness in healthy older adults: The health ABC long distance corridor walk. J Am Geriatr Soc. 2001;49:1544–1548. doi: 10.1046/j.1532-5415.2001.4911247.x. [DOI] [PubMed] [Google Scholar]
- 37.Gabriel KKP, Rankin RL, Lee C, Charlton ME, Swan PD, Ainsworth BE. Test–retest reliability and validity of the 400-meter walk test in healthy, middle-aged women. J Phys Act Health. 2010;7:649–657. doi: 10.1123/jpah.7.5.649. [DOI] [PubMed] [Google Scholar]
- 38.Meichenbaum D, Turk DC. Facilitating Treatment Adherence: A Practitioner’s Guidebook. New York: Plenum; 1987. [Google Scholar]
- 39.Borg G. Perceived Exertion and Pain Scales. Champaign, IL: Human Kinetics; 1998. [Google Scholar]
- 40.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59:739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- 41.Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. J Consult Clin Psychol. 2001;69:722–726. [PubMed] [Google Scholar]
- 42.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ewart CK. Self-efficacy and recovery from heart attack: Implications for a social cognitive analysis of exercise and emotion. In: Maddux JE, editor. Self-efficacy, Adaptation, and Adjustment: Theory, Research, and Application. New York: Plenum; 1995. pp. 203–226. [Google Scholar]
- 44.Cramp AG, Brawley LR. Moms in motion: A group-mediated cognitive-behavioral physical activity intervention. Int J Beh Nutr Phys Activity. 2006;3:23. doi: 10.1186/1479-S868-3-23. Open Access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cramp AG, Brawley LR. Sustaining self-regulatory efficacy and proximal outcome expectations for postnatal exercise: Effects of a group-mediated cognitive behavioural intervention. Br J Health Psychol. 2009;14:595–611. doi: 10.1348/135910708X383732. [DOI] [PubMed] [Google Scholar]